Chapter 32 Percutaneous approaches to the treatment of gallbladder disease
Image-Guided Intervention
Image-guided interventional techniques have been developed to provide minimally invasive treatment of gallbladder disease (see Chapters 28 and 31). Percutaneous, image-guided cholecystostomy is now an accepted method to decompress the acutely inflamed gallbladder if surgery is not indicated. Various methods aiming at elective, nonsurgical removal of gallbladder stones were introduced in the early 1990s, including extracorporeal shock-wave lithotripsy (ESWL), contact dissolution of gallstones with methyl tert-butyl ether (MTBE), and percutaneous mechanical cholecystolithotomy. As a result of the successful introduction of laparoscopic cholecystectomy (see Chapter 34), surgical treatment of cholecystolithiasis has become less invasive, and definitive treatment of cholecystolithiasis may be accomplished with much shorter hospitalization. Because none of the existing nonsurgical techniques of gallstone removal can prevent recurrent gallstone formation, the indication to perform percutaneous gallstone removal without surgery is now very limited. This chapter gives an overview of image-guided treatment methods for gallbladder disease.
Percutaneous Cholecystostomy for Acute Cholecystitis
Surgical cholecystostomy (see Chapters 28 and 31) has long been used to provide external decompression of the acutely inflamed gallbladder in patients who are at high risk for operation or general anesthesia, such as those with sepsis, diabetes, or severe cardiac, pulmonary, hepatic, or renal failure. Percutaneous cholecystostomy was initially developed to provide a minimally invasive method of gallbladder decompression in elderly and very ill patients with acute acalculous or calculous cholecystitis or with gallbladder hydrops secondary to malignant disease (Elyaderani & Gabriele, 1979; Pearse et al, 1984). Percutaneous cholecystostomy also has been used to treat complications of cholecystitis (e.g., gallbladder perforation, empyema, or pericholecystic abscesses) or as an alternative to percutaneous transhepatic drainage of the bile ducts in obstructive jaundice. More recently, percutaneous cholecystostomy has been used to provide access to the gallbladder for elective gallstone treatment with stone dissolution techniques, percutaneous cholecystolithotomy, or other techniques.
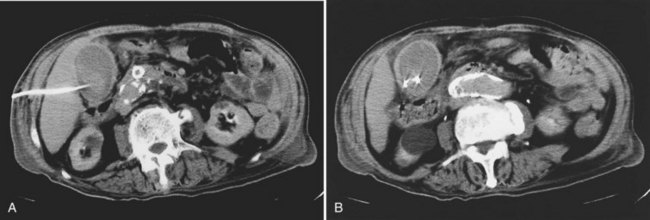
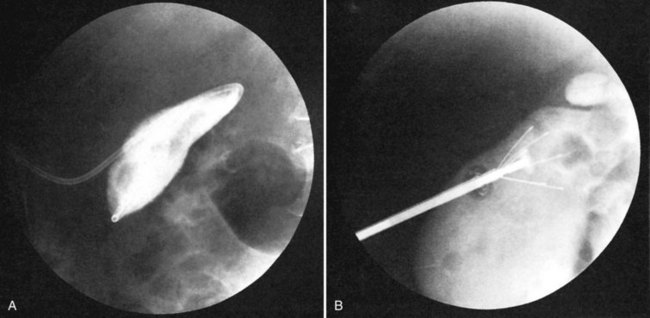
The percutaneous access route to the gallbladder usually is determined with ultrasound (US) and is based on the individual anatomic situation. Computed tomography (CT) can be used if US does not provide sufficient information. Most authors favor the transhepatic approach to the gallbladder, because a puncture through the attached portion of the gallbladder should reduce the risk of bile leakage into the peritoneal cavity (Fig. 32.1). The area of attachment cannot be anticipated reliably with imaging techniques, and the direct, transperitoneal route also has been used successfully (Vogelzang & Nemcek, 1988). The acutely inflamed gallbladder is usually distended and immediately adjacent to the anterior abdominal wall, and the direct approach through the gallbladder fundus avoids the trauma to the liver that may be associated with percutaneous gallstone removal at a later date. The use of a removable percutaneous anchor was proposed to prevent the gallbladder wall from moving away from the trocar or from the catheter during exchange over a guidewire (Cope et al, 1990).
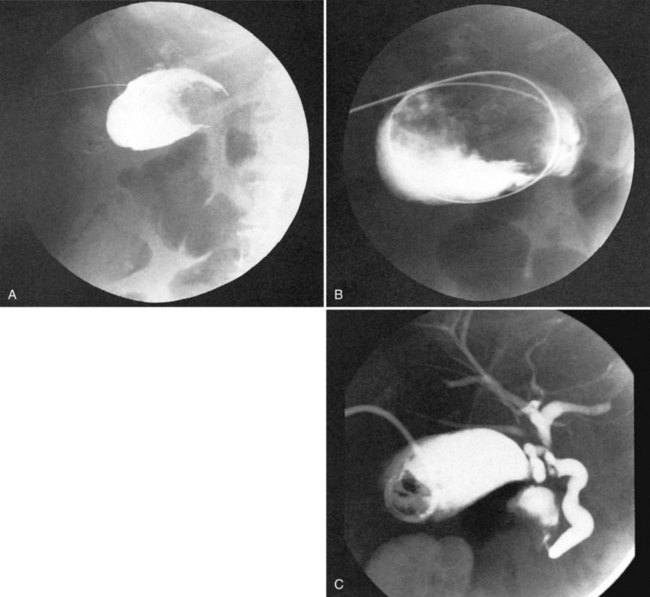
The initial gallbladder puncture is performed under local anesthesia, and prophylactic administration of atropine has been recommended to prevent vasovagal reactions (vanSonnenberg et al, 1984). With portable US equipment, the percutaneous cholecystostomy procedure can be performed at the patient’s bedside (e.g., in the intensive care unit). If there is doubt regarding a safe access route, however, it may be preferable to combine US or CT with fluoroscopy (Fig. 32.2). Several suitable needle/catheter or needle/guidewire systems are available, and the optimal method of catheter introduction is a matter of personal preference. Repeat punctures with introducer needles should be avoided, because leakage of gallbladder content through the puncture channel may lead to internal decompression of the gallbladder into the peritoneal cavity and prevent further attempts to enter the gallbladder lumen. A catheter size of 6.5 to 7 Fr is usually sufficient to provide effective external gallbladder drainage, but 8 Fr or more may be necessary to drain gallbladder empyema or pericholecystic abscesses (Fig. 32.3; vanSonnenberg et al, 1991). If percutaneous cholecystostomy is done for acute cholecystitis, catheter manipulations should be kept to a minimum to avoid inadvertent perforation of the frail inflamed gallbladder wall or leakage of gallbladder contents alongside the catheter. To prevent inadvertent dislodgment of the catheter on the ward, it is preferable to use a self-retaining catheter. Diagnostic cholangiography through the cholecystostomy catheter may be obtained after a few days to assess the presence of gallstones and patency of the cystic duct. It is advisable to leave the cholecystostomy catheter in place for 7 to 10 days to let a tract develop and to avoid bile leakage into the peritoneal cavity.
Although transient right upper quadrant pain is a relatively common side effect of percutaneous cholecystostomy, serious procedure-related complications are uncommon. In a review of 252 percutaneous cholecystostomies reported in the English language literature, there were 4 cases of bile peritonitis and 1 death (0.3%); other procedure-related complications included vasovagal reaction or hypotension, self-limited hemobilia, and acute cholecystitis secondary to an impacted stone in the cystic duct (Teplick, 1989). In a series of 127 patients undergoing gallbladder puncture and cholecystostomy, the reported rate of minor and major complications was 3.9% and 8.7%, respectively. The 30-day mortality rate of that series was 3.1%, but all deaths were due to underlying diseases (vanSonnenberg et al, 1992).
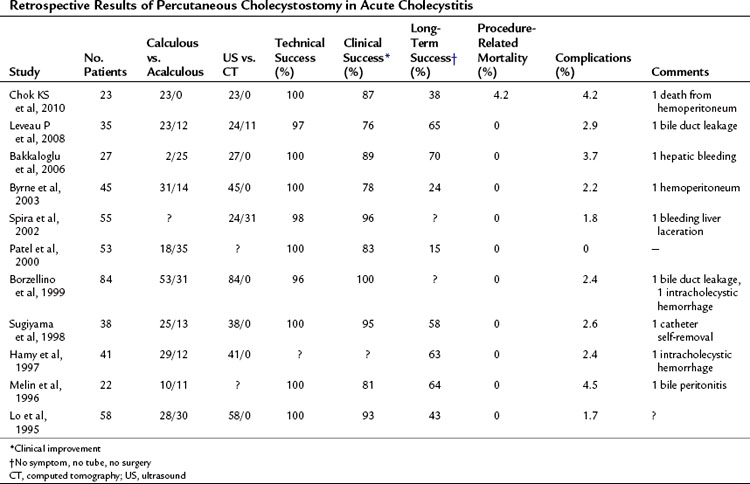
In view of the severely compromised health of most patients undergoing the procedure, percutaneous cholecystostomy is relatively safe. The efficacy of percutaneous cholecystostomy is difficult to determine, because the diagnosis of acute cholecystitis is often unreliable in patients with multiple concomitant medical and surgical problems (McGahan & Lindfors, 1988, 1989). If the indication for percutaneous cholecystostomy is restricted to patients with clinical or imaging findings of acute cholecystitis, a response rate of 90% can be expected (van Overhagen et al, 1996). If patients with unexplained abdominal sepsis are included, the response rate is lower (Boland et al, 1994; Lee et al, 1991; McGahan & Lindfors, 1989). In patients with acute acalculous cholecystitis, interval cholecystectomy may be unnecessary, and percutaneous cholecystostomy may be a definitive therapy (Vauthey et al, 1992). A randomized, controlled trial showed that percutaneous cholecystostomy and drainage is significantly more effective than simple gallbadder aspiration (Ito et al, 2004). Results of retrospective clinical studies on percutaneous cholecystostomy are summarized in Table 32.1. Current experience indicates that percutaneous cholecystostomy is an effective temporizing measure in elderly or critically ill patients with acute cholecystitis and a safe alternative to emergency surgery (Chok et al, 2010). Recently, this has been recognized by a surgical consensus conference (Miura et al, 2007). In clinical situations that warrant, interval cholecystectomy can be performed on an elective basis.
Nonsurgical Techniques to Remove Gallbladder Stones
Percutaneous Gallstone Removal via Cholecystostomy
Percutaneous Contact Dissolution of Gallbladder Stones with Methyl Tert-Butyl Ether
MTBE is the most potent cholesterol solvent available. Because of its boiling point of 55.2° C, it remains liquid at body temperature and is easier to handle than diethyl ether. Direct instillation of MTBE through a small percutaneous cholecystostomy catheter has been used successfully to dissolve cholesterol stones of the gallbladder within hours (Allen, 1985). Most treatments with MTBE have been done on an elective basis in patients who had an increased risk of surgery or anesthesia because of coexisting medical conditions or who refused to undergo surgery for other reasons (Hellstern et al, 1990; Thistle et al, 1989). The selection criteria for MTBE therapy includes symptomatic uncomplicated gallstone disease, uncalcified gallstones on CT, and normal hepatic laboratory test results.
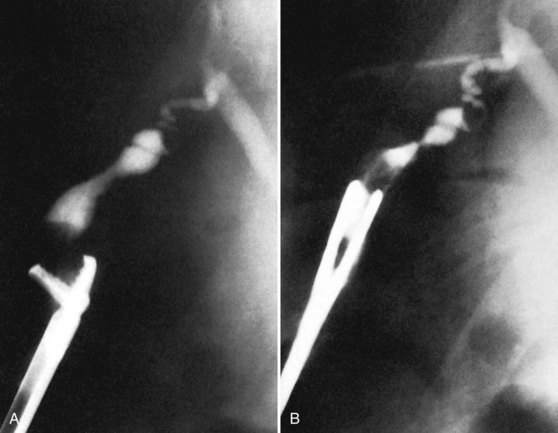
The use of MTBE requires several precautions. Because of its unpleasant odor, inflammability, and anesthetic effect, MTBE must be used in a well-ventilated room. Catheters, syringes, and stopcocks must be made of special materials, such as Teflon, polyethylene, glass, and metal. After percutaneous cholecystostomy, a 5-Fr pigtail catheter is positioned within the gallbladder under fluoroscopic control so as to provide close contact with the gallstones to be dissolved. The gallbladder overflow volume is assessed by contrast injection into the gallbladder. A similar volume of MTBE is instilled and aspirated in continuous cycles (Fig. 32.4). Depending on the stone volume, complete dissolution is usually accomplished during a hospitalization of 2 to 3 days with several hours of treatment each day.
Minor side effects include nausea, vomiting, or a burning sensation in the right upper abdomen, which may be due to the drug itself, to minor leakage of bile alongside the catheter, or to catheter manipulations within the gallbladder. Serious complications, such as major bile leakage, hemobilia, or stone impaction in the cystic duct or common bile duct, are uncommon. The success rate of MTBE dissolution treatment has been reported to be 96%, although residual debris was still visible on US in many patients at the time of discharge (Hellstern et al, 1990; Thistle, 1991; Thistle et al, 1989). In the era of laparoscopic cholecystectomy, indications for MTBE dissolution treatment of gallbladder calculi are rare (see Chapter 34).
Percutaneous Cholecystolithotomy
The term percutaneous cholecystolithotomy is used to describe a variety of techniques to remove gallbladder stones percutaneously. In contrast to MTBE dissolution treatment, percutaneous cholecystolithotomy can be done regardless of the size, number, and composition of the calculi. A small, shrunken, thick-walled gallbladder generally is considered a contraindication to all forms of percutaneous cholecystolithotomy. The common steps of all techniques of percutaneous cholecystolithotomy are 1) percutaneous access to the gallbladder by means of percutaneous cholecystostomy; 2) immediate or sequential dilation of the cholecystostomy tract to a relatively large size, ranging from 10 to 30 Fr; 3) introduction of instruments for gallstone fragmentation and removal; and 4) external drainage of the gallbladder after the procedure (Akiyama et al, 1985; Kerlan et al, 1985).
Regardless of the technique used for tract dilation, the procedure is painful unless performed under intravenous sedation or general anesthesia. The most important risks are hemorrhage if a transhepatic access is used and bile leakage and loss of access if a subhepatic transperitoneal route is chosen. Smaller calculi can be removed with wire baskets (Cope et al, 1990). Fragmentation of larger calculi may be done with electrohydraulic, ultrasonic, or laser-mediated intracorporeal lithotripsy (Bogan et al, 1989; Burhenne, 1975; Gillams et al, 1992; Picus et al, 1989). These techniques require direct contact between the lithotripsy probes and the calculi under endoscopic vision. The rotary gallstone lithotrite was specially designed for percutaneous gallstone lithotripsy and enables pulverization of gallbladder calculi in a manner similar to a household blender: the device consists of a six-pronged basket surrounding a 3-mm impeller, which rotates in a 7-Fr catheter at 30,000 rpm, pulling the stones into the basket and crushing the stones into fragments smaller than 2 mm within minutes (Miller et al, 1991a, 1991b, 1991c). This technique can be performed under fluoroscopic vision and requires a percutaneous tract no larger than 10 Fr. Because the device must be able to open freely within the gallbladder, the stone volume should not exceed 75% of the volume of the gallbladder (Fig. 32.5).
The technical success rate of percutaneous cholecystolithotomy is 88% (Gillams et al, 1992). Procedure-related complications occur in 15% and include subhepatic bile collections, cholangitis, gallbladder perforation with pericholecystitis, and wound infections. Although in the early 1990s elective percutaneous cholecystolithotomy was proposed to avoid cholecystectomy in patients with symptomatic but uncomplicated cholecystolithiasis, this indication seems to be obsolete in the era of laparoscopic cholecystectomy. Now most procedures are done on an elective basis.
Combined Surgical and Radiologic Intervention: Minicholecystostomy
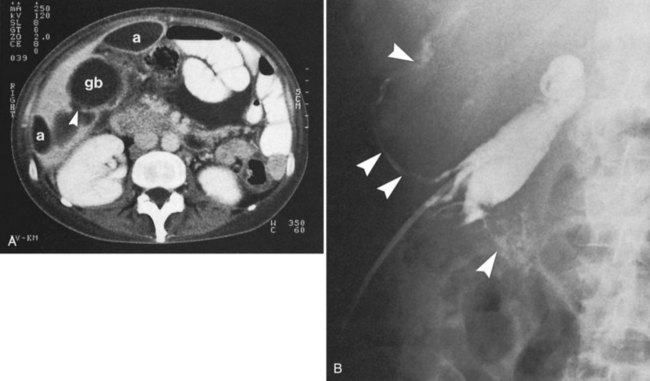
The minicholecystostomy procedure was described by Burhenne and Stoller (1985) and included provision of emergency decompression of the gallbladder and the possibility of percutaneous stone removal 7 to 10 days later without the need for tract dilation. After localization of the gallbladder by US, a small abdominal incision is made over the gallbladder fundus under local anesthesia and intravenous analgesia. A 24-Fr Foley catheter is placed into the gallbladder, and the fundus of the gallbladder is sutured to the combined peritoneum and posterior layer of the rectus sheath, creating a short, wide tract. After 1 week of external gallbladder drainage, the gallstones can be removed under fluoroscopic control, usually without analgesia. Large stones can be fragmented with stone-crushing forceps and removed mechanically with a variety of instruments (Fig. 32.6).
The minicholecystostomy approach avoids the risks of hepatic hemorrhage, bile leakage, and vasovagal reactions associated with dilation of a percutaneous cholecystostomy tract, and it facilitates repeated subhepatic access to the gallbladder. The success rate of stone removal was 97% for gallbladder stones, 86% for cystic duct stones, and 63% for common bile duct stones; no serious complications and no deaths resulted (Burhenne & Stoller, 1985; Gibney et al, 1987). Given the safety and efficacy of laparoscopic cholecystectomy and percutaneous cholecystostomy, this technique is rarely indicated.
Extracorporeal Shock-Wave Lithotripsy
ESWL of gallstones was developed in the 1980s as a noninvasive form of treatment in selected patients with symptomatic, uncomplicated cholecystolithiasis (Burhenne et al, 1989; Sackmann et al, 1991; Sauerbruch et al, 1986). The original investigators and most subsequent investigators used relatively strict selection criteria, including a normal gallbladder on US, opacification of the gallbladder on oral cholecystography, and a limited number (one to three) and size (0.5 to 3 cm) of calculi. Cholestasis, pancreatitis, severe liver disease, hemorrhagic diathesis, abdominal aortic aneurysm, and pregnancy are considered contraindications, and most treatment protocols restrict ESWL treatment to calculi consisting of cholesterol, and they combine ESWL with adjuvant oral bile acid therapy. Usually two competing mechanisms lead to clearance of fragments from the gallbladder after ESWL: spontaneous passage of fragments through the cystic duct and fragment dissolution within the gallbladder by the adjuvant bile acids. ESWL alone also may lead to successful gallbladder clearance, regardless of the composition of the calculi, but a high number of shock waves and multiple treatment sessions are often needed (Fache et al, 1990; Rawat & Burhenne, 1990).
The rate of fragment clearance after ESWL depends on the total stone volume and on the size of the largest remaining fragment. On average, 70% of patients are stone free within 1 year, and 80% are stone free within 1.5 years after successful ESWL and adjuvant bile acid therapy (Becker et al, 1992; Ell et al, 1990; Sackmann et al, 1991). If only patients with solitary gallstones 2 cm in diameter are treated, the stone clearance rate is 80% to 90% within 6 to 18 months (Pauletzki et al, 1994; Sackmann et al, 1991). The problem of gallstone recurrence remains unresolved. Studies have shown that more than two thirds of patients develop recurrence within 6 years, and it is argued that laparoscopic cholecystectomy should be performed in the first place (Barkun et al, 1997; Borch et al, 1996; Cesmeli et al, 1999; Go et al, 1995).
Percutaneous Ablation of the Gallbladder
Despite successful gallstone removal, none of the percutaneous techniques can provide definitive cure of gallstone disease, because the abnormal, lithogenic gallbladder remains in place. It must also be considered that gallbladder-preserving treatment does not eliminate the risk of gallbladder carcinoma (So et al, 1990).
Nonsurgical ablation of the gallbladder may be defined as fibrotic obliteration of the gallbladder lumen. Ideally, the gallbladder mucosa would be eradicated completely, because this not only would eliminate the possibility of gallstone recurrence but also the long-term risk of gallbladder adenocarcinoma. Percutaneous gallbladder ablation was developed and tested experimentally and clinically to prevent gallstone recurrence by eliminating the functioning gallbladder through a cholecystostomy. A two-step approach was developed, including preliminary obliteration of the cystic duct by means of bipolar radiofrequency electrocautery and subsequent sclerotherapy of the gallbladder. Concentrated ethanol and sodium tetradecyl sulfate were used for gallbladder sclerotherapy without toxic side effects. Histologic studies in preliminary animal experiments revealed necrosis of the gallbladder wall within 2 weeks and fibrotic obliteration of the gallbladder within 8 weeks (Becker et al, 1988, 1989). The ablation procedure was tested in a group of 10 patients who, because of multiple medical risk factors, had undergone cholecystostomy instead of cholecystectomy for acute gallbladder disease (Becker et al, 1990). Although follow-up US studies gave no evidence of mucocele formation or stone recurrence, small gallbladder lumina remained visible in all patients, indicating that mucosal ablation was still incomplete. Although occasional attempts at gallbladder ablation have been reported by other investigators (van Overhagen et al, 1996), further technical improvements would be needed before wider clinical application.
Akiyama H, et al. A new method for nonsurgical cholecystolithotomy. Surg Gynecol Obstet. 1985;161:73-74.
Allen MJ. Cholelitholysis using methyl tertiary butyl ether. Gastroenterology. 1985;88:122-125.
Bakkaloglu H, et al. Ultrasound guided percutaneous cholecystotomy in high-risk patients for surgical intervention. World J Gastroenterol. 2006;12:7179-7182.
Barkun AN, et al. McGill Gallstone Treatment Group. Costs and effectiveness of extracorporeal gallbladder stone shockwave lithotripsy versus laparoscopic cholecystectomy: a randomized clinical trial. Int J Technol Assess Health Care. 1997;13:589-601.
Becker CD, et al. Long-term occlusion of the porcine cystic duct by endoluminal radiofrequency electrocoagulation. Radiology. 1988;167:63-68.
Becker CD, et al. Gallbladder ablation through radiologic intervention: an experimental alternative to cholecystectomy. Radiology. 1989;171:235-240.
Becker CD, et al. Ablation of the cystic duct and gallbladder: clinical observations. Radiology. 1990;176:687-690.
Becker CD, et al. Cholecystolithiasis: three years experience with ultrasound-guided electromagnetic shock-wave lithotripsy. Eur Radiol. 1992;2:478-482.
Becker GJ. Can the newer interventional procedures replace cholecystectomy for cholecystolithiasis? Radiology. 1989;170:574.
Bogan ML, et al. Percutaneous cholecystolithotomy with endoscopic lithotripsy by using a pulsed-dye laser: preliminary experience. Radiology. 1989;173:481.
Boland GW, et al. Percutaneous cholecystostomy in critically ill patients: early response and final outcome in 82 patients. AJR Am J Roentgenol. 1994;163:339-342.
Borch K, et al. Extracorporeal shock-wave lithotripsy of gallbladder stones: an alternative for the selected few. Eur J Surg. 1996;162:379-384.
Borzellino G, et al. Emergency cholecystostomy and subsequent cholecystectomy for acute gallstone cholecystitis in the elderly. Br J Surg. 1999;86:1521-1525.
Burhenne HJ. Electrohydrolytic fragmentation of retained common bile duct stones. Radiology. 1975;117:721-722.
Burhenne HJ, Stoller JL. Minicholecystostomy and radiologic stone extraction in high-risk cholelithiasis patients: preliminary experience. Am J Surg. 1985;149:632-635.
Burhenne HJ, et al. Biliary lithotripsy: early observations in 106 patients: work in progress. Radiology. 1989;171:363-367.
Byrne MF, et al. Percutaneous cholecystostomy in patients with acute cholecystitis: experience of 45 patients at a US referral center. J Am Coll Surg. 2003;197:206-211.
Cesmeli E, et al. Gallstone recurrence after successful shock wave therapy: the magnitude of the problem and the predictive factors. Am J Gastroenterol. 1999;94:474-479.
Chok KS, et al. Results of percutaneous transhepatic cholecystostomy for high-risk surgical patients with acute cholecystitis. ANZ J Surg. 2010;80:280-283.
Cope C, et al. Percutaneous extraction of gallstones in 20 patients. Radiology. 1990;176:19-24.
Ell C, et al. Piezoelectric lithotripsy: stone disintegration and follow-up results in patients with symptomatic gallbladder stones. Gastroenterology. 1990;99:1439-1444.
Elyaderani M, Gabriele OF. Percutaneous cholecystostomy and cholangiography in patients with obstructive jaundice. Radiology. 1979;130:601-602.
Fache JS, et al. Extracorporeal cholecystolithotripsy without oral chemolitholysis. Radiology. 1990;177:719-721.
Gibney RG, et al. Combined surgical and radiologic intervention for complicated cholelithiasis in high-risk patients. Radiology. 1987;165:715-719.
Gillams A, et al. Technical considerations in 113 percutaneous cholecystolithotomies. Radiology. 1992;183:163-166.
Go PM, et al. Symptomatic gallbladder stones: cost-effectiveness of treatment with extracorporeal shock-wave lithotripsy, conventional and laparoscopic cholecystectomy. Surg Endosc. 1995;9:37-41.
Hamy A, et al. Percutaneous cholecystostomy for acute cholecystitis in critically ill patients. Surgery. 1997;121:398-401.
Hellstern A, et al. Gallstone dissolution with methyl-tert-butyl ether: how to avoid complications. Gut. 1990;31:922-925.
Ito K, et al. Percutaneous cholecystostomy versus gallbladder aspiration for acute cholecystitis: a prospective randomized controlled trial. AJR Am J Roentgenol. 2004;183:193-196.
Kerlan RKJr, et al. Percutaneous cholecystolithotomy: preliminary experience. Radiology. 1985;157:653-656.
Lee MJ, et al. Treatment of critically ill patients with sepsis of unknown cause: value of percutaneous cholecystostomy. AJR Am J Roentgenol. 1991;156:1163-1166.
Leveau P, et al. Percutaneous cholecystotomy: a bridge to surgery or definite management of acute cholecystitis in high-risk patients? Scand J Gastroenterol. 2008;43:593-596.
Lo LD, et al. Percutaneous cholecystostomy for the diagnosis and treatment of acute calculous and acalculous cholecystitis. J Vasc Interv Radiol. 1995;6:629-634.
McGahan JP, Lindfors KK. Acute cholecystitis: diagnostic accuracy of percutaneous aspiration of the gallbladder. Radiology. 1988;167:669-671.
McGahan JP, Lindfors KK. Percutaneous cholecystostomy: an alternative to surgical cholecystostomy for acute cholecystitis? Radiology. 1989;173:481-485.
Melin MM, et al. Percutaneous cholecystostomy: a valuable technique in high-risk patients with presumed acute cholecystitis. Br J Surg. 1996;83:1274-1277.
Miller FJ, et al. Percutaneous rotational contact biliary lithotripsy: initial clinical results with the Kensey Nash lithotrite. Radiology. 1991;178:781-785.
Miller FJ, et al, 1991b: Rotatory gallstone cholecystolithotripsy. Presented at the IV International Symposium on Biliary Stone Therapy, October 2-4, Rochester, MN.
Miller FJ, et al. Rotary gallstone lithotripsy: follow-up in 19 patients. In: Paumgartner, G, et al. Lithotripsy and Related Techniques for Gallstone Treatment. St Louis: Mosby Year Book; 1991:155-158.
Miura F, et al. Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg. 2007;14:27-34.
Patel M, et al. Percutaneous cholecystostomy is an effective treatment for high-risk patients with acute cholecystitis. Am Surg. 2000;66:33-37.
Pauletzki J, et al. Gallbladder emptying determines early gallstone clearance after shock-wave lithotripsy. Gastroenterology. 1994;107:1496-1502.
Pearse DM, et al. Percutaneous cholecystostomy in acute cholecystitis and common bile duct obstruction. Radiology. 1984;152:365-367.
Picus D, et al. Percutaneous cholecystolithotomy preliminary experience and technical considerations. Radiology. 1989;173:487.
Rawat B, Burhenne HJ. Extracorporeal shock-wave lithotripsy of calcified gallstones: work in progress. Radiology. 1990;175:667-670.
Sackmann M, et al. Early gallstone recurrence rate after successful shock-wave therapy. Gastroenterology. 1990;98:392-396.
Sackmann M, et al. The Munich Gallbladder Lithotripsy Study: results of the first 5 years with 711 patients. Ann Intern Med. 1991;114:290-296.
Sauerbruch T, et al. Fragmentation of gallstones by extracorporeal shock waves. N Engl J Med. 1986;314:818-822.
So CB, et al. Carcinoma of the gallbladder: a risk associated with gallbladder-preserving treatments for cholelithiasis. Radiology. 1990;174:127-130.
Spira RM, et al. Percutaneous cholecystostomy and delayed laparoscopic cholecystectomy in critically ill patients with acute calculous cholecystitis. Am J Surg. 2002;183:62-66.
Sugiyama M, et al. Is percutaneous cholecystostomy the optimal treatment for acute cholecystitis in the very elderly? World J Surg. 1998;22:459-463.
Teplick SK. Diagnostic and therapeutic interventional gallbladder procedures. AJR Am J Roentgenol. 1989;152:913-916.
Thistle JL, 1991: Stone recurrence following MTBE dissolution. Presented at the Fourth International Symposium on Biliary Stone Therapy. October 2-4, Rochester, MN.
Thistle JL, et al. Dissolution of cholesterol gallbladder stones by methyl-tert-butyl ether administered by percutaneous transhepatic catheter. N Engl J Med. 1989;320:633-639.
van Overhagen H, et al. Percutaneous cholecystectomy for patients with acute cholecystitis and an increased surgical risk. Cardiovasc Intervent Radiol. 1996;19:72-76.
vanSonnenberg E, et al. Life-threatening vagal reactions associated with percutaneous cholecystostomy. Radiology. 1984;151:377-380.
vanSonnenberg E, et al. Percutaneous treatment of gallbladder perforation and bile leakage. Radiology. 1991;178:687-689.
vanSonnenberg E, et al. Percutaneous gallbladder puncture and cholecystostomy: results, complications and caveats for safety. Radiology. 1992;183:167-170.
Vauthey JN, et al. Percutaneous cholecystostomy for acute cholecystitis: indications and limitations. Surg Gynecol Obstet. 1992;176:49-54.
Vogelzang RL, Nemcek AAJr. Percutaneous cholecystostomy: diagnostic and therapeutic efficacy. Radiology. 1988;168:29-34.