Morphea

Management strategy
Initial evaluation
The initial evaluation of patients with morphea should involve:
 Questions regarding recent development of new lesions/extension of existing lesions to determine level of activity
Questions regarding recent development of new lesions/extension of existing lesions to determine level of activity
 Symptoms (pain/itch) associated with activity, musculoskeletal complaints, eye complaints (especially en coup de sabre/hemifacial atrophy)
Symptoms (pain/itch) associated with activity, musculoskeletal complaints, eye complaints (especially en coup de sabre/hemifacial atrophy)
 Total body examination of the skin (patients frequently do not appreciate the extent of lesions) looking for active/inactive lesions
Total body examination of the skin (patients frequently do not appreciate the extent of lesions) looking for active/inactive lesions
 Palpation of affected areas for depth of sclerosis
Palpation of affected areas for depth of sclerosis
 Examination for limited range of motion, contracture, limb length discrepancy, and evidence of musculoskeletal involvement
Examination for limited range of motion, contracture, limb length discrepancy, and evidence of musculoskeletal involvement
 Imaging with MRI if musculoskeletal involvement is suspected.
Imaging with MRI if musculoskeletal involvement is suspected.
Active morphea lesions should be treated as the lesions are frequently symptomatic and can produce permanent cosmetic and functional sequelae. Initial evaluation should be focused on determining the extent, severity, and activity of morphea lesions laying the groundwork for rational therapeutic choices.
Specific investigations
First-line therapies
Second-line therapies








 Phototherapy: BB-UVA, NB-UVB, UVA1
Phototherapy: BB-UVA, NB-UVB, UVA1 Methotrexate + IV corticosteroids (PCMT)
Methotrexate + IV corticosteroids (PCMT) Methotrexate + oral steroids
Methotrexate + oral steroids Calciprotriene under occlusion
Calciprotriene under occlusion Topical tacrolimus (occluded)
Topical tacrolimus (occluded) Intralesional steroids
Intralesional steroids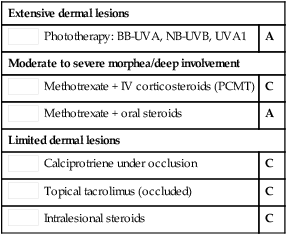
 PUVA (bath or cream)
PUVA (bath or cream) Mycophenolate mofetil
Mycophenolate mofetil Abatacept
Abatacept Imiquimod
Imiquimod Calciprotriol–betamethasone
Calciprotriol–betamethasone Cyclosporine
Cyclosporine Combination of oral medications
Combination of oral medications Combination of oral medications with light
Combination of oral medications with light








