CHAPTER 7 The hand
Note that the separation of conditions into those affecting the wrist and those affecting the hand has been done for convenience, and that in many cases examination of both regions is necessary.
Dupuytren’s Contracture
In this condition there is nodular thickening and a contracture of the palmar fascia. The palm of the hand is affected first, followed at a later stage by the fingers. The ring finger is most frequently involved, followed by the little and middle fingers. The index and even the thumb may be affected. In some cases there is corresponding thickening of the plantar fascia. The progressive flexion of the affected fingers interferes with the function of the hand and may be so severe that the fingernails dig into the palm. The condition mainly affects men over the age of 40. There is a definite genetic predisposition in 60–70% of cases, and in some cases there may be an association with epilepsy, diabetes or alcoholic cirrhosis. There is a distinct geographical distribution: it is rare in Africa, India and China. Below the age of 40, and in either sex, its onset may be precipitated by trauma. Under these circumstances it may pursue a particularly rapid course.
As far as treatment is concerned, a waiting policy may be pursued if the condition is confined to the palms. When the fingers are affected surgical treatment is usually advised, but this is complicated by a number of factors. If the fingers have been held in a flexed position for a long time, secondary changes in the interphalangeal joints may prevent finger extension even after the involved tissue has been removed. In the case of the little finger, amputation in these circumstances may be the best line of treatment. The digital nerve sheaths may blend with the fascia so that dissection is tedious and difficult; involvement of the skin may necessitate Z-plasties or other plastic procedures; and the patient’s age and general health may be adverse factors. In most cases wide excision of the affected fascia is advised. When this is not possible, improvement in function, often lasting for some years, may follow simple division of the contracted fascia in the palm.
Vibration Syndromes
Prolonged exposure to high-frequency vibration (such as may be experienced from the use of jack hammers or hand-held buffing, riveting and caulking machines) may affect bone, nerves and blood vessels. Bone is rarely affected to a significant degree, but new bone formation and hairline fractures (which are slow to heal) are sometimes seen. Involvement of the peripheral nerves may lead to pain and paraesthesia, numbness, tremor, loss of fine touch sensation, proprioception and discrimination. There may be muscle denervation and weakness involving especially the small muscles of the hand. In the case of the peripheral blood vessels there is disturbance of their autonomic control, and the arterioles of the hand become hypersensitive to cold and vibration. In the typical case there are attacks in which one or more fingers turn white on exposure to cold (‘episodic blanching’), with reactive hyperaemia on warming; and there is usually associated discomfort and clumsiness of the hand during attacks. As the condition progresses more fingers become involved, incidents occur both in summer and in winter, and hand function becomes permanently disturbed. The hand becomes weak and clumsy, and with impaired sensation and proprioception the patient has difficulty in dressing (e.g. doing up buttons and shoelaces), handling small objects (e.g. coins, nuts and screws), and carrying out many other tasks (e.g. tying fishing hooks). The differential diagnosis includes Raynaud’s disease, cervical rib and the costoclavicular syndrome, cervical spondylosis, and sensitivity to β-blockers.
There are a number of classifications of the stages of the condition, and the long-established Taylor–Pelmear scale is still widely used (Table 7.1). Well established cases are recognised as one of the prescribed diseases under the Social Security Act, and the qualifying criteria are clearly stated. (The condition must occur throughout the year, involve at least three fingers of one hand (with the middle and/or proximal phalanges being affected), and be due to exposure to vibrating tools.) No treatment is effective, but deterioration may be slowed or prevented by avoiding further exposure to vibration.
Table 7.1 The Taylor–Pelmear scale
| Stage | Condition of digits | Work and social interference |
|---|---|---|
| 0 | No blanching of digits | No complaints |
| 0T | Intermittent tingling | No interference with activities |
| 0N | Intermittent numbness | No interference with activities |
| 1 | Blanching of one or more fingertips, with or without tingling or numbness | No interference with activities |
| 2 | Blanching of one or more fingers, with numbness; usually confined to winter | Slight interference with home and social activities; no interference at work |
| 3 | Extensive blanching. Frequent episodes, summer and winter | Definite interference at work, at home, and with social activities. Restriction of hobbies |
| 4 | Extensive blanching. Most or all fingers affected. Frequent episodes, summer and winter | Occupation changed to avoid further exposure to vibration because of severity of signs and symptoms |
Tendon and Tendon Sheath Lesions
See also under Rheumatoid arthritis.
Mallet finger
In a mallet finger the distal interphalangeal joint is held in a permanent position of flexion; the deformity may be moderate or complete. The patient is unable to extend the distal joint of the finger, either not at all or only incompletely. The problem is that the extensor tendon, usually as a result of trauma, either ruptures close to its insertion in the distal phalanx, or it avulses its bony attachment. Healing may occur spontaneously over a 6–12-month period, but it is usual practice to treat these injuries for 6 weeks with a light splint that holds the distal interphalangeal joint in extension.
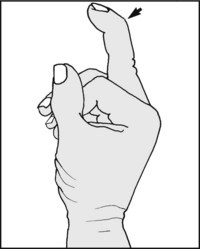
Mallet thumb
Delayed rupture of the extensor pollicis longus tendon may follow Colles’ fracture (see Ch. 6) or rheumatoid arthritis, and repair by tendon transfer (using extensor indicis proprius) is usually advised. If the tendon is damaged by an incised wound, repair by direct suture is undertaken.
Boutonnière deformity
Flexion of the interphalangeal joint of a finger with extension of the distal interphalangeal joint characterises this deformity, which is due to detachment of the central slip of the extensor tendon which is attached to the base of the middle phalanx. This may follow incised wounds on the dorsum of the finger and avulsion injuries, but is more commonly seen in rheumatoid arthritis. Surgical repair of the extensor band is often undertaken for isolated lesions of this type.
Extensor tendon division in the back of the hand
Extensor tendons divided by wounds on the back of the hand carry an excellent prognosis and are treated by primary suture and splintage for approximately 4 weeks.
Profundus tendon injuries
Trigger finger and thumb
This condition results from thickening of a fibrous tendon sheath or nodular thickening in a flexor tendon.
In young children the thumb is held flexed at the metacarpophalangeal (MP) joint, and a nodular thickening in front of the MP joint is palpable; not infrequently the deformity is wrongly considered to be congenital in origin and untreatable.
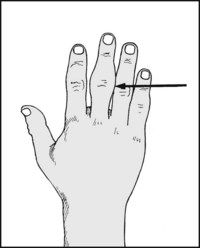
In adults, the middle or ring finger is most frequently involved. When the fingers are extended the affected finger lags behind and then quite suddenly straightens. Nodular thickening, always at the level of the MP joint, may also be palpable. Division of the sheath at the level of the MP joint gives an immediate and gratifying cure, although it should be noted that in children spontaneous resolution occurs in more than 60% of cases.
Rheumatoid Arthritis
Rheumatoid arthritis, as is well known, very frequently affects the hand, and as it progresses may involve joints, tendons, muscles, nerves and arteries, producing most severe deformities and crippling effects on hand function.
In the earliest phases the hands are strikingly warm and moist; later the joints become obviously swollen and tender. Synovial tendon sheath and joint thickening, with effusion, muscle wasting and deformity, then becomes apparent. Tendon ruptures and joint subluxations are the main factors leading to the more severe deformities.
Surgery of the rheumatoid hand is highly specialised, requiring particular skills and experience in judgement, timing and technique, and is difficult to summarise with any accuracy.
In the earliest stages of the disease, medications which have analgesic, anti-inflammatory and antiautoimmune effects may be prescribed, with the judicious use of physiotherapy and splintage to alleviate pain, preserve movement and minimise deformity. When there is much synovial thickening at a stage before joint destruction has advanced, synovectomy is often helpful in alleviating pain and delaying local progress of the condition. In a few well selected cases, where there is severe joint destruction and progressive deformity, joint replacement may be helpful; some cases of major tendon involvement may benefit from repair and other procedures.
Osteoarthritis of the Interphalangeal Joints
Nodular swellings situated dorsally over the bases of the distal phalanges (Heberden’s nodes), or less commonly over the bases of the middle phalanges (Bouchard’s nodes), are a sign of osteoarthritis of the finger joints. They occur most frequently in women after the menopause, and are often familial. They are not related to osteoarthritis elsewhere. In many cases they are symptom free, but they may be associated with progressive joint damage which does cause pain.
Carpometacarpal Joint of the Thumb
Osteoarthritic changes are common between the thumb metacarpal and the trapezium, and they may give rise to disabling pain and impaired function in the hand. There may on occasion be a history of a previous Bennett’s fracture, or of occupational overuse. Several surgical procedures (e.g. excision of the trapezium) are available which give relief of pain, sometimes at the expense of some functional loss.
Tumours in the Hand
Tumours in the hand are not uncommon. Most involve the soft tissues and are simple, but it need hardly be stressed that where the diagnosis is uncertain a full investigation is essential. Among the commonest tumours are the following:
Infections in the Hand
These three common infections are treated along well established lines, using antibiotics and surgical drainage if pus has formed.

Look first at the general shape of the hand and its size in proportion to the rest of the patient: e.g. in achondroplasia the fingers are short and stumpy; in acromegaly the hand is large and coarse; and in myxoedema the hand is often podgy and the skin dry.
In Marfan’s syndrome the proximal phalanges in particular are long and thin. In Turner’s syndrome the ring metacarpal is often very short. In hyperparathyroidism the fingertips may be short and bulbous, and in Down’s and Hurler’s syndromes the little fingers are incurved.

Note the presence of any hypertrophy of a finger. This may occur in Paget’s disease, neurofibromatosis and local arteriovenous fistula.
Note the presence of any fusiform swelling. The commonest causes are collateral ligament tears and rheumatoid arthritis. Less commonly this is seen in syphilis, TB, sarcoidosis and gout. In psoriatic arthritis the distal joint is usually involved.
Mallet finger: The distal interphalangeal joint is flexed. The patient cannot extend the terminal phalanx, although the joint can usually be extended passively. It is caused by rupture or avulsion of the extensor tendon, usually from trauma or rheumatoid arthritis.

Mallet thumb: Loss of active extension in the interphalangeal joint of the thumb is due to rupture of extensor pollicis longus. This is seen as a late complication of Colles’ fracture, from rheumatoid arthritis, or wounds of the wrist or the thumb with tendon division.

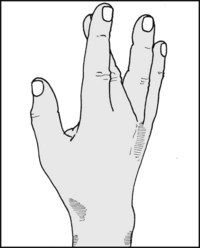
Swan-neck deformity (1): The distal interphalangeal joint is flexed and the proximal interphalangeal joint hyperextended. It is seen most often in rheumatoid arthritis, and may be produced by a number of different factors.

Swan-neck deformity (2): Extend the metacarpophalangeal joint of the affected finger. Improvement in the deformity indicates that shortening of extensor digitorum communis is a factor. If the deformity is made worse, tight interossei are likely to be responsible.

Swan-neck deformity (3): Hold all the fingers in an extended position but leave the affected finger free. Ask the patient to flex it. If he cannot, this indicates a rupture of flexor digitorum sublimis as the cause of the deformity.

Boutonnière deformity: The proximal interphalangeal joint is flexed and the distal joint extended. It occurs when the central extensor tendon slip to the middle phalanx is affected, by a wound on the dorsum of the finger, by traumatic avulsion, or by spontaneous rupture as in rheumatoid arthritis.

Z deformity of the thumb: The thumb is flexed at the metacarpophalangeal joint and hyperextended at the interphalangeal joint. The deformity is seen in rheumatoid arthritis secondary to displacement of the extensor tendons or rupture of flexor pollicis longus.
Flexion of a finger at the metacarpophalangeal joint, with inability to extend, follows rupture or division of the extensor tendon in the back of the hand or at the wrist.

Flexion of the little finger, mainly at the proximal interphalangeal joint, is seen in congenital contracture of the little finger.
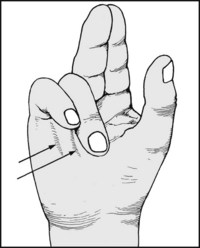
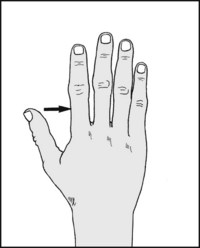
Flexion of the fingers at the metacarpophalangeal and interphalangeal joints, associated with nodular thickening in the palm and fingers, is characteristic of Dupuytren’s contracture. The thumb is occasionally involved.

Flexion of the middle or ring fingers at the proximal interphalangeal joint, with sudden extension on effort or with assistance, is seen in trigger finger. There is usually a palpable nodular thickening over the corresponding metacarpophalangeal joint.

Flexion of the interphalangeal (IP) joint of the thumb in infants and young children is usually due to stenosing tenovaginitis involving flexor pollicis longus. A nodular thickening is usually palpable over the metacarpophalangeal joint. The condition is said to be acquired (i.e. it is not congenital) and triggering is not a feature.

In Volkmann’s ischaemic contracture (which usually occurs as a sequel to brachial artery damage accompanying a supracondylar fracture) there is clawing of the thumb and fingers, and forearm wasting. The fingers can be extended if the wrist is flexed. Slight flexion of all the fingers at the MP and IP joints is sometimes seen in association with diabetes (diabetic cheiropathy); when the hands are put in a praying position, there is an uncloseable gap between them.
Ischaemic contracture of the small muscles of the hand (usually as a result of swelling within a tight forearm plaster) leads to fingers which are flexed at the metacarpophalangeal joints and extended at the interphalangeal joints. The thumb is adducted into the palm.
Ulnar deviation of the fingers at the metacarpophalangeal joints occurs in rheumatoid arthritis. In the later stages the metacarpophalangeal joints may dislocate.

Unilateral hypothenar wasting suggests a root, plexus or nerve lesion. Widespread involvement necessitates a full examination in order to exclude disorders such as generalised peripheral neuropathy, syringomyelia, multiple sclerosis and the muscular dystrophies.
Swellings (1): Note (A) Heberden’s nodes on the dorsal surface of the distal interphalangeal joint. (They are often associated with deviation of the distal phalanx and are a sign of osteoarthritis of the fingers.) (B) The proximal interphalangeal joints may be similarly affected (Bouchard’s nodes).
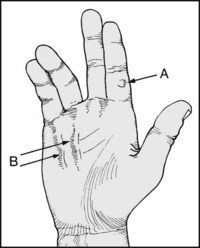
Swellings (2): Note (A) firm, pea-like ganglions are common along the line of the tendon sheaths. (B) Nodular swellings of the palm and fingers accompany Dupuytren’s contracture.
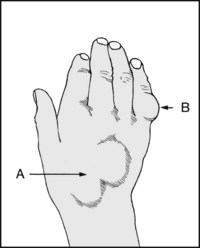
Swellings (3): Note (A) isolated rheumatoid nodules or synovial swellings. (B) Enchondroma is one of the commonest bone tumours to occur in the hand. Tumours of this type are sometimes multiple, and there may be a hereditary diathesis. If small, an enchondroma may not be noticed until it declares itself with a pathological fracture.
Note the nutrition of the skin and nails. In the case of the nails, note any disturbance of growth, deformity, evidence of fungal infection or psoriasis. In the skin, note the presence of finger burns or trophic ulceration, suggestive of a neurological disturbance. Note any alteration of skin colour, suggesting circulatory involvement from local arterial or sympathetic supply disturbance.
Note any generalised or local disturbance of temperature or sweating in the palm or volar surfaces of the fingers. The other hand may be used for comparison.

Palpate the individual finger joints between the finger and thumb, looking for thickening, tenderness, oedema and increased local heat. Note that in gouty arthritis a single joint only may be affected, especially in the early stages.

Try to tuck each finger into the palm, and ask the patient to repeat this unaided. Loss of active movements only is usually due to nerve or tendon discontinuity, whereas passive loss may be due to joint or tendon adhesions or arthritis.
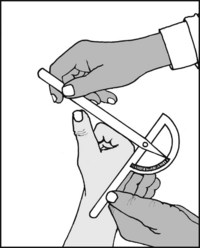
Where indicated for continued assessment or medicolegal purposes, both the active and the passive range in an affected finger should be recorded.
Metacarpophalangeal joint: Normal range = 0–90°.
Note that the metacarpophalangeal joints can usually be passively hyperextended by up to 45°.

Alternatively, ask the patient to put his hand, palm upwards, on a table, and note the linear discrepancy between it and the tip of the affected finger as he attempts to extend it. When passive extension is possible, loss of active extension suggests division, rupture or displacement of the extensor tendons, or a posterior interosseous palsy if all are affected.

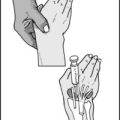
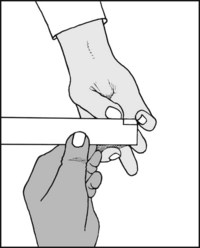
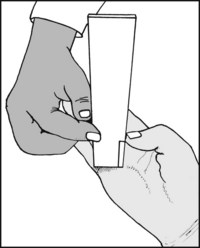
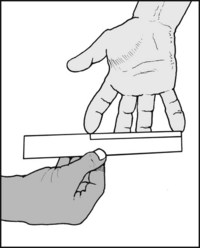
An alternative method of measuring the range of movements in the finger joints involves moulding a length of malleable wire over the finger (14 G, electrician’s or other solder wire, approximately 2 mm in diameter is suitable).

The wire is then transferred to the case record, and an outline drawn round it. The finger which has been examined and date should be noted. An additional record of extension may be superimposed. Subsequent assessment of progress is easily made by repeating the process.
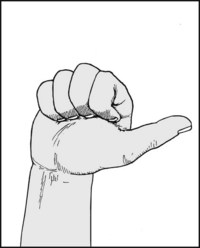
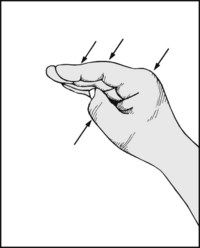
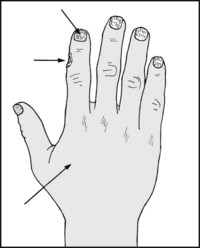
Total finger movements: As all the joints of all the fingers are involved in grasping and holding, ask the patient to make a fist. Normally the distal phalanges should ‘tuck in’, touching the palm at right angles.
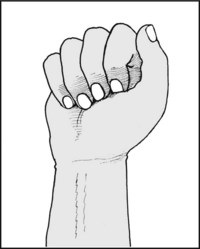
Only a slight loss at any level is sufficient to prevent ‘tuck in’. All the fingers may be involved, as shown. If a single finger is affected its prominence will be obvious. This screening test may be carried out earlier in the examination if desired.
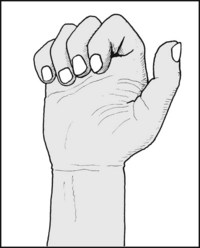
Greater reduction in movements will prevent the fingers from reaching the palm. Such a stand-off indicates more serious impairment of the patient’s ability to grasp and hold.

This important restriction of functional ability may be measured by noting the distance that the fingers stand proud of the palm on maximum flexion.

7.38. Assessment of the causes of loss of movements in the IP joints:
The Bunnell–Littler test: Hold the MP joint of the affected finger in extension and passively flex it, noting the total movement obtained. Now repeat with the MP joint flexed, noting any difference.
Diagnosis: if now greater, contracture of the intrinsic muscles; if the same, joint capsule contractures; if less, an extensor tendon contracture.

7.39. Movements (11): The thumb: The interphalangeal joint:
Normal flexion = 80°; Normal hyperextension = 20° (i.e. the IP joint can be extended 20° beyond the neutral position).

7.40. Movements (12): The thumb: The metacarpophalangeal joint: Normal flexion = about 55°; Normal hyperextension = 5°.

At this stage, test the stability of the metacarpophalangeal joint in a side-to-side plane. Extend the joint and stress the medial collateral ligament. Compare the sides. Excess mobility follows tears (‘gamekeeper’s thumb’) and rheumatoid arthritis, and can be very disabling.

Carpometacarpal joint: test extension (abduction parallel to the plane of the palm) by placing the hand palm down and measuring the range from a position in contact with the index to its fully extended position.
Carpometacarpal joint: test flexion: Measure this starting from the neutral position with the thumb in contact with the index.
Normal range of carpometacarpal flexion = 15°.
This angle is difficult to measure, and an accurate assessment is seldom of value.

Abduction of the thumb in a plane at right angles to the palm: The patient attempts to point the thumb at the ceiling, with the back of the hand resting on a table.

While examining the carpometacarpal joint of the thumb, note any crepitus in the joint. This finding is common when osteoarthritis and rheumatoid arthritis involve this joint, and there is often prominence of the base of the metacarpal.

Opposition (1): This tests several components of overall thumb and little finger movement, and involves abduction of the thumb at right angles to the palm, and thumb flexion and rotation. Normally the thumb should be able to touch the tip of the little finger.
Opposition (2): Loss of opposition may be assessed by measuring the distance between the tip of the thumb and the little finger.
Opposition (3): Alternatively, the distance between the tip of the thumb and the metacarpophalangeal joint of the little finger may be recorded.
Finger abduction may be assessed by measuring the spread between the index and little fingers, or the spread between individual fingers. Excessive abduction of the little finger is found in Ehlers–Danlos syndrome.

In vibration white finger, although little clinical abnormality may be found, (1) note if the hand becomes pale on elevation, and the speed with which it pinks up on depression; (2) see if an attack is precipitated by holding the hand under cold water for 2 minutes; (3) and check the flow in the digital vessels with a Doppler flowmeter. Note that the peripheral circulation may be disturbed by oral antihypertensives.

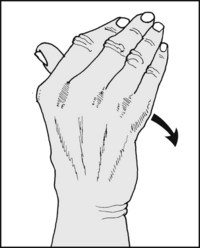
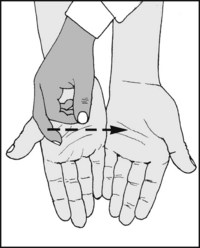
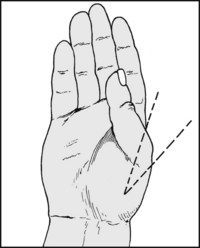
7.51. The Allen test for hand circulation:
Place your thumbs over the patient’s radial and ulnar arteries and get him to clench his hand three times in quick succession (1). Compress the vessels and ask him to extend the fingers. The hand should be blanched (2). Now release the radial artery and note whether the return of skin colour is delayed for more than 3 seconds (3). Repeat the test, this time releasing the ulnar artery. This gives a measure of the contribution made by each artery to the circulation of the hand.

7.52. Joint thickening and swelling:
The activity of the inflammatory process in a swollen joint is sometimes assessed by measuring the joint circumference from time to time. Accuracy without special equipment is difficult to achieve and the results are of limited value.
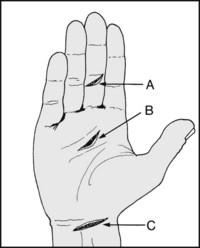
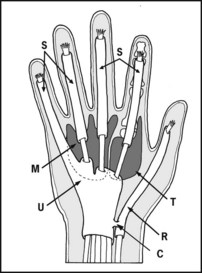
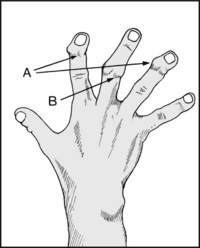
Note first the position of any wound, and try to work out the structures at risk, e.g. (A) flexor profundus, (B) flexor digitorum superficialis (sublimis), and if deeper, flexor digitorum profundus, (C) median nerve, flexor carpi radialis longus, flexor digitorum superficialis, and more deeply the flexor digitorum profundus tendons.
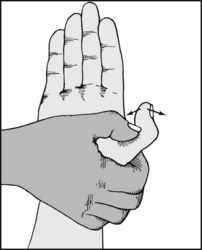
If the profundus tendon is suspect, support the finger and ask the patient to bend the tip. Loss of the ability to flex the terminal phalanx occurs when the flexor digitorum profundus tendon is divided.

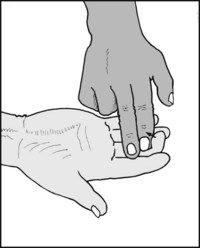
If the superficialis tendon is suspect, hold all the fingers except the suspect one in a fully extended position to neutralise the effect of flexor profundus. If the patient is able to flex the finger at the proximal interphalangeal joint then superficialis is intact.
Flexor and extensor pollicis longus: Support the proximal phalanx and ask the patient to flex and extend the tip.

Extensor digitorum communis: Ask the patient to extend the fingers. Any extensor tendon divided on the dorsum of the hand or finger will be obvious by the lack of extension in the finger, assuming the finger joints have been checked for mobility. To assess the distal slips, grasp the middle phalanx and ask the patient to try to extend the distal IP (DIP) joint.
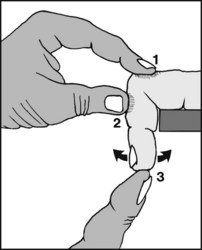
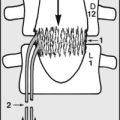
Elson’s middle slip test: Flex the proximal IP (PIP) joint of the finger over the edge of a table and steady the proximal phalanx (1). Ask the patient to try to extend the PIP joint, and feel for any activity (2): PIP extension occurs if the middle slip is intact, but the DIP joint will be flail (3). If the middle slip is ruptured, extension at the PIP joint does not occur and the DIP joint stiffens and extends.
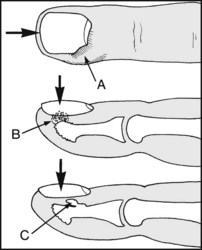
(A) Paronychia is the commonest infection. Pain is aggravated by pressure on the end of the nail. (B) Apical infections give pain which is aggravated by downward pressure on the nail. A subungual exostosis (C) (which can be confirmed by radiographs) may sometimes cause confusion.
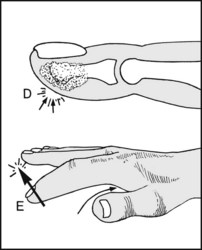
(D) Pulp infections are exquisitely tender and may lead to destruction of the distal phalanx. (E) Tendon sheath infections lead to a fusiform flexed finger. Any attempt to straighten the finger causes pain. Tenderness is marked and localised (usually to the base of the sheath).
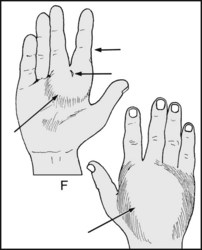
(F) In web space infections there is usually marked swelling of the back of the hand and web, with spreading of the fingers. Note the site of any causal wound.

(G) In thenar and midpalmar space infections there is gross swelling of the hand involving both the dorsal and palmar surfaces. In the case of the thenar space, the swelling may be more pronounced on the radial side of the palm.

7.63. Assessment of the principal functions of the hand (1):
Pinch grip: Ask the patient to pick up a small object between the tips of the thumb and index. Intact sensation is necessary for a satisfactory performance. The patient should be asked to repeat the test with his eyes closed. Note whether the tip of the adjacent middle finger can assist (chuck grip).

Thumb to side of index grip: The patient should be asked to grip a key between the thumb and side of the index in the normal fashion. Test the firmness of the grip by attempting to withdraw the key using your own pinch grip.

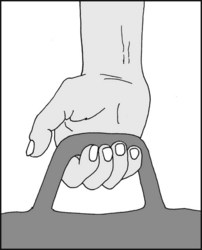
Grasp: Ask the patient to grasp a pen firmly in the hand, using the thumb and fingers. Attempt to withdraw the pen and note the resistance offered. Where finger flexion is restricted, repeat using an object of greater diameter.
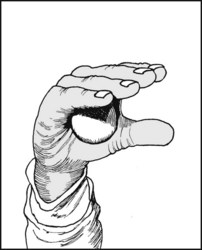
Palmar grasp: Test the cupping action of the hand by asking the patient to grasp a small ball in the palm of the hand. Note the patient’s ability to resist the ball being withdrawn.

Grip strength: This may be tested using a dynamometer; alternatively, inflate a rolled sphygmomanometer cuff to 20 mmHg and ask the patient to squeeze it as hard as he can. A normal hand should be able to achieve a reading of 200 mmHg or over.
7.69. Hand function (7): Bilateral function: Although the function in one hand may be assessed as described, it is important to note that impairment of function in one hand may clearly affect many activities that normally involve both performing together. The degree of overall functional impairment may be investigated by enquiring about, or testing, the patient’s ability to perform certain tasks. When progress is being measured, each of these may be scored on a scale (0–5 or 0–10) and summed. The following list (adapted from tests devised by Lamb et al.) may be found to be helpful, either selected or as a whole:
(See also Assessment of Combined Shoulder and Elbow function and QuickDASH, pp. 57–59).

7.70. Hand radiographs: examples of pathology (1):
in this radiograph of a child’s hand most of the terminal phalanx of the ring finger is no longer visible, and the soft tissue shadow suggests swelling of the digit.
Diagnosis: osteitis and destruction of the terminal phalanx secondary to a pyogenic infection of the pulp of the ring finger.

There is a partially ossified swelling arising from the region of the neck and distal portion of the index metacarpal.

The thumb and index appear quite normal, but the metacarpals and phalanges of the other fingers are distorted with many cystic tumours.
Diagnosis: multiple enchondromata typical of Ollier’s disease (multiple enchondromatosis).

There is broadening and distortion of the proximal end of the thumb metacarpal, narrowing of the carpometacarpal joint space, and lipping.
Diagnosis: the appearances are typical of advanced osteoarthritic changes in the carpometacarpal joint of the thumb.

There is narrowing of the distal interphalangeal joint and subluxation of the distal phalanx of this finger.
Diagnosis: the appearances are typical of osteoarthritis, and Heberden’s nodes were present clinically.

There is a bony fragment lying in relation to the medial side of the base of the proximal phalanx of the thumb.
Diagnosis: an avulsion fracture of the base of the proximal phalanx of the thumb where the medial collateral ligament is attached. This was associated clinically with instability in the metacarpophalangeal joint (gamekeeper’s thumb).