CHAPTER 6 The wrist
Study of the wrist cannot be separated from that of the hand, and in many cases careful examination of both may be required.
Complications Occurring After Colles’ Fracture
Considering the incidence of Colles’ fracture, the commonest of all fractures, it is surprising that complications from this injury are not seen more frequently; nevertheless, they do occur and are of importance. Excluding initial weakness of the wrist, the commonest complaints are of residual deformity, restriction of movements and pain.
The common deformities are radial deviation of the hand and prominence of the ulna. Owing to resorption of bone at the fracture site during healing, there is shortening of the radius with radial deviation of the hand. This may be aggravated by a poor reduction. At the back of the wrist, the head of the ulna becomes prominent. (Gross subluxations of the ulna of this pattern are sometimes referred to as Madelung’s deformity; this term was used initially to describe a condition occurring in adolescents where, following some disturbance of growth in the distal radial epiphysis, often idiopathic in origin, the ulna becomes relatively prominent.)
In all Colles’ fractures there is disturbance of the inferior radioulnar joint. In some cases this is responsible for persisting pain and tenderness just lateral to the ulnar styloid.
Again, disruption of the inferior radioulnar joint is partly responsible for loss of movements in the wrist. This certainly accounts for the loss of supination that causes patients the greatest concern. Although restriction of dorsiflexion occurs after most Colles’ fractures, this seldom gives rise to any functional problems.
Two other important complications are seen after Colles’ fracture: (a) delayed rupture of extensor pollicis longus tendon may occur some months after injury and is due to ischaemia or attrition of the tendon, and (b) Sudeck’s atrophy (complex regional pain syndrome), which is usually diagnosed some weeks after cast fixation has been discontinued, and which is characterised by marked swelling of the wrist, hand and fingers, gross stiffness of the fingers, and decalcification of the carpal bones which is obvious on radiographs of the region.
Regarding treatment of these complications, the patient is generally advised to accept minor degrees of residual deformity and stiffness. When there is gross prominence of the ulna causing symptoms, excision of the distal end of the bone may be advised. Ruptures of extensor pollicis longus are treated by tendon transfer (extensor indicis proprius is generally employed). Sudeck’s atrophy generally requires intensive physiotherapy, and often other measures if much permanent stiffness is to be avoided.
Ganglions
Ganglions are extremely common about the wrist and hand. In many cases they may have a tenuous communication with a carpal joint or tendon sheath. Some are spherical in shape, firm, and have no obvious connection to other structures. Tiny ganglions of this type are common in the fingers. Fluctuations in the size of ganglions and their rupture from trauma is well known, and diagnosis is not usually difficult unless the swelling is small. This applies in particular to small ganglions on the back of the wrist, arising from the radiocarpal joint; local swelling and tenderness may only be obvious when the wrist is palmarflexed. This type of ganglion is often the cause of persisting wrist pain in young women: their symptoms are often labelled as functional when this difficulty in examination has not been appreciated. Excision of most ganglions is advised, and this is essential if the ganglion is producing nerve complications (e.g. if a ganglion in the ulnar tunnel in the hand is producing ulnar motor and sensory loss).
De Quervain’s Disease
Tenosynovitis involving abductor pollicis longus and extensor pollicis brevis is known as de Quervain’s disease. It occurs in the middle-aged. The walls of the fibrous tendon sheaths on the lateral aspect of the radius are greatly thickened, and there is often marked underlying swelling. The patient complains of pain on certain movements of the wrist, and weakness of grip. Treatment is by splitting the lateral wall of the sheath.
Extensor Tenosynovitis
Acute frictional tenosynovitis occurs most frequently in the 20–40-year age group, generally following a period of excess activity. Any or all of the extensor tendons may be involved. The condition has a benign course and usually settles if the wrist is immobilised in a cast for 3 weeks.
Kienbock’s Disease
In this condition the lunate undergoes a form of avascular necrosis. The cause is unknown, but there is commonly a history of trauma. Abnormalities in the shape of the lunate and local osseous alignments have been described. The condition is seen most often in males in the 20–40-year age group, and gives rise to pain on the dorsum of the wrist and diminutions of grip strength. It may be complicated by an accompanying carpal tunnel syndrome. Although the diagnosis is usually established by plain radiographs, in the early stages an MRI scan may be helpful, and a CT scan may be used to detect early fracture or fragmentation, Temporary immobilisation of the wrist in a cast or other support may help relieve symptoms although not affecting the progress of the condition. A number of surgical procedures have been prescribed, none of which has any clear superiority over any of the others, or over conservative management.
Osteoarthritis of the Wrist
Osteoarthritis of the wrist is surprisingly uncommon considering the frequency with which the joint is involved in fractures. It is seen most often after avascular necrosis of the scaphoid following fracture of that bone, non-union of a scaphoid fracture, comminuted fractures involving the articular surface of the radius, and Kienbock’s disease (spontaneous avascular necrosis of the lunate, see above).
Where symptoms are severe, fusion of the wrist (radiocarpal joint) may be undertaken.
Rheumatoid Arthritis
Rheumatoid arthritis of the wrist is common, and extensive synovial thickening of the joint and related tendon sheaths leads to gross swelling, increased local heat, pain and stiffness. Fluctuation can sometimes be transmitted from just above the wrist to the palm, the synovial fluid being displaced from one level to the other underneath the flexor retinaculum (compound palmar ganglion). With progressive joint involvement the carpus tilts into ulnar deviation and subluxes in a palmar direction. The head of the ulna displaces dorsally, disrupting the inferior radioulnar joint and causing painful and reduced pronation and supination. Rarely tuberculosis of the wrist may produce a similar clinical picture, but the multifocal nature of rheumatoid arthritis usually makes differentiation easy.
As far as treatment is concerned, local measures can include the use of night splints; later, synovectomy of the wrist and of the inferior radioulnar joints may be effective in slowing the progress of the condition. Where pronation and supination are particularly affected, excision of the distal end of the ulna may give worthwhile functional improvement. Where there is gross destruction of the joint and marked local symptoms, fusion may have to be considered.
Carpal Tunnel Syndrome
This condition occurs most commonly in women in the 30–60-year age group. Basically there is compression of the median nerve, which leads to symptoms and signs related to its distribution. In some cases premenstrual fluid retention, early rheumatoid arthritis with synovial tendon sheath thickening, and old Colles’ or carpal fractures may be responsible by restricting the space left for the nerve in the carpal tunnel. The condition is sometimes seen in association with myxoedema, acromegaly and pregnancy; often, however, no obvious cause can be found, and it is very frequently bilateral. The patient complains of paraesthesia in the hand: often all the fingers are claimed to be involved, although theoretically at least the little finger should always be spared. Paraesthesia may also radiate proximally to the elbow. There may be pain in the same areas, and weakness in the hand. The symptoms may become most marked in the early hours of the morning, often waking the patient from sleep and causing her to shake the hand or hang it over the side of the bed. In many cases the history and results of the clinical examination are unequivocal. In others it may be difficult to differentiate the patient’s symptoms from those produced by cervical spondylosis, and indeed both conditions may be present at the same time; a trial period of immobilisation of the wrist in a cast or the use of a cervical collar may be helpful. Nerve conduction-time tests, showing a delay at the wrist, may be used to confirm the diagnosis. These studies are being employed with increasing frequency in the practice of defensive medicine.
Most cases are treated quite simply by division of the flexor retinaculum, which forms the roof of the carpal tunnel, thereby relieving pressure on the nerve; the procedure may be performed arthroscopically through a minimal incision. Conservative measures may be tried, especially in cases occurring in pregnancy, when diuretics may be prescribed with success. Other measures include the use of night splints and injections of hydrocortisone.
Note that on rare occasions the median nerve may be compressed proximal to the carpal tunnel. Above the elbow this may be due to a supracondylar bony spur (obvious on radiographs); just distal to the elbow, by the origin of pronator teres; and in the proximal part of the forearm by the sublimis. Proximal lesions of the median nerve give rise to the anterior interosseous nerve syndrome.
Ulnar Tunnel Syndrome
The ulnar nerve may be compressed as it passes through the ulnar carpal canal between the pisiform and the hook of the hamate. Both the sensory and the motor divisions of the nerve may be affected, but often one only is involved. The symptoms therefore may include small muscle wasting and weakness in the hand, with sensory disturbance on the volar aspect of the little finger. The sensory supply to the dorsum of the hand is given off in the distal forearm, so that sensory disturbance on the dorsum of the hand and little finger excludes a lesion at this level. In all cases every effort should be made to exclude a more proximal cause for the patient’s symptoms (e.g. ulnar neuritis at the elbow, and cervical spondylosis). Nerve conduction studies are often of particular value in this situation. The commonest causes of nerve involvement at the wrist are ganglionic compression, occupational trauma, ulnar artery disease, and old carpal or metacarpal fractures.
On the establishment of a firm diagnosis of a localised lesion in the ulnar tunnel, exploration and decompression of the nerve are carried out.
Ehlers–Danlos Syndrome
This is the name given to a number of closely related connective tissue disorders which are due to a collagen abnormality. The condition is comparatively rare (50 000 cases are said to be affected in the UK), with a strong (autosomal dominant) hereditary tendency. It is found in association with Marfan’s syndrome and osteogenesis imperfecta. The skin has a velvety feel and is fragile and hyperelastic; when grasped it can be raised and stretched by a remarkable amount. Wound healing is poor, leading to abnormal and somewhat keloid scarring, evidence of which may be widespread. Cases vary in severity, but in some healing may be so poor that surgery is contraindicated. The walls of blood vessels are affected, and bruising is a common problem. Ligaments lose their resistance to stretching, so that there is usually a striking increase in the range of movements in the affected joints; this is often well in excess of the normal range (sometimes to a grotesque degree), and there may be instability, leading to sprains and dislocations. There is no effective treatment.
Tuberculosis of the Wrist
Tuberculosis of the wrist is now rare in Britain. Marked swelling of the joint is followed by muscle wasting in the forearm, erosion, destruction and anterior subluxation of the carpus. The diagnosis is confirmed by synovial biopsy. Monoarticular rheumatism is the only other condition in this area that is likely to cause difficulty in diagnosis.
Carpal Instabilities
A carpal instability is a condition in which there is a loss of normal carpal alignment which develops at an early or a late stage after an injury. Untreated cases may lead to the development of osteoarthritis in the wrist.
In static carpal instabilities there is an abnormal carpal alignment, which can be seen by careful study of standard AP and lateral radiographs of the wrist.
In dynamic carpal instabilities routine radiographs are normal. The patient is usually able to toggle his carpal alignment from normal to abnormal and back. To establish the diagnosis in this situation, lead markers may be placed on the skin over points of local tenderness, and radiographs taken in both stable and unstable positions.
In the case of scapholunate instability (scapholunate dissociation), the commonest of these problems, AP views of the supinated wrist in both radial and ulnar deviation are usually diagnostic. Other investigations include examination of the wrist in motion using an image intensifier and radioisotope bone scans.
Acute cases may be stabilised by manipulative reduction and the insertion of K-wires, or by ligamentous repair. In chronic cases reattachment of the avulsed ligaments may be carried out, but where there are arthritic changes and subluxation a salvage procedure may have to be considered.
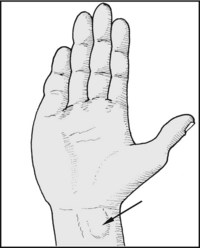
Note any deformity of the wrist, e.g. radial deviation of the hand, common after Colles’ fracture, and striking in congenital absence of the radius. Note any ulnar deviation, common in rheumatoid arthritis.
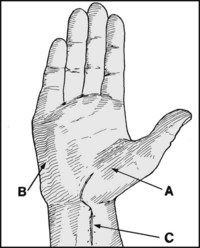
Note (A) thenar wasting in hand, (B) hypothenar wasting, (C) scars suggestive of previous surgery or injury.
If there is swelling at the wrist and also in the palm, try to demonstrate cross-fluctuation. This occurs in compound palmar ganglion, seen most often in rheumatoid arthritis and tuberculosis.
Note the presence of muscle wasting in the forearm, also suggestive of rheumatoid arthritis and tuberculosis. Widespread bilateral wasting is common in many neurological conditions (e.g. after cervical spine injuries, multiple sclerosis etc.) and in the muscular dystrophies.
Note any undue prominence of the ulna (common after Colles’ fracture or Madelung deformity), any anterior tilting of the plane of the wrist (e.g. after Smith’s fracture), backward tilting (post Colles’ fracture) or anterior subluxation (rheumatoid arthritis, old carpal injury or infective arthritis).

Swelling over the lateral aspect of the distal radius occurs in de Quervain’s tenosynovitis. If this is present, carry out additional tests (see Frame 6.34).

Palmarflex the wrist and compare one side with the other. Small ganglions between the radius and carpus are a common source of obscure wrist pain. Palmarflexion makes such ganglions obvious, and the presence of local tenderness should confirm the diagnosis.

Swelling of the wrist, hand and fingers, with a glazed appearance of the skin, diffuse tenderness, pain and stiffness is typical of Sudeck’s atrophy (complex regional pain syndrome), which may occur as a sequel to Colles’ fracture or carpal injury.

Pain in the wrist persisting after a Colles’ fracture, and due to disruption of the inferior radioulnar joint, is always associated with well localised tenderness at that site.

Tenderness in the anatomical snuffbox occurs classically after scaphoid fractures, but in fact is present after many wrist sprains and other minor injuries.

To help distinguish a sprain from fracture, also palpate the dorsal surface of the scaphoid. Tenderness here is usually present after fractures but not sprains. Scaphoid radiographs and plaster fixation are necessary in all cases of suspected fracture.

Diffuse tenderness is common in all inflammatory lesions (e.g. rheumatoid arthritis and tuberculosis of the wrist) and in Sudeck’s atrophy (complex regional pain syndrome).

Tenderness localised to the sheaths of abductor pollicis longus and extensor pollicis brevis is found in de Quervain’s tenosynovitis. There is often striking local thickening of the tendon sheaths over the dorsolateral aspect of the radius.

Tenderness over the median nerve, with the production of paraesthesia in the fingers and lateral side of the hand, is suggestive of the carpal tunnel syndrome. (See also Frame 6.36 et seq.)

In the same way, tenderness with paraesthesia on pressure over the ulnar nerve is suggestive of the ulnar tunnel syndrome.
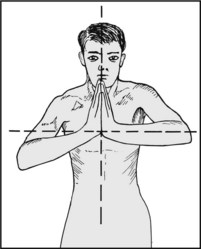
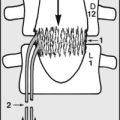
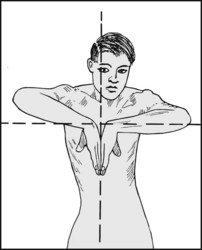
6.18. Movements: dorsiflexion (1):
Screening test: Ask the patient to press the hands together in the vertical plane and to raise the elbows to the horizontal. Loss of any dorsiflexion should be obvious. The commonest cause is stiffness after a Colles’ fracture.
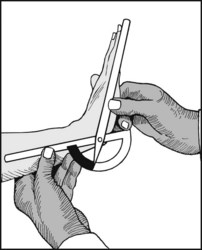
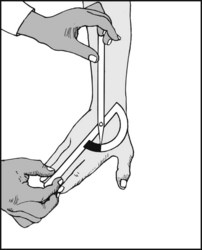
Dorsiflexion may be measured with a goniometer.
Hypermobility is not uncommon in women. If hypermobility is gross, however, other joints should be examined to exclude a joint laxity syndrome.
Screening test: Ask the patient to put the backs of the hands in contact, and then to bring the forearms into the horizontal plane. Loss of palmarflexion should be obvious.
Palmarflexion may be measured with a goniometer.
Normal range = 75°. If the range exceeds this, look for other signs of wrist (and other joint) hypermobility, as described in the following frames.
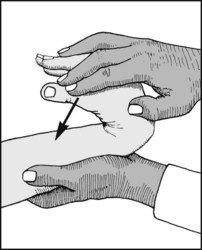
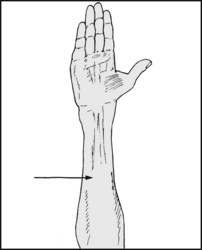
6.22. Joint hypermobility (1):
(1) Try to bring the thumb into contact with the forearm and measure any gap. The average separation is 4.5 cm at age  and it increases with age (as the ligaments lose some of their elasticity). Although the thumb contacting the forearm suggests hypermobility, this is nevertheless said to occur in 56% of normal subjects.
and it increases with age (as the ligaments lose some of their elasticity). Although the thumb contacting the forearm suggests hypermobility, this is nevertheless said to occur in 56% of normal subjects.
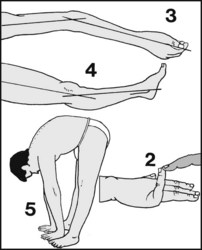
6.23. Joint hypermobility (2):
(2) Test whether the little finger can be passively dorsiflexed to 90° or more. (3) Check the elbow and (4) the knee to see if they can hyperextend by 10° or more. (5) Check if the spine can be flexed so that the palms of the hands can be placed on the floor. Joint laxity is diagnosed if any three of these tests (1–5) are positive.

6.24. Joint hypermobility (3):
Other evidence of hypermobility includes (6) hyperextension of the ankle beyond 45°; (7) an abnormal range of abduction of the little finger; (8) an increase in hip rotation in children (from 90–93° to about 110°), with the centre of the range displaced lateral to the midline. Joint hypermobility is a feature of the Ehlers–Danlos syndrome, Marfan’s disease, osteogenesis imperfecta and Morquio–Brailsford’s disease.

Radial deviation is measured as the angle formed between the forearm and the middle metacarpal. This test is best carried out in the mid position of the pronation/supination range.

Screening test: Ask the patient to hold the elbows firmly at the sides. Grasp the hands and turn them so that the palms are uppermost. Compare the amount of supination in both sides.

Screening test (2): Repeat, turning the palms downward to assess pronation. If no obvious cause for loss of pronation or supination is found at the wrist then the forearm and elbow must be carefully examined.
For accurate measurement, give the patient a pen to hold. Ask the patient to keep the elbows firmly at the sides and to pronate the wrist. Measure the angle between the vertical and the held pen.
Supination may be measured in the same way.
Where pronation and supination have been found to be affected, be sure to examine the elbow, and if necessary assess the curvature of the radius (see Frame 5.42).

6.31. Crepitus (1): radioulnar joint:
Place the index and thumb over the joint and pronate and supinate the wrist. Crepitus is common when the joint is disorganised, especially after a Colles’ fracture.

6.32. Crepitus (2): radiocarpal joint:
Encircle the wrist with the hand and ask the patient to dorsiflex, palmarflex, radial deviate and ulnar deviate the wrist. Osteoarthritis of the wrist is uncommon, but occurs after scaphoid and distal radius fractures, Kienbock’s disease etc.

While grasping the wrist, flex and extend the fingers. Ask the patient to repeat these movements on his own. Crepitus, fine in character, occurs in tenosynovitis of the extensor tendons. Auscultation over the tendons may reveal characteristic grating sounds.
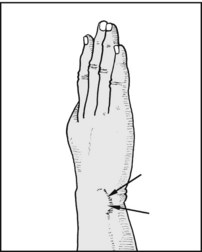
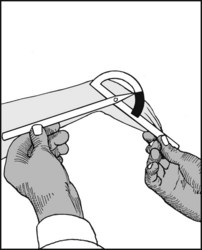
6.34. de Quervain’s tenosynovitis (of abductor pollicis longus and extensor pollicis brevis).
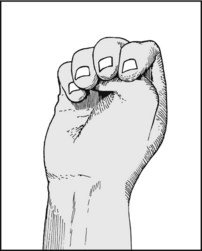
Where this is suspected from the history, local swelling and tenderness, confirm the diagnosis with the following test. Ask the patient to flex the thumb and close the fingers over it.

6.35. de Quervain’s tenosynovitis:
Now move the hand into ulnar deviation. In de Quervain’s tenosynovitis excruciating pain accompanies this manoeuvre.

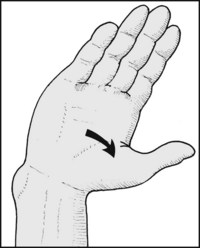
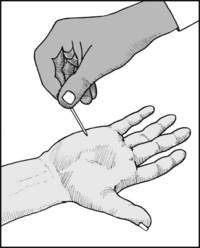
6.36. Carpal tunnel syndrome (1):
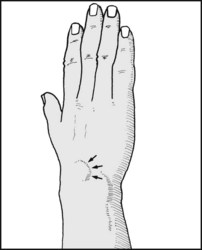
Where this is suspected, apply very firm, steady pressure with both thumbs for 30 seconds over the median nerve as it runs within the carpal tunnel. Note the interval between the application of pressure and the onset of numbness, pain or paraesthesia in the median distribution (average 16 seconds in carpal tunnel syndrome). This is the most reliable test for carpal tunnel syndrome.

6.37. Carpal tunnel syndrome (2):
Phalen test: Ask the patient to hold both wrists in a fully flexed position for 1–2 minutes. The appearance or exacerbation of paraesthesia in the median distribution is suggestive of the carpal tunnel syndrome, and is positive in 70% of those suffering from this condition.

6.38. Carpal tunnel syndrome (3):
Tinel’s sign: the test is positive if gentle finger percussion over the median nerve produces paraesthesia in its distribution. This test is said to be positive in 56% of cases of carpal tunnel syndrome.

6.39. Carpal tunnel syndrome (4):
Note any pain and paraesthesia on stretching the nerve by the manoeuvre of extending the elbow and dorsiflexing the wrist.

6.40. Carpal tunnel syndrome (5):
Test the motor division of the median nerve. Note the resistance offered by the patient as you try to push the vertically held thumb into the plane of the palm. Feel the tone in the thenar muscles.

6.42. Carpal tunnel syndrome (7):
Slide the tip of the index finger across the palm, noting frictional resistance and temperature. Increased thenar resistance (from lack of sweating) and temperature rise (vasodilatation) may occur with median nerve involvement.
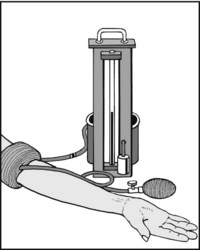
6.43. Carpal tunnel syndrome (8):
Apply a tourniquet and inflate it to just above the systolic blood pressure; maintain this for 1–2 minutes. The appearance or exacerbation of symptoms again suggests the carpal tunnel syndrome. This test, however, should be interpreted with caution.

6.44. Carpal tunnel syndrome (9):
If there is still doubt, apply a scaphoid plaster for 7–10 days. Improvement of symptoms while in plaster, and deterioration on removal, is suggestive of the carpal tunnel syndrome. Nerve conduction studies that show impairment of conduction at the level of the tunnel are virtually diagnostic, and are used by many to counter the chances of future litigation.

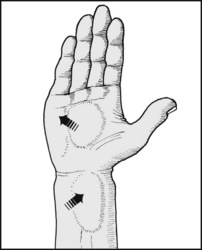
6.45. Ulnar tunnel syndrome (1):
Look for tenderness over the tunnel, and for signs of ulnar nerve involvement (hypothenar wasting, abduction of the little finger, early clawing of the ring and middle fingers).

6.46. Ulnar tunnel syndrome (2):
Test for involvement of the motor distribution of the nerve. The power of adduction of the little finger is a useful screening test. Note that weakness of adduction, but with normal power of abduction, is one early sign of cervical spinal myelopathy.
6.47. Ulnar tunnel syndrome (3):
Test for sensory impairment in the common area of sensory distribution of the nerve.

6.48. Distal radioulnar joint laxity:
Test for laxity in the joint; its presence may be associated with weakness of the wrist, clicking sensations and ulnar nerve involvement. Steady the carpus with one hand and use the other to hold the distal ulna and attempt to move it in a dorsal and then a volar direction, noting any clicking sensations or complaint of pain. Compare the sides.

6.49. Carpal instabilities (1):
Scapholunate instability: Watson’s test: press the thumb against the tubercle of the scaphoid, and with the other hand palmarflex and radially deviate the patient’s wrist. A click should be felt if the scaphoid subluxes over the distal radius, and reduction should occur if the pressure of the thumb is slackened. Accompanying pain is confirmatory.

6.50. Carpal instabilities (2):
Lunotriquetral instability: Ballottement test: the triquetral and lunate respectively are grasped between the thumb and index of each of the examiner’s hands, and an attempt made to displace them relative to one another, first in a dorsal and then in a volar direction. Note any associated and confirmatory pain or crepitus.

6.51. Carpal instabilities (3):
Midcarpal instability: with one hand steadying the distal forearm and the other grasping the patient’s hand, push the carpus against the radius and gently swing the wrist from a position of full ulnar deviation to full radial deviation. The test is positive if this normal smooth movement is irregular, with for example an accompanying clunking sensation.
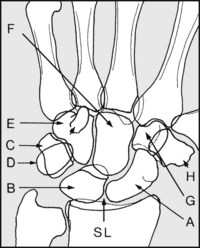
Landmarks: In the anteroposterior, identify the carpal bones and note their shape, density and position: (A) scaphoid, (B) lunate, (C) triquetral, (D) pisiform, (E) hamate with hook, (F) capitate, (G) trapezoid, (H) trapezium. Note the gaps between the various carpal bones, particularly between the scaphoid and lunate (SL), and whether these are diminished or excessive.
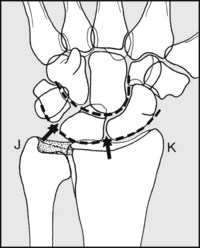
Note the smooth curves formed by the proximal and distal rows of the carpus, and that the distal end of the ulna stops short of the radius to make room for the triangular fibrocartilage. If there is any widening of the gaps between the scaphoid and lunate, or the lunate and triquetral, or any suggestion of carpal instability, obtain additional views in full radial and ulnar deviation. (J) Ulnar styloid, (K) radial styloid.
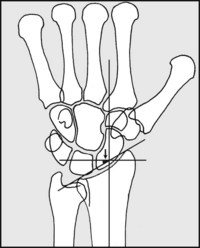
Note the radial inclination: this is the angle between the distal articular surface of the radius and the radial shaft. It is often decreased after a Colles’ fracture. For critical assessment it may be measured on the radiographs.
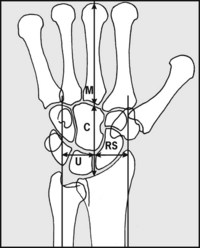
A line drawn through the middle metacarpal (M) and carpus (C), and its distance from the radial styloid (RS) and ulnar axis (U), may be very occasionally used to assess carpal height and drift, expressing these as ratios. Carpal height ratio = C/M (normal = 0.51–0.57); Chamay measurement = RS/M (normal = 0.25–0.31); McMurtry’s index = U/M (normal = 0.27–0.33).
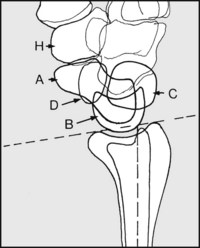
It is usually possible to make out in the lateral the following, in spite of the superimposition of the bony structures: (H) trapezium; (A) tubercle and body of the scaphoid; (D) pisiform; (B) crescent of lunate; (C) triquetral. Note that the plane of the wrist joint has normally a 5° anterior tilt.
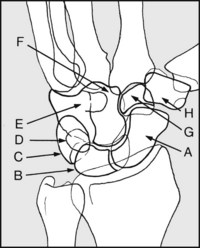
When the carpus is suspect, at least one (but preferably two) oblique views should be taken in addition to the routine anteroposterior and lateral. These are of particular value in detecting hairline crack fractures of the carpal bones. (The labelling is the same as in previous diagrams.)
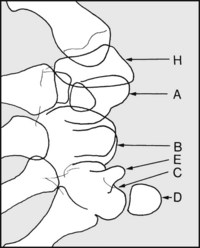
In suspected carpal tunnel syndrome a tangential projection of the tunnel should be obtained. This view occasionally shows osteoarthritic lipping or other causal pathology. (A) Scaphoid, (B) innate, (C) triquetral, (D) pisiform, (E) hook of hamate, (H) trapezium.
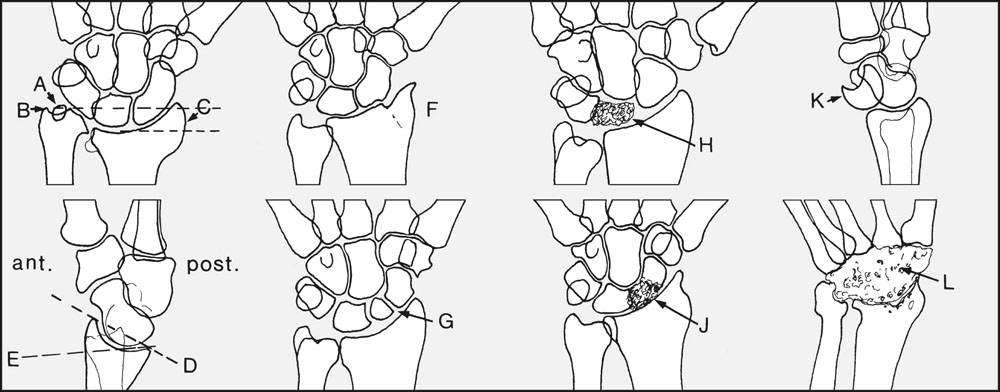
Look for evidence of previous injury. In the malunited Colles’ fracture there may be (A) non-union of the ulnar styloid; (B) prominence of the distal ulna secondary to (C) distortion and resorption at the radial fracture, with disturbance of the radial inclination. In the lateral the joint line (D) may also be tilted away from (E) the normal. Osteoarthritic changes are uncommon after Colles’ fracture, but are seen after (F) radial styloid fractures. Osteoarthritis may not always follow (G) non-union of a scaphoid fracture, but is nevertheless common. Note increased bone density and deformity in (H) Kienbock’s disease of the lunate or in (J) avascular necrosis of the scaphoid, both of which are almost invariably accompanied by osteoarthritis. Note any carpal malalignment, such as dislocation of the lunate (K), which is the most common. Gross porotic changes are seen most frequently in rheumatoid arthritis and in Sudeck’s atrophy (complex regional pain syndrome), whereas gross destructive changes are a feature of (L) tuberculosis and other infections.
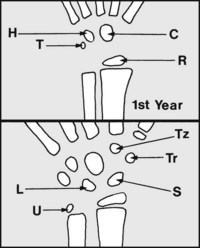
In the first year of life the ossification centres for the capitate (C) and hamate (H) appear at 2 months, the radius (R) at 6 months, and the triquetral (T) at 10 months. After the first year, the lunate (L) appears at about 2, the trapezium (Tr) at  , the trapezoid (Tz) and scaphoid (S) at 3, and the distal ulna (U) at
, the trapezoid (Tz) and scaphoid (S) at 3, and the distal ulna (U) at  years.
years.

6.63. Wrist radiographs: examples of pathology (1):
the radiograph shows a deformity of the upper limb in which there is absence of the radius and thumb, along with failure of carpal differentiation.

The radiographs show an upper and lower limb where the width of the bones is normal but they are proportionately short, contributing to the dwarfism associated with this hereditary abnormally. The metaphyses are wide, and there is defective modelling of the shafts.

In this radiograph of a child’s forearm there is a little metaphyseal widening and irregularity, with ulnar metaphyseal cupping (said to be due to pressure transmitted in crawling).

There are deformities of the distal radius and ulna, which are splayed. There is relative lengthening of the ulna, which is unduly prominent at the side and back of the wrist.

The history is of weakness and instability of the wrist, with clicking sensations and pain occurring with certain movements.
Diagnosis: carpal instability secondary to scapholunate dissociation.

The radiograph shows a defect in the continuity of the scaphoid, with increased density of its proximal pole.
Diagnosis: there has been a fracture of the scaphoid, followed by non-union and avascular necrosis.

The radiograph shows a long-established defect situated in the waist of the scaphoid. There is some narrowing of the joint space between the scaphoid and the radius.
Diagnosis: established non-union of the scaphoid following fracture, with early secondary radiocarpal osteoarthritis.

There is gross destruction of the carpal and wrist joints, with fibrous ankylosis.
Diagnosis: the findings are typical of the late appearances of an infective arthritis (in this case due to tuberculosis).

The radiograph was taken shortly after a fall on the outstretched hand, when there was complaint of pain in the wrist and paraesthesia over the ball of the thumb.
Diagnosis: the lateral projection shows two bones lying proud of the rest of the carpus at the front of the wrist: one is the normally situated pisiform; the other, semilunar in shape and lying more proximal, is a dislocated lunate. The symptoms suggest involvement of the median nerve.

The radiograph shows an abnormality of the distal radius. There is rounding of the proximal part of the small bone fragment in the region of the styloid process.
Diagnosis: fracture of the styloid process of the radius, which has failed to unite. The appearances are of a long-standing lesion. Such a condition may be symptom free, or give pain if secondary arthritic changes develop between the radius and scaphoid.

This radiograph of a child’s wrist and forearm shows gross distortion of the distal radius. There are apparently cystic spaces in the radial shaft, with extensive new bone formation.
Diagnosis: the appearances are typical of gross osteitis, with bone abscess formation. In this case the causal organism was, unusually, the tubercle bacillus. (NB: Most tuberculous infections have their principal effects on the joints, rather than the shafts of the long bones.)

There is widespread decalcification of the carpus and adjacent long bones, with loss of radiological carpal detail. There was complaint of pain and stiffness following a minor injury.
Diagnosis: Sudeck’s atrophy (complex regional pain syndrome). The radiological appearances are similar to those found in rheumatoid arthritis.

This anteroposterior radiograph shows distortion of the inferior radioulnar joint, relative lengthening and prominence of the ulna, and widening of the radius. The patient complained of pain in the wrist (in the radioulnar joint) and restriction of pronation/supination movements.

The lateral radiograph of the same case shows marked alteration in the plane of the radiocarpal joint, again due to malunion; this, apart from the deformed appearance, has the effect of seriously restricting palmar flexion.
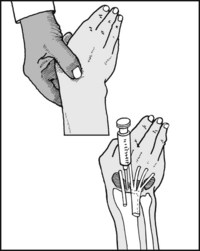
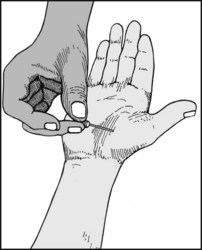
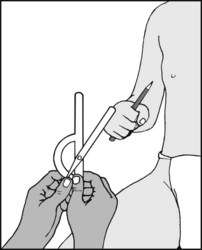
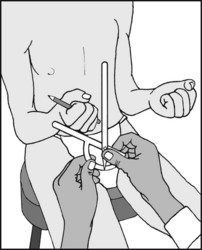
6.78. Aspiration of the wrist joint:
Using your thumb, feel for the depression at the back of the wrist which lies between the distal end of the radius and scaphoid, and which is bordered by extensor digitorum communis and extensor carpi radialis brevis. Infiltrate this area with local anaesthetic before introducing the aspirating needle. The tip of the needle should be directed cranially at an angle of 30° from the vertical.