Chapter 15 Gastroenterology
Antacids: Buffers
Pharmacokinetics
 Calcium, magnesium, and aluminum are typically poorly absorbed. However, patients with impaired renal function can have accumulation of these cations.
Calcium, magnesium, and aluminum are typically poorly absorbed. However, patients with impaired renal function can have accumulation of these cations.Side Effects
Ca2+-Containing Buffers
 Hypercalcemia (at high doses): These agents may lead to formation of calculi (milk alkali syndrome). Calculi are solid formations, typically consisting of minerals, which precipitate in organs such as the kidney and obstruct ducts.
Hypercalcemia (at high doses): These agents may lead to formation of calculi (milk alkali syndrome). Calculi are solid formations, typically consisting of minerals, which precipitate in organs such as the kidney and obstruct ducts.Important Notes
 Although these agents act locally in the stomach, they are not devoid of systemic adverse effects, particularly at higher doses or with chronic use.
Although these agents act locally in the stomach, they are not devoid of systemic adverse effects, particularly at higher doses or with chronic use. As with other antacids, buffers may reduce pH enough to interfere with absorption of drugs that require a low pH for absorption.
As with other antacids, buffers may reduce pH enough to interfere with absorption of drugs that require a low pH for absorption. Al3+ and Mg2+ are often combined into one antacid formulation because of their complementary onset of action (Mg2+ is rapid, Al3+ is slow reacting) and side effects (Mg2+ causes diarrhea, Al3+ constipation).
Al3+ and Mg2+ are often combined into one antacid formulation because of their complementary onset of action (Mg2+ is rapid, Al3+ is slow reacting) and side effects (Mg2+ causes diarrhea, Al3+ constipation). Simethicone is a surfactant added to antacids to decrease bloating. A surfactant is a substance that reduces surface tension, in this case reducing large bubbles into smaller ones. The foaming action of simethicone may also alleviate gastroesophageal reflux.
Simethicone is a surfactant added to antacids to decrease bloating. A surfactant is a substance that reduces surface tension, in this case reducing large bubbles into smaller ones. The foaming action of simethicone may also alleviate gastroesophageal reflux.FYI
 Although the agents in this class have traditionally been referred to as antacids, the term antacid has much wider use and applies to each of the many classes of drugs that reduce acid secretion. The more appropriate term for the agents in this class is buffer, as this describes their mechanism and distinguishes them from other classes.
Although the agents in this class have traditionally been referred to as antacids, the term antacid has much wider use and applies to each of the many classes of drugs that reduce acid secretion. The more appropriate term for the agents in this class is buffer, as this describes their mechanism and distinguishes them from other classes.H2 Antagonists
Moa (Mechanism of Action)
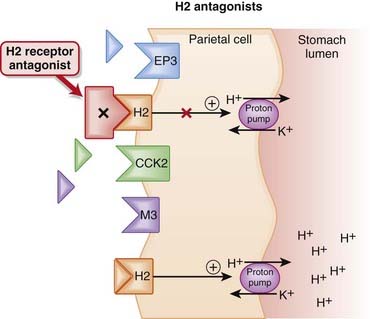
 The amount of gastric acid is largely determined by the secretion of protons (H+) by parietal cells in the stomach, as well as volume of stomach contents.
The amount of gastric acid is largely determined by the secretion of protons (H+) by parietal cells in the stomach, as well as volume of stomach contents. In the parietal cell, the proton pump, H+/K+ ATPase, creates an ion gradient by pumping H+ into the lumen of the stomach. The pump is key to creating the acidic environment of the stomach (pH <1) while maintaining a relatively normal intracellular pH (approximately 7.3).
In the parietal cell, the proton pump, H+/K+ ATPase, creates an ion gradient by pumping H+ into the lumen of the stomach. The pump is key to creating the acidic environment of the stomach (pH <1) while maintaining a relatively normal intracellular pH (approximately 7.3). The H2 receptor on parietal cells mediates both the basal and meal-stimulated release of acid. The binding of histamine to the H2 receptor stimulates the proton (H+/K+ ATPase) pump via the second messenger cyclic adenosine monophosphate (cAMP) (Figure 15-1).
The H2 receptor on parietal cells mediates both the basal and meal-stimulated release of acid. The binding of histamine to the H2 receptor stimulates the proton (H+/K+ ATPase) pump via the second messenger cyclic adenosine monophosphate (cAMP) (Figure 15-1). H2 antagonists competitively block the interaction of histamine with H2 receptors, thus reducing stimulation of the proton pump through this receptor.
H2 antagonists competitively block the interaction of histamine with H2 receptors, thus reducing stimulation of the proton pump through this receptor. Nocturnal acid secretion depends largely on histamine; thus the H2 antagonists have a greater impact on nocturnal acid secretion than meal-stimulated acid secretion, which is stimulated by gastrin and acetylcholine (ACh), in addition to histamine.
Nocturnal acid secretion depends largely on histamine; thus the H2 antagonists have a greater impact on nocturnal acid secretion than meal-stimulated acid secretion, which is stimulated by gastrin and acetylcholine (ACh), in addition to histamine. An additional mechanism, by which H2 antagonists are also able to attenuate the gastrin and ACh-stimulated release of gastric acid, has been proposed by some sources. ACh, by binding to muscarinic (M3) receptors, and gastrin, by binding to cholecystokinin (CCK2) receptors, also stimulate the proton pump.
An additional mechanism, by which H2 antagonists are also able to attenuate the gastrin and ACh-stimulated release of gastric acid, has been proposed by some sources. ACh, by binding to muscarinic (M3) receptors, and gastrin, by binding to cholecystokinin (CCK2) receptors, also stimulate the proton pump.Pharmacokinetics
Side Effects
 Rare central nervous system (CNS) side effects: Confusion, delirium, hallucinations, slurred speech, and headache can occur and are thought to be caused by antagonism of H2 receptors in the CNS. These CNS effects are more likely to occur with intravenous administration or in the elderly.
Rare central nervous system (CNS) side effects: Confusion, delirium, hallucinations, slurred speech, and headache can occur and are thought to be caused by antagonism of H2 receptors in the CNS. These CNS effects are more likely to occur with intravenous administration or in the elderly.Important Notes
 The H2 antagonists are considered to be less effective than the more expensive proton pump inhibitors (PPIs). However, it is important to note that the H2 antagonists are able to reduce daily acid secretion by about 60% to 70%.
The H2 antagonists are considered to be less effective than the more expensive proton pump inhibitors (PPIs). However, it is important to note that the H2 antagonists are able to reduce daily acid secretion by about 60% to 70%. Tolerance can develop to the acid-suppressant effects of the H2 antagonists, occurring as early as 3 days after initiation of therapy. One theory is that secondary hypergastrinemia may stimulate histamine release from enterochromaffin-like cells. Hypergastrinemia is an elevation in gastrin levels in the blood in response to low pH in the stomach. Gastrin stimulates the proton pump to release acid into the stomach.
Tolerance can develop to the acid-suppressant effects of the H2 antagonists, occurring as early as 3 days after initiation of therapy. One theory is that secondary hypergastrinemia may stimulate histamine release from enterochromaffin-like cells. Hypergastrinemia is an elevation in gastrin levels in the blood in response to low pH in the stomach. Gastrin stimulates the proton pump to release acid into the stomach.Evidence
Versus Other Agents for Endoscopy Negative Reflux Disease
 The same 2006 Cochrane review found that PPIs were more efficacious at achieving heartburn remission compared with H2 antagonists (three trials, RR 0.78) and compared with prokinetics (one trial, RR 0.72). Endoscopy-negative reflux disease is simply GERD without any evidence of histologic changes on endoscopic examination.
The same 2006 Cochrane review found that PPIs were more efficacious at achieving heartburn remission compared with H2 antagonists (three trials, RR 0.78) and compared with prokinetics (one trial, RR 0.72). Endoscopy-negative reflux disease is simply GERD without any evidence of histologic changes on endoscopic examination.Proton Pump Inhibitors (PPIs)
Moa (Mechanism of Action)
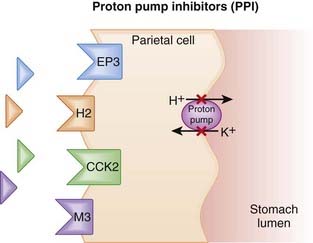
 The amount of gastric acid is largely determined by the secretion of protons (H+) by parietal cells in the stomach, as well as the volume of stomach contents.
The amount of gastric acid is largely determined by the secretion of protons (H+) by parietal cells in the stomach, as well as the volume of stomach contents. In the parietal cell, the proton pump, H+/K+ ATPase, creates an ion gradient by pumping H+ into the lumen of the stomach. The pump is key to creating the acidic environment of the stomach (pH <1) while maintaining a relatively normal intracellular pH (approximately 7.3) (Figure 15-2).
In the parietal cell, the proton pump, H+/K+ ATPase, creates an ion gradient by pumping H+ into the lumen of the stomach. The pump is key to creating the acidic environment of the stomach (pH <1) while maintaining a relatively normal intracellular pH (approximately 7.3) (Figure 15-2). PPIs enter the parietal cell and bind to the proton pump, resulting in an irreversible inactivation of the pump. This dramatically reduces the amount of H+ that is pumped into the lumen of the stomach, and because the binding is irreversible, the effects of PPIs persist until new pumps are synthesized. The reduction in gastric acid secretion can thus persist up to 48 hours after a single dose.
PPIs enter the parietal cell and bind to the proton pump, resulting in an irreversible inactivation of the pump. This dramatically reduces the amount of H+ that is pumped into the lumen of the stomach, and because the binding is irreversible, the effects of PPIs persist until new pumps are synthesized. The reduction in gastric acid secretion can thus persist up to 48 hours after a single dose. The PPIs tend to be particularly adept at reducing acid secretion because the proton pump is the final and key step in secreting acid (H+) into the lumen of the stomach. All other agents that suppress acid secretion work by reducing gastric H+ concentration act upstream of the proton pump, rather than directly at the proton pump.
The PPIs tend to be particularly adept at reducing acid secretion because the proton pump is the final and key step in secreting acid (H+) into the lumen of the stomach. All other agents that suppress acid secretion work by reducing gastric H+ concentration act upstream of the proton pump, rather than directly at the proton pump.Pharmacokinetics
 Although they act on cells in the stomach, PPIs must be absorbed into the systemic circulation from the small intestine. It is from the systemic circulation that they reach the parietal cells of the stomach.
Although they act on cells in the stomach, PPIs must be absorbed into the systemic circulation from the small intestine. It is from the systemic circulation that they reach the parietal cells of the stomach. This is important because the PPIs (ironically) tend to be unstable in an acidic environment. Hence all PPIs have some form of enteric coating, to protect them until they reach the small intestine and can be absorbed. Disruption of this enteric coating (e.g., by splitting the tablet) will likely reduce the bioavailability of the PPI.
This is important because the PPIs (ironically) tend to be unstable in an acidic environment. Hence all PPIs have some form of enteric coating, to protect them until they reach the small intestine and can be absorbed. Disruption of this enteric coating (e.g., by splitting the tablet) will likely reduce the bioavailability of the PPI. All PPIs are prodrugs that are activated in the acidic environment of the parietal cell acid canaliculi. Food intake stimulates acid secretion. Oral PPIs should be taken approximately 30 to 60 minutes before meals. This allows enough time for the PPI to be absorbed into the systemic circulation and to be distributed to the parietal cells. This will also ensure that the PPIs are active at the same time as maximal activation of the proton pumps.
All PPIs are prodrugs that are activated in the acidic environment of the parietal cell acid canaliculi. Food intake stimulates acid secretion. Oral PPIs should be taken approximately 30 to 60 minutes before meals. This allows enough time for the PPI to be absorbed into the systemic circulation and to be distributed to the parietal cells. This will also ensure that the PPIs are active at the same time as maximal activation of the proton pumps.Side Effects
Less Common
 Hypergastrinemia: Gastrin levels become elevated because of the body’s response to chronic gastric acid suppression. This may lead to rebound hypersecretion of gastric acid if the PPI is stopped. There is also concern over the chronic effects of hypergastrinemia, including development of gastric tumors.
Hypergastrinemia: Gastrin levels become elevated because of the body’s response to chronic gastric acid suppression. This may lead to rebound hypersecretion of gastric acid if the PPI is stopped. There is also concern over the chronic effects of hypergastrinemia, including development of gastric tumors.Important Notes
 Of all agents used to treat hyperacidity, PPIs are the most effective at reducing daily acid secretion, capable of reducing acid (basal and stimulated) by 80% to 95%. H2 antagonists are able to achieve a 60% to 70% reduction in acid.
Of all agents used to treat hyperacidity, PPIs are the most effective at reducing daily acid secretion, capable of reducing acid (basal and stimulated) by 80% to 95%. H2 antagonists are able to achieve a 60% to 70% reduction in acid. PPIs inhibit only active proton pumps. Not all proton pumps are active at the same time; therefore, although pumps are irreversibly inhibited once bound by the PPI, it takes a few days to achieve the inhibition of proton pumps seen at steady state.
PPIs inhibit only active proton pumps. Not all proton pumps are active at the same time; therefore, although pumps are irreversibly inhibited once bound by the PPI, it takes a few days to achieve the inhibition of proton pumps seen at steady state. PPIs are often prescribed in combination with other GI drugs and antibiotics for eradication of H. pylori. By increasing intragastric pH, PPIs appear to enhance the antimicrobial activity of these agents. PPIs may also have a minor antimicrobial effect. Some of the more common combinations are listed in Table 15-1.
PPIs are often prescribed in combination with other GI drugs and antibiotics for eradication of H. pylori. By increasing intragastric pH, PPIs appear to enhance the antimicrobial activity of these agents. PPIs may also have a minor antimicrobial effect. Some of the more common combinations are listed in Table 15-1.| Proton Pump Inhibitors | Other Agents | |
|---|---|---|
| Lansoprazole | Clarithromycin | Amoxicillin |
| Omeprazole | Clarithromycin | Metronidazole |
| Pantoprazole | Metronidazole | |
| Rabeprazole | Bismuth subsalicylate | Tetracycline |
Evidence
Versus Other Agents for Endoscopy Negative Reflux Disease
 The same 2006 Cochrane review found that PPIs were more efficacious at achieving heartburn remission compared with H2 antagonists (three trials, RR 0.78) and compared with prokinetics (one trial, RR 0.72). Endoscopy-negative reflux disease is simply GERD without any evidence of histologic changes on endoscopic examination.
The same 2006 Cochrane review found that PPIs were more efficacious at achieving heartburn remission compared with H2 antagonists (three trials, RR 0.78) and compared with prokinetics (one trial, RR 0.72). Endoscopy-negative reflux disease is simply GERD without any evidence of histologic changes on endoscopic examination.Versus H2 Antagonists for Acute Bleeding from Peptic Ulcer
 A 2006 Cochrane review (24 studies, N = 4373 patients) found no difference in mortality between PPIs and controls but did find that PPIs reduced rebleeding (incidence of 10.6% for PPI versus 17.3% control) and surgery (6.1% versus 9.3%, respectively) versus control. No benefit was seen for PPIs versus H2 antagonists with regard to surgery.
A 2006 Cochrane review (24 studies, N = 4373 patients) found no difference in mortality between PPIs and controls but did find that PPIs reduced rebleeding (incidence of 10.6% for PPI versus 17.3% control) and surgery (6.1% versus 9.3%, respectively) versus control. No benefit was seen for PPIs versus H2 antagonists with regard to surgery.Gastrointestinal Cytoprotectants
Moa (Mechanism of Action)
Prostaglandin Analogue
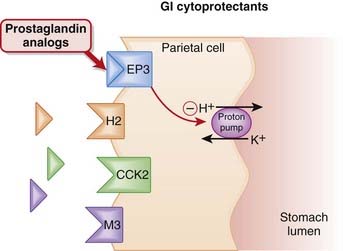
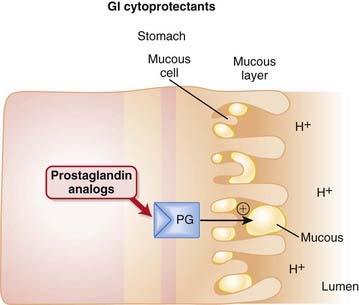
 Protection of the mucosal lining of the stomach can be achieved in two ways: by increasing gastric pH or by enhancing the mucosal barrier that protects the stomach.
Protection of the mucosal lining of the stomach can be achieved in two ways: by increasing gastric pH or by enhancing the mucosal barrier that protects the stomach. The prostaglandin E receptor 3 (EP3) receptors are found on parietal cells of the stomach and, when stimulated, have an inhibitory effect on the proton pump. The proton pump stimulates the release of hydrogen ions (acid) into the lumen of the stomach.
The prostaglandin E receptor 3 (EP3) receptors are found on parietal cells of the stomach and, when stimulated, have an inhibitory effect on the proton pump. The proton pump stimulates the release of hydrogen ions (acid) into the lumen of the stomach. Endogenous PGE2 acts as an agonist at EP3 receptors on parietal cells and reduces activity of the proton pump, thereby reducing secretion of gastric acid (Figure 15-3).
Endogenous PGE2 acts as an agonist at EP3 receptors on parietal cells and reduces activity of the proton pump, thereby reducing secretion of gastric acid (Figure 15-3). PGE2 also contributes to maintenance of the mucosal barrier, stimulating secretion of mucin and bicarbonate and enhancing mucosal blood flow. Mucin is a thick substance that has a protective effect on the lining of the stomach. Bicarbonate helps to raise the pH of the stomach, particularly in the area close to the mucosal lining.
PGE2 also contributes to maintenance of the mucosal barrier, stimulating secretion of mucin and bicarbonate and enhancing mucosal blood flow. Mucin is a thick substance that has a protective effect on the lining of the stomach. Bicarbonate helps to raise the pH of the stomach, particularly in the area close to the mucosal lining. NSAIDs work by inhibiting COX enzymes, thus reducing the amount of PGE2 and subsequently reducing the amount of protective mucus in the stomach. Nonselective (i.e., COX-1 and COX-2) inhibitors are thus implicated in damage to the gastric mucosa.
NSAIDs work by inhibiting COX enzymes, thus reducing the amount of PGE2 and subsequently reducing the amount of protective mucus in the stomach. Nonselective (i.e., COX-1 and COX-2) inhibitors are thus implicated in damage to the gastric mucosa.Sucralfate
 Sucralfate is a complex of sucrose and aluminum hydroxide that forms a viscous paste in aqueous acidic media. This negatively charged paste binds to positively charged proteins in the ulcer, forming a direct protective barrier for up to 6 hours.
Sucralfate is a complex of sucrose and aluminum hydroxide that forms a viscous paste in aqueous acidic media. This negatively charged paste binds to positively charged proteins in the ulcer, forming a direct protective barrier for up to 6 hours.Pharmacokinetics
 Sucralfate primarily acts locally in the GI tract, is only minimally absorbed, and is excreted mainly in the feces. It also must be administered 4 times daily. Sucralfate should be administered 1 hour before meals, as it is activated by acid.
Sucralfate primarily acts locally in the GI tract, is only minimally absorbed, and is excreted mainly in the feces. It also must be administered 4 times daily. Sucralfate should be administered 1 hour before meals, as it is activated by acid. Every tablet of sucralfate contains aluminum. Although only a very small proportion of aluminum is absorbed, because elimination relies on urinary excretion, caution should be exercised in those with chronic renal failure, as an accumulation of aluminum may occur. This is particularly important if these patients are also receiving aluminum in another form, such as an antacid.
Every tablet of sucralfate contains aluminum. Although only a very small proportion of aluminum is absorbed, because elimination relies on urinary excretion, caution should be exercised in those with chronic renal failure, as an accumulation of aluminum may occur. This is particularly important if these patients are also receiving aluminum in another form, such as an antacid.Indications
Contraindications
Bismuth Subsalicylate
 Similar to acetylsalicylic acid (ASA), bismuth subsalicylate may be associated with a higher risk of Reye’s syndrome in children; therefore it should be avoided in children or teenagers with viral infections such as influenza or chickenpox. Reye’s syndrome is an often fatal encephalopathy in children that has been associated with the use of ASA during viral infection.
Similar to acetylsalicylic acid (ASA), bismuth subsalicylate may be associated with a higher risk of Reye’s syndrome in children; therefore it should be avoided in children or teenagers with viral infections such as influenza or chickenpox. Reye’s syndrome is an often fatal encephalopathy in children that has been associated with the use of ASA during viral infection.Side Effects
Misoprostol
Important Notes
 The acid-suppressant effects of misoprostol are dose related. An oral dose of 100 to 200 mcg inhibits basal acid secretion by up to 95% and meal-stimulated acid secretion by up to 85%.
The acid-suppressant effects of misoprostol are dose related. An oral dose of 100 to 200 mcg inhibits basal acid secretion by up to 95% and meal-stimulated acid secretion by up to 85%. Because of the high risk of diarrhea, it is recommended that misoprostol be administered with food to mitigate this side effect.
Because of the high risk of diarrhea, it is recommended that misoprostol be administered with food to mitigate this side effect. Bismuth subsalicylate contains salicylic acid, with a dose of 30 mL having approximately the same salicylate content as a 325-mg ASA tablet. Thus people who have an allergy or intolerance to ASA must avoid bismuth subsalicylate.
Bismuth subsalicylate contains salicylic acid, with a dose of 30 mL having approximately the same salicylate content as a 325-mg ASA tablet. Thus people who have an allergy or intolerance to ASA must avoid bismuth subsalicylate.Evidence
Prevention of NSAID-Induced Upper GI Toxicity
 A 2002 Cochrane review (40 studies) compared interventions (PG analogues, H2-antagonists, PPIs) for prevention of NSAID-induced upper GI toxicity. The review found that although all classes prevented NSAID-related gastric and duodenal ulcers, only misoprostol reduced the risk of ulcer complications such as perforation, hemorrhage, and obstruction.
A 2002 Cochrane review (40 studies) compared interventions (PG analogues, H2-antagonists, PPIs) for prevention of NSAID-induced upper GI toxicity. The review found that although all classes prevented NSAID-related gastric and duodenal ulcers, only misoprostol reduced the risk of ulcer complications such as perforation, hemorrhage, and obstruction.Prokinetics: Dopamine Antagonists
Moa (Mechanism of Action)
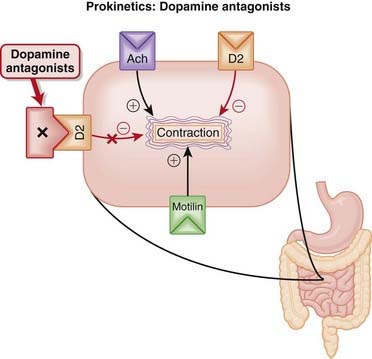
 Dopamine has an inhibitory effect on GI motility, mediated by the inhibitory effect of D2 receptors on ACh release. These natural inhibitory effects of dopamine include reduction of lower esophageal sphincter tone.
Dopamine has an inhibitory effect on GI motility, mediated by the inhibitory effect of D2 receptors on ACh release. These natural inhibitory effects of dopamine include reduction of lower esophageal sphincter tone. Therefore D2 antagonists increase lower esophageal sphincter tone, and stimulate contractions of the stomach and small intestine. The effects of metoclopramide and domperidone are largely confined to the upper GI tract, with minimal effect on the colon (Figure 15-5).
Therefore D2 antagonists increase lower esophageal sphincter tone, and stimulate contractions of the stomach and small intestine. The effects of metoclopramide and domperidone are largely confined to the upper GI tract, with minimal effect on the colon (Figure 15-5). The increase in lower esophageal sphincter tone is useful in reflux disorders such as GERD because it reduces the volume of gastric acid that enters the esophagus.
The increase in lower esophageal sphincter tone is useful in reflux disorders such as GERD because it reduces the volume of gastric acid that enters the esophagus. The D2 antagonists also act as antinauseants through central inhibition of the vomiting center (chemoreceptor trigger zone).
The D2 antagonists also act as antinauseants through central inhibition of the vomiting center (chemoreceptor trigger zone). Although they share D2 antagonism as a mechanism, the prokinetic actions of metoclopramide are very complex compared with those of domperidone. Metoclopramide also has the following actions:
Although they share D2 antagonism as a mechanism, the prokinetic actions of metoclopramide are very complex compared with those of domperidone. Metoclopramide also has the following actions:
Pharmacokinetics
 Metoclopramide is rapidly absorbed, undergoes hepatic metabolism, and is excreted mainly in the urine.
Metoclopramide is rapidly absorbed, undergoes hepatic metabolism, and is excreted mainly in the urine.Side Effects
Metoclopramide
 Extrapyramidal: Extrapyramidal effects are analogous to the side effects seen with the antipsychotics that are DA antagonists:
Extrapyramidal: Extrapyramidal effects are analogous to the side effects seen with the antipsychotics that are DA antagonists:
 Abnormal muscle tone (acute) and Parkinson-like symptoms (after a few weeks): Both are reversible and can also be managed with anticholinergics. DA plays an important role in normal movement, so blocking its effects will lead to disordered movement.
Abnormal muscle tone (acute) and Parkinson-like symptoms (after a few weeks): Both are reversible and can also be managed with anticholinergics. DA plays an important role in normal movement, so blocking its effects will lead to disordered movement. Tardive dyskinesia: These are abnormal, uncontrolled movements, particularly of the face (lips, tongue). They are seen with chronic therapy (months to years) and may not be reversible. Again, these are believed to be caused by inhibiting the effects of DA on normal movement. In this case, blockade of DA receptors may lead to enhanced sensitivity of these receptors, causing uncontrolled movement.
Tardive dyskinesia: These are abnormal, uncontrolled movements, particularly of the face (lips, tongue). They are seen with chronic therapy (months to years) and may not be reversible. Again, these are believed to be caused by inhibiting the effects of DA on normal movement. In this case, blockade of DA receptors may lead to enhanced sensitivity of these receptors, causing uncontrolled movement.Important Notes
 Domperidone does not cross the blood-brain barrier as readily as metoclopramide; therefore it lacks the extrapyramidal side effects associated with metoclopramide. Domperidone still does exert effects on areas that lie outside the blood-brain barrier, including the chemoreceptor trigger zone (nausea, vomiting). Hence domperidone maintains antinauseant effects.
Domperidone does not cross the blood-brain barrier as readily as metoclopramide; therefore it lacks the extrapyramidal side effects associated with metoclopramide. Domperidone still does exert effects on areas that lie outside the blood-brain barrier, including the chemoreceptor trigger zone (nausea, vomiting). Hence domperidone maintains antinauseant effects. The prokinetic activity of domperidone is considered to be relatively weak compared with that of metoclopramide.
The prokinetic activity of domperidone is considered to be relatively weak compared with that of metoclopramide. Children and young adults may be more susceptible to extrapyramidal side effects associated with metoclopramide.
Children and young adults may be more susceptible to extrapyramidal side effects associated with metoclopramide.Evidence
Nasoenteral Tube Migration
 A 2002 Cochrane review (four studies, N = 204 patients), updated in 2008, examined the use of intravenous metoclopramide on transpyloric passage of a nasoenteral tube compared with placebo or no intervention. The four included studies were small and did not find a statistically significant improvement in the enhancement of migration of nasoenteral tubes with metoclopramide.
A 2002 Cochrane review (four studies, N = 204 patients), updated in 2008, examined the use of intravenous metoclopramide on transpyloric passage of a nasoenteral tube compared with placebo or no intervention. The four included studies were small and did not find a statistically significant improvement in the enhancement of migration of nasoenteral tubes with metoclopramide.Antidiarrheals
Moa (Mechanism of Action)
Opiates
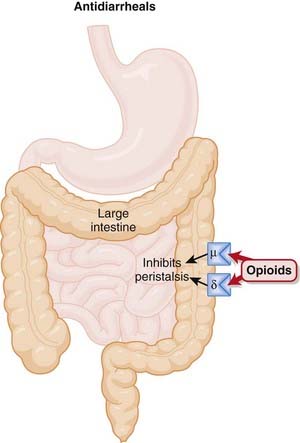
 The bowel contains both µ and δ opioid receptors. The δ receptors mediate intestinal secretion, the µ receptors mediate peristalsis, and both types of receptors play a role in intestinal absorption (Figure 15-6).
The bowel contains both µ and δ opioid receptors. The δ receptors mediate intestinal secretion, the µ receptors mediate peristalsis, and both types of receptors play a role in intestinal absorption (Figure 15-6). Loperamide and diphenoxylate are piperidines, structurally related to opiates such as meperidine. They are µ agonists, although they have less propensity for eliciting the euphoric effect typically seen with opiate analgesics because of limited CNS penetration.
Loperamide and diphenoxylate are piperidines, structurally related to opiates such as meperidine. They are µ agonists, although they have less propensity for eliciting the euphoric effect typically seen with opiate analgesics because of limited CNS penetration. µ Agonists reduce or completely abolish peristalsis in the colon, significantly delaying passage of feces through the bowel. The delayed transit through the bowel also increases the opportunity for increased absorption of fluid from the feces, producing a drying effect on the stool that further slows its progress through the bowel.
µ Agonists reduce or completely abolish peristalsis in the colon, significantly delaying passage of feces through the bowel. The delayed transit through the bowel also increases the opportunity for increased absorption of fluid from the feces, producing a drying effect on the stool that further slows its progress through the bowel.Bulk-Forming Agents
 Although bulk-forming agents are used to treat constipation, they have also been successfully used to treat mild cases of diarrhea. The mechanism is not well understood, but colloids that are insoluble and do not ferment may provide some additional structural integrity to the stool, reducing its viscosity.
Although bulk-forming agents are used to treat constipation, they have also been successfully used to treat mild cases of diarrhea. The mechanism is not well understood, but colloids that are insoluble and do not ferment may provide some additional structural integrity to the stool, reducing its viscosity.Pharmacokinetics
 Loperamide does not penetrate the blood-brain barrier very readily, in large part because of the actions of the P-glycoprotein (Pgp) transporter. This limits the euphoria experienced with loperamide use. It is not clear whether concomitant administration of Pgp inhibitors is able to increase the euphoria experienced with loperamide.
Loperamide does not penetrate the blood-brain barrier very readily, in large part because of the actions of the P-glycoprotein (Pgp) transporter. This limits the euphoria experienced with loperamide use. It is not clear whether concomitant administration of Pgp inhibitors is able to increase the euphoria experienced with loperamide. The bulk-forming or hydroscopic agents are generally clays that are able to absorb a significant amount of water. This absorptive ability is not selective, however, and agents such as kaolin may bind other substances, including drugs and nutrients. It is therefore advised that administration of these agents be separated from the administration of other agents by about 2 to 3 hours.
The bulk-forming or hydroscopic agents are generally clays that are able to absorb a significant amount of water. This absorptive ability is not selective, however, and agents such as kaolin may bind other substances, including drugs and nutrients. It is therefore advised that administration of these agents be separated from the administration of other agents by about 2 to 3 hours.Contraindications
Important Notes
 Diarrhea is generally considered to be a self-limiting condition that is best treated with oral rehydration and maintenance of electrolytes. In many cases, particularly with infectious diarrhea, treatment with constipating agents may actually prolong the disease, unless accompanied by antibiotic therapy (see evidence section).
Diarrhea is generally considered to be a self-limiting condition that is best treated with oral rehydration and maintenance of electrolytes. In many cases, particularly with infectious diarrhea, treatment with constipating agents may actually prolong the disease, unless accompanied by antibiotic therapy (see evidence section). Diphenoxylate and difenoxin are marketed as combination products with atropine. Atropine is an anticholinergic and will therefore also reduce GI motility. This reduces the need for higher doses of these agents, which in turn reduces the potential for abuse.
Diphenoxylate and difenoxin are marketed as combination products with atropine. Atropine is an anticholinergic and will therefore also reduce GI motility. This reduces the need for higher doses of these agents, which in turn reduces the potential for abuse. Although studies have shown that loperamide elicits very little euphoria, even at high doses, diphenoxylate does induce an opiate-like euphoric effect at higher doses (40 to 60 mg). Hence diphenoxylate remains a controlled drug, while loperamide is readily available without a prescription.
Although studies have shown that loperamide elicits very little euphoria, even at high doses, diphenoxylate does induce an opiate-like euphoric effect at higher doses (40 to 60 mg). Hence diphenoxylate remains a controlled drug, while loperamide is readily available without a prescription. Bismuth compounds are also widely used in the treatment of diarrhea (see the discussion of GI cytoprotectants in this chapter for other actions and details about bismuth compounds). Their mechanism in the treatment of diarrhea is not well defined, although they do contain clays and this might contribute as a bulk-forming agent, as described earlier. The bismuth compounds may also have antisecretory and antimicrobial effects.
Bismuth compounds are also widely used in the treatment of diarrhea (see the discussion of GI cytoprotectants in this chapter for other actions and details about bismuth compounds). Their mechanism in the treatment of diarrhea is not well defined, although they do contain clays and this might contribute as a bulk-forming agent, as described earlier. The bismuth compounds may also have antisecretory and antimicrobial effects. Somatostatin analogues (octreotide, somatostatin) are also used to treat certain forms of diarrhea. See the discussion of somatostatin analogues in Chapter 14.
Somatostatin analogues (octreotide, somatostatin) are also used to treat certain forms of diarrhea. See the discussion of somatostatin analogues in Chapter 14.Advanced
 Racecadotril is a novel antidiarrheal that targets δ opiate receptors indirectly, by inhibiting an enzyme (enkephalinase) that breaks down endogenous enkephalins, hence enhancing their stimulation of this opiate receptor. Thus this agent specifically targets the secretory component of diarrhea. It has been investigated in types of diarrhea characterized by large secretion of fluid.
Racecadotril is a novel antidiarrheal that targets δ opiate receptors indirectly, by inhibiting an enzyme (enkephalinase) that breaks down endogenous enkephalins, hence enhancing their stimulation of this opiate receptor. Thus this agent specifically targets the secretory component of diarrhea. It has been investigated in types of diarrhea characterized by large secretion of fluid.Evidence
Antimotility Agents in Combination with Antibiotics for Traveler’s Diarrhea
 A 2008 systematic review (nine trials, N = 1435 participants) examined the effect of using antimotility agents such as loperamide in conjunction with antibiotics for traveler’s diarrhea. The authors found that combinations of loperamide and antibiotics were more likely to produce a cure than antibiotics alone, both after 24 hours (odds ratio [OR] 2.6) and after 48 hours (OR 2.2).
A 2008 systematic review (nine trials, N = 1435 participants) examined the effect of using antimotility agents such as loperamide in conjunction with antibiotics for traveler’s diarrhea. The authors found that combinations of loperamide and antibiotics were more likely to produce a cure than antibiotics alone, both after 24 hours (odds ratio [OR] 2.6) and after 48 hours (OR 2.2).Antimotility Agents for Chronic Diarrhea in Patients with HIV/AIDS
 A 2008 Cochrane review (one trial, N = 91 participants) assessed the effectiveness of antimotility agents in treating chronic diarrhea in patients with human immunodeficiency virus (HIV) infection and acquired immunodeficiency syndrome (AIDS). The authors did not find any trials involving antimotility agents. They found no evidence that the adsorbent attapulgite was superior to placebo in controlling diarrhea.
A 2008 Cochrane review (one trial, N = 91 participants) assessed the effectiveness of antimotility agents in treating chronic diarrhea in patients with human immunodeficiency virus (HIV) infection and acquired immunodeficiency syndrome (AIDS). The authors did not find any trials involving antimotility agents. They found no evidence that the adsorbent attapulgite was superior to placebo in controlling diarrhea.Laxatives
Moa (Mechanism of Action)
Stimulant
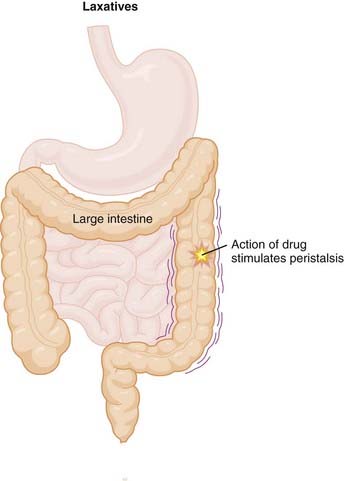
 Stimulant laxatives are also known as irritant laxatives, and, as the name suggests, they work by irritating the intestinal wall, which leads to an accumulation of fluid and electrolytes and increased motility.
Stimulant laxatives are also known as irritant laxatives, and, as the name suggests, they work by irritating the intestinal wall, which leads to an accumulation of fluid and electrolytes and increased motility. The method by which stimulant laxatives irritate the intestinal wall has not been clearly defined, although likely mediators include the activation of cAMP and cyclic guanosine monophosphate (cGMP) pathways, inhibition of Na/K-ATPase, and increased platelet activating factor production (Figure 15-7).
The method by which stimulant laxatives irritate the intestinal wall has not been clearly defined, although likely mediators include the activation of cAMP and cyclic guanosine monophosphate (cGMP) pathways, inhibition of Na/K-ATPase, and increased platelet activating factor production (Figure 15-7).Bulk
 Water is the largest determinant of stool volume, making up 70% to 85% of stool. A large amount of fluid is also extracted from stool as it makes its way through the intestines. Interruptions in this extraction of water, either excess extraction (constipation) or reduced extraction (diarrhea) can lead to GI problems.
Water is the largest determinant of stool volume, making up 70% to 85% of stool. A large amount of fluid is also extracted from stool as it makes its way through the intestines. Interruptions in this extraction of water, either excess extraction (constipation) or reduced extraction (diarrhea) can lead to GI problems. Fiber promotes intestinal motility by increasing the bulk of the stool. This is accomplished by increasing the bacterial content of stool by fermentation of fiber (fermentable fiber) or simply by drawing water into the stool (nonfermentable fiber). Many substances in the diet perform a combination of the two. Fiber, and specifically the short-chain fatty acids produced by fiber, may also have a direct stimulatory effect on the gut.
Fiber promotes intestinal motility by increasing the bulk of the stool. This is accomplished by increasing the bacterial content of stool by fermentation of fiber (fermentable fiber) or simply by drawing water into the stool (nonfermentable fiber). Many substances in the diet perform a combination of the two. Fiber, and specifically the short-chain fatty acids produced by fiber, may also have a direct stimulatory effect on the gut.Osmotics
 There are two types of osmotic laxatives: those made of sugars and alcohols and those that are salts of electrolytes.
There are two types of osmotic laxatives: those made of sugars and alcohols and those that are salts of electrolytes. A shared mechanism of both types is that they create an osmotic force, pulling water into the stool and creating additional bulk, in a manner analogous to that seen with the bulk agents. The sugars are typically nonabsorbable, such as mannitol, sorbitol, and lactulose.
A shared mechanism of both types is that they create an osmotic force, pulling water into the stool and creating additional bulk, in a manner analogous to that seen with the bulk agents. The sugars are typically nonabsorbable, such as mannitol, sorbitol, and lactulose. Additional mechanisms may contribute to the efficacy of the electrolyte salts, and these agents are generally considered to be more potent than the sugars. For example, magnesium-containing laxatives may stimulate CCK release, which in turn leads to increased fluid and electrolytes within the gut lumen and increased motility.
Additional mechanisms may contribute to the efficacy of the electrolyte salts, and these agents are generally considered to be more potent than the sugars. For example, magnesium-containing laxatives may stimulate CCK release, which in turn leads to increased fluid and electrolytes within the gut lumen and increased motility.Softeners
 As the name suggests, softeners are emollients that soften the stool, making defecation easier. They accomplish this in a variety of ways.
As the name suggests, softeners are emollients that soften the stool, making defecation easier. They accomplish this in a variety of ways.Pharmacokinetics
Side Effects
 Laxatives are generally well tolerated when used in moderation, with mild side effects that are typically an extension of their pharmacologic effect
Laxatives are generally well tolerated when used in moderation, with mild side effects that are typically an extension of their pharmacologic effectImportant Notes
 Osmotic sugar laxatives are useful in the treatment of constipation caused by opiates, as well as constipation in the elderly.
Osmotic sugar laxatives are useful in the treatment of constipation caused by opiates, as well as constipation in the elderly. Lactulose is used as a treatment for hepatic encephalopathy (confusion or decreased level of consciousness caused by liver failure). Patients with severe liver disease have difficulty detoxifying ammonia, which is produced by bacterial metabolism of feces. The actions of lactulose decrease intestinal pH, which traps ammonia within the lumen of the gut, facilitating its exit from the body.
Lactulose is used as a treatment for hepatic encephalopathy (confusion or decreased level of consciousness caused by liver failure). Patients with severe liver disease have difficulty detoxifying ammonia, which is produced by bacterial metabolism of feces. The actions of lactulose decrease intestinal pH, which traps ammonia within the lumen of the gut, facilitating its exit from the body.| Highly Fermentable | Poorly Fermentable or Nonfermentable |
|---|---|
| Hemicellulose | Lignin |
| Mucilages and gums | Cellulose |
| Pectins |
Evidence
Laxatives for Constipation in Palliative Care Patients
 A 2006 Cochrane review (four trials, N = 280 participants) compared laxatives used for constipation in palliative care patients. All laxatives demonstrated a limited degree of efficacy, although these results were confounded by significant use of rescue laxatives during the studies. The only significantly different treatments were in a comparison of lactulose + senna versus danthron + poloxamer. The authors concluded that there was a paucity of data for this indication in this population.
A 2006 Cochrane review (four trials, N = 280 participants) compared laxatives used for constipation in palliative care patients. All laxatives demonstrated a limited degree of efficacy, although these results were confounded by significant use of rescue laxatives during the studies. The only significantly different treatments were in a comparison of lactulose + senna versus danthron + poloxamer. The authors concluded that there was a paucity of data for this indication in this population.FYI
 Several of the most commonly used laxatives are plant-derived, including many of the stimulant laxatives such as cascara (bark of the Buckthorn tree), senna (leaflets on pods of Cassia angustifolia), and castor oil (bean of the castor plant).
Several of the most commonly used laxatives are plant-derived, including many of the stimulant laxatives such as cascara (bark of the Buckthorn tree), senna (leaflets on pods of Cassia angustifolia), and castor oil (bean of the castor plant).Cannabinoids
Moa (Mechanism of Action)
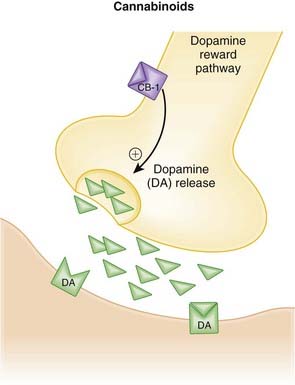
 The cannabinoid (CB) receptors are G-protein–coupled receptors that are widely distributed throughout the body, most notably in the CNS.
The cannabinoid (CB) receptors are G-protein–coupled receptors that are widely distributed throughout the body, most notably in the CNS. In the periphery, CB1 receptors are found in adipocytes, the adrenal gland, the ovaries, the testes, and the GI tract.
In the periphery, CB1 receptors are found in adipocytes, the adrenal gland, the ovaries, the testes, and the GI tract. The location of CB1 receptors in areas of the brain (i.e., the hypothalamus) associated with feeding, coupled with the longstanding observation of the appetite-stimulating effects of cannabis, led to the conclusion that CB1 receptors may play an important role in the treatment of obesity.
The location of CB1 receptors in areas of the brain (i.e., the hypothalamus) associated with feeding, coupled with the longstanding observation of the appetite-stimulating effects of cannabis, led to the conclusion that CB1 receptors may play an important role in the treatment of obesity. These regions of the brain are also interrelated with the mesolimbic DA pathway, also known as the reward pathway. This explains another, perhaps more well known effect of cannabis, that of euphoria and reward. The link between the reward pathways in the brain and the hypothalamus might also explain why eating is also associated with reward.
These regions of the brain are also interrelated with the mesolimbic DA pathway, also known as the reward pathway. This explains another, perhaps more well known effect of cannabis, that of euphoria and reward. The link between the reward pathways in the brain and the hypothalamus might also explain why eating is also associated with reward. Evidence of a link between smoking and the endocannabinoid pathway comes from the observation that THC triggers release of DA in the reward pathway via CB1 receptors, in the same way that nicotine stimulates DA release via nicotinic receptors. Chronic nicotine administration increases levels of endogenous cannabinoids, which then bind to CB1 receptors and elicit a feeling of reward.
Evidence of a link between smoking and the endocannabinoid pathway comes from the observation that THC triggers release of DA in the reward pathway via CB1 receptors, in the same way that nicotine stimulates DA release via nicotinic receptors. Chronic nicotine administration increases levels of endogenous cannabinoids, which then bind to CB1 receptors and elicit a feeling of reward. The potential of CB1 antagonists as antiobesity drugs is supported by the actions of CB1 in adipose tissue. CB1 antagonism may decrease lipogenesis and increase adiponectin levels. Adiponectin is a hormone secreted by adipocytes. It plays a role in lipid and glucose metabolism and also influences response to insulin. Low levels of adiponectin are found in obesity, and high levels are associated with reduced risk of heart attack.
The potential of CB1 antagonists as antiobesity drugs is supported by the actions of CB1 in adipose tissue. CB1 antagonism may decrease lipogenesis and increase adiponectin levels. Adiponectin is a hormone secreted by adipocytes. It plays a role in lipid and glucose metabolism and also influences response to insulin. Low levels of adiponectin are found in obesity, and high levels are associated with reduced risk of heart attack.Pharmacokinetics
Agonists
 Δ9-THC is well absorbed but undergoes extensive first-pass metabolism and significant distribution into tissues, thus limiting the amount (10% to 20%) of oral dose that reaches the systemic circulation.
Δ9-THC is well absorbed but undergoes extensive first-pass metabolism and significant distribution into tissues, thus limiting the amount (10% to 20%) of oral dose that reaches the systemic circulation.Contraindications
Important Notes
 The combination of Δ9-THC and cannabidiol, a nonpsychoactive plant cannabinoid, is being used for neuropathic pain in MS and as an adjunctive analgesic in advanced cancer.
The combination of Δ9-THC and cannabidiol, a nonpsychoactive plant cannabinoid, is being used for neuropathic pain in MS and as an adjunctive analgesic in advanced cancer.FYI
 Endocannabinoids such as anandamide are eicosanoids and are therefore derived from arachidonic acid. The name anandamide is derived from Sanskrit for bliss.
Endocannabinoids such as anandamide are eicosanoids and are therefore derived from arachidonic acid. The name anandamide is derived from Sanskrit for bliss. There are approximately 70 naturally occurring cannabinoids, and THC is the most important psychoactive compound of the group. There are many isomers of THC, but the Δ9-THC isomer is considered to be the most active.
There are approximately 70 naturally occurring cannabinoids, and THC is the most important psychoactive compound of the group. There are many isomers of THC, but the Δ9-THC isomer is considered to be the most active. The cannabinoids have been investigated in a variety of disorders, including neurologic disorders such as MS and Parkinson’s disease. In MS, cannabis is often used to treat spasticity. Cannabis has also been used since the 1970s for glaucoma.
The cannabinoids have been investigated in a variety of disorders, including neurologic disorders such as MS and Parkinson’s disease. In MS, cannabis is often used to treat spasticity. Cannabis has also been used since the 1970s for glaucoma. Legal issues around the use of medicinal marijuana have created problems with the study of cannabinoid agonists. Specific agonists such as dronabinol have been developed to further “medicinalize” the use of THC. However, the problem with using these specific compounds is that they may lose some of the pharmacologic contributions from the variety of other cannabinoids found in marijuana.
Legal issues around the use of medicinal marijuana have created problems with the study of cannabinoid agonists. Specific agonists such as dronabinol have been developed to further “medicinalize” the use of THC. However, the problem with using these specific compounds is that they may lose some of the pharmacologic contributions from the variety of other cannabinoids found in marijuana.Pancreatic Enzymes
Moa (Mechanism of Action)
 Deficiencies of pancreatic enzymes occur in disorders such as cystic fibrosis and chronic pancreatitis or in people in whom the pancreas has been surgically resected.
Deficiencies of pancreatic enzymes occur in disorders such as cystic fibrosis and chronic pancreatitis or in people in whom the pancreas has been surgically resected.Pharmacokinetics
Important Notes
 Most cystic fibrosis patients will experience pancreatic insufficiency. Cystic fibrosis is characterized by disruption of chloride transport as well as other transporters for sodium and bicarbonate. Patients have excessive intestinal mucoprotein, increasing the viscosity of the intestinal lumen. The increased viscosity leads to blockade of ducts, which damages acinar cells and causes fibrosis as well as exocrine pancreatic insufficiency.
Most cystic fibrosis patients will experience pancreatic insufficiency. Cystic fibrosis is characterized by disruption of chloride transport as well as other transporters for sodium and bicarbonate. Patients have excessive intestinal mucoprotein, increasing the viscosity of the intestinal lumen. The increased viscosity leads to blockade of ducts, which damages acinar cells and causes fibrosis as well as exocrine pancreatic insufficiency.Serotonin Antagonists
Moa (Mechanism of Action)
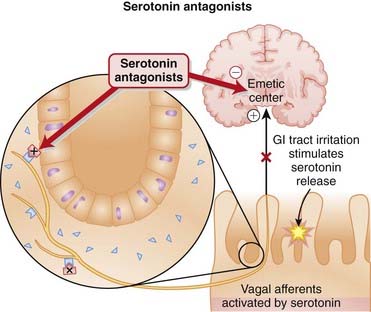
 5-HT3 receptors in the gut mediate contraction of various segments of the GI tract, including the fundus, corpus, and antrum. These receptors also sensitize spinal sensory neurons and participate in vagal signaling of nausea. 5-HT3 receptors in the brain also mediate nausea.
5-HT3 receptors in the gut mediate contraction of various segments of the GI tract, including the fundus, corpus, and antrum. These receptors also sensitize spinal sensory neurons and participate in vagal signaling of nausea. 5-HT3 receptors in the brain also mediate nausea. Chemotherapeutic agents used in cancer stimulate the release of 5-HT from enterochromaffin cells in the GI tract. This 5-HT activates 5-HT3 receptors on vagal sensory afferent neurons, and these neurons project to the emetic center in the brainstem (Figure 15-9).
Chemotherapeutic agents used in cancer stimulate the release of 5-HT from enterochromaffin cells in the GI tract. This 5-HT activates 5-HT3 receptors on vagal sensory afferent neurons, and these neurons project to the emetic center in the brainstem (Figure 15-9). 5-HT3 receptor antagonists were thus first developed for, and continue to be first-line agents in the treatment of chemotherapy-induced nausea and vomiting.
5-HT3 receptor antagonists were thus first developed for, and continue to be first-line agents in the treatment of chemotherapy-induced nausea and vomiting. Antagonism of 5-HT3 receptors also appears to slow intestinal transit and secretions of the small bowel and decreases colonic compliance. This accounts for the efficacy of some 5-HT3 antagonists in treating conditions such as irritable bowel syndrome (IBS).
Antagonism of 5-HT3 receptors also appears to slow intestinal transit and secretions of the small bowel and decreases colonic compliance. This accounts for the efficacy of some 5-HT3 antagonists in treating conditions such as irritable bowel syndrome (IBS).Pharmacokinetics
 The 5-HT3 antagonists all appear to have a prolonged biologic half-life, with actions persisting well past elimination from the systemic circulation.
The 5-HT3 antagonists all appear to have a prolonged biologic half-life, with actions persisting well past elimination from the systemic circulation.Side Effects
 Constipation or diarrhea: Constipation is more common, and likely occurs because of 5-HT3 antagonism in the gut, which slows intestinal transit. The mechanism for the diarrhea is not clear.
Constipation or diarrhea: Constipation is more common, and likely occurs because of 5-HT3 antagonism in the gut, which slows intestinal transit. The mechanism for the diarrhea is not clear.Rare but Serious
 Ischemic colitis has been associated with alosetron. This may be related to the ability of alosetron to induce contractions in the GI tract, in this case resulting in severe spasms in certain individuals.
Ischemic colitis has been associated with alosetron. This may be related to the ability of alosetron to induce contractions in the GI tract, in this case resulting in severe spasms in certain individuals. Electrocardiographic (ECG) changes: QT prolongation and other ECG changes have been reported. These changes are typically harmless but rarely may lead to clinically significant arrhythmias. Caution is advised when administering other drugs that may prolong the QT interval or in patients with QT prolongation.
Electrocardiographic (ECG) changes: QT prolongation and other ECG changes have been reported. These changes are typically harmless but rarely may lead to clinically significant arrhythmias. Caution is advised when administering other drugs that may prolong the QT interval or in patients with QT prolongation.Important Notes
 Alosetron was withdrawn from the U.S. market in 2000 because of concerns over ischemic colitis but was reintroduced in 2002 with a revised indication for women with severe IBS.
Alosetron was withdrawn from the U.S. market in 2000 because of concerns over ischemic colitis but was reintroduced in 2002 with a revised indication for women with severe IBS. Of all antiemetic agents, the 5-HT3 antagonists are among the most specific, having little if any affinity for any receptors other than serotonin receptors. This specificity may account for their paucity of side effects.
Of all antiemetic agents, the 5-HT3 antagonists are among the most specific, having little if any affinity for any receptors other than serotonin receptors. This specificity may account for their paucity of side effects.Evidence
Prevention of Postoperative Nausea and Vomiting
 A large (>100,000 subjects) 2006 Cochrane review compared a wide variety of agents with placebo and found that ondansetron, granisetron, tropisetron, and dolasetron were among eight drugs that prevented postoperative nausea and vomiting. Others were droperidol, dexamethasone, cyclizine, and metoclopramide.
A large (>100,000 subjects) 2006 Cochrane review compared a wide variety of agents with placebo and found that ondansetron, granisetron, tropisetron, and dolasetron were among eight drugs that prevented postoperative nausea and vomiting. Others were droperidol, dexamethasone, cyclizine, and metoclopramide.Relief of Emesis in Pediatric Gastroenteritis
 A 2006 Cochrane review examined the effectiveness of antiemetics in children and adolescents with vomiting induced by gastroenteritis. The conclusions were limited by the small studies (total of 396 subjects over three studies). The results suggested that ondansetron performed better than placebo in reducing the number of vomiting episodes in this population. This was at the expense of an increased incidence of diarrhea, thought to be a result of the retention of toxins that would normally have been eliminated by vomiting.
A 2006 Cochrane review examined the effectiveness of antiemetics in children and adolescents with vomiting induced by gastroenteritis. The conclusions were limited by the small studies (total of 396 subjects over three studies). The results suggested that ondansetron performed better than placebo in reducing the number of vomiting episodes in this population. This was at the expense of an increased incidence of diarrhea, thought to be a result of the retention of toxins that would normally have been eliminated by vomiting.