Chapter 52 Definition and classification of pancreatitis
Overview
Despite four international consensus meetings over 40 years, the issue of definition and classification of pancreatitis (see Chapters 53 to 55) is still under critical revision. The main reason is the difficulty, in contrast to other common inflammatory gastroenterologic diseases, to obtain pancreatic tissue specimens to define the diagnosis better during the inflammatory process. Any classification of pancreatitis must be based on clinical, morphologic, and laboratory features.
The history of the definition and classification of pancreatitis is characterized mainly by the distinction between acute and chronic pancreatitis as stated by Lagerlof in 1942. These two clinical conditions seemed to be two different and separate pathologic processes. In recent years, with the widening of clinical observation and improved accuracy of imaging studies, particularly magnetic resonance imaging (MRI) of the bile ducts and duct of Wirsung, the classic distinction between acute and chronic pancreatitis is under critical revision.
History of the Definition and Classification of Pancreatitis
The history of the definition and classification of pancreatitis shows the progressive awareness of experts that acute and chronic inflammation should be defined by different pathologic, clinical, and etiogenetic perspectives (Table 52.1). The different points of view correlate with each other and together provide the best comprehension of the inflammatory process. Consequently, the clinical management of an individual patient can be improved only by considering all the features of pancreatitis.
Table 52.1 A Synopsis of Pancreatitis Classification from 1946 to 2011
| Classification | Definition |
|---|---|
| Marseille, 1965 | Description of morphologic characteristics and etiologic factors of the disease; no categorization according to disease severity, no imaging findings |
| Cambridge, 1984 | Classification of disease severity based on pancreatic imaging criteria (US, CT, ERCP); discussion of etiologic factors and pancreatic function |
| Revised Marseille, 1985 | Description and further subclassification of morphologic changes; definition of “obstructive chronic pancreatitis” as a distinct form; no discussion of the correlation between anatomic and functional changes, no inclusion of pancreatic imaging findings |
| Marseille-Rome, 1988 | Further description of “chronic calcifying” and “chronic inflammatory” pancreatitis as distinct forms; description of etiologic factors; no further elaboration of clinical, functional, or imaging criteria |
| Atlanta, 1992 | Description of clinical and morphologic features of pancreatitis; dynamic classification system able to characterize the individual patient and predict severity |
| Zurich, 1997 | Description of clinical presentation and classification of the disease in “definite” and “probable” chronic pancreatitis according to imaging findings, functional testing, and histologic examination |
| Japan Pancreas Society, 1997 | Description of clinical presentation and classification of the disease in “definite” and “probable” chronic pancreatitis according to imaging findings, functional testing, and histologic examination; definition of radiologic and laboratory features in patients lacking etiologic and pathogenetic features |
| TIGAR-O, 2001 | Detailed categorization of etiologic risk factors and correlation between acute and chronic pancreatitis |
| ABC, 2002 | Disease grading according to clinical criteria; limited separation of different disease severities; not all clinical presentations categorized |
| Manchester, 2006 | Disease grading according to clinical criteria; limited separation of different disease severities |
| M-ANNHEIM, 2007 | Categorization of patients according to etiology, clinical stage, and severity of disease; severity of pancreatic inflammation assessed using a specific scoring system |
US, ultrasound; CT, computed tomography; ERCP, endoscopic retrograde cholangiopancreatography
The first effort to classify and define pancreatitis by a worldwide group of experts led to the Marseille Consensus Meeting in 1963 (Sarles, 1965). The panel of pancreatologists agreed that acute and chronic pancreatitis were different diseases mainly because of different morphologic patterns. Relapsing pancreatitis was characterized by the presence of multiple episodes in a morphologic pattern of acute or chronic processes. The distinctive features of the two diseases were the pathologic benign course of acute inflammation, with biologic restitution in the acute condition, and the progressively worsening parenchymal lesions in the chronic condition (Table 52.2). The present histology-based classification does not provide clinically useful definitions, making it impossible to compare different experiences. From the clinical point of view, acute and chronic pancreatitis show a similar pattern, at least in the earlier phases.
Table 52.2 Marseille Classification of Pancreatitis
| Feature | Acute Pancreatitis/Acute Relapsing Pancreatitis | Chronic Relapsing Pancreatitis/Chronic Pancreatitis |
|---|---|---|
| Clinical characteristics | Single/multiple episodes | Multiple episodes/no acute exacerbations is common |
| Morphologic characteristics | Not defined | Irregular sclerosis with destruction and focal segmental or diffuse loss of parenchyma with varying dilation of ductal system; strictures, intracanalicular stones (calcifications), cysts, pseudocysts; islets of Langerhans are involved much later in the course of the disease; morphologic picture is similar, independent of cause |
| Course | Clinical and biologic restitution if the cause is removed | Functional and morphologic lesions persist or progress after the cause is removed |
Modified from Sarles H, 1965: Proposal adopted unanimously by the participants of the symposium of acute pancreatitis in Marseille, 1963. Bibl Gastroenterol 7:7-8.
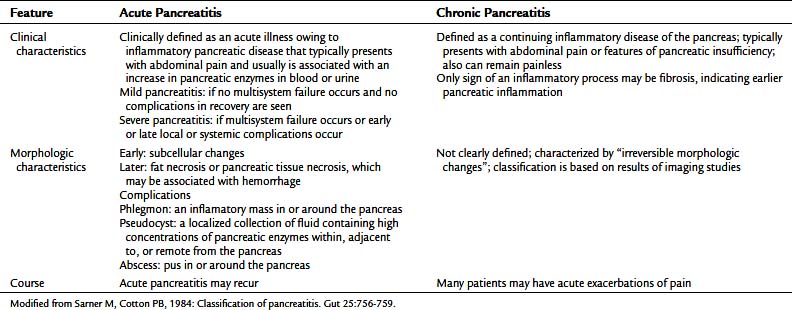
Progress in the comprehension of pancreatitis and its classification resulted from the Cambridge meeting (Sarner & Cotton, 1984). The distinction between acute and chronic pancreatitis was confirmed, and the term relapsing pancreatitis was avoided in the chosen terminology. The importance of the clinical impact of different severity systemic responses was emphasized (Table 52.3), and the importance of definition of a morphologic characterization of the inflammatory process was recognized, particularly for the acute pancreatitis group. The Cambridge group pointed out the relevant problem of etiology, and the role of imaging in chronic pancreatitis was addressed.
Endoscopic retrograde cholangiopancreatography (ERCP) classification (Table 52.4) is still in use in some centers. Several studies in the literature showed that ERCP findings are not pathognomonic of chronic pancreatitis but could coexist with many clinical conditions. In particular, cholelithiasis and its complications lead to demonstrable alterations in the morphology of the duct of Wirsung, as stated in the Cambridge classification (Buchler et al, 1987; Misra et al, 1990), and these morphologic changes could persist for many months. In biliary cirrhosis, Sjögren syndrome, and sclerosing cholangitis, pancreatic duct changes are commonly observed at ERCP (Bastid et al, 1990; Epstein et al, 1982; Lindstrom et al, 1991). For all these reasons, the ERCP morphology of the duct of Wirsung is not mandatory to diagnose chronic disease. In addition, increasing use of MRI of the bile ducts and duct of Wirsung provides excellent morphologic imaging of the main and side branch ducts.
Table 52.4 Grading of Chronic Pancreatitis by Endoscopic Retrograde Cholangiopancreatography
| Normal |
CT, Computed tomography
Modified from Sarner M, Cotton PB, 1984: Classification of pancreatitis. Gut 25:756-759.
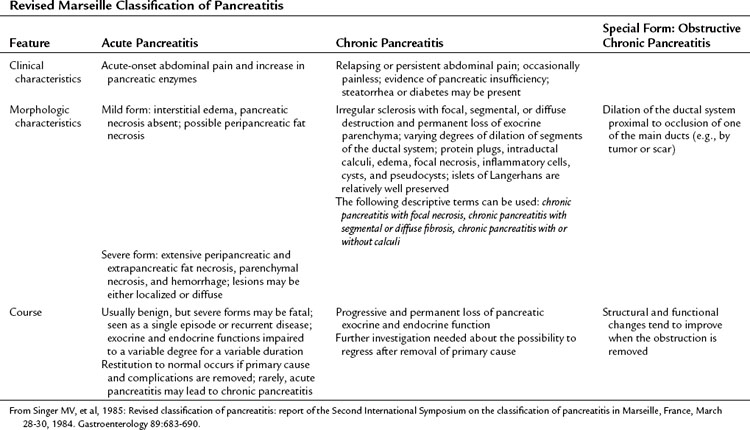
The increasing attention to duct morphology and consequently to the cause-and-effect relationship of obstruction resulted in new terminology at the second Marseille meeting held in 1984 (Singer et al, 1985). In addition to the classic distinction between acute and chronic disease, a new entity was identified: obstructive chronic pancreatitis (Table 52.5). The role of duct obstruction in the chronic inflammatory process was recognized as a distinctive pathway to developing pancreatitis. This new concept has gained importance over the years in distinguishing chronic calcifying pancreatitis in alcoholics from obstructive chronic pancreatitis initially presenting as relapsing acute attacks owing to strictures resulting from different conditions, such as solid tumors, mucinous plugs typical of intraductal papillary mucinous tumors, severe pancreatitis with duct disruption, and scar and inflammation of the sphincter of Oddi of biliary origin. Regarding acute pancreatitis, another hallmark was recognized by the second Marseille meeting: The rule in mild pancreatitis is the absence of necrosis. The recognition of a dramatic and central role of necrosis in severe pancreatitis opened the doors to wide-ranging and fundamental studies on severity assessment and complication prevention; increasing use of CT scan in staging of the disease also contributed (Beger et al, 1985).
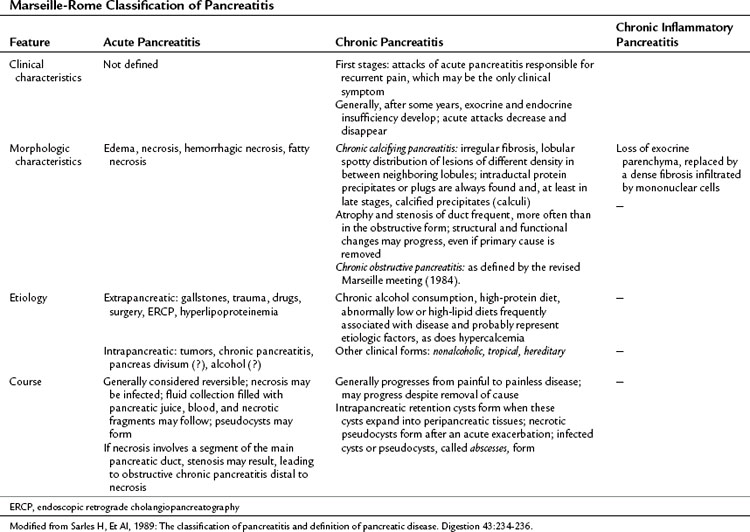
A panel of experts met in Rome in 1988 to integrate the second Marseille classification into use (Table 52.6). The main feature of the new classification (Sarles et al, 1989) was the statement about the reversibility of the lesions observed in the course of acute pancreatitis; even the severe forms responded to clinical observation in almost half of severe pancreatitis patients. In contrast, in chronic pancreatitis, some pathologic features were defined as permanent, and the condition was described as chronic inflammatory pancreatitis, morphologically characterized by loss of exocrine parenchyma and fibrosis with mononuclear cell infiltration. For the first time, etiology specifically was addressed, with pancreas divisum and alcohol as possible causes of acute pancreatitis.
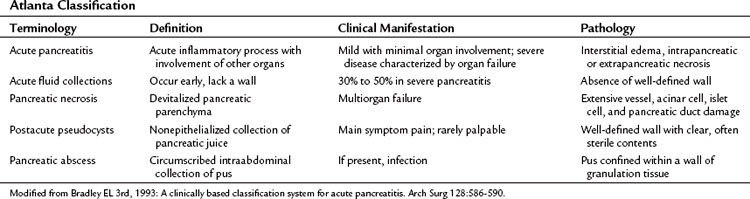
The need for further effort to better define acute pancreatitis resulted from the observation that the terminology of the Rome meeting was conflicting and not widely applied all over the world (Lumsden & Bradley, 1990). In 1992, 40 pancreatologists met in Atlanta and developed a new, reliable classification system of acute pancreatitis (Table 52.7; Bradley, 1993). The clinical and morphologic features of pancreatitis were considered, resulting in a dynamic ongoing classification system better able to characterize the individual patient and predict disease severity.
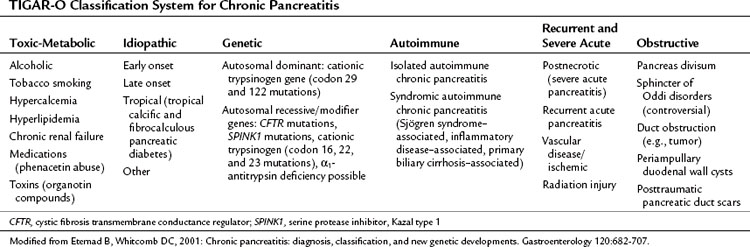
The Zurich classification for alcoholic chronic pancreatitis (Table 52.8; Amman, 1997) specifically addresses the most common cause of the disease and gives less importance to other causes, which are sometimes difficult to diagnose, resulting in a quite complex classification system not widely adopted. In 1997, a new definition of chronic pancreatitis was published, dividing definite from probable chronic pancreatitis (Table 52.9; Homma et al, 1997). This definition provided a list of radiologic or laboratory features in chronic pancreatitis patients lacking etiologic and pathogenetic features. The TIGAR-O risk factor classification system (toxic-metabolic, idiopathic, genetic, autoimmune, recurrent severe, obstructive) (Table 52.10), provides a complete overview of the risk factors for chronic pancreatitis development with special attention to the relationship between acute and chronic disease (Etemad & Whitcomb, 2001). In recent years, two main three-stage categorization systems have been mainly proposed: the ABC system (Ramesh, 2002) and the Manchester classification (Table 52.11; Bagul & Siriwardena, 2006). The aim of these systems is to provide an accurate description of chronic pancreatitis, underlining different therapeutic approaches and prognoses depending on disease stage. The ABC system divides patients into grades depending on the presence or absence of abdominal pain, complications, and deficiency in pancreatic function. The Manchester classification uses the terms mild, moderate, and end stage to represent disease progression, allowing comparison between patient groups.
Table 52.8 Zurich Classification for Alcoholic Chronic Pancreatitis
| Definite Alcoholic Chronic Pancreatitis | Probable Alcoholic Chronic Pancreatitis |
|---|---|
| In addition to a typical history or a history of excessive alcohol intake (≥80 g/day), ≥1 of the following criteria establish the diagnosis: Calcification in the pancreas Moderate to marked ductal lesions (Cambridge criteria) Marked exocrine insufficiency defined as steatorrhea (>7 g fat/24 h) normalized or markedly reduced by enzyme supplementation Typical histology of an adequate surgical specimen |
In addition to a typical history or a history of excessive alcohol intake (≥80 g/day), the diagnosis of probable chronic pancreatitis is likely if any of the following criteria are present: |
| Mild ductal alterations (Cambridge criteria) | |
| Recurrent or persistent pseudocysts | |
| Pathologic secretin test | |
| Endocrine insufficiency | |
| Etiologic Factors* | |
|
Alcoholic chronic pancreatitis Nonalcoholic chronic pancreatitis Tropical (nutritional) chronic pancreatitis Hereditary chronic pancreatitis Metabolic (hypercalcemic, hypertriglyceridemic) chronic pancreatitis Idiopathic (early and late onset) chronic pancreatitis Autoimmune chronic pancreatitis Chronic pancreatitis resulting from miscellaneous causes (e.g., radiation injury, phenacetin abuse) Chronic pancreatitis associated with anatomic abnormalities (anatomic chronic pancreatitis—periampullary duodenal wall cysts, pancreas divisum, obstructive pancreatitis, posttraumatic pancreatic duct scars) |
|
| Clinical Staging | |
* These diagnostic definitions also may be used for nonalcoholic chronic pancreatitis.
From Amman RW, 1997: A clinically based classification system for alcoholic chronic pancreatitis: summary of an international workshop on chronic pancreatitis. Pancreas 14:215-221.
Table 52.9 Diagnostic Criteria for Chronic Pancreatitis from the Japan Pancreas Society
| Definite Chronic Pancreatitis | Probable Chronic Pancreatitis |
|---|---|
| Ultrasound: pancreatic stones evidenced by intrapancreatic hyperreflective echoes with acoustic shadows behindCT: pancreatic stones evidenced by intrapancreatic calcifications | Ultrasound: intrapancreatic coarse hyperreflective echoes, irregular dilation of pancreatic ducts, or pancreatic deformity with irregular contour CT: pancreatic deformity with irregular contour |
| ERCP: irregular dilation of pancreatic duct branches of variable intensity with scattered distribution throughout the entire pancreas or irregular dilation of the main pancreatic duct and branches proximal to complete or incomplete obstruction of the main pancreatic duct (with pancreatic stones or protein plugs) | ERCP: irregular dilation of the main pancreatic duct alone; intraductal filling defects suggest noncalcified pancreatic stones or protein plugs |
| Secretin test: abnormally low bicarbonate concentration combined with either decreased enzyme outputs or decreased secretory volume Histologic examination: irregular fibrosis with destruction and loss of exocrine parenchyma in tissue specimens obtained by biopsy, surgery, or autopsy; fibrosis with an irregular and patchy distribution in the interlobular spaces; intralobular fibrosis alone not specific for chronic pancreatitis |
Secretin test: abnormally low bicarbonate concentration alone or decreased enzyme output plus decreased secretory volume; tubeless tests: simultaneous abnormalities in benzoyl-tyrosyl-p-amino benzoic acid and fecal chymotrypsin tests observed at two points several months apart |
| Histologic examination: intralobular fibrosis with one of the following findings: loss of exocrine parenchyma, isolated islets of Langerhans, or pseudocysts | |
| Protein plugs, pancreatic stones, dilation of the pancreatic ducts, hyperplasia and metaplasia of the ductal epithelium, and cyst formation |
CT, computed tomography; ERCP, endoscopic retrograde cholangiopancreatography
Modified from Homma T, et al, 1997: Diagnostic criteria for chronic pancreatitis by the Japan Pancreas Society. Pancreas 15:14-15.
Table 52.11 Manchester Classification System for Chronic Pancreatitis
| Mild: Five Essential Criteria |
| Moderate: Five Essential Criteria |
| End Stage |
Note that abdominal pain may or may not be present.
ERP, endoscopic retrograde pancreatography; MRP, magnetic resonance pancreatography; CT, computed tomography
Modified from Bagul A, Siriwardena AK, 2006: Evaluation of the Manchester Classification System for Chronic Pancreatitis. J Pancreas (Online) 7(4):390-396.
The most recent classification attempt is represented by the M-ANNHEIM multiple risk factor system (Table 52.12), aimed to provide a standardized method for the clinical diagnosis of chronic pancreatitis according to etiology, clinical stage, and severity of disease and to direct clinical practice (Schneider et al, 2007).
Table 52.12 The M-ANNHEIM Multiple Risk Factor Classification System
| Multiple Risk Factor Classification | Clinical Staging of Chronic Pancreatitis |
|---|---|
| Alcohol consumption | Asymptomatic chronic pancreatitis |
| Nicotine consumption | 0. Stage of subclinical chronic pancreatitis |
| Nutritional factors | Symptomatic chronic pancreatitis |
| Hereditary factors | I. Stage without pancreatic insufficiency |
| Efferent duct factors | II. Stage of partial pancreatic insufficiency |
| Immunologic factors | III. Stage of painful complete pancreatic insufficiency |
| Miscellaneous and rare metabolic factors | IV. Stage of secondary painless disease (burnout) |
| Diagnostic Criteria of Chronic Pancreatitis | |
| The diagnosis requires a typical clinical history of chronic pancreatitis, such as recurrent pancreatitis or abdominal pain, except for primary painless pancreatitis. Based on these features, the three forms of chronic pancreatitis are 1) definite chronic pancreatitis, 2) probable chronic pancreatitis, and 3) borderline chronic pancreatitis. | |
| Scoring System for the Grading of Clinical Features of Chronic Pancreatitis Points | |
| Patient report of pain | 0-4 |
| Pain control | 0-2 |
| Surgical intervention | 0 or 4 |
| Exocrine insufficiency | 0-2 |
| Endocrine insufficiency | 0 or 4 |
| Morphologic status on pancreatic imaging | 0-4 |
| Severe organ complications | 0, 2, or 4 |
| Severity Index of Chronic Pancreatitis | |
| Severity Level | Point Range |
| M-Annheim A Minor | 0-5 Points |
| M-Annheim B Increased | 6-10 points |
| M-Annheim C Advanced | 11-15 points |
| M-Annheim D Marked | 16-20 points |
| M-Annheim E Exacerbated | >20 points |
Modified from Schneider A, Lohr JM, Singer MV, 2007: The M-ANNHEIM classification of chronic pancreatitis: introduction of a unifying classification system based on a review of previous classification of the disease. J Gastroenterol 42:101-119.
Amman RW. A clinically based classification system for alcoholic chronic pancreatitis: summary of an international workshop on chronic pancreatitis. Pancreas. 1997;14:215-221.
Bagul A, Siriwardena AK. Evaluation of the Manchester Classification System for Chronic Pancreatitis. JOP. J Pancreas. 2006;7(4):390-396.
Bastid C, et al. Spontaneous healing of sclerosing cholangitis associated with stricture of the main pancreatic duct. Pancreas. 1990;4:489-492.
Beger HG, et al. Results of surgical treatment of necrotizing pancreatitis. World J Surg. 1985;9:972-979.
Bradley ELIII. A clinically based classification system for acute pancreatitis. Arch Surg. 1993;128:586-590.
Buchler M, et al. Follow-up after acute pancreatitis: morphology and function. In: Beger, HG, Buchler, M. Acute Pancreatitis—Research and Clinical Management. Berlin: Springer-Verlag; 1987:367-374.
Epstein O, et al. The pancreas in primary biliary cirrhosis and primary sclerosing cholangitis. Gastroenterology. 1982;83:1177-1182.
Etemad B, Whitcomb DC. Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterology. 2001;120:682-707.
Homma T, et al. Diagnostic criteria for chronic pancreatitis by the Japan Pancreas Society. Pancreas. 1997;15:14-15.
Lagerlof HO, 1942: Pancreatic function and pancreatic disease studied by means of secretin. Stockholm, PA Norstedt & Soner.
Lindstrom E, et al. Pancreatic ductal morphology and function in Sjögren’s syndrome. Int J Pancreatol. 1991;8:141-149.
Lumsden A, Bradley EL3rd. Secondary pancreatic infections. Surg Gynecol Obstet. 1990;170:459-467.
Misra SP, et al. Pancreatic duct abnormalities in gall stones disease: an endoscopic retrograde cholangiopancreatographic study. Gut. 1990;31:1073-1075.
Sarles H. Proposal adopted unanimously by the participants of the symposium of acute pancreatitis in Marseille, 1963. Bibl Gastroenterol. 1965;7:7-8.
Sarles H, et al. The classification of pancreatitis and definition of pancreatic disease. Digestion. 1989;43:234-236.
Sarner M, Cotton PB. Classification of pancreatitis. Gut. 1984;25:756-759.
Singer MV, et al. Revised classification of pancreatitis: report of the Second International Symposium on the classification of pancreatitis in Marseille, France, March 28-30, 1984. Gastroenterology. 1985;89:683-690.
Ramesh H. Proposal for a new grading system for chronic pancreatitis: the ABC system. J Clin Gastroenterol. 2002;35:67-70.
Schneider A, Lohr JM, Singer MV. The M-ANNHEIM classification of chronic pancreatitis: introduction of a unifying classification system based on a review of previous classification of the disease. J Gastroenterol. 2007;42:101-119.