Complementary and Alternative Medicine
• Complementary and alternative medicine encompasses various approaches to all aspects of medical assessment and management that are not commonly or extensively applied or recommended by conventional western medical practitioners.
• Complementary and alternative medicine approaches are frequently used by patients, but patients often do not discuss their use of these approaches with their health care team.
• Some products purported to be dietary supplements may be unsafe for patients with cancer because of adverse effects of the natural components, adverse interactions with medications, contamination with toxic compounds, or adulteration with drugs.
• St. John’s wort and potentially various other herbal products can significantly alter the pharmacokinetics of certain chemotherapy drugs, such as irinotecan.
• High-dose alpha-tocopherol (i.e., 400 IU per day) should not be given to patients with head and neck cancer who are receiving radiation therapy with curative intent.
• Acupuncture can be useful for managing cancer pain and postsurgical pain.
• Exercise can be an effective intervention for preventing and managing cancer-related fatigue.
• Yoga may be effective in preventing or managing fatigue and improving sleep and quality of life in patients with cancer.
• Acupuncture, ginger, hypnosis, relaxation therapy, and imagery can provide additional relief from chemotherapy-induced nausea and vomiting in patients receiving standard antiemetic regimens.
• High-dose oral glutamine and intravenous glutathione may decrease the frequency of neuropathy from drugs containing paclitaxel and platinum.
• Preliminary evidence indicates that acupuncture may effectively decrease hot flash symptomatology in women undergoing treatment for breast cancer and in men receiving androgen-deprivation therapy for prostate cancer.
• Aloe vera or honey taken orally and intravenously administered glutamine may decrease the incidence or severity of chemotherapy-induced oral mucositis.
• Several interventions have been found useful for stress reduction and to increase the quality of life among patients with cancer, including music, meditation, relaxation therapy, and imagery therapy.
Introduction
Complementary and alternative medicine (CAM) is defined by the National Center for Complementary and Alternative Medicine (NCCAM), a component of the U.S. National Institutes of Health (NIH), as “a group of diverse medical and health care systems, practices, and products that are not generally considered part of conventional medicine,” with “conventional medicine” defined as “…medicine as practiced by holders of M.D. (medical doctor) and D.O. (doctor of osteopathic medicine) degrees and by allied health professionals, such as physical therapists, psychologists, and registered nurses.”1 The World Health Organization defines CAM as “a broad set of health care practices that are not part of that country’s own tradition and are not integrated into the dominant health care system.”2
It is generally accepted that complementary therapies are those that are used along with conventional medical care for a given condition and alternative therapies are those that are used independent of conventional care. Box 33-1 provides a categorization of CAM intervention and therapeutic systems using a modification of schema developed by NCCAM.
A recent, large, national, population-based survey showed that 43.3% of U.S. patients with cancer had used at least one CAM intervention in the preceding 12 months.3 Evidence suggests that the use of such approaches, even those with the greatest theoretical potential for interaction with conventional therapy, is often not disclosed to the treating oncologist.4,5
Integrative medicine is defined by the Consortium of Academic Health Centers for Integrative Medicine as “an approach to the practice of medicine that makes use of the best-available evidence taking into account the whole person (body, mind, and spirit), including all aspects of lifestyle. It emphasizes the therapeutic relationship and makes use of both conventional and complementary/alternative approaches.”6
Nutritional Therapeutics
Patients with cancer often have unmet needs for dietary advice.7,8 Various small studies have shown that nutritional counseling and education improves outcomes (i.e., quality of life and/or survival) for patients with head and neck,9 colorectal,10 and lung cancer.11
Dietary Supplements
The term “dietary supplement” refers to “a product (other than tobacco) intended to supplement the diet that bears or contains one or more of the following dietary ingredients: a vitamin; a mineral; an herb or other botanical; an amino acid; a dietary substance for use by man to supplement the diet by increasing the total dietary intake.”12
Contamination and Adulteration
The FDA and various state and local drug regulatory authorities and academic researchers frequently find that dietary supplements that are sold in U.S. stores or are available through the Internet are contaminated with heavy metals13 or adulterated with prescription medications.14 For example, PC-SPES was an herbal product manufactured and distributed by a U.S.-based company and advertised as preserving prostate health, but it was extensively used by patients with prostate cancer. PC-SPES was also being investigated as a potential prostate cancer therapy until the product was voluntarily withdrawn from the market in 2005 after the California Department of Health Services and the FDA published warnings indicating that several production lots were found to contain various amounts of warfarin and diethylstilbesterol.15
Adverse Effects
Adverse effects of a dietary supplement may be due to the labeled contents in the supplement or a contaminant or adulterant. In the case of herbal supplements, instances have occurred of the substitution of a different herb for one listed on the label, sometimes because of misidentification of the plant. The Natural Medicine Comprehensive Database16 and Micromedex17 contain referenced information about the adverse effects of a large number of dietary supplement components. The following sections provide examples of some adverse effects that are relevant to patients with cancer.
Chaparral (Larrea divaricata Coville)
The leaves of chaparral, a desert shrub also known as the creosote bush, are reportedly used in Native American medicine.18 The plant contains nordihydroguaiaretic acid, a compound that is under investigation as an anticancer agent.19 Renal and hepatic toxicity have been associated with chronic use of products that contain chaparral.22–22
Kava (Piper methysticum)
Kava is an herbal remedy generally recommended for the treatment of anxiety or to improve sleep.23 Two randomized, controlled trials have confirmed evidence of its anxiolytic activity.24 However, several cases of severe liver toxicity associated with the consumption of products labeled as containing extracts of kava have been reported. Consequently, kava is banned in several European countries,25 and the U.S. FDA has issued a consumer advisory warning of the potential risk of hepatic toxicity from kava ingestion26; however, products containing kava may still be legally sold in the United States as dietary supplements.27
Laetrile
Laetrile, also known as amygdalin, is a cyanogenic glucoside found in the pits of many fruits, in raw nuts, and in other plants such as lima beans, clover, and sorghum.28,29 Although it is frequently called vitamin B17 in the lay literature, amygdalin is not recognized as a vitamin by the Committee on Nomenclature of the American Institute of Nutrition. Laetrile has been given orally and intravenously with different pharmacokinetics and toxicity profiles. Laetrile became a popular alternative cancer therapy in the 1950s and remained so through the 1980s. Currently, its sale in the United States is banned by the FDA; however, products labeled as containing laetrile can easily be purchased via the Internet. When orally ingested, laetrile can be hydrolyzed by intestinal beta-glucosidase to produce hydrogen cyanide, benzaldehyde, and glucose. The enzymatic activity of beta-glucosidase, and thus the rate of production of cyanide, can be increased under various conditions, including the presence of vitamin C.30 Signs and symptoms of cyanide poisoning have been reported both from individual patients with cancer who ingested products containing laetrile31,32 and from patients enrolled in clinical trials of oral laetrile.33,34
Cesium Chloride
Cesium chloride has been promoted in books and on the Internet as a cancer therapy. No clinical trials of the use of cesium chloride have been published, but several case reports have described patients with cancer in whom QT prolongation and torsades de pointes ventricular tachycardia developed after they ingested products containing cesium chloride.35–40 In some of these reported episodes of toxicity, the patients also demonstrated hypokalemia and/or hypomagnesemia. In one case, the patient was successfully treated with 4 weeks of oral Prussian blue.35
Aloe Vera
Leaves from aloe vera, a fleshy, cactus-like plant, contain a clear gel that is often used to soothe minor skin irritations, although a systematic review of the research failed to find firm evidence for a preventive effect with regard to radiation-induced skin reactions.41 Aloe latex is an extract of the inside of the outer lining of the leaves and is approved by the German Commission E for treating constipation.42 The gel can also be made into a juice that has been promoted as a cancer cure. In a male patient with HER2+ breast cancer who was taking capecitabine, trastuzumab, and 1 L a day of aloe vera juice for 2 weeks, severe hypokalemia developed that responded to potassium supplementation after ingestion of the aloe juice was stopped.43 In clinical trials of smaller doses of aloe juice (i.e., 10 mL taken three times a day), hypokalemia has not been found to be an associated adverse effect.44,45
Licorice (Glycyrrhiza species)
The root of the licorice plant has been used in TCM formulations for centuries. The now-banned herbal product PC-SPES reportedly contained Glycyrrhiza glabra,46 as do some herbal products currently used by patients with prostate cancer. Glycyrrhizic acid, a component of licorice, inhibits 11β-hydroxysteroid dehydrogenase, thus resulting in mineralocorticoid excess, which can cause hypertension and hypokalemia.47 Severe consequences of hypokalemia, including paralysis and torsades de pointes ventricular arrhythmia, have been reported in patients taking products that contain licorice.48,49
Herbs Containing Aristolochic Acid
Aristolochic acid, a nephrotoxin that also may induce urothelial tumors, is found in herbs of the Aristolochiaceae family, as well as some from Bragantia and Asarum genera.50 Some of these herbs are used in TCM (e.g., guan mu tong [Caulis aristolochiae manshuriensis], which is used for dysmenorrhea and breast disorders), and they are used in some weight-loss formulas found in Europe. Case reports have been published of patients in the United States who have experienced toxicities (e.g., renal failure and urothelial cancer) after ingesting supplements derived from these plants.51 The FDA has found that some botanical products labeled as containing “Aristolochia,” “Bragantia,” or “Asarum” contain aristolochic acid.52
Adverse Interactions between Dietary Supplements and Drugs
Cytochrome P450 Inducers and Inhibitors
The enzymes of the cytochrome P450 (CYP450) superfamily are responsible for the activation or inactivation of the vast majority of drugs currently in use.53 Drugs or other exogenous chemicals ingested in the diet or via dietary supplements can affect the activity of CYP450 enzymes to a sufficient degree to meaningfully change the clinical effectiveness or toxicity of various chemotherapy drugs. Table 33-1 lists some herbs that have been shown to affect various CYP450 enzyme activities in humans and other herbs for which the effects on CYP450 enzymes have been predominantly determined by in vitro or animal studies, and thus are of uncertain clinical significance. Other herbs interfere with drug PK via effects on the activity of the P-glycoprotein multidrug transporter (e.g., curcumin) or other adenosine triphosphate–binding cassette drug transporters (e.g., genistein).54
Table 33-1
| Herb | Drug | Affect | Source |
| St. John’s wort | Irinotecan | Increases enzyme activity and decreases AUC of active metabolite SN38 | Clinical trial55 |
| St. John’s wort | Imatinib | Increases clearance and decreases AUC of drug | Clinical trial56 |
| Green tea | Sunitinib | Decreases drug absorption | Animal study and case report59 |
| Ginkgo biloba | Teniposide | May decrease circulating concentration | Clinical trial (theoretical interaction based on known effects of herb on a similarly metabolized drug)183 |
| Black cohosh | Substrates of CYP2D6 | Increases drug metabolism | Clinical trial184 |
| Garlic | Saquinavir | Decreases serum levels | Clinical trial185 |
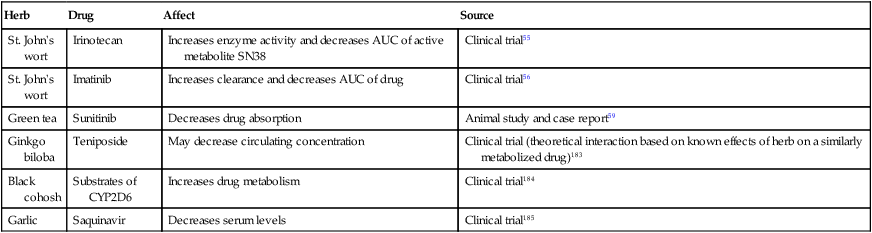
St. John’s Wort
A classic example of an herb affecting drug PK is St. John’s wort. Plasma levels of the active metabolite of irinotecan, SN-38, were decreased by 42% in five patients receiving irinotecan and a commonly used dose of St. John’s wort (300 mg three times daily), apparently because of induction of the CYP3A4 isoform.55 Imatinib is also a CYP3A4 substrate, and a study using the same dosing schedule of St. John’s wort found a 43% increase in the drug’s clearance and a 30% decrease in the area under the curve of the plasma concentration.56
Green Tea Extract and Epigallocatechin Gallate
Green tea and its polyphenols such as epigallocatechin gallate (EGCG) can affect drug metabolism and effectiveness via actions on either PK or PD. A PD-related dietary supplement–drug interaction has been noted in preclinical studies of the combination of green tea and bortezomib. EGCG blocked bortezomib’s anticancer effect on human multiple myeloma and glioblastoma cell lines in vitro by binding to the boronic acid component of the drug; this action occurred at concentrations achievable in the blood of humans after ingesting dietary supplements containing green tea.57 In addition, the same research group reported that intragastric EGCG administration (50 mg/kg) completely abrogated bortezomib-induced apoptosis in plasmacytoma xenografts in nude mice. Another animal study also demonstrated that the antitumor activity of bortezomib on human prostate cancer xenografts in severe combined immune deficiency mice was completely eliminated with the very high plasma concentrations obtained after intravenous EGCG administration but not with the lower concentrations resulting from subcutaneous administration.58 No human studies have been performed that directly address the clinical significance of this interaction.
A published case report describes a Chinese patient with metastatic renal cell carcinoma who was being treated with sunitinib and noted aggravated symptoms from a retro-orbital ocular metastasis at times when he increased the amount of green tea that he drank.59 An animal study of the effects of coadministration of sunitinib and EGCG revealed the formation of a precipitate in the stomach, resulting in lowered sunitinib absorption.
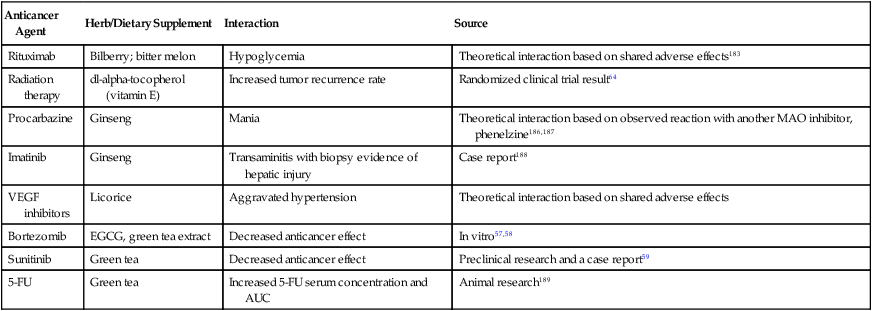
Table 33-2 lists several other herb-drug interactions of potential relevance when advising and managing patients with cancer.
Table 33-2
Adverse Interactions between Dietary Supplements and Cancer Therapies
| Anticancer Agent | Herb/Dietary Supplement | Interaction | Source |
| Rituximab | Bilberry; bitter melon | Hypoglycemia | Theoretical interaction based on shared adverse effects183 |
| Radiation therapy | dl-alpha-tocopherol (vitamin E) | Increased tumor recurrence rate | Randomized clinical trial result64 |
| Procarbazine | Ginseng | Mania | Theoretical interaction based on observed reaction with another MAO inhibitor, phenelzine186,187 |
| Imatinib | Ginseng | Transaminitis with biopsy evidence of hepatic injury | Case report188 |
| VEGF inhibitors | Licorice | Aggravated hypertension | Theoretical interaction based on shared adverse effects |
| Bortezomib | EGCG, green tea extract | Decreased anticancer effect | In vitro57,58 |
| Sunitinib | Green tea | Decreased anticancer effect | Preclinical research and a case report59 |
| 5-FU | Green tea | Increased 5-FU serum concentration and AUC | Animal research189 |
Antioxidants
Several different nutrients (e.g., vitamin C, vitamin E, and selenium) and other bioactive food components (e.g., glutathione) can act as electron donors in vivo and thus are considered antioxidants. Various chemotherapy agents and radiation therapy induce the production of chemically reactive free radicals (e.g., hydrogen peroxide, ⋅OH− and superoxide, O2⋅−) that can damage a variety of cellular components (e.g., DNA and lipid membranes). Antioxidants can act as free radical scavengers and thus could potentially alter both the therapeutic and adverse effects of cancer therapies that produce free radicals. Consequently, the risk-benefit assessment for the concurrent use of high-dose antioxidant supplements during chemotherapy or radiation therapy remains controversial. Specific clinical trial results, however, have generally failed to show a detrimental effect of antioxidants on chemotherapy or radiation therapy effectiveness,60 although there is at least one notable exception.
Vitamin E
The term “vitamin E” can refer to any of eight compounds (four tocopherols and four tocotrienols) with related chemical structures and antioxidant properties, or a mixture of them. From among the individual vitamin E compounds, only alpha-tocopherol has been studied for its potential to prevent chemotherapy- or radiation therapy–induced adverse effects in humans. Alpha-tocopherol at a dose of 400 IU per day has been found to decrease the acute toxicity of radiation for patients receiving therapy for head and neck cancer.61,62 However, in the largest randomized study thus far reported, the patients who received the alpha-tocopherol supplements also experienced a higher risk of recurrence of the tumor, more frequently experienced the development of new primary tumors while receiving the vitamin E, and had a poorer mean overall survival.63,64
Anticoagulant Interactions
Various dietary supplements are suspected of having independent anticoagulant activity, although the evidence is largely from case reports. Several dietary supplements have been found to inhibit platelet aggregation to varying degrees in vitro (see Box 33-2), and human trials have demonstrated that vitamin E can augment aspirin’s antiplatelet affects.65 Table 33-3 provides some examples of supplements reported to interact with warfarin.
Table 33-3
Supplements that May Interact with Warfarin
| Supplement | Action | Source |
| CoQ10 | Decreased warfarin effect | Animal studies and in vitro human microsomes studies |
| Dan shen (Salvia miltiorrhiza) | Increased warfarin effect | Animal study |
| Dong quai (Angelica sinensis) | Increased warfarin effect | Animal study |
| Fenugreek | Increased warfarin effect | Clinical case report |
| Green tea | Decreased warfarin effect | Clinical case report |
Cancer Treatment
Breast Cancer
Nutrition and Physical Activity
Low-Fat, High-Fruit, and Vegetable Diet
Two prospective studies have addressed the potential impact of dietary modification, and to a lesser extent physical activity, on the survival of women with early-stage breast cancer. The Women’s Intervention Nutrition Study randomly assigned 2437 women with stage I to III breast cancer and who had completed their adjuvant chemotherapy, when given, to either a diet low in fat (15% of calories) and high in fruits and vegetables or a control group that received general dietary advice from a dietician.66 After a median of 60 months of follow-up, women following the low-fat diet experienced a statistically significant 24% reduced risk of relapse. The primary end point of relapse-free survival, however, was not statistically different (P = .07) for the entire study group, although women with estrogen receptor–negative tumors did have a significantly longer relapse-free survival (P = .03). Another similarly designed and sized study, the Women’s Healthy Eating and Living trial, failed to find a significant difference in recurrence rate for women on the low-fat diet, although a better recurrence rate was seen in the subgroup of women who adhered to the low-fat diet and undertook a greater degree of physical activity.67,68 Another notable difference between the two trials was that women following the low-fat diet in the Women’s Intervention Nutrition Study trial lost weight, whereas women following the investigational diet on the Women’s Healthy Eating and Living trial did not lose weight.
Soy
Various foods such as legumes contain phytoestrogens; soy is particularly abundant in these compounds and has drawn the most attention regarding its potential to produce estrogenic adverse effects. Much speculation has occurred about the risk of soy intake by women with breast cancers that express estrogen receptors and, largely because of preclinical research findings about the effects of the phytoestrogens in soy, such women frequently receive recommendations to avoid eating soy products. However, an analysis of the pooled data from two large U.S. trials and one trial from China, with a total of more than 9500 women, found a nonsignificant reduced risk of breast cancer–specific mortality and a statistically significant reduced risk of breast cancer recurrence for women who consumed >10 mg of soy isoflavones per day after their cancer diagnosis. 69
Mind-Body Approaches
Studies in which animals bearing implanted tumors are exposed to stressful conditions thought to mimic psychological stress in humans often result in increased tumor growth and metastases rates and diminished responsiveness of the tumor to chemotherapy. However, the potential for a mind-body intervention to affect the course of cancer progression or treatment response in humans has been very controversial, and few relevant experimental data are available. Several studies of support group interventions that included assessments of patient survival have been performed in patients who have cancer with conflicting results. Specifically regarding metastatic breast cancer, at least six randomized trials have been reported,70–74 although only the first study yielded positive results for survival.70 This first study found that patients who received the combined support group and hypnosis interventions experienced a longer median survival than did those in the control group.70 However, three subsequent studies utilizing a very similar intervention failed to confirm this finding, showing no benefit in survival for the patients receiving the expressive-support therapy.71,73,74
Only two studies have specifically explored the effects of psychosocial support or stress-reduction approaches on recurrence or survival in women with early-stage breast cancer. The studies utilized different support interventions, and the study that used a stress-reduction intervention (26 sessions over 12 months) found a statistically significant benefit both for risk of recurrence and survival, although the number of both events was very small.75 The other study utilized cognitive-existential group therapy weekly (20 weekly sessions) and found no effect on recurrence or survival.76
Pancreatic Cancer
Curcumin
In addition to many chemotherapy agents, a few dietary compounds have been paired with gemcitabine in pancreatic cancer treatment trials. Oral curcumin at a dose of 8 g a day showed signs of single-agent activity in a phase 2 trial; however, the same dose was not as well tolerated when given with gemcitabine.81,82 A nanoparticle formulation of curcumin for intravenous administration has been produced and may prove to be better tolerated.83,84
Kelley-Gonzalez Regimen
Dr. William D. Kelley, a dentist from Texas, developed a complex regimen based on the treatment approach of an earlier alternative medicine physician, Dr. Max Gerson, and promoted it as a cancer therapy. A main component of this approach is the use of oral pancreatic enzymes, but the regimen also includes (1) vitamin and mineral supplementation, (2) concentrates of raw beef organs and glands in pill form, (3) other digestive aids, including hydrochloric acid and bile salts, and (4) a “detoxification” regimen including frequent coffee enemas.85 An initial uncontrolled study of this regimen yielded promising survival results for the subset of patients with unresectable pancreatic cancer who had the best compliance with the regimen.86 However, a subsequent prospective, nonrandomized cohort study of patients with unresectable pancreatic cancer found an inferior survival for patients who self-selected to receive the Kelly-Gonzalez therapy compared with patients treated with various chemotherapy regimens containing gemcitabine.87
Colorectal Cancer
Exercise
As with breast cancer, observational studies have demonstrated a strong association between the degree of physical activity and outcomes of patients with early-stage colorectal cancer. Two such studies, one in women with stage I to III colorectal cancer and the other of men and women with stage III colorectal cancer, both showed statistically significant improvements with moderate to strenuous physical activity for both risk of recurrence and survival.88,89 Several relatively small trials are underway that are designed primarily to assess the potential benefit of increased physical activity on quality of life, functional measures, or biological end points, but none yet focusing on survival.
Prostate Cancer
Lifestyle Modification during Active Surveillance
The Prostate Cancer Lifestyle Trial was a 1-year randomized controlled trial of 93 patients with early-stage prostate cancer (Gleason score <7; prostate-specific antigen, 4-10 ng/mL) who were undergoing active surveillance. The experimental group received a low-fat, plant-based (vegan) diet supplemented with soy, fish oil, vitamin E, selenium, and vitamin C, along with a regimen of moderate aerobic exercise (walking 30 minutes, 6 days weekly) and stress management (gentle yoga-based stretching, breathing, meditation, imagery, and progressive relaxation for 60 minutes daily) and 1-hour weekly group support sessions to enhance adherence to the program. Control patients received usual care. At the end of the 1-year program, patients in the experimental group had had a significant reduction in prostate-specific antigen level and fewer prostate cancer–related clinical events compared with control patients.90 After 2 years of follow-up, fewer patients in the experimental group experienced signs of progression that required medical or surgical management (2 of 43 [5%] vs. 13 of 49 [27%], P = .05).91
Symptom/Adverse-Effect Management and Quality of Life
Complementary therapies have gained greatest acceptance, both in research and practice, for the management of cancer symptoms and treatment adverse effects and for their potential to improve overall quality of life. This section presents some approaches that are available and in use to varying degrees in North America. Many of these approaches may affect multiple complaints simultaneously, so-called symptom clusters, and thus present the potential for efficient, well-tolerated management.92,93 However, various factors limit the interpretation of the research findings, lessening the utility of the evidence base for each of these practices. Many of these interventions are poorly standardized, if at all, and thus variables that are carefully controlled in a good-quality clinical trial (e.g., product quality) may not be so carefully controlled in general practice. For some dietary supplements, particularly herbs, the active ingredient(s) may not be known.
Pain
Acupuncture
Acupuncture has demonstrated analgesic activity in animal models of cancer pain through studies in at least two independent laboratories.94,95 These studies have also identified effects on various mediators of pain sensation, including substance P, endorphins, and interleukin 1–beta. Other work has supported a role for effects of vasopressin secretion.94,96
Acupuncture, acupressure, and acustimulation (i.e., electrical stimulation of acupuncture points) have been used and studied for their effects in relieving various types of pain. However, very few well-designed clinical trials of these modalities have been conducted in patients with cancer-related pain. One randomized, controlled clinical trial of auricular acupuncture was performed in patients whose pain was not adequately controlled with analgesic medications. In this study, patients who received electroacupuncture applied to the proposed active points had significantly less pain than did patients in the placebo treatment groups.97
Postsurgical Pain
One small, nonrandomized study reported greater pain relief and an increased range of motion in patients treated with acupuncture after breast cancer surgery and axillary lymph node dissection.98 A randomized trial comparing weekly acupuncture versus usual care in patients after surgical resection for head and neck cancer found significant improvements in pain and dysfunction among patients receiving acupuncture.99
Imagery
The exploration of guided imagery as a potential therapeutic modality in the management of cancer pain has been very limited; only a few small studies have been conducted, with no two exploring the same clinical situation. A pilot study of progressive muscle relaxation and “analgesic imagery” showed some positive effects for each among hospitalized patients with pain related to cancer.100 A randomized, controlled trial using relaxation, imagery, and cognitive-behavior training found lower mucositis pain scores in patients undergoing bone marrow transplantation.101 Another study in patients with pain due to metastatic breast cancer failed to demonstrate an effect of the combination of relaxation, visualization, and cognitive coping skills training on pain intensity or its psychological effect.102
Reiki
Reiki is a healing system based on Tibetan scriptures but developed in Japan. The therapy is provided by practitioners called Reiki masters and is a form of energy therapy that involves placing one’s hands near or on portions of the patient’s body while maintaining a specific therapeutic intention. This intervention has been studied in only a few clinical trials. A randomized phase 2 study demonstrated improved pain control in patients with advanced cancer who received Reiki therapy compared with a resting control.103
Aromatase Inhibitor–Induced Arthralgia
Acupuncture
A small randomized, blinded study of acupuncture for aromatase-related joint symptoms found that true acupuncture given for 30 minutes twice weekly for 6 weeks was significantly more effective than sham acupuncture.104 The research base for the Southwest Oncology Group Community Clinical Oncology Program has recently initiated a follow-up study using the same acupuncture approach.105 However, another multicenter trial was stopped early for futility based on interim results.106
Vitamin D
Although low serum levels of vitamin D have not consistently been associated with the risk of developing aromatase inhibitor–induced musculoskeletal symptoms, recent studies have shown promising results from vitamin D supplementation.107 A randomized, placebo-controlled trial in woman with anastrozole-induced musculoskeletal symptoms demonstrated a significant benefit with high-dose oral vitamin D2 supplementation (i.e., 50,000 IU weekly for varying periods), while simultaneously contributing to diminished bone loss.108 A similar but less intense strategy was employed in a study using high-dose vitamin D3 supplementation to attempt to prevent musculoskeletal symptoms in women about to start taking letrozole. Beneficial effects were seen in the women having the greatest improvement in 25-hydroxyvitamin D levels.109
Cachexia
Nutritional Therapeutics
The ingestion of high doses of fish oil, or the omega-3 fatty acids derived from it, has been proposed to produce salutary effects in patients with various conditions. Results from one randomized controlled trial demonstrated improvement in appetite and lean body mass in patients with advanced pancreatic cancer.110 Another trial, however, failed to demonstrate any improvement in appetite, nutritional status, caloric intake, or other related symptoms in patients with other types of advanced cancer.111 Fish oil generally is well tolerated at doses up to 3 g per day. Higher doses can cause eructation, halitosis, heartburn, gastrointestinal upset, nausea, and loose stools.112
Fatigue
Cancer-related fatigue is the perception of unusual tiredness that varies in pattern of severity and has a negative impact on the ability to function in patients who have or have had cancer.113 Its etiology is likely multifactorial, but recent work has found an association with inflammation.114
Acupuncture
Three randomized controlled trials have been reported, all of which used some acupuncture points in common, but no two of the studies used exactly the same protocol; all three trials used sham acupuncture controls. One study116 attempted to prevent fatigue in patients receiving external radiation therapy and failed to show a statistically significant advantage of the true acupuncture intervention. The other two trials117,118 attempted to ameliorate chronic fatigue after completion of chemotherapy, but only one trial117 showed an advantage for the true acupuncture intervention.
Exercise
Various exercise approaches have been studied in several different patient populations at different points in the continuum of care. A meta-analysis of 18 randomized controlled trials of patients with various cancer types, although mostly breast cancer and prostate cancer, has shown that supervised exercise is more effective than unsupervised, home-based exercise; however, even home-based exercise produced a significant benefit versus usual care or a placebo stretching program.119 A prospective clinical trial assessing the potential benefits of enhanced physical activity during cancer treatment on fatigue and quality of life of patients with breast and colon cancer is underway.120
Yoga
Yoga may be most accurately defined as a system of physical, mental, and spiritual development that originated in ancient India, but in the modern international context, the term includes many variations on the traditional practices (e.g., restorative yoga), as well as practices, both ancient and recent, that developed in other countries (e.g., Tibetan yoga). The major components of the many systems of yoga include physical postures, breath control, and meditation. A metaanalysis of yoga’s effects on cancer-related fatigue has synthesized the results of several trials.121 The type of yoga intervention and the length and frequency was different in each trial. The pooled results of all studies (n = 362) found that yoga compared with control was associated with a significantly greater improvement in fatigue. Another recent large multicenter randomized study (n = 410) assessed the effect of the University of Rochester’s Yoga for Cancer Survivors program on cancer survivors without metastatic disease who also had fatigue and moderate or greater sleep disruption. On average, the patients in the yoga intervention group experienced improved sleep quality, fatigue, and quality of life.122
Energy Therapies
Various energy therapy approaches have been prospectively studied as potential fatigue therapies with somewhat mixed results. Two randomized controlled trials in patients with cancer have demonstrated the potential of “healing touch” to improve fatigue and other physical and psychological adverse effects of chemotherapy.123,124 A study of “therapeutic touch” found significant improvement over relaxation or usual care both for fatigue and quality of life, and a recent study of an approach known as “energy chelation therapy” showed improvement in patients’ fatigue for both the active and sham treatment groups compared with an untreated control group.125
Herbs and Other Dietary Supplements
Ginseng
Both Asian ginseng (Panax ginseng) and American ginseng (Panax quinquefolius) have been studied for their potential effects on cancer-related fatigue, yielding positive results in small single-arm and randomized trials. These plants are classified by herbalists as “adaptogens” because of the belief, supported by some research results, that their use can help improve a person’s ability to better adapt to physical stress. Both types of ginseng contain several bioactive compounds, including polysaccharides and triterpene saponins, known as ginsenosides. The North Central Cancer Treatment Group recently completed a multicenter, randomized, placebo-controlled trial in which American ginseng, standardized to contain 5% ginsenoside, at a dose of 2000 mg per day in two divided doses, significantly improved a validated measure of cancer-related fatigue in patients with cancer who were undergoing, or had completed, treatment with curative intent.126 A randomized, placebo-controlled trial of Asian ginseng in patients undergoing chemotherapy or radiation therapy is underway at MD Anderson Cancer Center.
Guarana
The caffeine-containing herb guarana was tested against placebo in a small study of patients with breast cancer who were experiencing fatigue while undergoing chemotherapy and was found to be effective.127 Apparently, no randomized controlled trials of caffeine alone for cancer-related fatigue have been reported.
L-Carnitine
Preliminary evidence indicated that correction of carnitine deficiency in adult patients with cancer who experienced fatigue led to improvement of the symptom.128 However, a larger multicenter trial failed to find a significant improvement in a more heterogeneous group of patients with a diagnosis of invasive cancer and fatigue but who were not required to have carnitine deficiency prior to study entry.129
Sleep
Yoga
A randomized trial of Tibetan yoga versus wait-list control in patients with lymphoma showed improvements in sleep quality, sleep latency, sleep duration, and use of sleep medications.130 More recently, a multicenter, randomized, controlled trial demonstrated that a program utilizing yoga postures (asanas), breathing exercises (pranayama), and meditation could decrease the use of sleep medications among patients with cancer who experienced moderate or greater sleep disruption.122
Nausea and Vomiting
Acupuncture and Acupressure
After a systematic review of the literature, the NIH Consensus Development Panel on Acupuncture in 1997 found “promising results” had emerged suggesting efficacy in managing chemotherapy-induced nausea.132 Among the studies reviewed by the panel were three randomized controlled trials, all of which evaluated the effects of electrical stimulation at the P6 (Neiguan) acupuncture point on the volar surface of the wrist with or without costimulation at other acupuncture sites, and all of which included only adult patients with cancer as subjects, with control groups receiving antiemetic regimens that did not include a 5-hydroxytryptamine (5-HT) receptor antagonist. Several subsequent studies have continued to demonstrate the effectiveness of acupuncture for the prevention of chemotherapy-induced nausea in patients already receiving a 5-HT receptor antagonist, in children, and using other acupuncture points (e.g., ST35, known as “Zusanli”).
Most studies thus far indicate that acupuncture is primarily effective for the prevention of acute chemotherapy-induced vomiting and less effective against acute nausea or delayed nausea. For example, a multicenter, randomized controlled trial of acustimulation wrist bands applied to the P6 point did not show a significant effect on delayed nausea of women receiving chemotherapy for breast cancer.133
Only one randomized controlled trial of acupuncture for the prevention of radiation-induced nausea and vomiting has been reported in full article form, and it showed decreased nausea and vomiting in both the true and sham acupuncture groups.134
Ginger
A large randomized, double-blind, placebo-controlled trial has demonstrated an additive antiemetic effect of ginger extract (either 0.5 or 1.0 g taken orally twice daily) to a 5HT receptor antagonist for the prevention of acute chemotherapy-induced nausea.135
A small randomized, double-blind, placebo-controlled trial found improved measures of nausea and vomiting in children and young adults receiving a weight-adjusted dose of oral encapsulated ginger powder (up to 2 g per day) while undergoing cisplatin and doxorubicin therapy for bone sarcomas. Both acute and delayed nausea and vomiting were improved with this regimen.136
Hypnosis
Hypnosis, including self-hypnosis, has been studied in clinical trials of both pediatric and adult patients with cancer for a variety of indications. At least one small pilot study137 and three small randomized controlled trials101,138,139 have demonstrated efficacy for hypnosis as a treatment of anticipatory or chemotherapy-induced nausea and vomiting in patients with cancer. Other less-studied mind-body approaches, such as cognitive distraction approaches, have also shown positive effects in randomized controlled trials.140
Relaxation and Imagery
Relaxation and or imagery interventions have been studied in at least seven randomized clinical trials against a control, with anticipatory or chemotherapy-induced nausea and vomiting as a predetermined study end point.141–147 In all of these trials the relaxation/imagery group fared significantly better than the control group for at least one relevant outcome measure.
Neuropathy
Acupuncture
Herbs and Dietary Compounds
Glutathione
Glutathione is an abundant tripeptide that acts as the primary endogenous, intracellular antioxidant for mammalian cells. Exogenously administered glutathione has been reproducibly shown to protect against certain chemotherapy-related toxicities. Several small randomized controlled trials have demonstrated that intravenous glutathione given in doses of 1.5 to 3 g/m2 over 15 to 20 minutes prior to cisplatin or oxaliplatin administration resulted in lower rates of clinically significant neuropathy without compromising the anticancer effect of the chemotherapy agent.60
Vitamin E
Doses of either 300 mg daily or twice a day of dl-alpha-tocopherol have been found to be effective in decreasing the frequency of development of neuropathic symptoms in patients being treated with chemotherapy regimens containing cisplatin.151,152 However, the largest randomized, placebo-controlled clinical trial conducted thus far failed to show a benefit of alpha-tocopherol on the development of neuropathy in a mixed group of patients, some receiving taxanes and others receiving various platinum-based chemotherapeutic agents.153
Hot Flashes
Acupuncture
Acupuncture given twice a week for 30 minutes per session has been shown to decrease hot flash symptomatology, both in women with breast cancer and men with prostate cancer who were receiving androgen-deprivation therapy.154,155 The degree of effectiveness appears to be at least equivalent to that of venlafaxine.155 Multiple acupuncture points (e.g., 9 to 20 points) are generally needled simultaneously in each treatment session.
Hypnosis
Very little research has been reported on the use of hypnosis for the treatment or prevention of hot flashes. A pilot study in which hypnosis was compared with a no-treatment control suggested a beneficial effect for hypnosis,156 and a larger randomized trial with an attention control is underway.157
Phytoestrogens
No significant effect was noted in a small randomized, placebo-controlled trial of 20 g of soy protein containing 160 mg total isoflavones on vasomotor symptoms in men with prostate cancer who were undergoing androgen deprivation.160 In three randomized, placebo-controlled trials of women with early-stage breast cancer, various soy isoflavone supplements in doses ranging from 70 to 150 mg per day failed to demonstrate a significant benefit on menopausal symptoms.163–163 A systematic review in 2007 found five trials with data suitable for pooling for metaanalysis.164 No significant difference was detected in the frequency of hot flashes between a red clover extract and placebo.
Black Cohosh
Despite some promising data from a single-arm pilot study, the two randomized, placebo-controlled trials of black cohosh supplements (20 mg twice a day in one and dose not given in the other) have failed to demonstrate that the black cohosh supplement provided any greater relief from hot flashes than did placebo.167–167
Mucositis
Various CAM approaches have been studied in randomized controlled trials for their potential preventive or therapeutic effects on chemotherapy- or radiation-induced mucositis in patients with cancer. At least three of these (aloe vera, intravenous glutamine, and honey) have had more than one trial with statistically significant findings demonstrating a benefit compared with either placebo or no treatment.168 Aloe vera gel (not the latex component) has also been demonstrated in at least one randomized controlled trial to improve symptomatology of ulcerative colitis169 and has been proposed by some herbalists as a therapy for radiation-induced rectal mucositis.
Homeopathy
Traumeel S is a multicomponent, over-the-counter product containing a mixture of low-concentration botanical extracts. It is produced following homeopathic principles and has been traditionally recommended to treat inflammatory conditions. Traumeel S was studied in a small pilot trial to attempt to prevent and treat oral mucositis in pediatric patients undergoing bone marrow transplantation, yielding positive results.170 However, a follow-up multicenter, randomized controlled study by the Children’s Oncology Group failed to show a significant benefit for Traumeel S in the same patient population.171
Stress Reduction and Quality of Life
Aromatherapy
Aromatherapy, with and without massage, has been studied in several randomized controlled trials of patients with cancer.172–175 In these trials, a weekly aromatherapy massage intervention often did demonstrate improved symptoms during the course of treatment. However, in one study in which patients were undergoing radiotherapy, a statistically significant advantage was actually found for the control group over the aromatherapy group.174
Music
Music may be used with therapeutic intent either to create a distraction from the stress-inducing cancer treatment experience or as a means to promote a positive, adaptive response. The term “music therapy” has generally been applied to the use of a music intervention by a trained music therapist and incorporating an individualized musical experience. A metaanalysis of randomized controlled trials of music interventions used with patients with cancer found significantly lower anxiety levels and improved quality of life in patients receiving the music intervention.176
Meditation
Meditation is a component of several so-called “mind-body” approaches, as well as some exercise therapies, including yoga, tai chi, and mindfulness-based stress reduction (MBSR). MBSR is a structured program that combines yoga exercises, educational sessions on lifestyle modification, and a sequence of meditation exercises. Randomized controlled trials of MBSR have consistently found that this approach can improve quality of life and mood and reduce distress in patients with cancer.179
Relaxation and Imagery
Relaxation training, often accompanied by imagery, is frequently advocated to assist patients with cancer in managing the stress of receiving a cancer diagnosis, as well as stress in the treatment and follow-up periods. Various forms of this therapy have been utilized in several randomized controlled trials with indicators of stress, coping, and quality of life as outcomes, with mixed results.180 Most studies have utilized a type of progressive muscle relaxation that the patient learns through a series of guided experiential sessions and then practices independently. Two of the larger trials have studied women with localized breast cancer. The trials showed significant benefits of relaxation with or without imagery over standard care181 or a semistructured one-on-one encounter session.182 At least one study showed some advantage of adding imagery to relaxation for relieving anxiety.182 Most of the studies of the effect of relaxation and imagery on stress reduction and quality of life have enrolled patients who were early in their diagnosis with limited stage disease. Studies are needed to assess the utility of these interventions in other clinical settings.
Xerostomia
Acupuncture
Small single-arm and randomized studies have indicated that acupuncture and acupuncture-like transcutaneous nerve stimulation179 can improve saliva flow and quality of life among patients with head and neck cancer who have severe xerostomia. A systematic review in 2010180 found three eligible trials, all with significant risks of bias, and concluded that evidence was insufficient to recommend acupuncture for the management of this adverse effect. Subsequently, the results of three more randomized trials have been reported. One trial comparing weekly acupuncture versus usual care found significant improvements in xerostomia among patients receiving acupuncture.99 The other two studies explored whether acupuncture might be able to prevent xerostomia if given simultaneously with a course of radiation for head and neck cancer and both found improved outcomes in the acupuncture-treated groups.181,182
Information Resources
Databases
The National Cancer Institute’s Physicians’ Data Query (http://www.cancer.gov/cancertopics/pdq/cam) provides summaries of the literature for several types of CAM approaches. Most topics have separately designed summaries for health care practitioners and patients.
MedlinePlus, a service of the U.S. National Library of Medicine, provides an easily searched format with useful information on CAM topics, including a page providing links to several summaries of the literature on herbs and supplements from the NIH, Natural Medicines Comprehensive Database, and the National Toxicology Program (http://www.nlm.nih.gov/medlineplus/druginfo/herb_All.html).
MD Anderson Cancer Center (http://www.mdanderson.org/education-and-research/resources-for-professionals/clinical-tools-and-resources/cimer/index.html) provides complementary/integrative medicine education resources.
Memorial Sloan Kettering Cancer Center (http://www.mskcc.org/cancer-care/integrative-medicine/about-herbs-botanicals-other-products) provides information about herbs, botanicals, and other products.
The American Cancer Society’s Web site provides an herbs, vitamins, and minerals page with links to summaries on various related topics (http://www.cancer.org/treatment/treatmentsandsideeffects/complementaryandalternativemedicine/herbsvitaminsandminerals/index).






