CHAPTER 3 The cervical spine
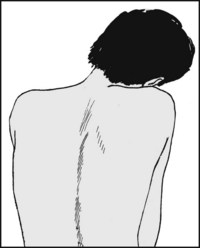
Postural Neck Pain
In this common condition, pain in the neck and shoulders occurs in association with some abnormality of neck posture. It is commonest in females under the age of 40, many of whom have sedentary jobs (such as computer operators) which entail the head being maintained for long periods in a position that may be short of ideal. In some cases there may be a history of minor trauma which exacerbates or precipitates the complaint. Clinically the head and neck may be held in a somewhat protracted position, with some loss of the normal cervical curvature, but there is usually a full range of neck movements with normal radiographs. Analgesics and physiotherapy are usually helpful in the acute case, but in the long term change of work practices and in the patient’s working environment are likely to be of the greatest benefit.
Acute Neck Pain in the Young Adult
In the 20–35-year age group, and often before there is any radiological evidence of arthritic change in the spine, a sudden movement of the neck may produce severe neck and arm pain accompanied by striking protective muscle spasm and limitation of cervical movements. In some cases these symptoms are produced by an acute disc prolapse similar to those occurring more familiarly in the lumbar region. In others, with identical symptoms, investigations including MRI scans may be quite negative; some disturbance of the facet joints or related structures is often thought responsible. Most cases respond to a period of rest in a cervical collar, or physiotherapy in the form of traction. In a few resistant cases gentle manipulation of the cervical spine may be helpful.
Cervical Spondylosis (Cervical Osteoarthrosis: Osteoarthritis of The Cervical Spine)
Cervical spondylosis is easily the most common condition affecting the neck. Degenerative changes appear early in life in the cervical spine, often during the third decade. The disc space between the fifth and sixth cervical vertebrae is most frequently involved. The earliest changes are confined to the disc, but the facet joints and the uncovertebral joints (joints of Luschka) may soon become involved. There is inevitable restriction of movements at the affected level, but this is often impossible to detect clinically as it is masked by persisting mobility in the joints above and below. The condition may in fact never attract attention, but unfortunately in many cases symptoms do occur, sometimes being triggered by minor trauma. Pain may be felt centrally in the neck and may radiate to the occiput, giving rise to severe occipital headache which may be confused with migraine; pain may also radiate distally, often and inexplicably further than might be expected on anatomical grounds, to the region of the lower scapulae. Often there is pain at the side of the neck, quite sharply localised, or in the supraclavicular region. With nerve root involvement from arthritic changes in the facet or uncovertebral joints, there may be radiation of pain into the shoulders, arms and hands, with paraesthesia and, on rare occasions, demonstrable neurological involvement; this may include absent arm reflexes, muscle weakness, and sensory impairment.
In cervical spondylosis the cervical canal may be narrowed by osteophytic lipping of the facet or uncovertebral joints, by central disc herniations, by thickening of the ligamentum flava, or even from local cervical vertebral subluxations associated with ligamentous laxity. Developmental narrowing of the canal may be an additional factor. The reduction in the size of the canal may lead to cord compression (cervical spondylotic myelopathy). The disturbance of cord function that results may cause neck pain, difficulty in walking and unsteadiness on the feet, numbness, paraesthesia, weakness, and loss of upper limb dexterity. There is often coexisting compression of cervical nerve roots, leading to radicular symptoms which may complicate the clinical picture. Bladder dysfunction may occur, but is not common, and extensor plantar responses may appear late. Severe progressive myelopathy from spinal stenosis often requires operative treatment by decompression and stabilisation.
Vertebral artery involvement by osteophytic outgrowths or local spinal instability may cause drop attacks precipitated by extension of the neck. Osteophytes arising from the anterior vertebral margins may sometimes, because of their size, give rise to dysphagia.
The mainstay of treatment in spondylosis is the judicious use of a cervical collar and the prescription of analgesics. If root symptoms are prominent, intermittent or continuous, cervical traction is often employed. Manipulation of the cervical spine, especially in the younger age groups with no neurological involvement, is sometimes advocated. Severe, protracted symptoms may be investigated further by MRI scans, or myelography followed by CT scanning. If a positive lesion is demonstrated, exploration may be carried out; if not, a local cervical fusion may sometimes be advised.
Thoracic Outlet Syndrome
The lower trunk of the brachial plexus and the subclavian artery pass between the anterior and middle scalene muscles and over the first rib. Compression of these structures may result from a cervical rib, a definite but rare occurrence. Slightly more commonly, the same structures may be kinked by fibrous bands or abnormalities in the scalene attachments at the root of the neck, or by a Pancoast tumour. Paraesthesia in the hand is usually severe, and there may be hypothenar and, less commonly, thenar wasting. There is sometimes sympathetic disturbance, with increased sweating of the hand. The radial pulse may be absent, and other signs of vascular impairment may be present. Complete vascular occlusion, sometimes accompanied by thrombosis and emboli, may lead to gangrene of the fingertips. In some cases symptoms may be precipitated by loss of tone in the shoulder girdle, with drooping of the shoulders; in such cases, physiotherapy is often successful in restoring tone to the affected muscles and relieving symptoms. When vascular involvement predominates, arteriography and exploration may be required.
Whiplash and Extension Injuries of the Neck
Whiplash injuries are now a common cause of persistent cervical symptoms. A true whiplash injury occurs classically when, as a result of a rear impact, a stationary or slowly moving vehicle strikes another vehicle or object in front. Because of the inertial mass of the head of the car occupant, there is rapid extension of the cervical spine followed by flexion. In the partial whiplash injury the main element is extension of the neck; this also commonly occurs as a result of a rear impact, but in this case the vehicle in which the occupant is travelling comes to rest more gradually, without striking anything ahead. Unfortunately, the attractive nature of the term has led to its misuse, and some recommend that because of its present imprecision it should be avoided altogether. If, however, it is going to be used, then it should be reserved for soft tissue injuries of the neck where extension is the main element. In the majority of cases the radiographs show normal alignment of the cervical vertebrae, but occasionally small avulsion fractures of the anterior margins of the vertebral bodies give evidence of the forcible extension of the spine. In some cases there are minor fractures involving the uncovertebral joints. Where there are spondylotic changes that interfere with the dissipation of the forces involved (because of localised areas of rigidity in the spine), there may be avulsion of anterior osteophytes. The flexion element may sometimes produce wedge compression fractures of the vertebral bodies or avulsion fractures of the spinous processes. Nevertheless, the discovery of unequivocal pathology in the spine is uncommon, and it is now apparent that there is a significant non-organic element in many cases. Although malingering does occasionally occur, this is considered to be rare. It is thought that in many cases a significant component of late disability is psychological, even if this is not at a conscious level, and that psychological elements and sometimes illness-related behaviour are often established within 3 months of injury.
Symptoms of all degrees of severity may be encountered. There is always pain and stiffness in the neck, sometimes with neurological disturbance involving the upper, and occasionally the lower, limbs. Even minor symptoms may be most protracted, often lasting 18 months or longer. In some cases disability is permanent. Analgesics for short periods and an early return to work are generally advocated, and it is thought best to avoid the use of cervical collars.
Severe extension injuries may occur in falls (often downstairs), when the neck is forcibly extended as the head strikes the ground. There is often telltale bruising of the forehead. In a car accident an unbelted occupant may also suffer severe extension of the neck in the early phases of deceleration, when the forehead strikes the roof and ricochets backwards. In both sets of circumstances the head injury may attract prior attention, but the possibility of these injuries must not be overlooked. Cervical spondylosis again has a deleterious localising effect on the forces involved, and the neurological disturbance may be profound. In some cases thrombosis extends from the area of local cord involvement, so that there may be a deteriorating and sometimes fatal neurological outcome.
Barré–Lieou Syndrome
This may follow a whiplash incident. There is complaint of headache, vertigo, tinnitus, ocular problems and facial pain. It is thought that it may be due to a sympathetic nerve disturbance at the C3–4 level, and in 75% of the cases there is impairment of sensation in the C4 dermatome, with weakness of shoulder and scapular movements. Myelography may show nerve root sleeve disturbances. Good results have been claimed for anterior discectomy combined with local cervical fusion.
Rheumatoid Arthritis in the Cervical Spine
Rheumatoid arthritis frequently involves the neck, often in a patchy fashion so that additional stresses are thrown on the remaining mobile elements. With the ligamentous stretching that often accompanies rheumatoid arthritis there may be progressive subluxation of the cervical spine, particularly at the atlantoaxial and midcervical levels. As this progresses, pain and stiffness in the neck become accompanied by root and cord symptoms. In the case of atlantoaxial subluxations there may be severe occipital headache. The gait tends to become ataxic and there is progressive paralysis, often with bladder involvement. These lesions are usually treated by local cervical fusion if the patient’s general condition permits.
Klippel–Feil Syndrome
In this condition there is restriction of movements in the cervical spine owing to a congenital abnormality characterised by a failure of the cervical vertebrae to differentiate. One or more groups of vertebrae are fused together, and the condition may be associated with congenital elevation of the shoulder (Sprengel’s shoulder). The condition gives rise to an increased susceptibility to injury and often neurological compromise.
Neoplasms in the Cervical Region
Tumours of the cervical spine are rare, secondary deposits being the most common. They may cause vertebral body erosion or collapse, affect issuing nerve roots, or give rise to cord involvement. Of the primary tumours in this region, sarcoma and multiple myeloma are the most common. Primary involvement of the cord may arise with meningiomas and intradural neurofibromata, which may also affect isolated nerve roots.
Osteitis of the Cervical Spine
Osteitis affecting the cervical vertebrae is a rare occurrence in the UK. Tuberculosis, when it occurs, is seen most frequently in children, and may produce widespread bone destruction, vertebral collapse and cord involvement.
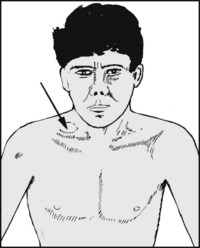
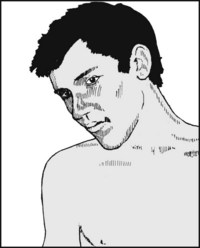
Note any asymmetry in the supraclavicular fossae: this will require separate investigation (e.g. Pancoast tumour). (2) Note the presence of torticollis, where the head is pulled to the affected side and the chin often tilted to the opposite. In congenital torticollis there may be in the infant a small tumour in the sternomastoid muscle, and in the untreated case some facial asymmetry.
NB: in about a third of cases the abnormal head posture is due to ocular muscle weakness, and a specialist ocular assessment is mandatory in every case.
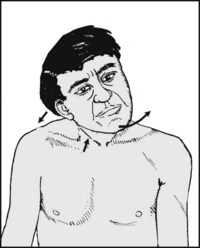
Torticollis contd.: The head is tilted and rotated, the sternomastoid cord-like, and there is often facial asymmetry. In acquired torticollis protective muscle spasm may result from tonsillar or vertebral body infection. It is sometimes seen accompanying the Klippel–Feil syndrome. It may also be due to a vertebral malalignment (especially at the C1/C2 level), from trauma or upper respiratory infection. In advanced infections and tumours the head may be supported by the hands.
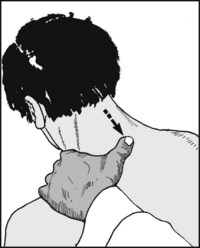
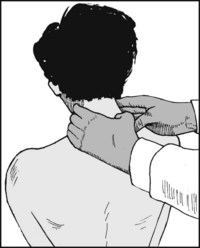
Begin by looking for tenderness in the midline, working from the occiput distally. Tenderness localised to one space is common in cervical spondylosis, and much more rarely accompanies infections of the cervical spine.
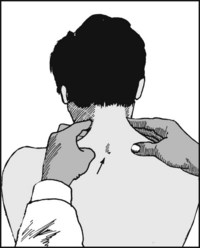
Now palpate the lateral aspects of the vertebrae, looking for masses and tenderness. Note that the most prominent spinous process is that of T1, and not the vertebra prominens, C7.
Continue palpation into the supraclavicular fossae, looking particularly for the prominence of a cervical rib with local tenderness; look also for tumour masses and enlarged cervical lymph nodes.
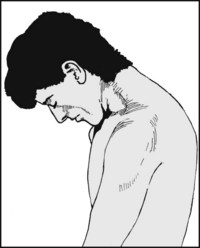
Flexion: Ask the patient to bend the head forward. Normally the chin can be brought down to touch the region of the sternoclavicular joints. The chin–chest distance may be measured for record purposes.
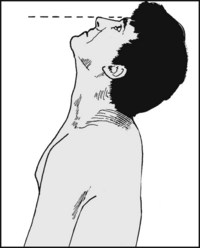
Extension: Ask the patient to tilt the head backward. The patient should be seated (preferably in a high-backed chair) and erect. The plane of the nose and forehead should normally be nearly horizontal, but guard against contributory thoracic and lumbar spine movements.
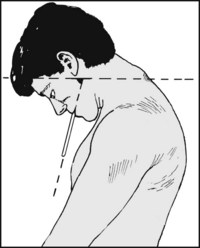
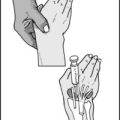
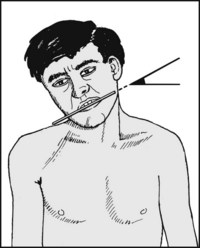
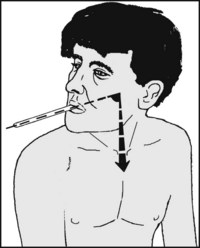
Recording motion in the cervical spine with any accuracy is difficult, but may be attempted using a spatula in the clenched teeth as a pointer. Stand back, and ask the patient to flex the head forward. Line up the legs of a goniometer with the spatula and the horizontal, respectively. Read off the included angle.
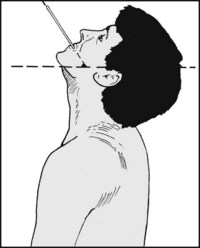
Now ask the patient to extend the head to measure the range of extension from the neutral position.
Normal range = 50°. The total range in the flexion and extension planes should be assessed, either by a single measurement or by the summation of flexion and extension.
Normal range = 130°. Of this total, about a fifth occurs in the atlantoaxial and atlanto-occipital joints.
Lateral flexion: Ask the patient to tilt his head on to his right shoulder. In the normal case lateral flexion, with only slight shrugging of the shoulder, will allow the ear to touch the shoulder. Repeat on the other side and note any difference.
Lateral flexion: For greater accuracy, a spatula clenched in the teeth may again be used as a pointer.
Normal range = 45°. About a fifth of this movement occurs at the atlantoaxial and atlanto-occipital joints. Loss is common in cervical spondylosis.
If lateral flexion cannot be carried out without forward flexion, this is indicative of pathology involving the atlantoaxial and atlanto-occipital joints.
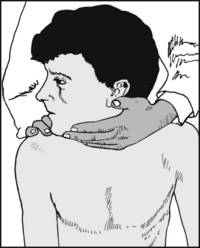
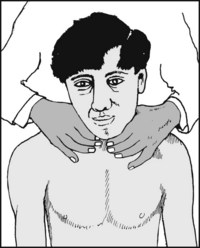
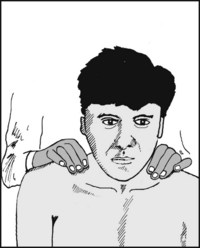
Rotation (1): Ask the patient to look over the shoulder. The movement may be encouraged with one hand and movement of the shoulder restrained with the other. Normally the chin falls just short of the plane of the shoulders.
Rotation (2): Again a spatula may be used as a pointer for measurement.
Normal range = 80° to either side. About a third of this occurs in the first two cervical joints. Rotation is usually restricted and painful in cervical spondylosis.
Spread the hands on each side of the neck and ask the patient to flex and extend the spine. Facet joint crepitus is normally detectable in this fashion, and is a common finding in cervical spondylosis; if in doubt, auscultate on either side of the spine while the patient flexes and extends.
3.17. Thoracic outlet syndrome (1):
This may result from involvement of the space between scalenus anterior, scalenus medius and the first rib, so that the subclavian artery and/or the anterior primary rami of the lower cervical and first thoracic nerves may be affected. Begin by looking for evidence of ischaemia in one hand (e.g. coldness, discoloration, trophic changes). Bilateral changes are more in favour of Raynaud’s disease.
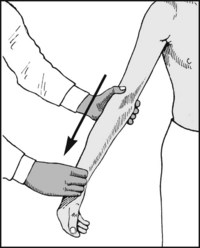
3.18. Thoracic outlet syndrome (2):
Palpate the radial pulse and apply traction to the arm. Obliteration of the pulse is not diagnostic, but when the test reveals no change when repeated on the other side it is suggestive. Note that the syndrome occurs most commonly when the space is narrowed with fibrous bands or other pathology, such as a cervical rib or a Pancoast tumour.
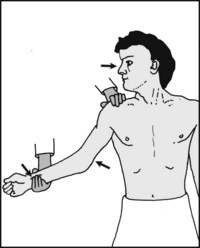
3.19. Thoracic outlet syndrome (3):
Adson’s test: Abduct the shoulder to about 30° and locate the radial pulse (which is assumed to be present). Now ask the patient to turn his head fully to the affected side. He should then be asked to take and hold a deep breath.

3.20. Thoracic outlet syndrome:
Adson’s test contd.: The patient should then exhale, look forward, and lower the arm to the side. The pulse obtained in the first position should be compared with the second. Obliteration or reduction, especially if there is duplication of the patient’s symptoms, is usually significant, but compare the sides. The test may also be tried with the head rotated to the opposite side.

3.21. Thoracic outlet syndrome (4):
The Roos test: The shoulders should be abducted and externally rotated, and the elbows flexed to a right angle. (In this position the arms are in the aptly named ‘surrender’ position.) The hands should be repeatedly and slowly clenched for up to 3 minutes. Neurological and/or vascular symptoms, and early disappearance of the radial pulse on the affected side, are highly significant.

3.22. Thoracic outlet syndrome (5):
Look for neurological disturbance, paying particular attention to myotomes and dermatomes. Note any hypothenar or, much less commonly, thenar wasting. Note any disturbance of the pattern of sweating in the hand. (6): Auscultate over the subclavian artery. A murmur is suggestive of a mechanical obstruction, but repeat on the other side. (7): Examine radiographs for the presence of a cervical rib.
Cord compression and cervical myelopathy (1): In this condition dysfunction in the cervical cord results from local compression. It may be seen where there is developmental narrowing of the spinal canal, or follow old ununited fractures of the dens, or spinal subluxations. It may occur in cervical spondylosis (from osteophytes protruding posteriorly from the vertebral bodies or from the uncovertebral joints) or from cervical disc prolapses. The main finding is of muscle weakness which is greater in the upper than in the lower limbs. In the arms lower motor signs at the level of the compression predominate (although there may be a mixed lesion). In the legs there is a lower motor lesion, which may include exaggerated lower limb reflexes, clonus, an extensor plantar response, loss of proprioception, and often a broad-based or ataxic gait. Extensor plantar responses are late in onset, and the sensory deficit is not dermatomal. The differential diagnosis includes multiple sclerosis (where there are usually abnormal cranial nerve findings), amyotrophic lateral sclerosis (where there is no alteration in sensation), syringomyelia, subacute combined degeneration (where the difference between the findings in the upper and lower limbs is less striking), spinal cord or cerebral tumour, and hydrocephalus.

3.24. Cervical myelopathy (2):
(a) Hoffmann’s test: Rapidly extend the distal phalanx of the middle finger by flicking its anterior surface (i.e. the pulp): the test is positive (indicating corticothalamic dysfunction) if it results in flexion of the interphalangeal joints of the thumb and index. (b) Dynamic Hoffmann test: Repeat while the patient flexes and extends the neck, which often facilitates the response.
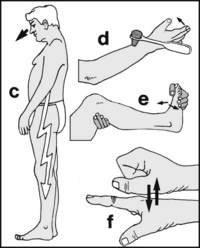
3.25. Cervical myelopathy (3):
(c) L’hermitte’s test: Flexion or extension of the neck produces electric shock-like sensations, particularly in the legs. (d) Inverted radial reflex: This highly specific test is positive if the fingers flex when the radial reflex is elicited. (e) Clonus. (f) Myelopathy hand (indicative of pyramidal tract damage). This has two elements: (i) Kinetic: there is inability to rapidly flex and extend the fingers. Time the patient over 10 seconds. The normal is in excess of 20 cycles.
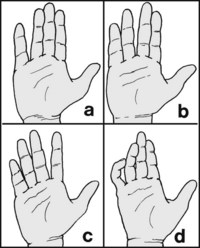
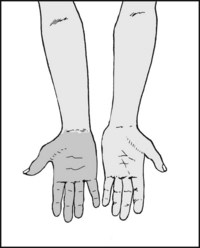
3.26. Cervical myelopathy (4):
Myelopathy hand: (ii) Postural: There is deficient adduction, and often extension, of the ulnar fingers 1–3. In the mildest cases, when the fingers are extended the little finger lies in a slightly abducted position (a); if it can adduct, this position cannot be held for long. The power of abduction is normal, distinguishing it from ulnar nerve palsy. In more severe cases the little, ring (b), and sometimes the middle finger (c) may abduct, and/or the same fingers may flex (d) and lose their power of extension.

The standard projections are the lateral and anteroposterior views of the lower and upper cervical vertebrae. Illustrated: normal lateral projection, with a small non-significant opacity lying anterior to the body of C5. Note the well defined pharyngeal shadows.
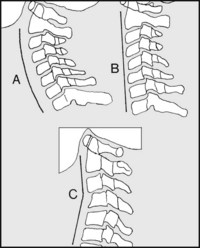
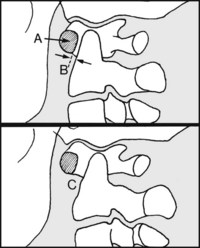
Begin your study of the lateral projection by noting the cervical curve, which is normally slightly convex anteriorly: (A) normal, regular curve; (B) loss of curvature: this can be a positional error, but in those with chronic neck pain (especially postural in origin) it may be due to protective muscle spasm. This is, however, a rather unreliable sign; (C) kinking (from a local lesion such as a subluxation, or from intense local muscle spasm).
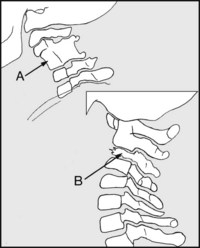
Now look at the general shape of the bodies of the vertebrae, comparing one with another. Note, for example, (A) congenital vertebral fusion, such as occurs in the Klippel–Feil syndrome; (B) vertebral collapse, from tuberculosis, tumour or fracture.
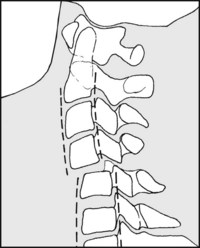
Note the relationship of each vertebra to the ones above and below. It is often helpful in doubtful cases to trace the posterior margins of the bodies. Displacement occurs in dislocations, and may be small when the facet joints on one side only are involved.
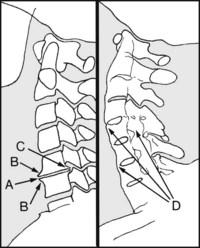
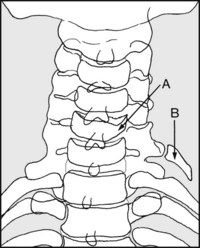
Look at the disc spaces and the related margins of the vertebrae. Note (A) disc space narrowing, (B) anterior lipping, (C) posterior lipping (all typical of cervical spondylosis). Note any evidence of vertebral fusions, (D), typical of ankylosing spondylitis.
Note the presence (A) of an osteophyte or marginal fracture, suggestive of an extension injury of the neck; (B) fracture of a spinous process, suggestive of a flexion injury of the cervical spine. Syringomyelia (which can produce pain in the head, neck and limbs) may cause vertebral body erosions and dilatation of the canal. The diameter of the canal at C5 (C) should not exceed the vertebral body diameter (D) by more than 6 mm.
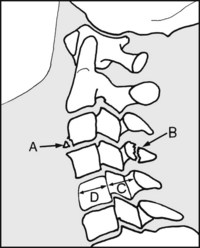
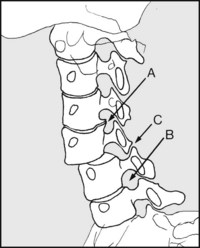
(A) Note that the anterior arch of the atlas lies in front of the lower cervical vertebrae. (B) The distance between the arch and the axis is normally 1–4 mm. A greater distance (C) suggests rupture or laxity of the transverse ligament (e.g. from trauma, rheumatoid arthritis or infection).
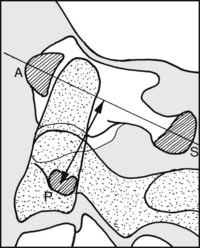
Proximal (cranial) migration of the odontoid process is also commonly seen in rheumatoid arthritis. In the adult this may be assessed by noting the distance between the pedicle (P) of C2 (shown hatched) and a line connecting the spinous process (S) with the arch (A) of C1. If this is less than 11.5 mm, proximal migration is considered to be present.
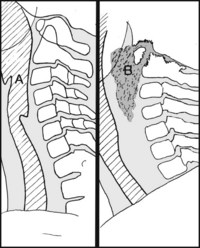
Note the pharyngeal shadow, which normally lies fairly close to the bodies of the vertebrae as at (A). Displacement suggests a retropharyngeal mass, e.g. (B) suboccipital tuberculosis with abscess. Other causes include haematoma and tumour.
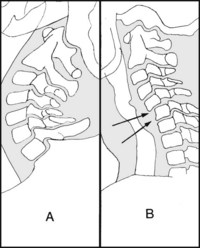
Where instability is suspected the lateral projection should be supervised with the neck (A) in extension, and (B) in flexion. Any latent instability should be discernible by comparing these views. If doubt remains, intensifier screening of movement may help.
In the anteroposterior view interpretation is difficult owing to the complexity of the superimposed structures. Note the shape of the vertebral bodies, observing (A) any lateral wedging, e.g. from fracture, tumour or infection. Note (B) the presence of any cervical rib.
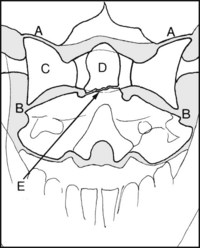
In the anteroposterior view of C1–3, note (A) the atlanto-occipital joints, (B) the atlantoaxial joints, (C) the lateral mass of the atlas. Note any lack of symmetry in the alignment of the odontoid process with the atlas, and look for any evidence of fracture (E). Occasionally congenital abnormalities of the odontoid process (such as hypoplasia, or failure of fusion between its ossification centre and the main mass of the axis) may cause difficulties in interpretation.
Right and left oblique projections are invaluable in demonstrating (A) localised lipping in the uncovertebral joints (joints of Luschka) which may be encroaching on the neural foramina (B). They may also show overlapping (locked) facet joints (C) in cervical subluxations.
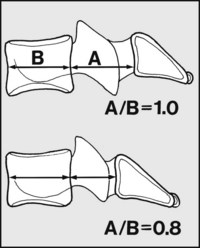
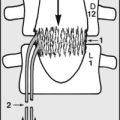
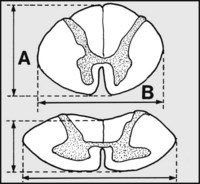
Suspected cervical myelopathy (1): (a) the Pavlov ratio. Normally, the depth (A) of the cervical canal, as seen in the lateral projection, is as great as that of its related vertebral body (B), giving a Pavlov ratio (A/B) of 1.0, and more than adequate room for the spinal cord. A Pavlov ratio of 0.8 or less indicates a developmentally narrow cervical canal, with risk of cord compression. If the ratio is reduced check the lumbar spine, as there may well be an associated lumbar spinal stenosis.
Suspected cervical myelopathy (2): If there are axial MRI scans (or postmyelographic CT scans) which show the cord at the suspect levels, the presence and degree of cord compression may be assessed by working out the cord compression ratio. This is calculated by dividing the (sagittal) diameter (thickness) (A) of the cord by its width (B). (As this is a ratio, the reduction effects of the scans are immaterial.) Note also that the cord may be considerably distorted, so use its minimal sagittal diameter for the calculation. A value of 0.4 is indicative of a serious degree of compression, and if decompression surgery is planned it is best done before a figure as low as this is reached.

3.45. Cervical spine radiographs: examples of pathology (1):
The cervical curvature is reversed: there is wedging of the body of C6.

This oblique projection shows osteophytes arising from the uncovertebral joint.
Diagnosis: cervical spondylosis, associated in this case with unilateral compression of the C6 nerve root.

The inferior articular process of C4 is displaced anteriorly over the upper articular process of C5. (The corresponding oblique projection of the other side is normal.)
Diagnosis: unilateral facet joint dislocation, in this case with entrapment of C5.

There is widespread fusion of the intervertebral facet joints, and the anterior longitudinal ligament is calcified.

There is marked loss of vertebral alignment, and the inferior articular processes of C6 are lying in front of the superior articular processes of C7. The spinous processes of C5 and C6 are fractured.
Diagnosis: dislocation of cervical spine (C6 on C7) with locked facets.

There is narrowing of the C5–6 disc space and, to a lesser extent, that of C6–7. There is anterior lipping of C4, 5, 6 and 7. There is posterior lipping of C5.

There is gross anterior lipping of C5, 6 and 7, with near anterior interbody fusion. The pharyngeal shadow is distorted.
Diagnosis: severe cervical spondylosis, associated in this case with dysphagia. Similar appearances are found in Forestier’s disease, a condition in which there is excessive, widespread osteophyte formation and abnormal ligamentous calcification (especially of the anterior longitudinal ligament).

There is loss of the normal cervical curvature, narrowing of the C5–6 disc space and anterior lipping. There is an avulsion fracture of the anterior inferior margin of C4.
Diagnosis: extension injury of the spine with a marginal fracture and cervical muscle spasm in a patient susceptible to injury because of pre-existing cervical spondylosis.

The radiograph has been taken in flexion (one part of a flexion and extension pair) and shows an excessive gap between the anterior arch of the atlas and the odontoid process. There is generalised vertebral demineralisation.
Diagnosis: rheumatoid arthritis with an atlantoaxial subluxation.

There is deformity of the cervical spine, with the presence of only half of a vertebral body at the C6 level.
Diagnosis: congenital deformity of the cervical spine (hemivertebra cervicalis).