CHAPTER 283 Treatment of Thoracic Disk Herniation
The incidence of thoracic disk herniation ranges from 7% to 37%.1,2 However, only 0.25% to 0.57% of all disk herniations are symptomatic.3 Thoracic disk herniation may present with neurological manifestations that include pain; sensory loss; bowel, bladder, or sexual dysfunction; paraparesis; and paraplegia. In this chapter we review the evolution of surgical techniques that can be used to perform thoracic diskectomies.
History and Epidemiology
Middleton and Teacher4 performed the first thoracic diskectomy in 1911 on a paraplegic man who subsequently died. In those days, diagnosis was based on the identification of calcification in the disk space and clinical acumen. The limited diagnostic resources made it difficult to diagnose early disease and localize it accurately. Many patients presented with frank myelopathy and severe neurological deficits.5
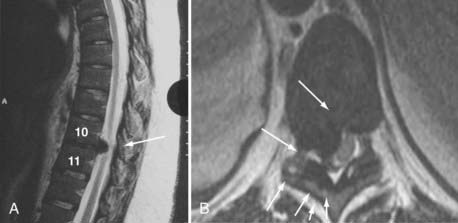
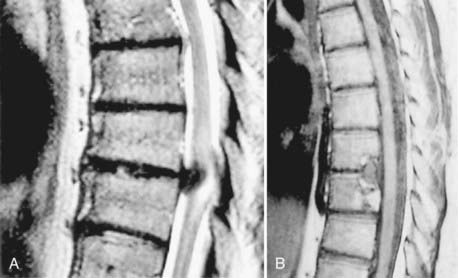
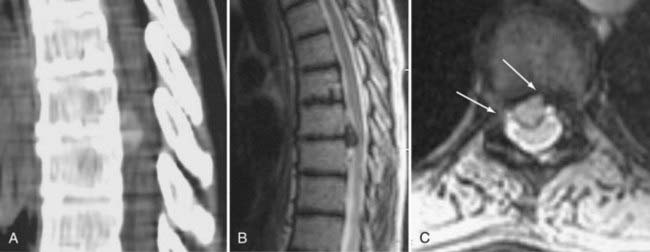
The advent of computed tomography (CT) and later magnetic resonance imaging (MRI) dramatically improved the ability to diagnose and localize the level of the herniated thoracic disk.6 With the further development of MRI techniques, clinicians can now accurately diagnose and pinpoint the level of disk herniation in the thoracic spine. CT-myelography provides additional information in certain cases, especially when the disk is calcified or when reoperation is being performed at the same level to determine the extent of prior bone resection. Currently, MRI is considered the first-line modality to diagnose thoracic disk herniation. It is noninvasive and provides a precise image of the herniated disk and its relationship to the dural sac and the nerve; it provides additional information about the conformation of the cord and whether an intramedullary signal change, and hence cord injury, is present.
Most thoracic disk herniations occur in patients between the fourth and sixth decades of life, with a slight male predominance.7 A history of trauma is reported in 22% to 50% of symptomatic patients.8 It is usually associated with a fall landing on the feet or buttocks, combined with an axial spinal rotation. Thoracic disk herniations are much less common than herniations of the lumbar and cervical spine. This is because of the limited mobility of the thoracic spine, the smaller disks, and the stabilizing effect of the rib cage.9,10
Early surgical attempts to treat thoracic disks involved a posterior laminectomy, dural sac retraction, and completion of the diskectomy. These operations were associated with a high rate of neurological deterioration and death. Published series quoted neurological deterioration in 18% to 66% of patients and mortality rates of 14% to 50%.9,11–15
Clinical Presentation and Differential Diagnosis
Pain is the most common symptom associated with thoracic disks. The pain is dorsal and midline in 57% to 88% of patients but may be dermatomal in 9% to 57%. When dermatomal, the pain is lancinating and often unilateral, but it may be bilateral in some cases. The next most common complaint is sensory changes in a radicular pattern, occurring in 39% to 100% of patients. Dermatomal sensory loss is quite rare because of the overlap in sensation from adjacent-level nerve roots. In addition, patients may present with findings associated with spinal cord compression, including myelopathy (9% to 100% of patients), weakness (41% to 100%), and bowel and bladder dysfunction (18% to 78%).8,16–20
Unusual presentations have been reported as well. A herniated disk at the level of C7-T1 or T1-2 has been reported to cause Horner’s syndrome.21–24 Another unusual presentation is dysesthesia in the medial arm, which may erroneously be associated with myocardial infarction, angina, thoracic aortic dissection, or bronchogenic tumor.25 Also, far lateral thoracic disk herniation may present as flank pain.26
Patients may present with spinal cord syndromes associated with thoracic disk herniation. The specific presentation is dependent on the pattern of neural compression on the cord. Brown-Séquard syndrome may occur when the herniated disk is lateral and compressing one side of the spinal cord, whereas anterior spinal artery syndrome occurs when the herniated disk is central and compressing the anterior spinal artery; conus medullaris syndrome is caused by a herniated disk compressing the conus medullaris at the thoracolumbar junction.13,16,19 Other differential diagnoses include primary and metastatic neoplasm, demyelinating disease, primary motoneuron disease, neuromuscular disease, myopathy, muscular dystrophy, motor neuropathy, spinal cord infarction, and spinal cord vascular malformation. Other entities that need to be considered are those related to visceral referred pain, such as renal colic, gallbladder colic, colitis, intercostal neuritis, and costochondritis.25
Radiologic Evaluation
Magnetic Resonance Imaging
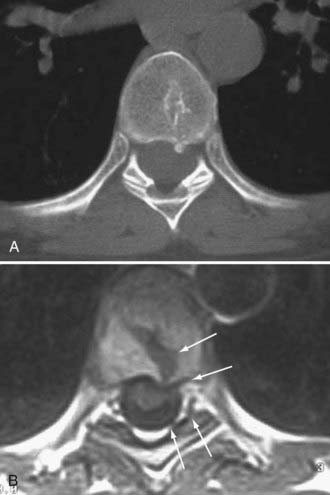
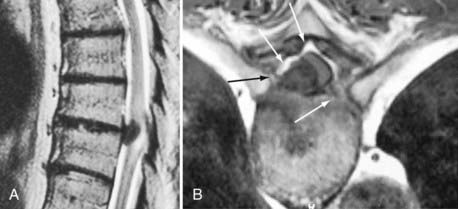
The primary care physician often performs MRI of the thoracic spine in the evaluation of back pain. It is the best screening method for thoracic disk herniation, given its noninvasive nature and high sensitivity. However, it is also associated with 14.5% false-positive rate, making it crucial to correlate the MRI information with the clinical examination.27,28 The exaggeration of disk herniation (which is not unique to the thoracic spine), especially in sagittal images, has been attributed to the edge effect, which occurs when two substances of different proton densities are next to each other. The edge effect is most pronounced on T2-weighted images between the disk substance and the adjacent cerebrospinal fluid. Axial images provide further information about the level of stenosis caused by the herniated thoracic disk. Increased signal on T2-weighted images may be seen in the spinal cord when it is significantly compressed. In addition, MRI can distinguish herniated disks in the thoracic spine from neoplastic, demyelinating, or infectious pathologies. It can also distinguish intradural versus extradural lesions. When the accuracy of MRI is in doubt, it is best to obtain a thoracic myelogram and postmyelogram CT to further delineate the extent of dural sac compression, presence of calcification in the herniated disk, and presence of posterior osteophytes and their relation to the dural sac.29,30 Thoracic myelograms and postmyelogram CT scans are most useful for extradural lesions.
Myelography and Postmyelography Computed Tomography
Some clinicians still consider the combination of myelography and postmyelography CT the “gold standard” in patients with calcified herniated disks. It typically shows an indentation caused by an extradural mass compressing the dural sac at the level of the disk. Postmyelography CT allows the distinction among bone, calcified soft tissue, soft tissue, dural sac, and spinal cord. It also allows the visualization of posterior osteophytes and disk material and their relationship to the dural sac. Twelve percent of thoracic disk herniations are associated with calcifications in the spinal canal, which suggests an intradural extension of the herniated disk.22,29,31,32 CT-myelography, like MRI, has a high false-positive rate (13.5%) in diagnosing symptomatic thoracic disk herniation.33
Management
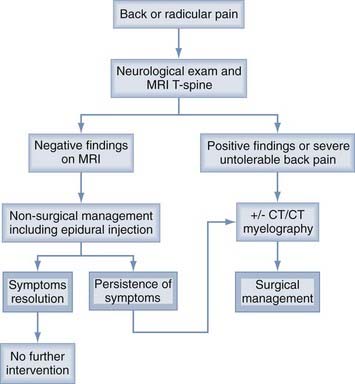
Management of symptomatic disk herniation is illustrated in Figure 283-1. Nonsurgical management should be instituted first, unless there is an associated neurological deficit or intolerable pain. Surgical intervention is indicated when there is radiographic evidence of spinal cord compression and clinical examination findings of myelopathy, weakness, or bowel, bladder, or sexual dysfunction, or when the patient is experiencing severe back or radicular pain. Patients with mild to moderate pain that is refractory to conservative management may be good surgical candidates as well. The aim of conservative therapy is to allow the herniated disk to resorb34 and the inflamed nerve root to heal.18,28,29,35
Nonsurgical Management
Nonsurgical management includes restricted activity, immobilization with a hyperextension brace, oral steroids, nonsteroidal anti-inflammatory drugs, oral pain medications, and epidural injections.18,28,29,35 Figure 283-1 summarizes the nonsurgical management protocol.
Surgical Management
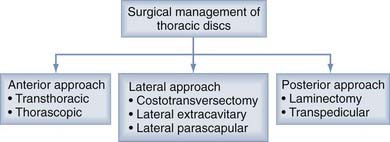
Three surgical approaches can be used: posterior, posterolateral, and anterior (Fig. 283-2). The posterior approach includes dorsal laminectomy and a transpedicular approach. The posterolateral approach includes costotransversectomy and lateral extracavitary and lateral parascapular approaches. The anterior approach includes transthoracic and thoracoscopic approaches. Table 283-1 summarizes the pros and cons of each approach.
TABLE 283-1 Pros and Cons of Surgical Approaches for Thoracic Diskectomy
| APPROACH | PROS | CONS |
|---|---|---|
| Laminectomy | Simple to perform | High morbidity and mortality Limited exposure Need to retract dural sac |
| Transpedicular | Simple to perform Minimally invasive Good for lateral disks; may be used for paracentral disks with poor visualization |
Difficult to visualize ventral dural sac Difficult to dissect midline calcified disks Limited exposure for multilevel OPLL |
| Costotransversectomy | Extrapleural Good for lateral disks; may be used for paracentral disks with better visualization than transpedicular approach |
Difficult to visualize ventral dural sac Difficult to dissect midline calcified disks Limited exposure for multilevel OPLL |
| Lateral extracavitary | Extrapleural Best visualization of midline structures among posterior and posterolateral approaches Access to multiple levels Adequate exposure to resect multilevel OPLL Allows fusion if needed |
Limited visualization of ventral dural sac Painful Potentially higher risk for radicular artery injury leading to spinal cord infarction45 |
| Transthoracic (open) | Best visualization of large midline calcified or soft herniated disks Access to multiple levels Adequate exposure to resect multilevel OPLL Access for fusion if needed |
Painful Potential morbidity Need for chest tube |
| Thoracoscopic | Best visualization of large midline calcified or soft herniated disks Access to multiple levels (up to three) Minimally invasive |
Limited exposure for multilevel OPLL Need for chest tube Steep learning curve |
OPLL, ossification of the posterior longitudinal ligament.
Identification of Surgical Level
Identification of the correct surgical level may be challenging. Preoperative lumbar and thoracic films are helpful in determining the number of lumbar vertebrae and identifying the last thoracic rib in relation to the herniated disk level. Intraoperative identification of the surgical level is performed with high-quality fluoroscopy, anteroposterior and lateral films, or imaging guidance when available.36,37
Posterior Approach
Posterior thoracic laminectomy was the first approach described for thoracic diskectomies. However, it provides inadequate exposure of midline herniated disks, and significant retraction of the dural sac is almost always needed. It is estimated that 70% to 90% of thoracic disk herniations that cause spinal cord or nerve compression are central or paracentral.22,29,31,32 This explains the necessity of dural sac retraction to reach the herniated disk. There are reports that thoracic laminectomy performed for thoracic diskectomy is associated with unacceptably high rates of morbidity and mortality. It is estimated that there is at least a 45% chance of experiencing neurological deterioration or no benefit with this approach.14,38,39 Currently, this approach is completely contraindicated in the management midline calcified herniated thoracic disks,40 and surgeons should consider the other approaches discussed.
![]() Alternatively, the transpedicular approach allows better exposure of the paracentral herniated disk, with minimal dural sac retraction and sparing of the facet (Fig. 283-3). The foramen of the affected level is unroofed by drilling the medial half of the inferior facet of the above vertebra and the medial half of the superior facet along with the superior part of the pedicle of the lower vertebra. A trough is created with a high-speed diamond drill in the posterior inferior vertebrae overlying the relevant disk space; in the posterior superior vertebrae below the disk space, including the end plates; and in the lateral aspect of the disk space laterally. The resultant trough should be large enough to pull the disk material into the trough without significant manipulation of the dura. (See Video 283-1.)
Alternatively, the transpedicular approach allows better exposure of the paracentral herniated disk, with minimal dural sac retraction and sparing of the facet (Fig. 283-3). The foramen of the affected level is unroofed by drilling the medial half of the inferior facet of the above vertebra and the medial half of the superior facet along with the superior part of the pedicle of the lower vertebra. A trough is created with a high-speed diamond drill in the posterior inferior vertebrae overlying the relevant disk space; in the posterior superior vertebrae below the disk space, including the end plates; and in the lateral aspect of the disk space laterally. The resultant trough should be large enough to pull the disk material into the trough without significant manipulation of the dura. (See Video 283-1.)
The transpedicular approach reportedly yields satisfactory results for both soft and calcified disks in the lateral and centrolateral position. However, it is inadequate for central herniated thoracic disks.2 Fusion is rarely needed with the transpedicular approach because it spares the facet and maintains the integrity of the anterior column, anterior longitudinal ligament, posterior longitudinal ligament, and posterior band. One report described a delayed compression fracture after a transpedicular approach,41 but we have encountered no such adverse complications. This approach has been performed through an endoscope42 and through a minimally invasive tube,43 with favorable outcomes.
Posterolateral Approach
In the costotransversectomy approach, the transverse process and a proximal piece of the rib head are resected, providing further direct midline exposure of the ventral dura. Hulme44 reported good results with the costotransversectomy approach to thoracic diskectomy.
The lateral extracavitary and lateral parascapular approaches involve much more lateral exposure and dissection than the costotransversectomy approach. They allow better visualization of midline structures and may be especially useful when an extensive exposure is required for the placement of cages or the performance of vertebrectomy for infectious, neoplastic, or traumatic lesions.25,45 The lateral extracavitary approach as described by Maiman and coworkers17 involves cutting the head of the rib as well as 8 cm of the rib distal to the dorsal root ganglion. The intercostal nerve is sacrificed by tying it 3 cm distal to the dorsal root ganglion. A posterior vertebral body trough is created with a drill, into which calcified disk and osteophytes are fractured, decompressing the dura. The lateral extracavitary approach has yielded satisfactory results in thoracic diskectomy.17 In addition, it allows an extrapleural approach to the anterior elements without the need for postoperative chest tubes, as well as the option of anterior or posterior instrumentation in the same setting if needed. A modified lateral extracavitary approach has been described whereby the neurovascular bundle is preserved, avoiding the potential complication of intercostal neuralgia or anesthesia dolorosa secondary to intercostal nerve resection25 or spinal cord infarction secondary to a radicular artery injury.46 The extracavitary approach can be performed in a minimally invasive fashion by using the METRx tube (Medtronic Sofamor Danek, Memphis, TN) and an endoscope, as described by Lidar and associates.47
The costotransversectomy and lateral extracavitary approaches are not facet-sparing; therefore, fusion should be considered for some patients, especially in the lower thoracic levels, where the rib cage does not provide as much support (Figs. 283-4 to 283-6).
Anterior Approach
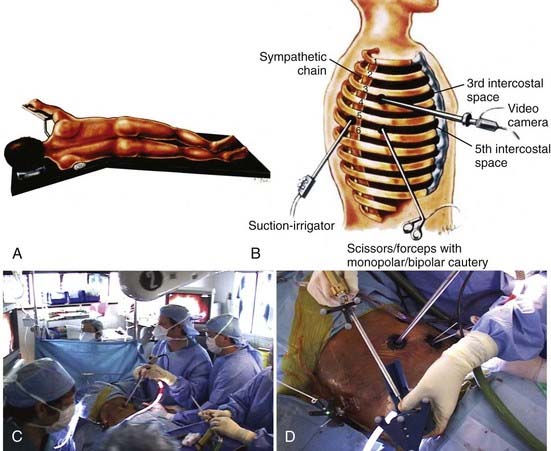
At the T11-L1 region, the diaphragm limits the surgeon’s working channel and must be retracted. At those levels, either a retroperitoneal approach and release of the diaphragm or a thoracoscopic approach may be indicated.48 A right-sided approach at the level of the third rib may be performed for the upper levels when using a transthoracic approach.49 In contrast, the thoracoscopic approach may be performed from either side from T2 down to T12, and the choice of the surgical side is determined by the lesion’s laterality (Figs. 283-7 and 283-8).
Understanding the anatomy is paramount. Each rib articulates with the superior posterior part of the same level vertebra and with the inferior posterior part of the above vertebra (except the 1st, 11th, and 12th ribs, which articulate only with the same level vertebrae).48 Hence, from an anterior lateral approach, the posterior part of the disk and the neural foramen are parallel and behind the rib head. Therefore, access to the herniated disk and neural foramen necessitates drilling the rib head.
Few ligaments are encountered; the radiate, costotransverse, intertransverse, and capsular ligaments and their relation to the surgical site are illustrated in Figure 283-9.22,48,50 The radiate ligament attaches the tip of the rib head in a web-like fashion to the vertebra of the above level, the same level vertebra, and disk space between them. The different costotransverse ligaments attach the rib head to the transverse process, and the capsular ligament (not shown in Fig. 283-9) connects the ventral part of the transverse process to the dorsal portion of the articulating rib.
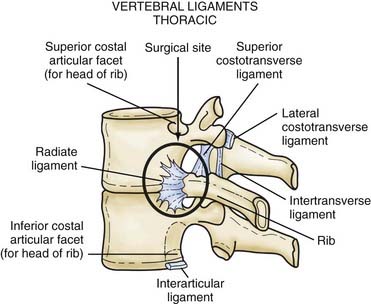
FIGURE 283-9 Diagram illustrating the surgical site and its relationship to the surrounding ligaments from an anterior approach.
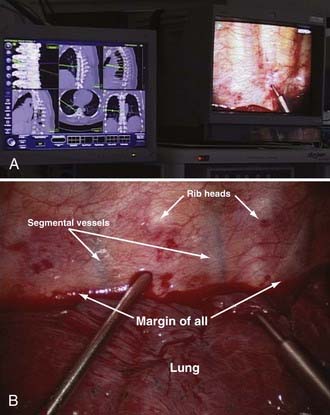
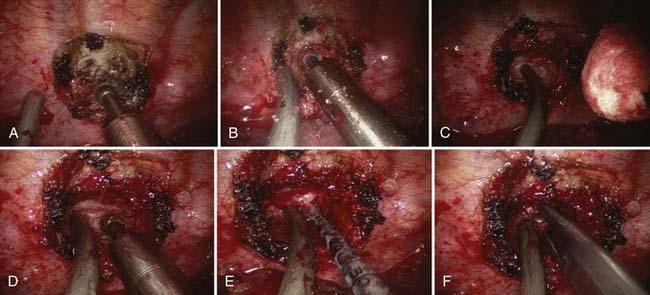
The proximal 2 cm of the rib head is skeletonized with the electrocautery and then drilled with a high-speed coarse diamond drill, exposing the pedicle and neural foramen (Fig. 283-10). The pedicle is subsequently drilled until the dura and nerve sleeve are visualized. At that time, the surgeon will be able to recognize the posterior part of the overlying vertebra and same level vertebra. A trough is created with the high-speed coarse diamond drill in the posterior inferior vertebra above the relevant disk space and in the posterior superior vertebra below the disk space, until reaching the midline. The posterior cortex of the vertebra is left to avoid compression on the dural sac. With a curet, the herniated disk and the posterior longitudinal ligament are dissected off the dural sac and pushed anteriorly, along with the posterior cortical bone that was left undrilled. Using pituitary and Kerrison rongeurs, the herniated disk, posterior longitudinal ligament, and posterior cortex of the vertebra are removed. A chest tube is placed, and the patient is weaned off it postoperatively per protocol.
![]() Thoracoscopic surgery is a minimally invasive approach that achieves the same results as its open counterpart, with reduced postoperative pain, morbidity, and length of stay.51–53 It was first used simultaneously by Mack and colleagues54,55 in the United States and Rosenthal and associates56 in Germany. Unlike its open counterpart, the thoracoscopic technique can manage disks through a left- or right-sided approach from T5-6 down to T11-12 (Figs. 283-11 to 283-13). Its downside is the steep learning curve associated with the technique, making it less practical for surgeons who do not perform thoracic diskectomies on a regular basis. We have used the endoscopic approach in combination with an image guidance system that allows consistent correct localization of the affected level. The surgical technique is otherwise very similar to the open thoracotomy described earlier. (See Video 283-2.)
Thoracoscopic surgery is a minimally invasive approach that achieves the same results as its open counterpart, with reduced postoperative pain, morbidity, and length of stay.51–53 It was first used simultaneously by Mack and colleagues54,55 in the United States and Rosenthal and associates56 in Germany. Unlike its open counterpart, the thoracoscopic technique can manage disks through a left- or right-sided approach from T5-6 down to T11-12 (Figs. 283-11 to 283-13). Its downside is the steep learning curve associated with the technique, making it less practical for surgeons who do not perform thoracic diskectomies on a regular basis. We have used the endoscopic approach in combination with an image guidance system that allows consistent correct localization of the affected level. The surgical technique is otherwise very similar to the open thoracotomy described earlier. (See Video 283-2.)
Some surgeons prefer the open thoracic approach because of its familiarity and broader application. Unlike its thoracoscopic counterpart, the open thoracic approach does not have a steep learning curve, and it can be used for multilevel vertebrectomies for neoplastic or infectious lesions requiring instrumentation and fusion, small or giant intervertebral disk herniation, and unstable traumatic fractures requiring instrumentation and fusion.57,58
Results and Complications
Results of thoracic diskectomy in patients with myelopathy may depend on the duration and severity of preoperative myelopathy. Hence, patients with new-onset mild myelopathy may have a better chance for improvement or recovery.59 It is hard to compare the results of the different approaches because of the low incidence of thoracic disk herniation, the nonstandardized measurement of results, and some surgeons’ preference for one particular approach. Good results have been reported with all approaches, with the exception of laminectomy. The improvement rate for myelopathic patients ranges from 71% to 97%.8,18,29,38,51 For back and radicular pain, the improvement rate varies between 67% and 94%.20,25,60
McCormick and coworkers46 reviewed all approaches for complications and found that neither neurological nor nonneurological complications were significantly higher with any particular approach (excluding laminectomy). They evaluated rate of infection, pneumonia, pulmonary embolism, intercostal neuralgia, and cerebrospinal fluid leak and found no significant difference among approaches. Furthermore, they found that postoperative spinal instability is most likely due to preoperative predispositions and is not directly related to any particular approach. However, they found a number of misdiagnoses and misidentifications of surgical level that could have been prevented with preoperative lumbar and thoracic plain films, CT of the thoracic spine, and use of high-quality intraoperative fluoroscopy or an intraoperative image-guided system.
The need to reoperate has been reported in patients in whom the surgical level was misidentified46,61,62 or in whom the herniated disk was incompletely dissected owing to its inadequate visualization.46,61 Incompletely dissected herniated disks are most often midline and calcified.61 When they are intradural, they are extremely challenging to dissect.61 Hence, an anterior approach, providing an oblique view of the posterior longitudinal ligament and herniated disk, and resection of the posterior longitudinal ligament along with the herniated disk for complete spinal cord decompression are encouraged for midline, calcified disks.46,61–65
Aizawa T, Sato T, Sasaki H, et al. Results of surgical treatment for thoracic myelopathy: minimum 2-year follow-up study in 132 patients. J Neurosurg Spine. 2007;7:13-20.
Bartels RH, Peul WC. Mini-thoracotomy or thorascopic treatment for medially located thoracic heniated disc. Spine. 2007;32:581-584.
Bilsky M. Transpedicular approach for thoracic disc herniations. Neurosurg Focus. 2000;9(4):E3.
Dickman CA, Rosenthal D, Regan JJ. Reoperation for herniated thoracic discs. J Neurosurg Spine. 1999;91:157-162.
Dickman CA, Theodore N, Hurlbert RJ, et al. Thoracic disc [letter]. J Neurosurg. 1996;85:187.
Fessler RG, Dietze DD, MacMillan M, et al. Lateral parascapular extrapleural approach to the upper thoracic spine. J Neurosurg. 1991;75:349-355.
Hamilton MG, Thomas HG. Intradural herniation of a thoracic disc presenting as flaccid paraplegia: case report. Neurosurgery. 1990;27:482-484.
Johnson JP, Filler AG, McBride DQ. Endoscopic thoracic discectomy. Neurosurg Focus. 2000;9(4):E11.
Johnson JP, Stokes JK, Oskouian RJ. Image-guided thoracoscopic spinal surgery: a merging of 2 technologies. Spine. 2005;30:572-578.
Kalfas I. Laminectomy for thoracic spincal canal stenosis. Neurosurg Focus. 2000;9(4):E2.
Lidar Z, Lifshutz J, Bhattacharjee S, et al. Minimally invasive, extracavitary approach for thoracic disc herniation: technical report and preliminary results. Spine J. 2006;6:157-163.
Lifshutz J, Lidar Z, Maiman D. Evolution of the lateral extracavitary approach to the spine. Neurosurg Focus. 2004;16(1):E12.
Maiman DJ, Pintar FA. Anatomy and clinical biomechanics of the thoracic spine. Clin Neurosurg. 1991;38:296-324.
McCormick WE, Will SF, Benzel EC. Surgery for thoracic disc disease. Complication avoidance: overview and management. Neurosurg Focus. 2000;9(4):13.
Oskouian RJ, Johnson JP. Endoscopic thoracic microdiscectomy. Neurosurg Focus. 2005;18(3):E11.
Oskouian RJ, Johnson JP. Endoscopic thoracic microdiscectomy. J Neurosurg Spine. 2005;3:459-464.
Sheikh H, Samartizis D, Perez-Cruet MJ. Techniques for the operative management of thoracic disc herniation: Minimally invasive thoracic microdiscectomy. Orthop Clin North Am. 2007;38:351-361.
Stillerman CB, Chen TC, Couldwell WT, et al. Experience in the surgical management of 82 symptomatic herniated thoracic discs and review of the literature. J Neurosurg. 1998;88:623-633.
Stillerman CB, Chen TC, Couldwell WT, et al. Thoracic disc [letter]. J Neurosurg. 1996;85:189-190.
Stillerman CB, Weiss MH. Management of thoracic disc disease. Clin Neurosurg. 1991;38:325-352.
Vollmer DG, Simmons NE. Transthoracic approaches to thoracic disc herniations. Neurosurg Focus. 2000;9(4):E8.
1 Carson J, Grumpert J, Jefferson A. Diagnosis and treatment of thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry. 1971;34:68-77.
2 Bilsky M. Transpedicular approach for thoracic disc heniations. Neurosurg Focus. 2000;9(4):E3.
3 Stillerman CB, Chen TC, Couldwell WT, et al. Experience in the surgical management of 82 symptomatic herniated thoracic discs and review of the literature. J Neurosurg. 1998;88:623-633.
4 Middleton GS, Teacher JH. Injury of the spinal cord due to rupture of an intervertebral disc during muscular effort. Glasgow Med J. 1911;1:16.
5 Benjamin V. Diagnosis and management of thoracic disc disease. Clin Neurosurg. 1983;30:577-605.
6 Burke TG, Caputy A. Treatment of thoracic disc herniation: Evolution toward the minimally invasive thoracoscopic technique. Neurosurg Focus. 2000;9(4):E9.
7 Arseni C, Nash F. Thoracic intervertebral disc protrusion: a clinical study. J Neurosurg. 1960;17:418-430.
8 Otani K, Yoshida M, Fujii E. Thoracic disc herniation: surgical treatment in 23 patients. Spine. 1988;13:1262-1267.
9 Hawk WA. Spinal compression caused by ecchondrosis of the intervertebral fibrocartilage: with a review of the recent literature. Brain. 1936;59:204-224.
10 McInerney J, Ball P. The pathophysiology of thoracic disc disease. Neurosurg Focus. 2000;9(4):E1.
11 Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl Surg Soc. 1934;211:210-215.
12 Muller R. Protrusion of thoracic intervertebral discs with compression of the spinal cord. Acta Med Scand. 1951;139:99-104.
13 Love JG, Kiefer EJ. Root pain and paraplegia due to protrusions of thoracic intervertebral discs. J Neurosurg. 1950;7:62-69.
14 Loque V. Thoracic intervertebral disc prolapse with spinal cord compression. J Neurol Neurosurg Psychiatry. 1952;15:227-241.
15 Tovi D, Strang RR. Thoracic intervertebral disc protrusions. Acta Chir Scand. 1960;267:3-41.
16 Arce CA, Dohrmann GJ. Thoracic disc herniation: improved diagnosis with computed tomographic scanning and a review of the literature. Surg Neurol. 1985;23:356-361.
17 Maiman DJ, Larson SJ, Luck E, et al. Lateral extracavitary approach to the spine for thoracic disc herniation: report of 23 cases. Neurosurgery. 1984;14:178-182.
18 Fessler RG, Dietze DD, MacMillan M, et al. Lateral parascapular extrapleural approach to the upper thoracic spine. J Neurosurg. 1991;75:349-355.
19 Arce CA, Dohrmann GJ. Herniated thoracic disks. Neurol Clin. 1985;3:383-392.
20 Stillerman CB, Weiss MH. Management of thoracic disc disease. Clin Neurosurg. 1991;38:325-352.
21 Gelch MM. Herniated thoracic disc at T1-2 level associated with Horners syndrome: case report. J Neurosurg. 1978;48:128.
22 Hann EC. Experience with ruptured T1-T2 discs. J Indiana State Med Assoc. 1980;73:598-599.
23 Kumar R, Nuckley T. First thoracic disc protrusion. Spine. 1986;11:449.
24 Lloyd TV, Johnson JC, Paul DJ. Horner’s syndrome secondary to herniated disc at T1-T2. Am J Radiol. 1980;134:184-185.
25 Santiago P, Fine AD, Shafron D, et al. Benign extradural lesions of the dorsal spine. In: Winn RH, editor. Youmans Neurological Surgery. 5th ed. Philadelphia: Saunders; 2004:4491-4506.
26 Ozturk C, Tezer M, Sirvanci M, et al. Far lateral thoracic disc herniation presenting with flank pain. Spine J. 2006;6:201-203.
27 Williams MP, Cherryman GR, Husband JE. Significance of thoracic disc herniation demonstrated by MR imaging. J Comput Assist Tomogr. 1989;13:211.
28 Williams MP, Cherryman GR. Thoracic disk herniation: MR imaging. Radiology. 1988;167:874-875.
29 Dietze DD, Fessler RG. Thoracic disc herniations. Neurosurg Clin N Am. 1993;4:75-90.
30 Blumenkopf B. Thoracic intervertebral disc herniations: Diagnostic value of magnetic resonance imaging. Neurosurgery. 1988;23:36-40.
31 Chowdhary UM. Intradural thoracic disc protrusions. Spine. 1987;12:718-719.
32 Hamilton MG, Thomas HG. Intradural herniation of a thoracic disc presenting as flaccid paraplegia: case report. Neurosurgery. 1990;27:482-484.
33 Awwad EE, Martin DS, Smith KR, et al. Asymptomatic versus symptomatic herniated thoracic discs: their frequency and characteristics as detected by computed tomography after myelography. Neurosurgery. 1991;28:180-186.
34 Haro H, Domoto T, Maekawa S, et al. Resorption of thoracic disc herniation. J Neurosurg Spine. 2008;8:300-304.
35 Ogilivie JW. Thoracic disc herniation. In: Bridwell KH, DeWold RL, editors. Textbook of Spinal Surgery. Philadelphia: JB Lippincott; 1991:711-718.
36 Kim KD, Babbitz JD, Mimbs J. Imaging-guided costotransversectomy for thoracic disc herniation. Neurosurg Focus. 2000;9(4):E7.
37 Johnson JP, Stokes JK, Oskouian RJ. Image-guided thoracoscopic spinal surgery: a merging of 2 technologies. Spine. 2005;30:572-578.
38 Bennett MH, McCallum JE. Experimental decompression of spinal cord. Surg Neurol. 1977;8:63-67.
39 Doppman JL, Girton M. Angiographic study of the effect of laminectomy in the presence of acute anterior epidural masses. J Neurosurg. 1976;45:195-202.
40 Kalfas I. Laminectomy for thoracic spinal canal stenosis. Neurosurg Focus. 2000;9(4):E2.
41 Singounas EG, Karvounis P. Thoracic disc protrusion. Acta Neurochir (Wien). 1979;49:245-254.
42 Jho HD. Endoscopic transpedicular thoracic discectomy. Neurosurg Focus. 2000;9(4):E4.
43 Sheikh H, Samartizis D, Perez-Cruet MJ. Techniques for the operative management of thoracic disc herniation: minimally invasive thoracic microdiscectomy. Orthop Clin North Am. 2007;38(3):351-361.
44 Hulme A. The surgical approach to thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry. 1960;23:133-137.
45 Lifshutz J, Lidar Z, Maiman D. Evolution of the lateral extracavitary approach to the spine. Neurosurg Focus. 2004;16(1):E12.
46 McCormick WE, Will SF, Benzel EC. Surgery for thoracic disc disease. Complication avoidance: overview and management. Neurosurg Focus. 2000;9(4):13.
47 Lidar Z, Lifshutz J, Bhattacharjee S, et al. Minimally invasive, extracavitary approach for thoracic disc herniation: technical report and preliminary results. Spine J. 2006;6:157-163.
48 Vollmer DG, Simmons NE. Transthoracic approaches to thoracic disc herniations. Neurosurg Focus. 2000;9(4):E8.
49 Rodts GEJr, Haid RWJr, Foley KT. Ventral and lateral thoracic and lumbar fixation techniques. In: Benzel EC, editor. Spine Surgery: Techniques, Complication Avoidance, and Management. New York: Churchill Livingston; 1999:1023-1037.
50 Abbot KH, Retter RH. Protrusions of thoracic intervertebral disks. Neurology. 1956;6:1-10.
51 Oskouian RJ, Johnson JP. Endoscopic thoracic microdiscectomy. J Neurosurg Spine. 2005;3:459-464.
52 Oskouian RJ, Johnson JP. Endoscopic thoracic microdiscectomy. Neurosurg Focus. 2005;18(3):E11.
53 Johnson JP, Filler AG, McBride DQ. Endoscopic thoracic discectomy. Neurosurg Focus. 2000;9(4):E11.
54 Mack MJ, Regan JJ, Bobechko WP, et al. Application of thorascopy for diseases of the spine. Ann Thorac Surg. 1993;56:736-738.
55 Regan JJ, Mack MJ, Picetti GDIII, et al. A comparison of video assisted thoracoscopic surgery (VATS) with open thoracotomy in thoracic spinal surgery. Todays Ther Trends. 1994;11:203-218.
56 Rosenthal D, Marquardt G, Lorenz R, et al. Anterior decompression and stabilization using a microsurgical endoscopic technique for metastatic tumors of the thoracic spine. J Neurosurg. 1996;84:565-572.
57 Hott JS, Feiz-Erfan I, Kenny K, et al. Surgical management of giant herniated thoracic discs: analysis of 20 cases. J Neurosurg Spine. 2005;3:191-197.
58 Bartels RH, Peul WC. Mini-thoracotomy or thorascopic treatment for medially located thoracic herniated disc. Spine. 2007;32:581-584.
59 Aizawa T, Sato T, Sasaki H, et al. Results of surgical treatment for thoracic myelopathy: minimum 2-year follow-up study in 132 patients. J Neurosurg Spine. 2007;7:13-20.
60 Maiman DJ, Pintar FA. Anatomy and clinical biomechanics of the thoracic spine. Clin Neurosurg. 1991;38:296-324.
61 Dickman CA, Rosenthal D, Regan JJ. Reoperation for herniated thoracic discs. J Neurosurg Spine. 1999;91:157-162.
62 Bohlman HH, Zdeblick TA. Anterior excision of herniated thoracic discs. J Bone Joint Surg Am. 1988;70:1038-1047.
63 Dickman CA, Theodore N, Hurlbert RJ, et al. Thoracic disc [letter]. J Neurosurg. 1996;85:187.
64 El-Kalliny M, Tew JMJr, Van Loveren H, et al. Surgical approaches to thoracic disc herniations. Acta Neurochir. 1991;111:22-32.
65 Stillerman CB, Chen TC, Couldwell WT, et al. Thoracic disc [letter]. J Neurosurg. 1996;85:189-190.