Chapter 4 Transport of the critically ill
All intensive care units (ICUs) are required to move critically ill patients for investigations or procedures that cannot be performed in the ICU. These patients have reduced or absent physiological reserves and even short trips can result in significant adverse events.1,2 These events can be reduced by the use of trained personnel.3,4
In addition, ICU personnel are frequently involved in the stabilisation and transfer of critically ill patients into an ICU,5 and some units may be involved in the transport of patients from the site of a prehospital incident, or between hospitals.6,7 The interhospital transfer could be due to the increasing sophistication of critical care facilities in tertiary hospitals compared with district or rural hospitals, different subspecialty capabilities, local bed shortages3 or, in certain health systems, for insurance or financial reasons. In some cases, the complexity of these interhospital transfers can be further complicated by the need for rapid transport, or the distances involved. All patient movement is associated with an increase in mortality or morbidity, but with an integrated approach using high-level clinical personnel who have the correct equipment and undertake sufficient planning, adverse events can be reduced.3,4,6–8 Regular ambulances or untrained hospital staff should not be expected to manage ICU patients. Compared with specialist transport teams, standard ambulances with junior doctor escorts are associated with more cases of hypotension, acidosis and death.9
The hospital of the future has been described as the critical care hub of a dispersed network of facilities linked by information systems and critical care transport services.10 Critical care transport should be part of a regional intensive care network and adhere to promulgated minimum standards for transport of the critically ill.11,12
INTERHOSPITAL TRANSPORT
COMPUTED TOMOGRAPHY SCANNING
The most common diagnostic investigation necessitating transport is computed tomography (CT). On most occasions very little planning and preparation is required for what is almost a routine procedure. The exceptions are patients with head injuries, the administration of nasogastric contrast and the increased aspiration risk in patients with decreased gastric motility. Repeated CT scanning of head-injury patients is common. In those patients with decreased cerebral compliance, movement and changes in body position or PaCO2 can result in marked changes in intracranial pressure (ICP). Prior to transport, EtCO2 should be measured on the transport monitor while the patient remains connected to the ICU ventilator. ICP changes caused by ventilator-induced variations in PaCO2 when switching to the transport ventilator can be reduced by adjusting the minute volume to maintain a stable EtCO2. Adequate sedation will also decrease movement-induced rises in ICP. Ideally, the ICP should be measured on the transport monitor but this is often not possible. Whether a staff member remains in the scanner room or views the patient and monitor from outside depends on patient stability. Radiation exposure is small and is not considered a risk, and depends on where personnel stand in relation to the scanner’s ‘doughnut’, from where the radiation is emitted.
MAGNETIC RESONANCE IMAGING SCANNING
MRI units vary in policy, from prohibiting any equipment in the room to having minimal equipment that is placed as far away from the magnet as possible. The ability of ventilators and infusion pumps to function in the MRI scan room must have been tested prior to any patient being scanned, as some modern transport ventilators have failed in the MRI. Ideally, the equipment should be left outside the room with extensions added to the infusion and ventilator tubing, but this increases the risk of disconnection. There is one reported case of the external part of a pulmonary artery catheter burning through during an MRI scan,16 probably caused by the development of radiofrequency eddy currents. Thermodilution pulmonary artery catheters are probably safe, but although patients with internal defibrillators and permanent pacemakers have been scanned with no consequence, deaths have been reported. Prior discussion with individual MRI units on how ICU patients can be scanned is required.
INTERHOSPITAL TRANSPORT
ORGANISATIONAL ASPECTS
Provision of critical care transport services needs to be a part of regional ICU services. The staffing of critical care transport teams will depend on the workload, with around 300 per year being the threshold for a specific transport roster, depending on transport duration and regulations affecting duty times. Other factors include regional demographics, resources and geography. A team from within that unit, or from another ICU, or an emergency department, or a stand-alone transport service may provide transport of patients to a particular ICU. The merits of each system have been summarised.17 Whatever arrangement is chosen, staff should not be conscripts but selected from those interested in critical care transport, and should be appropriately trained. Use of junior inexperienced staff is associated with increases in preventable mortality and morbidity.18,19 Rostering of teams needs to be appropriate for the workload and take into account the potential for significant overtime hours when urgent requests occur near shift changeovers. If personnel are also allocated to other clinical duties, they need to be readily relieved when required. Equipment should be prechecked and the team should have a practised routine to enable prompt departure.
A coordination centre should be used in systems involving multiple requests and transport teams.
PERSONNEL
The aim of the transport team is at least to maintain but preferably to enhance the level of care. This requires transport teams to have diagnostic and procedural skills to provide the full complement of care for the full range of patients transported. Ideally, the personnel caring for the patient in transit should be equivalent to the ‘front-line’ clinical team at the destination, implying a physician-based team, although transport of well-stabilised patients by non-physician teams has been reported.20
The transport team should be a minimum of two people. For multiple patients a formula of n + 1 personnel for n critical patients has been suggested.21 Multidisciplinary teams of physicians, nurse and/or ambulance officers offer advantages of a wider range of skills and training than a team from any single profession. In certain circumstances, other specialised staff may need to be taken, for example a surgeon or obstetrician.6 It is preferable and safer to add a specialist to the standard team because of the latter’s familiarity with the practicalities of the transport environment. Other desirable attributes in staff include: good teamwork and communication skills; adaptability; reasonable body habitus and physical condition; and no significant visual or auditory impairment or susceptibility to motion sickness. Travel sickness medications such as hyoscine (scopolamine) are of limited value, needing to be taken up to 4 hours pretransport and possibly causing significant side-effects.22
PATIENT SELECTION
Both receiving hospitals and ambulance services need to be alert to possible cases where critical care transport is indicated, but not identified by the referring team. A mechanism that is highly sensitive and specific at identifying patients unsuitable for standard ambulance transport is required. Triage mechanisms and tables to aid in patient selection have been described.23,24
COMMUNICATIONS
A systematic approach is necessary to ensure a smooth response when the need for transport of a critically ill patient is identified. A single toll-free telephone number with conference call capability is the ideal. Facsimile and teleradiology capabilities may also be of value. The one call for assistance should result in the provision of clinical advice if required, the dispatch of a transport team, and finding a bed in an appropriate hospital. Concise, simple clinical advice appropriate for the capabilities of the referring hospital by either the receiving hospital or the transport service is paramount. No matter how fast the transport team’s response, without some interim care the patient with major airway, breathing or circulatory compromise will not survive.6,7 Ongoing advice, including stabilisation and preparation of the patient for transport, may be required prior to the arrival of the transport team. The provision to referring hospitals of a checklist for patient management and preparation for transport may assist.
EQUIPMENT
GENERAL CONSIDERATIONS
Minimum standards for supplies, equipment and monitoring for critical care transport have been developed.10,17 Equipment selection is a compromise between providing for every conceivable scenario and being mobile. The aim should be to have a core set of equipment plus optional items for specific scenarios plus some back-up redundancy for vital supplies and equipment such as oxygen, airway devices and basic circulatory monitoring. A suggested equipment schedule is given in Table 4.1. Meticulous checking of equipment after each use and on a regular basis is essential.
Table 4.1 Suggested equipment schedule for interhospital critical care transport
| Respiratory equipment |
| Intubation kit |
| Endotracheal tubes and connectors – adult and paediatric sizes |
| Introducers, bougies, Magill forceps |
| Laryngoscopes, blades, spare globes and batteries |
| Ancillaries: cuff syringe and manometer, clip forceps, ‘gooseneck’ tubing, heat moisture exchanger/filter(s), securing ties, lubricant |
| Alternative airways: |
| Simple: Guedel and nasopharyngeal |
| Supraglottic: laryngeal masks and/or Combitube |
| Infraglottic: cricothyrotomy kit and tubes |
| Oxygen masks (including high-FiO2 type), tubing, nebulisers |
| Suction equipment: |
| Main suction system – usually vehicle-mounted |
| Spare (portable) suction – hand, O2 or battery-powered |
| Suction tubing, handles, catheters and spare reservoir |
| Self-inflating hand ventilator, with masks and positive end-expiratory pressure (PEEP) valve |
| Portable ventilator with disconnect and overpressure alarms |
| Ventilator circuit and spares |
| Spirometer and cuff manometer |
| Capnometer/capnograph. |
| Pleural drainage equipment: |
| Intercostal catheters and cannulae |
| Surgical insertion kit and sutures (see below) |
| Heimlich-type valves and drainage bags |
| Main oxygen system (usually vehicle-mounted) of adequate capacity with flowmeters and standard wall outlets |
| Portable/reserve oxygen system with flowmeter and standard outlet |
| Circulatory equipment |
| Defibrillator/monitor/external pacemaker, with leads, electrodes and pads |
| Intravenous fluid administration equipment: |
| Range of fluids: isotonic crystalloid, dextrose, colloids |
| High-flow and metered-flow giving sets |
| Intravenous cannulae in range of sizes: peripheral and central/long lines |
| Intravenous extension sets, three-way taps and needle-free injection system |
| Syringes, needles and drawing-up cannulae |
| Skin preparation wipes, intravenous dressings and BandAids |
| Pressure infusion bags (for arterial line also) |
| Blood pressure-monitoring equipment: |
| Arterial cannulae with arterial tubing and transducers |
| Invasive and non-invasive (automated) blood pressure monitors |
| Aneroid (non-mercury) sphygmomanometer and range of cuffs (preferably also compatible with non-invasive arterial blood pressure) |
| Pulse oximeter, with finger and multisite probes |
| Syringe/infusion pumps (minimum 2) and appropriate tubing |
| Miscellanous equipment |
| Urinary catheters and drainage/measurement bag |
| Gastric tubes and drainage bag |
| Minor surgical kit (for intercostal catheter, central venous lines, cricothyrotomy, etc.): |
| Sterile instruments: scalpels, scissors, forceps, needle holders |
| Suture material and needles |
| Antiseptics, skin preparation packs and dressings |
| Sterile gloves (various sizes); drapes ± gowns |
| Cervical collars, spinal immobilisation kit, splints |
| Pneumatic antishock garment (military antishock trousers (MAST) suit) |
| Thermometer (non-mercury) and/or temperature probe/monitor |
| Reflective (space) blanket and thermal insulation drapes |
| Bandages, tapes, heavy-duty scissors (shears) |
| Gloves and eye protection |
| Sharps and contaminated waste receptacles |
| Pen and folder for paperwork |
| Torch ± head light |
| Drug/additive labels and marker pen |
| Nasal decongestant (for barotitis prophylaxis) |
| Pharmacological agents |
| Central nervous system drugs: |
| Narcotics ± non-narcotic analgesics |
| Anxiolytics/sedatives |
| Major tranquillisers |
| Anticonvulsants |
| Intravenous hypnotics/anaesthetic agents |
| Antiemetics |
| Local anaesthetics |
| Cardiovascular drugs: |
| Antiarrhythmics |
| Anticholinergics |
| Inotropes/vasoconstrictors |
| Nitrates |
| α- and β-blockers; other hypotensives |
| Electrolytes and renal agents: |
| Sodium bicarbonate |
| Calcium (chloride) |
| Magnesium |
| Antibiotics |
| Oxytocics |
| Potassium |
| Loop diuretics |
| Osmotic diuretics |
| Endocrine and metabolic agents: |
| Glucose (concentrate) ± glucagon |
| Insulin |
| Steroids |
| Other agents: |
| Neuromuscular blockers: depolarising and non-depolarising |
| Anticholinesterases (neuromuscular block reversal) |
| Narcotic and benzodiazepine antagonists |
| Bronchodilators |
| Antihistamines |
| H2-blockers/proton pump inhibitors |
| Anticoagulants |
| Thrombolytics |
| Vitamin K |
| Tocolytics |
| Diluents (saline and sterile water) |
| Additional/optional equipment |
| Transvenous temporary pacing kit and pacemaker |
| Blood (usually O negative) and/or blood products |
| Additonal infusion pumps and associated intravenous sets |
| Obstetrics kit |
| Additional paediatric equipment (depending on capability of basic kit) |
| Antivenene (polyvalent or specific) |
| Specific drugs or antagonists |
Transport monitors, infusion pumps and ventilators must work outside the transport vehicle. This requires equipment to be battery-powered and readily portable. Although newer monitors and other devices have rechargeable batteries with improved endurance, problems can still occur. The equipment-checking process includes different charging regimes. Nickel cadmium (NiCad) batteries need to be fully discharged before recharging to decrease memory effect, which reduces endurance, whereas sealed lead–acid or lithium batteries perform best when continually charged between uses.25
Portability can be addressed in two ways. Equipment can be vehicle-mounted but readily detachable to accompany the patient, either as individual devices or more conveniently as a modular unit.26 Alternatively, a mobile intensive care module can be incorporated into the stretcher, either in the base27 or as a ‘stretcher bridge’ straddling the patient.28 Such designs are now widely used and allow the patient and equipment to be assembled into one unit at the referral point; this reduces loading and unloading time, ventilator and other device disconnections, and the risk of leaving equipment behind. Minor disadvantages include the increase in weight (25–30 kg), with corresponding reduction in maximum patient weight, and slight top-heaviness of the stretcher/patient combination.
MONITORING
Clinical observation by experienced personnel remains the mainstay of monitoring,10 but some clinical assessments such as auscultation are impossible during transit. Hence monitoring by appropriate equipment should be at the same level or a higher level than what the patient receives in the stationary setting. Referring institutions should not allow patients to be transported by teams with inferior monitoring capability. Compact transport monitors offering electrocardiogram (ECG), SpO2, non-invasive and multichannel invasive pressures, capnography and temperature monitoring have largely superseded older techniques, such as systolic pressure estimation by palpation and mean arterial pressure monitoring via an aneroid interface and gauge. These older techniques can still be used for back-up, as can defibrillators for ECG, while small hand-held pulse oximeters and EtCo2 detector are also available. Non-invasive blood pressure and pulse oximetry devices are susceptible to artefact29,30 and the use of invasive arterial monitoring or shielding pulse oximetry probes may be required. Mercury-containing devices are unsuitable, especially in aircraft. For longer transports, or patients with major biochemical or respiratory disturbances, compact biochemical and blood gas analysers may be valuable.31
VENTILATION AND RESPIRATORY SUPPORT
A mechanical ventilator should be used on all ventilated patients during transport. Manual ventilation occupies one team member fully and cannot reliably deliver constant tidal volumes and stable EtCo2.32 Transport ventilators are a compromise between portability and features.
The characteristics of an ideal transport ventilator are outlined in Table 4.2. No currently available transport ventilator meets all of these, and different models are optimised for different scenarios, so selection of a transport ventilator should take into account likely clinical and operational requirements. Back-up manual ventilation equipment must be available. In some cases of severe respiratory disease, a standard ICU ventilator may be needed. This may require medical air and AC power, although newer hybrid ICU/transport ventilators can provide enhanced ventilation capability without supply of these.33 Similar requirements will apply to transport of patients on extracorporeal membrane oxygenation.
The provision of continuous positive airways pressure (CPAP) in transport remains problematic. ‘Clapperboard’-type systems are economical on gas consumption, but being gravity-driven perform poorly during movement. Conventional CPAP systems have extremely high gas consumption, rendering them impractical except for short road transports. Electronically triggered CPAP is a feature of some newer transport ventilators; however, though they have been successfully used on occasions, poor performance with mask CPAP has been reported,34 and some patients may need to be converted to synchronised intermittent mandatory ventilation or intermittent positive-pressure ventilation (IPPV) for transport.
Maintenance of humidification of inspired gases is important during transport. In most cases, heat and moisture exchangers should provide adequate protection for intubated patients.35 In special circumstances, for example, in neonates and cystic fibrosis patients, it may be necessary to use active humidification.
A suction system and preferably a reserve are needed during all phases of transport. These may be Venturi systems, electrical-powered pumps or manual aspirators. Oxygen Venturi systems are lighter than electrical systems and outperform manual aspirators, but have high oxygen consumption, > 40 l/min.36
MISCELLANEOUS EQUIPMENT
Transcutaneous pacing is adequate in an emergency, or during very short transports, but in other circumstances elective transvenous pacing should be instituted. Equipment to institute or maintain other specialised therapy en route should be carried if required. In some situations, such as with an intra-aortic balloon pump, the equipment may be bulky and can influence the selection of the transport vehicle.37
MODE OF TRANSPORT
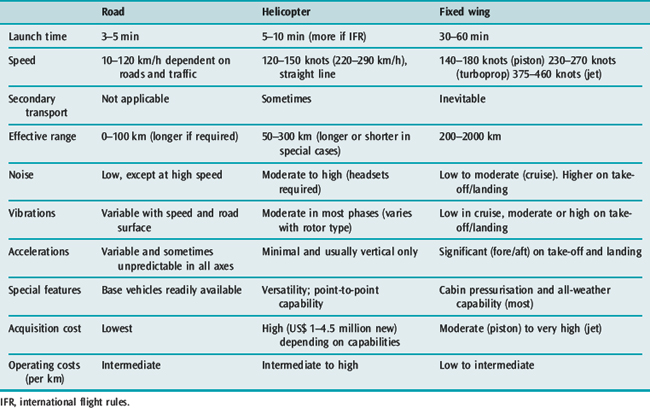
Three types of transport vehicle are commonly employed: road, aeroplane (fixed-wing), and helicopter (rotary-wing). Basic requirements for critical care transport vehicles are listed in Table 4.3. Ideally, dedicated vehicles for all transport modes should be used, but the workload may not justify this and often vehicles that can be readily converted for mobile ICU use are seconded as required. The mode of transport depends on distances involved between referring and receiving hospitals and transport team locations; it also depends on the urgency of the case, which is often influenced by the clinical capability of the referring centre. Guidelines for vehicle utilisation should be developed but should have some flexibility for special circumstances, e.g. workload, traffic congestion, weather. Features and limitations of different modes of transport are summarised in Table 4.4.
ROAD TRANSPORT
The ground ambulance remains the most commonly used critical care vehicle. With patients for whom time is not critical and level of care in transit is more important than speed, road transport over considerable distances is feasible and may be safer in some patient groups.38
SAFETY AND TRAINING
Transport by any mode involves risk to staff and patients, and also imposes limitations on the delivery of care. In the aeromedical environment unfamiliar personnel perform clinical tasks poorly,39 so teams must be appropriately trained and equipped to function effectively and safely in each mode of transport. They need to be familiar with use of the various transport vehicles’ oxygen, suction, medical power, communications systems, and other equipment and stores. A senior member of their own professional group should train and accompany new personnel for several missions. Other specialist staff added to a team should receive a thorough safety brief and work under the direction of regular transport team members. Aeromedical crew training should encompass safety equipment, crash response, emergency egress and survival. Safety should be a foremost consideration in any transport. Activities that compromise road and air safety such as hazardous driving or flying below safe minima are not acceptable, and clinical teams must avoid attempting to coerce drivers or pilots to take risks. This has been recognised as a contributor to air ambulance accidents.40
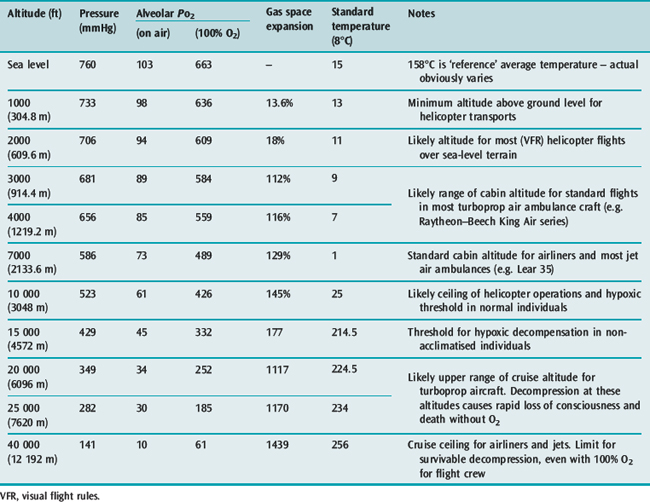
ALTITUDE AND TRANSPORT PHYSIOLOGY
All transport modes result in increased noise, vibration, turbulence and accelerations in various or all axes (see Table 4.4). Personnel need to be aware of altitude-related complications that can occur with air transport. Increasing altitude results in decreasing oxygen partial pressure in accordance with Dalton’s law; while gas volumes increase or where volume change is restricted, relative increases in pressure occur in accordance with Boyle’s law (Table 4.5). Good introductory41,42 and more detailed43,44 aviation physiology texts are available.
OXYGENATION AND HYPOXIA
Critical patients who are already dependent on an increased FiO2 will be compromised by reduction in atmospheric pressure. Further oxygen supplementation will be required to maintain arterial PaO2. Only in special or unexpected circumstances, for example, alpine helicopter operations or cabin decompression, would hypoxia be expected to affect the medical crew; however, they should be aware of the risk and be alert to symptoms. The manifestations of hypoxia are well described elsewhere.37–40
GAS EXPANSION
Air-containing equipment includes: endotracheal and tracheostomy tube cuffs; Sengstaken–Blakemore tubes; pulmonary artery catheter balloons; air splints, pneumatic antishock garments (military antishock trousers (MAST) suit); and pleural, gastric and some wound drainage bags. Endotracheal cuff pressures need to be adjusted during flight, or filled with water. Increases in tidal volume in pneumatically controlled ventilators can occur with altitude, necessitating setting changes.45
CABIN PRESSURISATION
Most fixed-wing air ambulances have pressurised cabins, which decreases hypoxia and gas expansion. The pressurisation creates a cabin pressure equivalent to flying at a lower altitude, hence the term ‘cabin altitude’. The maximum pressure differential that can be generated depends on the aircraft model. Most turboprop air ambulances can provide around 350 mmHg (46.7 kPa) differential, or cabin altitude of 1000 m (3000 ft) while flying at 6500 m (20 000 ft). Once maximum differential has been achieved, lower cabin altitude can only be provided by lower flight, which may be relatively or absolutely contraindicated – for example, a slower more turbulent flight or beneath lowest safe altitude, respectively. The medical team should not request a lower cabin altitude than what is required, with the final decision resting with the pilot. Failure of cabin pressurisation is rare, but if sudden can have dramatic consequences, and teams should be aware of procedures to follow.
OTHER CONSIDERATIONS
Temperature falls by 2°C for every 300 m (1000 ft) altitude increase. Water partial pressure also falls and is not corrected by cabin pressurisation. Respiratory and other exposed mucosa can become dehydrated and could eventually lead to systemic hypovolaemia. All intubated patients should have at least passive humidification. On prolonged journeys, staff may also be affected. Staff rostered for air transport should refrain from compressed-gas diving for at least 24 hours prior to the shift.46
PATIENT PREPARATION FOR TRANSPORT
Appropriate documentation, including a referral letter, results of investigations and hospital and ambulance observations, needs to accompany the patient. The team should ensure that any relevant legal requirements have been complied with and, where possible, consent for transport obtained.47 The final step prior to transport should be a series of checks, as listed in Table 4.6.
| A. Before leaving hospital | |
| Patient identity and next of kin | Recorded |
| Consent for transport | Obtained and documented |
| Paperwork and X-rays | Collected |
| Drugs for transport | Present and sufficient |
| Emergency drugs/equipment | Available |
| Medical equipment | Collected and repacked |
| Monitors, ventilator and infusions | Connected and on |
| Tubes, lines, drains and catheters | Secured |
| Altitude request (if applicable) | Passed to pilot |
| Receiving unit | Contacted and updated |
| B. In-vehicle and predeparture | |
| Stretcher and patient restraints | Secured and checked |
| Oxygen supply | On and sufficient |
| Monitors, ventilator and infusions | Working and secure |
| Emergency drugs/equipment | Stowed and accessible |
| Other medical packs | Stowed |
| Intravenous fluids | Hung and running |
| Intravenous injection port | Accessible |
| Medical power | On and connected |
| Communications | Checked as applicable |
| Seatbelts | On and checked |
| Staff/patient headsets | On/checked (if applicable) |
PATIENT CARE DURING TRANSPORT
If the patient is adequately prepared this phase should be uneventful. Special vigilance should be employed in the initial stages of movement, as this is the most likely time for either physiological decompensation or technical problems such as disconnections to occur. Once in the transport vehicle, a further set of checks is advisable (see Table 4.6). Therapy, monitoring and documentation should continue during transport. Transported patients are vulnerable to hypothermia, especially if intubated and/or paralysed and/or receiving multiple infusions.2,48 Active heating in transit may be possible using the vehicle heating, while passive heat conservation should be practised during loading and unloading. Transport crews should be restrained during transport. If a critical event occurs necessitating the crew leaving their seats, the driver or pilot should be informed.
Death in transport should be a rare occurrence.6,7 If it does occur, distance and the expectations and location of relatives should be taken into account in making the decision whether or not to continue transport to the destination. Carriage of relatives remains a controversial issue. For conscious patients, especially children, the presence of family members may have a beneficial effect. For unconscious patients it is less clear and needs to be balanced against space constraints in the mobile ICU vehicle, and the potential reaction of relatives in case of a critical event. Transport services should have policies in place both for carriage of relatives and for death in transit.
QUALITY ASSURANCE IN EDUCATION AND RESEARCH
Critical care transport is a recent development where accepted standards and guidelines are still evolving.49 This means there is still considerable likelihood of problems, errors and critical incidents, with corresponding scope for research and quality improvement. This requires good clinical and operational data collection and patient outcomes. The process should be sensitive to the existence of system errors as well as individual patient, equipment or staff incidents. Preliminary results from the use of a critical incident monitoring system have been reported.13 Users of the service must be informed of recommendations and system changes resulting from this process. Innovation and research by staff involved in this area should be encouraged.
SPECIAL TRANSPORT SITUATIONS
PERINATAL TRANSPORT
This encompasses both in utero and extrauterine transport of the neonate. Specialised neonatal teams normally perform neonatal transport.50 Alternatively, part or all of the regular transport team may accompany specialist neonatal personnel. Neonatal transport stretchers are bulky and heavy, and require a vehicular power output of up to 250 W for the incubator and active humidifier as well as monitors, ventilator and infusion pumps. They also require a supply of medical air to allow precise regulation of FiO2.51 Transport of the pregnant patient carries the risk of precipitating labour, and in rare cases, delivery in transit.52 This is suboptimal, especially where the baby is premature or otherwise at risk. Where labour cannot be suppressed, consideration should be given to delivery at the referring hospital, with subsequent neonatal and maternal transport.
TRANSPORT OF DIVING-INJURY PATIENTS
Patients with decompression sickness or arterial gas embolus require expeditious transport to a recompression facility. This must be balanced against the risk of even small decreases in ambient pressure; even a 10-m (30-ft) increase in altitude can exacerbate pathogenesis.42 Divers with other problems such as marine animal envenomation or other medical conditions will still have increased total body nitrogen stores and can be at risk of developing evolved gas disorders during air transport. The use of transportable hyperbaric chambers has been reported53 but their use severely compromises speed of response, and therapy possible in transit. Transport at or very near sea-level cabin pressure on 100% oxygen is the usual procedure.
INTERNATIONAL AND LONG-DISTANCE TRANSPORTS
International transport of critically ill patients is becoming increasingly common. There are often complex medical, social and economic factors for returning patients to their own medical system. These must be balanced against the immigration, visa and logistic requirements, and medical problems of ultralong-distance transport.54 A physician-based team is less likely to have problems relating to drug carriage and status compared with a paramedical team. Logistic problems include carriage of sufficient supplies, and clinical staff to work shifts for prolonged transports. Pressure may be exerted to utilise cheaper regular passenger transport services instead of much more expensive air ambulances. Most international airlines will accept a stable seated patient, but there is considerable variation among airlines willing to carry stretcher patients and associated equipment. Such transports require considerable planning to arrange stretcher fitment and sufficient supplies of oxygen and electric power. A separate oxygen system for critical care transports is required as the aircraft’s emergency oxygen system is not permitted for patient care and the oxygen systems for in-flight use by passengers with medical conditions can only deliver up to 4 l/min.50 Airline engineering clearance of medical equipment is often required. Aircraft power needs to be negotiated or sufficient batteries carried. An air ambulance may be indicated for cases that are urgent, infective or require low cabin altitude, whereas stable post myocardial patients can be safely transported in commercial aircraft with appropriate escorts.55
CRITICAL CARE SCENE RESPONSES
Critical care teams offer a wide range of measures to complement standard prehospital providers, especially for major trauma, including: sedative/relaxant-assisted intubation; cricothyrotomy; tube thoracostomy; intravenous cutdown or central line insertion; and blood administration, as well as triage to an appropriate hospital.56 These teams are only useful for trapped patients in the urban setting,57 but combined with helicopter transport can improve outcomes in rural patients with blunt trauma.56,58,59 In these situations the team should include an experienced prehospital provider. With appropriate activation the team may reach the patient at the scene or supplement management at the local hospital.
Critical care teams may also be of value in disaster situations.60 Disaster medicine involves a change in emphasis to performing a small number of basic life-saving procedures on a large number of patients. Personnel with transport/prehospital experience are likely to be better trained and equipped to work at disaster scenes than traditional hospital disaster teams.61 The order of priority remains the same as traditional critical care transport: triage, treatment and then transport.
1 Braman S, Dunn S, Amico CA, et al. Applications of intrahospital transport in critically ill patients. Ann Intern Med. 1987;107:469-473.
2 Ridley S, Carter R. The effects of secondary transport on critically ill patients. Anaesthesia. 1989;44:822-827.
3 Duke GJ, Green JV. Outcome of critically ill patients undergoing interhospital transfer. Med J Aust. 2001;174:122-125.
4 Edge WE, Kantar RK, Weigle CG, et al. Reduction of morbidity in interhospital transport by specialised paediatric staff. Crit Care Med. 1994;22:186-191.
5 Hourihan F, Bishop G, Hillman KM, et al. The medical emergency team: a new strategy to identify and intervene in high risk patients. Clin Int Care. 1995;6:269-272.
6 Gilligan JE, Griggs WM, Jelly MT, et al. Mobile intensive care services in rural South Australia. Med J Aust. 1999;171:617-620.
7 Havill JH, Hyde PR, Forrest C. Transport of the critically ill: example of an integrated model. NZ Med J. 1995;108:378-380.
8 Flabouris A. Patient referral and transportation to a regional tertiary ICU: patient demographics, severity of illness and outcome comparison with non-transported patients. Anaesth Intens Care. 1999;27:385-390.
9 Bellingan G, Olivier T, Batson S, et al. Comparison of a specialist retrieval team with current United Kingdom practice for the transport of critically ill patients. Intens Care Med. 2000;26:740-744.
10 Goldsmith JC. The US health care system in the year 2000. JAMA. 1986;256:3371-3375.
11 Joint Faculty of Intensive Care, Australian and New Zealand College of Anaesthetists, and Australasian College of Emergency Medicine. Policy document IC10. Minimum Standards for Transport of Critically Ill Patients, 2003. Available online at www.anzca.edu.au/jficm/resources/policy/ic10_2003
12 Commission on Accreditation of Medical Transport Systems. Accreditation Standards. CAMTS: Anderson, SC, 1997.
13 Waydhas C. Intrahospital transport of critically ill patients. Crit Care. 1999;3:R83-R89.
14 Predictors of respiratory function deterioration after transfer of critically ill patients. Intens Care Med. 1998;24:1157-1162.
15 Kollef MH, Von Harz B, Prentice D, et al. Patient transport from intensive care increases the risk of developing ventilator-associated pneumonia. Chest. 1997;112:765-773.
16 ECRI. A new MRI complication. In Health Devices Alert. ECRI; 1988.
17 Flabouris A, Seppelt I. Optimal interhospital transport systems for the critically ill. In: Vincent JL, editor. 2001 Yearbook of Intensive Care and Emergency Medicine. Berlin: Springer-Verlag; 2001:647-660.
18 Deane SA, Gaudry PL, Woods WPD, et al. Interhospital transfer in the management of acute trauma. Aust NZ J Surg. 1990;60:441-446.
19 Gentleman D, Jennett B. Hazards of interhospital transfer of comatose head injured patients. Lancet. 1981;2:853-855.
20 Beyer AJIIIrd, Land G, Zaritsky A. Non-physician transport of intubated paediatric patients: a system evaluation. Crit Care Med. 1992;20:961-966.
21 International Society of Aeromedical Services Australasian chapter. Aeromedical Standards. Arncliffe, Sydney: ISAS Australasia, 1993.
22 Benson AJ. Motion sickness. In: Ernsting J, King PF, editors. Aviation Medicine. Butterworth-Heinemann: Oxford; 1988:318-338.
23 Lee A, Lum ME, Beehan SJ, et al. Interhospital transfers: decision making analysis in critical care areas. Crit Care Med. 1996;24:618-623.
24 New South Wales Health Department/Ambulance Service. Guidelines for Retrieval of the Critically Ill. Sydney: NSW Health Department, 1995.
25 Gates Energy Products Technical Marketing Staff. Rechargeable Batteries Applications Handbook. Stoneham, MA: Butterworth-Heinemann, 1992.
26 Noy-Man Y, Papa MZ, Margaliot SZ. Portable air mobile life support unit. Aviat Space Environ Med. 1985;56:598-600.
27 Grant-Thompson JC. The Mobile Intensive-care Rescue Facility (MIRF): a close look at the intensive care aeromedical evacuation capability. US Army Med Dept J. 1997;Sept–Oct:23-26.
28 Wishaw KJ, Munford BJ, Roby HP. The Care Flight stretcher bridge: a compact mobile intensive care module. Anaesth Intens Care. 1990;18:234-238.
29 Rutten AJ, Isley AH, Skowronski GA, et al. A comparative study of mean arterial blood pressure using automatic oscillometers, arterial cannulation, and auscultation. Anaesth Intens Care. 1986;14:58-65.
30 Lawless ST. Crying wolf: false alarms in a paediatric intensive care unit. Crit Care Med. 1994;22:981-985.
31 Hankins DG, Herr DM, Santrach PJ, et al. Utilisation of a portable clinical analyser in air rescue. In: ADAC/International Society of Aeromedical Services AIRMED 96 Congress Report. Munich: Wolfsfellner Medizin Verlag; 1997:109-111.
32 Erler CJ, Rutherford WF, Rodman G, et al. Inadequate respiratory support in head injury patients. Air Med J. 1993;12:223-226.
33 Wong LS, McGuire NM. Laboratory assessment of the Bird T–Bird VS ventilator performance using a model lung. Br J Anaesth. 2000;84:811-817.
34 Porges KJ, Kelly SL. A comparison of the imposed work of breathing in continuous positive pressure ventilation mode between three different ventilators. Emerg Med. 1999;1:111-117.
35 Hedley RM, Allt-Graham J. Heat and moisture exchangers and breathing filters; a review. Br J Anaesth. 1994;73:227-236.
36 Russell WJ. Venturi suction. In Equipment for Anaesthesia and Intensive Care, 2nd edn., Adelaide, SA: WJ Russell; 1997:27-29.
37 Mertlich G, Quaal SJ. Air transport of the patient requiring intra-aortic balloon pumping. Crit Care Nursing Clin North Am. 1989;1:443-458.
38 Schneider NS, Borok Z, Heller M, et al. Critical cardiac transport: air versus ground. Am J Emerg Med. 1988;6:449-452.
39 Harris BH. Performance of aeromedical crew members: training or experience? Am J Emerg Med. 1986;4:409-413.
40 National Transportation Safety Board (US) Safety Study: Commercial Emergency Medical Services Helicopter Operations. USA: NTSB, 1988. SS/88/01
41 Blumen IJ, Callejas S. Transport and physiology: a reference for air medical personnel. In: Blumen IJ, Lemkin DL, editors. Principles and Direction of Air Medical Transport. Salt Lake City, UT: Air Medical Physician Association; 2003:357-377.
42 Martin TE, Rodenberg HD. The physiological effects of altitude. In: Martin TE, Rodenberg HD, editors. Aeromedical Transportation: A Clinical Guide. Aldershot, UK: Avebury Aviation; 1996:37-54.
43 De Hart RL, editor. Fundamentals of Aerospace Medicine. Philadelphia: Lea & Febiger, 1985.
44 Ernsting J, King PF, editors. Aviation Medicine. Oxford: Butterworth-Heinemann, 1988.
45 Thomas G, Brimacombe J. Function of the Drager Oxylog ventilator at high altitude. Anaesth Intens Care. 1994;22:276-280.
46 Edmonds C, Lowry C, Pennefather J, editors. Diving and Subaquatic Medicine, 3rd edn.. Butterworth-Heinemann, Oxford, UK, 1992;186-187. 434–6
47 Dunn JD. Legal aspects of transfers. Problems Crit Care. 1990;4:447-448.
48 Fiege A, Rutherford WF, Nelson DR. Factors influencing patient thermoregulation in flight. Air Med J. 1996;15:18-23.
49 Robinson KJ, Kamin R. Quality improvement for transport programs. In: Principles and Direction of Air Medical Transport. Salt Lake City, UT: Air Medical Physician Association; 2003:148-156.
50 American Academy of Pediatrics Task Force on Interhospital Transport. Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients. Elk Grove, IL: American Academy of Pediatrics, 1993.
51 James AG. Neonatal resuscitation, stabilisation and emergency neonatal transportation. Intens Care World, 11. 1995, 53-57.
52 Low RB, Martin D, Brown C. Emergency air transport of pregnant patients: the national experience. Am J Emerg Med. 1988;6:41-48.
53 Gilligan JE, Gorman DF, Millar I. Use of an airborne recompression chamber and transfer under pressure to a major hyperbaric facility. In: Shields TG, editor. Proceedings of the XIV Meeting of the European Undersea Biomedical Society. Aberdeen, UK: European Undersea Biomedical Society, 1988. abstract (paper no. 5)
54 Munford BJ, Roby HP, Xavier X. Considerations in international air medical transport. In: Principles and Direction of Air Medical Transport. Salt Lake City, UT: Air Medical Physician Association; 2003:59-75.
55 Essebag V, Lutchmedial S, Churchill-Smith M. Safety of long distance aeromedical transport of the cardiac patient: a retrospective study. Aviat Space Environ Med. 2001;72:182-187.
56 Garner A, Rashford S, Lee A, et al. Addition of physicians to paramedic helicopter services decreases blunt trauma mortality. Aust NZ J Surg. 1999;69:697-700.
57 Hanrahan BJ, Munford BJ. Air medical scene re-sponse to the entrapped trauma patient. In: AIRMED 96. ADAC/International Society of Aeromedical Services Congress Report. Munich: Wolfsfellner Medizin Verlag; 1997:375-380.
58 Baxt WG, Moody P. The impact of a physician as part of the aeromedical prehospital team in patients with blunt trauma. JAMA. 1987;257:3246-3250.
59 Schmidt U, Scott BF, Nerlich ML, et al. On-scene helicopter transport of patients with multiple injuries – comparison of a German and American system. J Trauma. 1992;33:548-555.
60 Nocera A, Dalton AM. Disaster alert! The role of physician staffed helicopter emergency medical services. Med J Aust. 1994;161:689-692.
61 Garner A, Nocera A. Should New South Wales hospital disaster teams be sent to major incident sites? Aust NZ J Surg. 1999;69:702-707.