Chapter 43 Status epilepticus
Status epilepticus (SE) is a medical emergency requiring prompt intervention to prevent the development of irreversible brain damage.
The duration of seizure activity required to define SE has not been universally agreed upon. Most authors have defined SE as more than 30 minutes’ duration of either a single seizure, or intermittent seizures with no regaining of consciousness between seizures.1–4 This definition is most useful for epidemiological research and is based on experimental studies that show that irreversible neuronal damage occurs after 30 minutes of seizure activity.5,6
More recently an operational definition of SE as 5 minutes of continuous seizure activity, or two or more discrete seizures with no intervening recovery of consciousness, has been used.7 This definition promotes earlier diagnosis and treatment of SE. It has arisen from the generally accepted need to initiate treatment for SE rapidly and the observation that seizures persisting beyond this duration are unlikely to remit spontaneously.8
Refractory SE is defined as failure of initial therapy, such as benzodiazepines and phenytoin, with seizures persisting beyond 1–2 hours and usually requiring agents that induce general anaesthesia to control them.9,10 Refractory SE is associated with a worse prognosis.9,11
SE is commonly separated into two categories:
The incidence of SE is U-shaped, being greatest under 1 year and over 60 years of age.2
PATHOPHYSIOLOGY
Ongoing or recurrent seizures result from failure of normal seizure-terminating mechanisms or excessive excitation causing seizure activity to persist. The major inhibitory mechanism in the brain is γ-aminobutyric acid A (GABAA) receptor-mediated inhibition. Glutamatergic excitatory synaptic transmission is important in sustaining SE.12
AETIOLOGY
SE may occur de novo (approximately 60% of presentations) or, less commonly, in a previously diagnosed epileptic.2 The aetiologies of SE, in decreasing order of frequency as they occur in adults, are given in Table 43.1.2
| Low antiepileptic drug levels (poor compliance, recent dose reduction or discontinuation) |
| Temporally remote causes (previous central nervous system injury e.g. stroke, trauma, tumour, meningitis) |
| Stroke – vascular occlusion or haemorrhage |
| Cerebral hypoxia/anoxia |
| Metabolic disturbances (electrolyte abnormalities, uraemia, hyperglycaemia, hypoglycaemia) |
| Alcohol – withdrawal or intoxication |
| Central nervous system tumours – primary or secondary |
| Systemic infection |
| Idiopathic |
| Central nervous system infection – meningitis, encephalitis |
| Head trauma |
| Drug toxicity (tricyclic antidepressants, phenothiazines, theophylline, isoniazid, cocaine, amphetamine) |
GENERALISED CONVULSIVE STATUS EPILEPTICUS
GCSE is the most common and dangerous type of SE and accounts for approximately 75% of cases.2 It encompasses a broad spectrum of clinical presentations, from overt generalised tonic-clonic seizures to subtle convulsive movements in a profoundly comatose patient.13
CLINICAL
Typically, early in the evolution of seizures, patients are unresponsive with obvious tonic (sustained contractions) and/or clonic (rhythmic jerking) movements (overt GCSE). Motor manifestations may be symmetrical or asymmetrical.
With time, the clinical manifestations may become subtle, and patients have only small-amplitude twitching movements of the face, hands or feet or nystagmoid jerking of the eyes (late or subtle GCSE).13
Later still some patients will have no observable repetitive motor activity and the detection of ongoing seizures requires EEG (electrical GCSE). Most authors classify this as a form of NCSE.14–16 Such patients are still at risk of central nervous system (CNS) injury and require prompt treatment.
EEG CHANGES
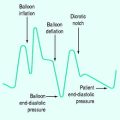
Just as there is a progression from overt to increasingly subtle motor manifestations, there is also a predictable sequence of EEG changes during untreated GCSE. Initially, discrete electrographic seizures merge to a waxing and waning pattern of seizure activity, followed by continuous monomorphic discharges, which become interspersed with increasing periods of electrographic silence and, eventually, periodic epileptiform discharges on a relatively flat background.13,17 The presence of any of these EEG patterns should suggest the diagnosis of GSCE.
ENDOCRINE AND METABOLIC EFFECTS
Early in GCSE there is a marked increase in plasma catecholamines, producing systemic physiologic changes that resolve if SE is stopped early (Table 43.2). However, if seizures continue, many of these early physiologic changes reverse and the resultant hypotension and hypoglycaemia may exacerbate neurological injury.18
Table 43.2 Physiological changes in generalised convulsive status epilepticus18,56
| Hypoxia |
| Respiratory acidosis |
| Lactic acidosis |
| Hyperpyrexia |
| Hypertension (early)/hypotension (late) |
| Hyperglycaemia (early)/hypoglycaemia (late) |
| Tachycardia |
| Cardiac arrhythmias |
| Blood leukocytosis |
| Cerebrospinal fluid pleocytosis, increased cerebrospinal fluid protein |
| Intracranial hypertension |
| Neurogenic pulmonary oedema |
| Aspiration pneumonitis |
| Rhabdomyolysis |
PSEUDOSEIZURES
An important differential diagnosis of generalised convulsive epilepsy is pseudoseizures. These can occur in patients with or without a history of epilepsy.19 Clinical features suggestive of pseudoseizures are listed in Table 43.3. Distinction between the two may be extremely difficult, and can only be made with complete certainty using EEG monitoring.19 Pseudo-status, misdiagnosed as true SE, is often refractory to initial therapy and can lead to patients receiving general anaesthesia and mechanical ventilation.
| Lack of stereotyped seizures, with behavioural manifestations varying from event to event |
| Lack of sustained convulsive activity – ‘on–off’ appearance |
| Increase in movement if restraint is applied |
| Abolition of motor movements with reassurance or suggestion |
| Resistance to eye opening and gaze aversion |
| Poor response to treatment, refractory status epilepticus |
| Absence of pupillary dilatation |
| Normal tendon reflexes and plantar responses immediately after convulsion |
| Lack of metabolic consequences despite some hours of apparent fitting |
NON-CONVULSIVE STATUS EPILEPTICUS
This may account for approximately 25% of SE, though its incidence is probably underestimated because of failure to recognise and diagnose the condition.
The diagnosis of NCSE should be considered in any patient with an unexplained altered conscious state, particularly those with CNS injury, metabolic disturbance, hepatic encephalopathy and sepsis. Series where EEG has been performed in critically ill patients with an unexplained depressed conscious state have found a high incidence of NCSE (8–18%).20–22 EEG monitoring is required in patients with GCSE who do not recover consciousness after resolution of overt convulsive activity; in one study more than 14% of such patients had NCSE.14
Considerable debate exists regarding the precise criteria for diagnosing NCSE and published reports often describe diverse cohorts of patients. The diagnosis of NCSE generally requires a change in behaviour and/or mentation from baseline for at least 30 minutes, no overt seizure activity and an EEG with epileptiform discharges. A response to intravenous antiepileptic drugs (e.g. benzodiazepines), with clinical improvement and resolution or improvement in EEG epileptic activity, is helpful in confirming the diagnosis.23
Various classifications for NCSE have been suggested.4,23–25 Traditionally NCSE is divided into absence SE (ASE) and complex partial SE (CPSE), though it may not always be possible to differentiate between the two types.23,24
ASE is characterised by bilateral diffuse synchronous seizures.23 Typical ASE has generalised 3-Hz spike-wave discharge EEG activity occurring with altered behaviour or loss of responsiveness and is seen in children with idiopathic generalised epilepsy who are otherwise normal. This form of SE is relatively benign. Atypical ASE is a heterogeneous syndrome occurring in patients with mental retardation and epilepsy with multiple seizure types, or with other forms of diffuse cerebral dysfunction. The prognosis is usually poor and is related to the underlying condition.
CPSE, also referred to as ‘epileptic twilight state’ and ‘temporal-lobe SE’, is accompanied by lateralised seizure activity on EEG.23 A wide variety of clinical features and degree of impairment of consciousness is possible and includes confusion, agitation, bizarre or aggressive behaviour and coma. Behavioural accompaniments such as lip smacking, automatisms and gaze deviation may occur, depending on the seizure origin within the brain. Debate exists over whether the seizure activity causes brain injury and much of the morbidity appears attributable to the underlying illness.
EPILEPTIFORM ENCEPHALOPATHIES
Some variants of SE deserve mention, such as comatose patients with epileptiform patterns on EEG who do not fit into the traditional classification of NCSE. Some of these cases may be late GCSE but many occur without prior clinical convulsions. In such situations it is unclear whether the abnormal discharges seen on the EEG are responsible for, or contribute to, the altered consciousness and abnormal movements, or are merely a reflection of a severe cerebral insult.24
Myoclonic SE that follows a hypoxic insult falls into this category. Patients have incessant, at times asynchronous, rhythmic jerks that may involve the entire body. This clinical appearance after an anoxic insult is associated with an extremely poor outcome.26
INVESTIGATIONS
Not all of the investigations listed in Table 43.4 need to be performed in every patient. The selection of tests depends on both the patient’s history and presentation.
| Initial studies |
| Blood glucose, electrolytes (sodium, potassium, calcium, magnesium), urea |
| Oximetry Spo2 or arterial blood gases |
| Anticonvulsant drug levels |
| Full blood count |
| Urinalysis |
| Further investigations after stabilisation |
| Liver function tests, lactate, creatine kinase |
| Toxicology screen |
| Lumbar puncture |
| Electroencephalogram |
| Brain imaging with computed tomography or magnetic resonance imaging |
NEUROIMAGING
Most patients with SE should have a computed tomography (CT) scan of the brain performed at some point. Many patients with established epilepsy who have already been thoroughly evaluated do not require another brain-imaging procedure after an episode of SE.1 However, if there is reason to suspect a new problem, and when the need for imaging is not urgent, magnetic resonanceimaging (MRI) may be preferable because it occasionally reveals abnormalities not visualised on CT scans. In children, emergent imaging is required if there is a persisting neurological deficit or abnormal mental state, and electively for focal seizures. Imaging should only be performed after control of SE and patient stabilisation.27
LUMBAR PUNCTURE
In any patient, especially in young children with fever and SE, CNS infection and lumbar puncture along with blood cultures should be considered. Meningitis is an uncommon cause of SE in adults and, unless the suspicion of CNS infection is high, brain imaging should be performed before a lumbar puncture. Contraindications to lumbar puncture include intracranial hypertension, mass lesion and hydrocephalus. If meningitis is suspected but a lumbar puncture cannot be performed expediently, antibiotics should be administered immediately rather than delayed. Approximately 20% of patients have a modest CSF white cell count pleocytosis after SE and such patients should be treated for suspected meningitis until the diagnosis is excluded by culture or other means.1
MANAGEMENT
GENERALISED CONVULSIVE STATUS EPILEPTICUS
An accurate history should be obtained, with particular emphasis on eye-witness accounts of the onset and nature of the seizures, and a full physical examination performed. However, neither should delay initial emergency management. There is evidence that the longer SE goes untreated, the harder it is to control with drugs.28,29
Few controlled data are available to support the use of any particular agents. The most useful evidence comes from a randomised, double-blind clinical trial for treatment of GCSE which found that lorazepam, phenobarbital or diazepam followed by phenytoin are all acceptable as initial treatment, but that phenytoin alone was not as effective as lorazepam.29 Another randomised controlled trial in the pre-hospital setting found intravenous lorazepam and diazepam to be equally effective and superior to placebo in terminating GCSE.7
The EEG goal of treatment for refractory SE remains controversial, with some advocating EEG background suppression (isoelectric) and others suppression of seizures regardless of the EEG background activity.10,16,30
Various protocols for SE management have been suggested.1,16,30 One approach is outlined in Box 43.1.
Box 43.1 Protocol for management of status epilepticus
* If IV access is not obtainable, consider rectal diazepam, buccal/sublingual or intranasal or intramuscular midazolam, intramuscular fosphenytoin.
† High infusion rates for prolonged periods require caution.
‡ In refractory status epilepticus, consider giving pyridoxine for children < 18 months or if isoniazid toxicity is suspected in adults.GCS, Glasgow Coma Score; ECG, electrocardiogram; IV, intravenous; EEG, electroencephalogram; BP, blood pressure.
NON-CONVULSIVE STATUS EPILEPTICUS
Patients with NCSE are a heterogeneous group who are likely to vary in their response to treatment depending on the underlying aetiology.23
There is considerable debate as to whether NCSE presents the same degree of risk of neurological injury as GCSE.25 Prompt treatment is generally recommended and the use of additional non-anaesthetising anticonvulsants, such as phenobarbital and valproate, prior to embarking on general anaesthesia has been suggested.16,23 Others recommend that, for comatose patients with NCSE, a similar treatment approach to GCSE be taken.30
The potential side-effects of aggressive treatment (hypotension, immunosuppression) need to be balanced against the potential neurologic morbidity of NCSE.24,31 Particularly in elderly patients, aggressive treatment and anaesthesia may be associated with more risk than benefit and result in a worse outcome.31,32
Prognosis is most closely related to the underlying aetiology.33
DRUGS FOR STATUS EPILEPTICUS
BENZODIAZEPINES
Benzodiazepines are fast-acting antiseizure drugs and are therefore preferred as initial therapy. They act mainly by enhancing the neuroinhibitory effects of GABAA. The efficacy of benzodiazepines may diminish with prolonged use in SE due to reduced receptor affinity for benzodiazepines.12
Lorazepam is less lipid-soluble than diazepam and after intravenous injection, brain and CSF levels rise at a slower rate than those of diazepam. However, a double-blind, randomised comparison of intravenous diazepam and lorazepam in SE in the pre-hospital setting found both drugs to be equally safe and effective.7 Despite their equivalence as initial therapies, lorazepam has a longer duration of antiseizure effect than diazepam, and has a lower incidence of seizure recurrence when used alone.1
Midazolam has a short duration of action that may allow earlier assessment of the patient’s postictal neurologic condition than longer-acting benzodiazepines. Midazolam has the advantage of being able to be administered via buccal, intranasal and intramuscular routes. Intranasal midazolam is as effective as intravenous diazepam in children34 and buccal midazolam is as effective as rectal diazepam in prolonged seizures.35 Whereas intramuscular administration of diazepam and lorazepam is not recommended owing to their slow absorption, intramuscular midazolam is rapidly absorbed and in one study it was equally efficacious as intravenous diazepam in treating motor seizures in children.36 These alternative routes of administration may be more convenient and acceptable than intravenous and rectal administration, particularly in the pre-hospital setting and when intravenous access is difficult.
Midazolam administered by bolus and infusion may terminate seizures when other agents have failed. It may also have fewer side-effects than alternative agents available for the treatment of refractory SE.37 A limiting factor in its use is tachyphylaxis, which may necessitate a several-fold increase in the dose to maintain seizure control.30 There is a wide variation in recommended infusion rates, from 0.1–0.4 mg/kg per hour16 to 0.2–2.9 mg/kg per hour.10
PHENYTOIN
Phenytoin is useful for maintaining a prolonged antiseizure effect after rapid termination of seizures with a benzodiazepine, or when benzodiazepines fail. When used alone as initial therapy phenytoin is not as efficacious as benzodiazepines for terminating seizures.29
Fosphenytoin, a new water-soluble prodrug of phenytoin, is converted to phenytoin by endogenous phosphatases.38 Doses of fosphenytoin are expressed as phenytoin equivalents (PE). Fosphenytoin can be administered at rates of up to 150 PE mg/min, since it is not formulated with propylene glycol, allowing therapeutic serum concentrations of fosphenytoin to be attained within 10 minutes. However, this may not necessarily result in more rapid CNS penetration and onset of action.39
Systemic side-effects are similar for phenytoin and fosphenytoin, although reactions at the infusion site are less common with fosphenytoin.38
SODIUM VALPROATE
There are reports of intravenous valproate being used to treat both GCSE and NCSE in adults and children. It is non-sedating and it appears to be well tolerated with few reports of hypotension or respiratory depression.40 An initial dose of 25–45 mg/kg administered at a maximum rate of up to 6 mg/kg per min has been recommended.16 The exact role of valproate in the management of SE remains to be established and there are insufficient data to recommend its use before phenytoin.
BARBITURATES
Phenobarbital is a potent anticonvulsant with a long duration of action. The usual dose is 15–20 mg/kg intravenously. It has equal efficacy to benzodiazepines and phenytoin when used first-line, but may cause greater depression of respiration, blood pressure and consciousness and therefore is often only used if these agents fail. However, many would advocate alternative and more aggressive measures for treatment of refractory SE at this point as the likelihood of phenobarbital controlling seizures when these other agents have failed is small.10,15
Compared with other agents used in refractory SE (midazolam and propofol), barbiturates may result in a lower frequency of short-term treatment failure and breakthrough seizures but more hypotension and slower recovery from anaesthesia.41
PROPOFOL
Compared with high-dose barbiturates (pentobarbital) in adult patients with refractory SE, propofol has been found to control seizures more quickly and, because of its shorter duration of action, allows earlier re-emergence from anaesthesia.42 However, seizures tend to recur with sudden discontinuation of propofol, necessitating recommencement of the infusion and a more gradual tapering of the dose, such that both drugs may ultimately result in similar duration of ventilation and ICU stay.42
There is concern that prolonged high-dose propofol use (e.g. > 5 mg/kg per hour) may result in myocardial failure, hypoxia, metabolic acidosis, lipaemia, rhabdomyolysis and death (propofol infusion syndrome).43 Initial reports were in children but later also adults and, as such, its use requires caution. There are series, however, of prolonged high-dose propofol use in adults with SE without major adverse effects.44
OTHER AGENTS OF POTENTIAL USE IN REFRACTORY STATUS EPILEPTICUS
Ketamine may be a useful adjuvant in the treatment of refractory SE.45 The newer antiepileptic drugs such as topiramate may also have a role in refractory SE treatment.46 Inhalational anaesthetic agents such as isoflurane may also be useful.47
INTENSIVE CARE MONITORING
Monitoring using ECG, intra-arterial and central venous catheters, capnography and pulse oximetry should be considered in patients with, or at risk of, cardiorespiratory compromise. Indications for EEG monitoring are listed in Table 43.5. Cerebral function monitors are useful in titrating doses of anaesthetic agents to EEG background suppression, but may not have sufficient sensitivity to detect seizure activity at other times. Intracranial pressure monitoring should be considered if elevated intracranial pressure is suspected.
Table 43.5 Indications for electroencephalogram (EEG) monitoring14
| Refractory status epilepticus, to aid the titration of anticonvulsant anaesthetic drugs (minimising dose and toxicity) and ensure suppression of seizure activity* |
| Patients receiving neuromuscular blockade* |
| Patients who continue to have a poor conscious state after apparent cessation of seizures |
| Suspected non-convulsive status epilepticus in a patient with an altered conscious state |
| Suspected pseudoseizures |
* Continuous or regular intermittent EEG monitoring is recommended.
OUTCOME
The prognosis of patients with SE is most strongly related to age and aetiology.3,33 Overall 30-day mortality is 15–20%.3,4 Children have a much lower mortality of 3%51 whereas those aged over 65 years have a mortality rate of 30%.3,4 SE that is precipitated by low antiepileptic drug levels or systemic infection has a very low mortality.3 Patients who develop SE secondary to an acute CNS or systemic metabolic insult have a higher mortality than those who develop SE without a clear precipitant.3 SE precipitated by hypoxia is usually fatal.26 NCSE detected in comatose critically ill patients, despite recognition and treatment, has a poor outcome.22,32 Refractory SE carries a worse prognosis that is mainly determined by the underlying cause.9,11
The duration of SE and time to provision of adequate treatment are also important factors that may influence the ease with which seizures can be controlled, the risk of residual neurological deficits and mortality.9,28,29 The degree of impairment of consciousness at presentation may also be an important factor influencing outcome.4
The EEG may provide useful prognostic information, with periodic epileptiform discharges present at any time during or after SE being associated with a worse outcome.52
Neurone-specific enolase (NSE) is a well-studied marker of brain injury and high serum levels have been found in GCSE and NCSE, particularly CPSE.53 Elevated levels may reflect either the severity of brain injury resulting from SE, the underlying brain pathology, or both. Increases in serum NSE have been correlated with the duration and prognosis of GCSE.53
STATUS EPILEPTICUS IN CHILDREN
The majority of paediatric cases of SE occur in young children, with 80% occurring in those below 4 years of age.51 The vast majority of cases are convulsive and generalised.27
The distribution of causes is highly age dependent, with febrile SE and that due to acute neurological disease (e.g. CNS infection) being more common in children under 4 years. Remote symptomatic causes and SE in a child with previously diagnosed epilepsy are more common in older children.51 The most frequent aetiologies of SE in children are listed in Table 43.6.27,51
| Febrile (previously neurologically normal, temperature > 38°C, central nervous system infection excluded) |
| Acute symptomatic – meningitis, encephalitis, trauma, metabolic derangement, hypoxia, drug-related, cerebrovascular disease |
| Remote symptomatic causes – previous traumatic brain injury or cerebral insult, central nervous system malformation, cerebral palsy |
| Progressive neurologic conditions |
| Cryptogenic |
The likelihood of bacterial meningitis is much higher (12%) in febrile children presenting with a first-ever episode of SE as opposed to a brief seizure (1%) and a high index of suspicion is required to investigate and treat for meningitis.51
Treatment of SE in children is essentially the same as in adults.54
The underlying cause is the main determinant of mortality, which is negligible for prolonged febrile seizures and 12–16% for acute symptomatic causes.55 Similarly, the risk of subsequent epilepsy is low in neurologically normal children but higher than 50% in those with acute or remote symptomatic causes.55
1 Treatment of convulsive status epilepticus. Recommendations of the Epilepsy Foundation of America’s Working Group on Status Epilepticus. JAMA. 1993;270:854-859.
2 DeLorenzo RJ, Hauser WA, Towne AR, et al. A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology. 1996;46:1029-1035.
3 Logroscino G, Hesdorffer DC, Cascino G, et al. Short-term mortality after a first episode of status epilepticus. Epilepsia. 1997;38:1344-1349.
4 Rossetti AO, Hurwitz S, Logroscino G, et al. Prognosis of status epilepticus: role of aetiology, age, and consciousness impairment at presentation. J Neurol Neurosurg Psychiatry. 2006;77:611-615.
5 Meldrum BS, Brierley JB. Prolonged epileptic seizures in primates. Ischemic cell change and its relation to ictal physiological events. Arch Neurol. 1973;28:10-17.
6 ILAE Commission Report. The epidemiology of the epilepsies: future directions. International League Against Epilepsy. Epilepsia. 1997;38:614-618.
7 Alldredge BK, Gelb AM, Isaacs SM, et al. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631-637.
8 Shinnar S, Berg AT, Moshe SL, et al. How long do new-onset seizures in children last? Ann Neurol. 2001;49:659-664.
9 Mayer SA, Claassen J, Lokin J, et al. Refractory status epilepticus: frequency, risk factors, and impact on outcome. Arch Neurol. 2002;59:205-210.
10 Bleck TP. Refractory status epilepticus. Curr Opin Crit Care. 2005;11:117-120.
11 Rossetti AO, Logroscino G, Bromfield EB. Refractory status epilepticus: effect of treatment aggressiveness on prognosis. Arch Neurol. 2005;62:1698-1702.
12 Macdonald RL, Kapur J. Acute cellular alterations in the hippocampus after status epilepticus. Epilepsia. 1999;40:S9-20. discussion S21–2
13 Treiman DM. Electroclinical features of status epilepticus. J Clin Neurophysiol. 1995;12:343-362.
14 DeLorenzo RJ, Waterhouse EJ, Towne AR, et al. Persistent nonconvulsive status epilepticus after the control of convulsive status epilepticus. Epilepsia. 1998;39:833-840.
15 Dhar R, Mirsattari SM. Current approach to the diagnosis and treatment of refractory status epilepticus. Adv Neurol. 2006;97:245-254.
16 Meierkord H, Boon P, Engelsen B, et al. EFNS guideline on the management of status epilepticus. Eur J Neurol. 2006;13:445-450.
17 Kaplan PW. The EEG of status epilepticus. J Clin Neurophysiol. 2006;23:221-229.
18 Walton NY. Systemic effects of generalized convulsive status epilepticus. Epilepsia. 1993;34:S54-58.
19 Betts T. Pseudoseizures: seizures that are not epilepsy. Lancet. 1990;336:163-164.
20 Towne AR, Waterhouse EJ, Boggs JG, et al. Prevalence of nonconvulsive status epilepticus in comatose patients. Neurology. 2000;54:340-345.
21 Claassen J, Mayer SA, Kowalski RG, et al. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology. 2004;62:1743-1748.
22 Pandian JD, Cascino GD, So EL, et al. Digital video-electroencephalographic monitoring in the neurological–neurosurgical intensive care unit: clinical features and outcome. Arch Neurol. 2004;61:1090-1094.
23 Kaplan PW. The clinical features, diagnosis, and prognosis of nonconvulsive status epilepticus. Neurologist. 2005;11:348-361.
24 Krumholz A. Epidemiology and evidence for morbidity of nonconvulsive status epilepticus. J Clin Neurophysiol. 1999;16:314-322. discussion 353
25 Kaplan PW. No, some types of nonconvulsive status epilepticus cause little permanent neurologic sequelae (or: “the cure may be worse than the disease”). Neurophysiol Clin. 2000;30:377-382.
26 Wijdicks EF, Hijdra A, Young GB, et al. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67:203-210.
27 Riviello JJJr., Ashwal S, Hirtz D, et al. Practice parameter: diagnostic assessment of the child with status epilepticus (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2006;67:1542-1550.
28 Lowenstein DH, Alldredge BK. Status epilepticus at an urban public hospital in the 1980s. Neurology. 1993;43:483-488.
29 Treiman DM, Meyers PD, Walton NY, et al. A comparison of four treatments for generalized convulsive status epilepticus Veterans. Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339:792-798.
30 Marik PE, Varon J. The management of status epilepticus. Chest. 2004;126:582-591.
31 Walker MC. Status epilepticus on the intensive care unit. J Neurol. 2003;250:401-406.
32 Litt B, Wityk RJ, Hertz SH, et al. Nonconvulsive status epilepticus in the critically ill elderly. Epilepsia. 1998;39:1194-1202.
33 Shneker BF, Fountain NB. Assessment of acute morbidity and mortality in nonconvulsive status epilepticus. Neurology. 2003;61:1066-1073.
34 Mahmoudian T, Zadeh MM. Comparison of intranasal midazolam with intravenous diazepam for treating acute seizures in children. Epilepsy Behav. 2004;5:253-255.
35 Scott RC, Besag FM, Neville BG. Buccal midazolam and rectal diazepam for treatment of prolonged seizures in childhood and adolescence: a randomised trial. Lancet. 1999;353:623-626.
36 Chamberlain JM, Altieri MA, Futterman C, et al. A prospective, randomized study comparing intramuscular midazolam with intravenous diazepam for the treatment of seizures in children. Pediatr Emerg Care. 1997;13:92-94.
37 Prasad A, Worrall BB, Bertram EH, et al. Propofol and midazolam in the treatment of refractory status epilepticus. Epilepsia. 2001;42:380-386.
38 Browne TR. Fosphenytoin (Cerebyx). Clin Neuropharmacol. 1997;20:1-12.
39 Walton NY, Uthman BM, El Yafi K, et al. Phenytoin penetration into brain after administration of phenytoin or fosphenytoin. Epilepsia. 1999;40:153-156.
40 Limdi NA, Shimpi AV, Faught E, et al. Efficacy of rapid IV administration of valproic acid for status epilepticus. Neurology. 2005;64:353-355.
41 Claassen J, Hirsch LJ, Emerson RG, et al. Treatment of refractory status epilepticus with pentobarbital, propofol, or midazolam: a systematic review. Epilepsia. 2002;43:146-153.
42 Stecker MM, Kramer TH, Raps EC, et al. Treatment of refractory status epilepticus with propofol: clinical and pharmacokinetic findings. Epilepsia. 1998;39:18-26.
43 Vasile B, Rasulo F, Candiani A, et al. The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intens Care Med. 2003;29:1417-1425.
44 Rossetti AO, Reichhart MD, Schaller MD, et al. Propofol treatment of refractory status epilepticus: a study of 31 episodes. Epilepsia. 2004;45:757-763.
45 Nathan BN, Smith TL, Bleck TP. The use of ketamine in refractory status epilepticus. Neurology. 2002;58:A197.
46 Towne AR, Garnett LK, Waterhouse EJ, et al. The use of topiramate in refractory status epilepticus. Neurology. 2003;60:332-334.
47 Mirsattari SM, Sharpe MD, Young GB. Treatment of refractory status epilepticus with inhalational anesthetic agents isoflurane and desflurane. Arch Neurol. 2004;61:1254-1259.
48 Ma X, Liporace J, O’Connor MJ, et al. Neurosurgical treatment of medically intractable status epilepticus. Epilepsy Res. 2001;46:33-38.
49 Duane DC, Ng YT, Rekate HL, et al. Treatment of refractory status epilepticus with hemispherectomy. Epilepsia. 2004;45:1001-1004.
50 Winston KR, Levisohn P, Miller BR, et al. Vagal nerve stimulation for status epilepticus. Pediatr Neurosurg. 2001;34:190-192.
51 Chin RF, Neville BG, Peckham C, et al. Incidence, cause, and short-term outcome of convulsive status epilepticus in childhood: prospective population-based study. Lancet. 2006;368:222-229.
52 Nei M, Lee JM, Shanker VL, et al. The EEG and prognosis in status epilepticus. Epilepsia. 1999;40:157-163.
53 DeGiorgio CM, Heck CN, Rabinowicz AL, et al. Serum neuron-specific enolase in the major subtypes of status epilepticus. Neurology. 1999;52:746-749.
54 Prasad AN, Seshia SS. Status epilepticus in pediatric practice: neonate to adolescent. Adv Neurol. 2006;97:229-243.
55 Raspall-Chaure M, Chin RF, Neville BG, et al. Outcome of paediatric convulsive status epilepticus: a systematic review. Lancet Neurol. 2006;5:769-779.
56 Simon RP. Physiologic consequences of status epilepticus. Epilepsia. 1985;26:S58-66.