Chapter 104 Equipment for paediatric intensive care
This chapter discusses equipment and its performance required in paediatric and neonatal intensive care. How to use equipment is not discussed. Examples of equipment are given, but exhaustive lists are not intended. Only essential equipment is considered.
AIRWAY MANAGEMENT
ENDOTRACHEAL TUBES
TUBE SIZE
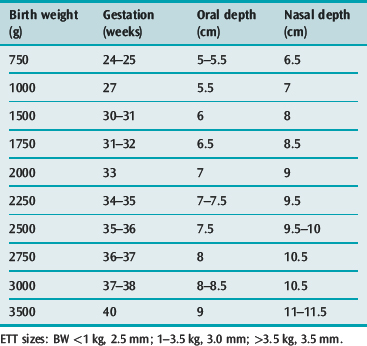
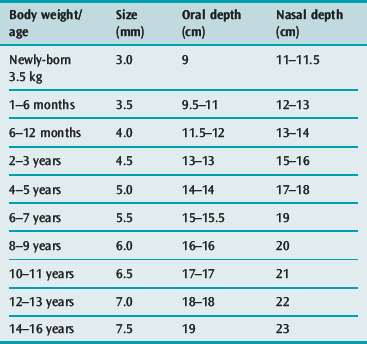
A selection of sizes, one larger and one smaller than the anticipated size, should be available at intubation. Tube sizes according to body weight and age are given in Table 104.1 and 104.2. A rough guide for internal diameter size in the child is age (in years)/4 + 4 mm.
TUBE LENGTH (DEPTH)
The endotracheal tube tip should be located in the mid-trachea so that the risks of accidental extubation and endobronchial intubation are minimised. Correct positioning of the tube should always be checked by auscultation in the axillae, by chest X-ray immediately after intubation and daily thereafter.1 At intubation, visualisation of the depth of the tube passed through the cords should be a guide only, since the tube advances when the head is released from extension as the laryngoscope is removed.2
The lengths (depths) at which orotracheal and nasotracheal tubes can be chosen initially on the basis of weight or gestation in premature neonates are given in Table 104.1, and on the basis of age for infants and children in Table 104.2. The lengths are at the lips for oral tubes and at the exit from the nose for nasal tubes. For oral tubes, a guide to correct depth for 2 years and over is given by the formula: (age in years/2 + 12 cm), while for nasal tubes the formula is: (age in years/2 + 15 cm). The depth of insertion of any tube should be documented or marked on the tube.
SUCTION CATHETERS
Sizes 5, 6, 8, 10 and 12 FG should be available. The suction catheter should be large enough to remove secretions but not too large to occlude the endotracheal/tracheostomy tube lumen (Table 104.3). Many suitable types are available – differing in number and location of suction ports (end and side ports are needed) and whether the tip is angled or straight. Angled tips facilitate entry into the left main bronchus. Satin-finish types with smooth port edges are needed. Single use suction catheters may be reused up to 24 hours without adding to the risk of pneumonia.3 Closed suction systems permit suction without disconnection from ventilator as may be indicated during nitric oxide therapy, severe lung disease or frequent suction.
| Internal diameter (mm) of ETT or tracheostomy | Recommended suction catheter (FG) |
|---|---|
| 2.5 | 5 |
| 3.0 | 6 |
| 3.5–5.5 | 8 |
| 6.0–6.5 | 10 |
| 7.0 and larger | 12 |
ETT, endotracheal tube.
OROPHARYNGEAL AIRWAYS
A range of Guedel airways (sizes 000, 00, 0, 1, 2 and 3) constructed of polyvinyl chloride with a metal insert should be available: an airway that is too small may be occluded by the surface of the tongue or displace the tongue backwards to obstruct the airway; an airway that is too large may enter the oesophagus. The correct size, when placed alongside the cheek, extends from the centre of the lips to the angle of the mandible. Nasopharyngeal airways are available for the older child, but any size can be constructed from an endotracheal tube. A guide to length is from the tip of the nose to the tragus of the ear.
MECHANICAL VENTILATION
RESUSCITATOR ‘BAGGING’ CIRCUITS
SELF-INFLATED BAGS
With Laerdal and Partner bags, negligible amounts of oxygen (0.1–0.3 l/min) issue from the patient valve when 5–15 l/min of oxygen is introduced into bags unconnected to patients.4 The valve is unlikely to open unless the mask is sealed well on the face. The delivered oxygen concentration is dependent on the flow rate of oxygen, use of the reservoir bag, and the state of the pressure relief valve (whether open or closed).
Other self-inflated bags include the Combibag, Ambu, AirViva and Hudson RCI.
MASKS
Masks should facilitate an airtight seal on the face with minimal dead space.
Masks with rims created by infolding of the body are more difficult to use.
MECHANICAL VENTILATORS
CONVENTIONAL VENTILATORS
A generic classification of ventilators, their operational characteristics and their modes of ventilation has been proposed.5 It is described here briefly to enable functional description and comparison of some ventilators.
PHASE VARIABLES
Volume/flow-control modes are suitable for conditions in which lung compliance and resistance are variable. In these circumstances, the peak inspiratory pressure attained is a valuable observation. However, when a pressure limit is imposed, such information is lost. A mode consisting of flow control, time triggering, pressure limitation and time cycling is commonly used because of the relative ease of operation. However, relatively small leaks may severely compromise tidal volume, mean airway pressure and oxygenation. Large leaks may also delay attainment of preset pressure until late in the inspiratory cycle. Thus, it is helpful to display the volume and pressure waveforms. Some ventilators do, however, provide leak compensation (e.g. Bird VIP Gold). Gas flow should be set above 2 l/kg per min to achieve the preset pressure early in the inspiratory period. This flow rate is also suitable for peak inspiratory flow rate during spontaneous respiratory effort with intermittent mandatory ventilation.
Pressure in the circuit should be monitored in close proximity to the endotracheal tube. Changes in endotracheal tube resistance from encrustation or kinking have a major adverse effect on tidal volume.6
Neonates and infants have small tidal volumes (5–50 ml), and are therefore prone to alveolar hypoventilation when variable air leaks occur around the endotracheal tube and from the ventilator–humidifier circuit. Moreover, the internal compliance and compressible volume of the circuit may exceed the tidal volume. Small tidal volumes are difficult to set and maintain when the lung compliance and resistance are abnormal.7
Most neonatal intensive care units (ICUs) use pressure-control modes which in hyaline membrane disease achieves adequate oxygenation with minimal barotrauma.8 The pressure-control mode is more appropriate than the volume-control mode for neonates and infants 0.5–5.0 kg body weight. Ventilators, which are pressure controllers, deliver a variable flow dependent on lung and airway characteristics.
Improvements in ventilatory management of newborns are observed with a new generation of ventilators, which utilise changes in airway pressure, airway gas flow or abdominal movement to trigger inspiration, and which have ultrashort trigger delays.9 Previously, ventilators were unable to cope with the very short inspiratory times (mean 0.31, SD 0.06 seconds) of newborns with respiratory distress syndrome.10 Patient-triggered ventilation (PTV) permits synchronous ventilation with better gas exchange, prevents the patient fighting the ventilator and reduces the need for neuromuscular paralysis. 11,12 Some ventilators suitable for paediatric use are the Bear Cub 2001, Bear Cub 750vs, Bird T Bird, Bird VIP Gold, Drager Babylog 8000 (plus), Drager Evita 4, Evita XL, Infant star 950, Sechrist IV-100B, Sechrist IV-200 SAVI, Siemens Servo 900C, Siemens Servo 300, Siemens Servo-i, Viasys Avea, and SLE 5000.
HIGH-FREQUENCY VENTILATORS
These provide ventilation at at least four times normal rate and may be classified into five types:5
High-frequency oscillatory ventilation (HFO) at 15 Hz has been shown to achieve better gas exchange with less barotrauma than conventional mechanical ventilation in infants with respiratory distress.13,14 Examples of high-frequency oscillators are the Sensor Medics and 3100A and 3100B (adult) and the Humming series models, of which the latest is Atom Humming V. The latter also offers a synchronised intermittent mandatory ventilation mode. An example of a high-frequency jet ventilator is the Bunnell Life Pulse jet ventilator which is used in conjunction with a conventional ventilator to provide positive end-expiratory pressure (PEEP) and humidified gas for spontaneous ventilation. An example of a high-frequency positive-pressure ventilator is the Nellcor Puritan-Bennett Infant Star 950, which operates as a flow interrupter.
NON-INVASIVE VENTILATION (NIV)
CPAP is commonly used to relieve upper-airway obstruction or improve oxygenation in lung disease. BiPAP is commonly used to provide ventilation in chronic hypoventilatory states such as congenital central hypoventilation syndrome, neuromuscular diseases, pretransplantation cystic fibrosis and in acute conditions such as asthma, pneumonia and pulmonary oedema. Both CPAP and BiPAP are used before resorting to invasive ventilation and after extubation. Although stand-alone, BiPAP machines are primarily intended for use in adult patients with obstructive sleep apnoea and are not generally intended for use as life support. Consequently, many machines are not licensed to provide ventilation via endotracheal tube or tracheostomy but this capability is a distinct advantage and may be provided as an optional mode in mechanical ventilators.
OXYGEN THERAPY AND MONITORING
OXYGEN CATHETERS
Sizes 6, 8 and 10 FG should be available and placed in the same nostril as the nasogastric tube, to limit airway resistance. Size 6 FG is suitable for neonates, 8 FG for infants and small children and 10 FG for older children. It should be appreciated that oxygen catheters placed in the nasopharynx provide a small amount of PEEP, and indeed may be used for that purpose.15 Nasal cannulae (two-pronged) are not recommended. Excessive flow may cause gastric distension. Flow rate for infants should be regulated by a low-flow meter, graduated 0–2.5 l/min.
OXYGEN MASKS
Masks may not be well tolerated by the infant or small child; oxygen catheters are preferable.
OXYGEN ANALYSERS
These are essential to regulate oxygen therapy via incubator or head box. The devices utilise either a polarographic electrode or galvanic cell (microfuel cell) as oxygen sensor. The polarographic types require a source of power (battery or mains), are more expensive to buy but cheaper to run, and have a faster response time.13,16 An incorporated alarm is recommended. The sensing electrode should be placed close to the patient’s head.
TRANSCUTANEOUS GAS ANALYSERS
Transcutaneous gas tensions in paediatric patients equate well with arterial gas tensions. However, PaO2 is underestimated by PtcO2 during mild hyperoxaemia in neonates.17 Transcutaneous gas values are dependent on both arterial gas tensions and on blood flow. During normovolaemia with adequate flow, PtcO2 reflects PaO2 and PtcCO2 reflects PaCO2. However, during circulatory failure, a reduction in PtcO2 reflects a reduction in flow, provided PaO2 is normal.18 Likewise, during circulatory failure, PtcCO2 exceeds PaCO2 and is flow dependent.19 Typical transcutaneous dual function single electrodes are Hewlett Packard Virida tcpO2/tcCO2, Sensormedics FasTrac SaO2/CO2 monitor.
Continuous pulse oximetry (SpO2) has evolved to be an integral part of monitoring in neonatal and paediatric intensive care. Transcutaneous pulse oximetry is more convenient than transcutaneous partial pressure measurement. Each patient should have a pulse oximeter. The value of pulse oximetry is detection of hypoxaemia, not hyperoxaemia. They cannot be used accurately to titrate oxygen therapy, which requires blood or transcutaneous partial pressure measurement. The accuracy of pulse oximetry at low SaO2 (< 75%) is poor.20 Numerous devices are available.
APNOEA MONITORS
Infant apnoea is often due to upper-airway obstruction, seizures or gastro-oesophageal reflux,21 although it may be idiopathic and is commonly associated with prematurity. Short apnoeic spells (< 15 seconds) are normal during sleep and feeding. Significant apnoea is associated with bradycardia, cyanosis and hypotonia. The detection and treatment of apnoea in intensive care are dependent on cardiovascular monitoring and constant nursing observation. In the home or ward, where observation is less than that available in the ICU, apnoea may be detected by the use of a pressure sensor in a pad or mattress under the infant, or by impedance pneumography, in which diaphragmatic movement causes a change in resistance between two electrodes on the skin. Apnoea of central origin is detected early by these devices but obstructive apnoea, resulting in paradoxical respiratory effort, is detected late. Some devices incorporate electrocardiogram monitoring and rely upon bradycardia as evidence of hypoxaemia, which is a useful but late sign in obstructive apnoea, when both hypoxaemia and movement of the diaphragm are present. False-positive alarms are not uncommon.
THERMOREGULATION
RADIANT HEATERS AND INCUBATORS
Adequate temperature regulation is essential in neonates and infants to avoid cold stress and to maintain a thermoneutral environment.22 Numerous heaters and incubators are available with special features for transport, resuscitation, intensive care and regular ward nursing. Open-type radiant heaters (e.g. Drager Babytherm 8000 OC, Air Shields Vickers IICS-90, Datex Ohmeda Infant Warmers series) are more suitable for use in intensive care. The ideal radiant heater should incorporate:
Incubators are less suitable for use in intensive care because of limited access, but are better for transportation. Heating is via a conductive mattress. Double-walled infant incubators (e.g. Air-Shields Isolette C2000) reduce heat loss, attain preset temperature rapidly, do not produce excessive air currents or sound levels, and do not permit carbon dioxide accumulation.23 Oxygen therapy and mechanical ventilation are possible with both types of unit, but are technically easier with all open-cot radiant heaters.
HUMIDIFIERS
Adequate humidification of ventilator circuits is of utmost importance in the paediatric patient. Unless adequately humidified, the relatively narrow endotracheal and tracheostomy tubes are prone to encrustation and blockage. Insensible water and heat loss are also prevented with adequate humidification. High-flow heated humidifiers provide near 100% humidification (44 mg H2O/l gas, 47 mmHg) at body temperature and are preferred. They are easily adapted for use into ventilator circuits, face and tracheostomy masks, T-piece circuits and oxygen head boxes. When used in ventilator circuits, it is important to realise that they contribute to internal compliance and a compressible volume, which produce errors in both volume-preset and pressure-preset ventilators. Ideally, the compliance should not exceed 1.0 ml/cmH2O for infants less than 10 kg body weight.24
Several methods exist to maintain the water level including an airlock system, parallel-fill system, float-system and a pinch-clamp system.5 Systems that automatically maintain a constant level are preferred for the aforementioned reasons. Incorporation of servo-control is also important. A thermistor probe incorporated into the proximal inspiratory circuit and heating of the inspiratory limb ensure that gas is delivered to the patient at body temperature. However, because some heat loss may occur along the inspiratory limb and much more along the expiratory limb (which is not heated), significant condensation (rain-out) occurs. A water trap must be incorporated to gather ‘rain-out’ and the circuit, particularly the expiratory limb, positioned in a dependent manner to prevent aspiration by the patient. Such water, although potentially contaminated by airway bacteria, does not pose nosocomial infection risk and may be allowed to drain into the humidifier where high temperature inhibits bacterial growth. Circuits may be changed infrequently. Examples of servo-controlled heated humidifiers are Puritan-Bennett Cascade II and Fisher and Paykel MR600, 700, 720, 850 series.
Condenser-type humidifiers or ‘artificial noses’ have a role in intensive care. They are passive humidifiers capturing exhaled water vapour and heat, permitting their reuse on inhalation (heat and moisture exchangers, HME). Numerous devices exist, some incorporating filters and/or hydroscopic materials leading to subclassifications of heat and moisture exchanging filter (HMEF), hydroscopic heat and moisture exchanger (HHME) and hydroscopic heat and moisture exchanging filter (HHMEF). They are often added to tracheostomy or endotracheal tubes of spontaneously breathing patients or inserted into the inspiratory limb of a ventilator circuit for short periods, e.g. for transport. They cannot replace full humidification. HMEs provide approximately one-quarter to one-third relative humidity whereas HHME/HHMEFs provide approximately one-half to three-quarters relative humidity.5 Problems with these devices include deterioration of performance with time, resistance and dead space. The appropriate size for the patient (adult, paediatric, neonatal) must be used. They are not suitable for use if the patient is hypothermic, has thick or bloody secretions or requires frequent changes. They should never be used in conjunction with heated water humidifiers because of potential circuit blockage. They should not be moistened and the addition of oxygen, although sanctioned by some manufacturers, will compromise performance.
MISCELLANEOUS EQUIPMENT
INFUSION DEVICES
Numerous electromechanical devices have been developed to overcome the deficiencies of gravity-fed i.v. infusion sets. They enable constant and accurate infusion of predetermined volumes. These devices have wide clinical application and are used to control the administration of potent drugs, hormones and parenteral nutrition. Performance and application are variable.25,26
SYRINGE PUMPS AND DRIVERS
These are suitable for infusion of potent drugs in concentrated form at very low rates (down to 0.1 ml/hour). They are mains electricity and/or battery powered. The latter are suitable for use during transport and miniaturised models are suitable for ambulant use. These devices are suitable for i.v., intra-arterial, intramuscular, subcutaneous infusion or enterogastric feeding, being particularly suitable for use in neonates and infants. They are not suited to infusion of large volumes and offer no safeguard against extravasation unless an overpressure alarm is incorporated. Generally, the pumps utilise specified syringes unless recalibrated. Some syringe brands do not run smoothly. At low flows (< 1 ml/hour) infusion line compliance contributes to irregular drug delivery associated with vertical displacement of the pump.27
INDIRECT MEASUREMENT OF BLOOD PRESSURE
Continuous non-invasive measurement of blood pressure may be measured with the Ohmeda Finapres non-invasive blood pressure monitor. Blood pressure measured with these non-invasive devices correlates well with simultaneous measurement by direct intra-arterial measurement in neonates,28 infants and children.29 Generally, systolic pressure is underestimated by only 2–4 mmHg (0.3–0.5 kPa), while the diastolic pressure is overestimated by a similar amount. Venostasis and radial nerve compression are occasional complications.30
PLASMAPHERESIS/HAEMOFILTRATION
Generally, the techniques described in dialytic therapy are applicable to infants and children. Although separate veins – or an artery and a vein – may be cannulated, it is common to perform these procedures via a double lumen catheter inserted into a large vein (femoral, jugular, subclavian), i.e. to perform continuous venovenous haemo/diafiltration (CVVH, CVVHD), plasmafiltration or haemoperfusion. In infants (0–1 year), this requires a 6.5 FR catheter to achieve blood flow of 25–40 ml/min, small children (1–8 years) an 8.5 FR catheter to achieve 30–60 ml/min and in large children (> 8 years) an 11 FR catheter to achieve 50–100 ml/min via a blood pump (e.g. Gambro MPM 10, Kimal ultra or Infomed HF400). Typically, the filtration rate is approximately one-third of the blood flow while the size of the molecules appearing in the filtrate is determined by filter size. To remove molecules up to 30 000 Daltons, Gambro FH 22, 55, 66, 77 or 88 is used. To remove molecules up to 3 million Daltons, Gambro PF1000 or PF2000 is used.
1 Greenbaum DM, Marshall KE. The value of routine daily chest X-rays in intubated patients in the medical intensive care unit. Crit Care Med. 1982;10:29-30.
2 Bosman YK, Foster PA. Endotracheal intubation and head posture in infants. South Afr Med J. 1977;52:71-78.
3 Scoble MK, Copnell B, Taylor A, et al. Effect of reusing suction catheters on the occurrence of pneumonia in children. Heart Lung. 2001;30:225-233.
4 Carter BG, Fairbank B, Tibballs J, et al. Oxygen delivery using self-inflating resuscitation bags. Pediatr Crit Care Med. 2005;6:125-128.
5 Branson RD, Hess DR, Chatburn RL. Respiratory Care Equipment. Philadelphia: Lippincott Williams and Wilkins, 1999.
6 Abrahams N, Fisk GC, Vonwiller JB, et al. Evaluation of infant ventilators. Anaesth Intensive Care. 1975;3:6-11.
7 Simbruner G, Gregory GA. Performance of neonatal ventilators: the effects of changes in resistance and compliance. Crit Care Med. 1981;9:509-514.
8 Reynolds EOR, Taghizadeh A. Improved prognosis of infants mechanically ventilated for hyaline membrane disease. Arch Dis Child. 1974;49:505.
9 Greenough A, Milner AD. Respiratory support using patient triggered ventilation in the neonatal period. Arch Dis Child. 1992;67:69-71.
10 South M, Morley CJ. Respiratory timing in intubated neonates with respiratory distress syndrome. Arch Dis Child. 1992;67:446-448.
11 Hird MF, Greenough A. Patient triggered ventilation using a flow triggered system. Arch Dis Child. 1991;66:1140-1142.
12 Cleary JP, Bernstein G, Mannino FL, et al. Improved oxygenation during synchronized intermittent mandatory ventilation in neonates with respiratory distress syndrome: a randomized, crossover study. J Pediatr. 1995;126:407-411.
13 Ogawa Y, Miyasaka K, Kawano T, et al. A multicenter randomized trial of high frequency oscillatory ventilation as compared with conventional mechanical ventilation in preterm infants with respiratory failure. Early Human Dev. 1993;32:1-10.
14 HiFO study group. Randomized study of high-frequency oscillatory ventilation in infants with severe respiratory distress syndrome. J Pediatr. 1993;122:609-619.
15 Shann F, Gatachalian S, Hutchinson R. Nasopharyngeal oxygen in children. Lancet. 1988;2:1238-1240.
16 Cole AGH. Small oxygen analysers. Br J Hosp Med. 1983;29:469-471.
17 Martin RJ, Robertson SS, Hopple MM. Relationship between transcutaneous and arterial oxygen tension in sick neonates during mild hyperoxaemia. Crit Care Med. 1982;10:670-672.
18 Tremper KK, Shoemaker WC, Shippy CR, et al. Transcutaneous oxygen monitoring of critically ill adults with and without low flow shock. Crit Care Med. 1981;9:706-709.
19 Tremper KK, Shoemaker WC, Shippy CR, et al. Transcutaneous PCO2 monitoring on adult patients in the ICU and operating room. Crit Care Med. 1981;9:752-755.
20 Carter BG, Carlin JB, Tibballs J, et al. Accuracy of two pulse oximeters at low arterial hemoglobin–oxygen saturation. Crit Care Med. 1998;26:1128-1133.
21 Brown LW. Home monitoring of the high-risk infant. Clin Pediatr. 1984;11:85-100.
22 Hull D, Chellappah G. On keeping babies warm. In: Chiswick ML, editor. Recent Advances in Perinatal Medicine. Edinburgh: Churchill Livingstone; 1983:153-168.
23 Bell EF, Rios GR. Performance characteristics of two double-walled infant incubators. Crit Care Med. 1983;11:663-667.
24 Holbrook PR, Taylor G, Pollak MM, et al. Adult respiratory distress syndrome in children. Pediatr Clin North Am. 1980;27:677-685.
25 Shyam VSR, Tinker J. Recent developments in infusion devices. Br J Hosp Med. 1981;25:69-75.
26 Dickenson JR. Syringe pumps. Br J Hosp Med. 1983;29:187-191.
27 Weiss M, Banziger O, Neff T, et al. Influence of infusion line compliance on drug delivery rate during acute line loop formation. Intensive Care Med. 2000;26:776-779.
28 Lui K, Doyle PE, Buchanan N. Oscillometric and intra-arterial blood pressure measurements in the neonates: evaluation and comparison of methods. Aust Paediatr J. 1982;18:32-34.
29 Savage JM, Dillon MJ, Taylor JFN. Clinical evaluation and comparison of the infrasonde, arteriosonde and mercury sphygmomanometer in measurements of blood pressure in children. Arch Dis Child. 1979;54:184-189.
30 Showman A, Betts EK. Hazard of automatic noninvasive blood pressure monitoring. Anesthesiology. 1981;55:717-719.