Chapter 64 Principles of antibiotic use
The intensive care unit (ICU) is always the area of any hospital associated with the greatest use of antibiotics. Much of this high usage is unavoidable, but the clinician working in the ICU must realise that there is an essential consequence of this use. Antibiotic use which should eliminate susceptible organisms promotes (over)growth of other, non-susceptible organisms, especially fungi. As far as bacteria are concerned, antibiotics confer enormous selective advantage to resistant strains, and therefore these strains will congregate where their advantage is greatest, in the ICU. Resistance (and fungal overgrowth) is a direct consequence of usage, and every course of inappropriate antibiotics should be avoided to help reduce the burden of resistance.
Antibiotic stewardship1 has been suggested as a new strategy to help limit resistance. This involves selecting an appropriate drug and optimising its dose and duration to cure an infection while minimising toxicity and conditions for selection of resistant bacterial strains. Inadequate doses of even the ‘correct’ antibiotic may lead to survival of initially susceptible organisms.2,3 For the optimal use of antibiotics not only should antibiotic pharmacokinetics be understood, but there should be clear and rational principles on which each specific antibiotic prescription in the ICU is based. Also, it is probably better to have portions of the ICU population receive different classes of antibiotics at the same time.
GENERAL PRINCIPLES4–8
| Old | New |
|---|---|
| Start with penicillin | Get it right first time (broad-spectrum) |
| Cost-efficient low dose | Hit hard up front |
| Low doses = fewer side-effects | Low dose → resistance |
| Long courses ≥ 2 weeks | Seldom longer than 7 days |
COMMON ERRORS WHEN USING ANTIBIOTICS
SPECIFIC ISSUES
PHARMACOKINETIC PRINCIPLES
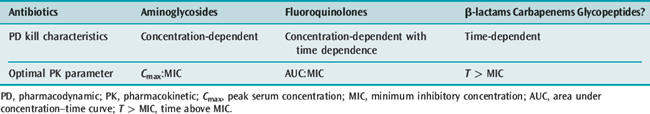
The various antibiotic classes have different ‘kill characteristics’ and therefore should be dosed differently21 (Table 64.2).
β-LACTAMS (ALL PENICILLINS AND CEPHALOSPORINS, MONOBACTAMS)22,23
CARBAPENEMS
AMINOGLYCOSIDES (THE BEST PHARMACOKINETICALLY STUDIED OF THE ANTIBIOTIC CLASSES)22,23
QUINOLONES22,23
ANTIBIOTIC PROPHYLAXIS4,6,7,28
The main indications for prophylaxis are:
Basic principles of choice of prophylactic regimen should include:
TIMING AND DURATION OF PROPHYLAXIS
DOSES
SURVEILLANCE
Some type of simple laboratory-oriented surveillance which primarily collects data and resistance patterns of microbiological isolates is important. There are a few international projects,11 but each unit should have access to its own such data as there is increasing prevalence of resistant organisms in ICUs. This is complicated even further by different units having differing resistance patterns.10 Empiric antibiotic therapy must take these factors into account. Some form of surveillance that provides units with their own microbiological data, updatable quarterly or biannually, is therefore beneficial in helping choose empiric and prophylactic regimens that are applicable to any specific unit.10
MULTIRESISTANT ORGANISMS
Although this chapter is on antibiotics, the point must be made that without good, efficient and effective infection control policies in all areas treating critically ill patients, the spread of multiresistant organisms would be rampant and the control thereof useless.20 Part of these policies should involve attention to good hand hygiene and the use of antiseptic soaps and alcohol-based hand rubs.20 Hands are still the most documented and incriminated mode of transmission of infection. In this regard a decrement in nursing numbers has also been incriminated in outbreaks of infections, possibly due to the time it takes to wash adequately between procedures.20
MONOTHERAPY VERSUS COMBINATION THERAPY14,15
BROAD-SPECTRUM INITIAL COVER WITH DE-ESCALATION32 (SEE Table 64.1)
In view of the morbidity and mortality of delayed appropriate therapy for nosocomial sepsis,12,13,32 particularly pneumonias, patients with risk factors for infection with resistant pathogens should initially receive broad-spectrum antibiotics, possibly even combination therapy,12,32 and, as soon as the pathogen and the susceptibilities are available, treatment should be simplified to a more targeted one – so-called ‘de-escalation’ therapy.32 In the limited studies to date, de-escalation has led to less antibiotic usage, shorter durations of therapy, fewer episodes of secondary pneumonia and reduced mortality, without increasing the frequency of antibiotic resistance.
1 Fishman N. Antimicrobial stewardship. Am J Med. 2006;119:S53-61.
2 Tam VH, Schilling AN, Neshat S, et al. Optimization of meropenem minimum concentration/MIC ratio to suppress in vitro resistance of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49:4920-4927.
3 Zhou J, Dong Y, Zhao X, et al. Selection of antibiotic-resistant bacterial mutants: allelic diversity among fluoroquinolone-resistant mutations. J Infect Dis. 2000;182:517-525.
4 Reese RE, Douglas RGJnr, editors. A Practical Approach to Infectious Diseases. Boston: Little, Brown, 1986.
5 Lundberg GD. Making use of the microbiology laboratory. 1. Use of the laboratory. JAMA. 1982;247:857-859.
6 Sanford JP. Guide to Antimicrobial Therapy. West Bethesda, Maryland: Antimicrobial Therapy, 1993.
7 Mandell GL, Douglas RG, Bennett JE. Principles and Practice of Infectious Diseases, 4th edn. New York: Churchill Livingstone, 1994.
8 Neu HC. Antimicrobial agents: role in the prevention and control of nosocomial infections. In: Wentzel RP (ed.) Prevention and Control of Nosocomial Infections, 2nd edn. Baltimore: Williams & Williams; Chapter 18
9 Weinstein MP. Current blood culture methods and systems: clinical concepts, technology, and interpretation of results. Clin Infect Dis. 1996;23:40-46.
10 Namias N, Samiian L, Nino D, et al. Incidence and susceptibility of pathogenic bacteria vary between intensive care units within a single hospital: implications for empiric antibiotic strategies. J Trauma. 2000;49:638-645.
11 Marchese A, Schito GC. Role of global surveillance in combating bacterial resistance. Drugs. 2001;61:167-173.
12 Mutlu GM, Wunderink RG. Severe pseudomonal infections. Curr Opin Crit Care. 2006;12:458-463.
13 Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31(Suppl. 4):S131-8.
14 Paul M, Benuri-Silbiger I, Soares-Weiser K, et al. Beta lactam monotherapy versus beta lactam-aminoglycoside combination therapy for sepsis in immuno-competent patients: systematic review and meta-analysis of randomised trials. Br Med J. 2004;328:668-672.
15 Safar N, Handelsman J, Maki DG. Does combination antimicrobial therapy reduce mortality in Gram-negative bacteraemia? A meta-analysis. Lancet Infect Dis. 2004;4:519-527.
16 Chastre J, Wolff M, Fagon JY, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290:2588-2598.
17 Singh N, Rogers P, Atwood CW, et al. Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med. 2000;162:505-511.
18 Baker EM, Aitchison JM, Crindland JS, et al. Rectal administration of metronidazole in severely ill patients. Br Med J. 1983;287:311-314.
19 Uzzan B, Cohen R, Nicolas P, et al. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med. 2006;34:1996-2003.
20 Pittet D, Allegranzi B, Sax H, et al. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006;6:641-652.
21 Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26:1-10.
22 Pinder M, Bellomo R, Lipman J. Pharmacological principles of antibiotic prescription in the critically ill. Anaesth Intens Care. 2002;30:134-144.
23 Roberts J, Lipman J. Antibacterial dosing in intensive care: pharmacokinetics, degree of disease and pharmacodynamics of sepsis. Clin Pharmacokinet. 2006;45:755-773.
24 Lipman J, Wallis S, Rickard C. Low cefepime levels in critically ill septic patients: pharmacokinetic modeling indicates improved troughs with revised dosing. Antimicrob Agents Chemother. 1999;43:2559-2561.
25 Kasiakou SK, Lawrence KR, Choulis N, et al. Continuous versus intermittent intravenous administration of antibacterials with time-dependent action: a systematic review of pharmacokinetic and pharmacodynamic parameters. Drugs. 2005;65:2499-2511.
26 Lomaestro BM, Drusano GL. Pharmacodynamic evaluation of extending the administration time of meropenem using a Monte Carlo simulation. Antimicrob Agents Chemother. 2005;49:461-463.
27 Nicolau DP, Freeman CD, Belliveau PP, et al. Experience with a once daily aminoglycoside program administered to 2184 adult patients. Antimicrob Agents Chemother. 1995;39:650-655.
28 Classen DC, Evans RS, Pestotnik SL, et al. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992;326:281-286.
29 Nimmo GR, Coombs GW, Pearson JC, et al. Meticillin-resistant Staphylococcus aureus in the Australian community: an evolving epidemic. Med J Aust. 2006;184:384-388.
30 Schmidt-Ioanas M, de Roux A, Lode H. New antibiotics for the treatment of severe staphylococcal infection in the critically ill patient. Curr Opin Crit Care. 2005;11:481-486.
31 Rahal JJ. Novel antibiotic combinations against infections with almost completely resistant Pseudomonas aeruginosa and Acinetobacter species. Clin Infect Dis. 2006;43(Suppl. 2):S95-9.
32 Niederman MS. De-escalation therapy in ventilator-associated pneumonia. Curr Opin Crit Care. 2006;12:452-457.