Chapter 667 Torsional and Angular Deformities
667.1 Normal Limb Development
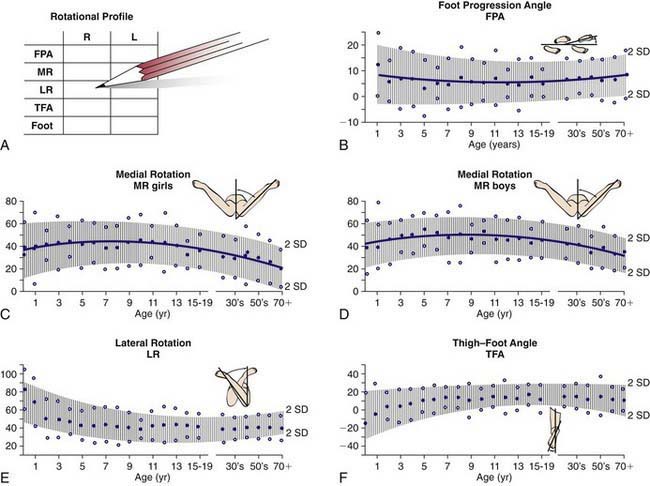
An understanding of normal limb development is essential for pediatricians to recognize pathologic conditions during routine and targeted exams. During the 7th wk of intrauterine life, the lower limb rotates medially to bring the great toe toward the midline. The hip joint forms by the 11th wk; the proximal femur and acetabulum continue to develop until physeal closure in adolescence. At birth, the femoral neck is rotated forward approximately 40 degrees. This forward rotation is referred to as anteversion (the angle between the axis of the femoral neck and the transcondylar axis). The increased anteversion increases the internal rotation of the hip. Femoral anteversion decreases to 15-20 degrees by 8-10 yr of age. The second source of limb rotation is found in the tibia. Infants can have 30 degrees of medial rotation of the tibia, and by maturity the rotation is between 5 degrees of medial rotation and 15 degrees of lateral rotation (Fig. 667-1). Excessive medial rotation of tibia is referred to as medial tibial torsion. The tibial torsion is the angular difference between the axis of the knee and the transmalleolar axis. The medial or lateral rotation beyond ±2 standard deviations (SDs) from the mean is considered abnormal rotation.
The normal tibiofemoral angle at birth is 10-15 degrees of physiologic varus. The alignment changes to 0 degrees by 18 mo, and physiologic valgus up to 12 degrees is reached in between 3 and 4 yr of age. The normal valgus of 7 degrees is achieved by 5-8 yr of age (Fig. 667-2). Persistence of varus beyond 2 yr of age may be pathologic. Overall, 95% of developmental physiologic genu varum and genu valgum cases resolve with growth. Persistent genu valgum or valgus into adolescence is considered pathologic and deserves further evaluation.
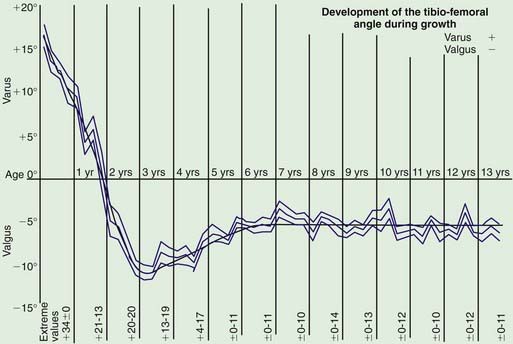
Figure 667-2 The normal coronal alignment of the knee plotted for age.
(From Salenius P, Vanka E: The development of the tibiofemoral angle in children. J Bone Joint Surg Am 57:259–261, 1975.)
Arazi M, Ogun TC, Memik R. Normal development of the tibiofemoral angle in children: a clinical study of 590 normal subjects from 3 to 17 years of age. J Pediatr Orthop. 2001;21:264-267.
Cahuzac JP, Vardon D, Sales de Gauzy J. Development of the clinical tibiofemoral angle in normal adolescents: a study of 427 normal subjects from 10 to 16 years of age. J Bone Joint Surg Br. 1995;77:729-732.
Heath CH, Staheli LT. Normal limits of knee angle in white children—genu varum and genu valgum. J Pediatr Orthop. 1993;13:259-262.
Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259-261.
667.2 Evaluation
Foot Progression Angle
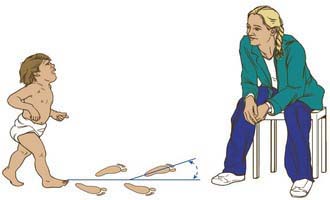
Limb position during gait is expressed as the foot progression angle (FPA) and represents the angular difference between the axis of the foot with the direction in which the child is walking. Its value is usually estimated by asking the child to walk in the clinic hallway (Fig. 667-3). Inward rotation of the foot is assigned a negative value, and outward rotation is designated with positive value. The normal FPA in children and adolescents is 10 degrees (range, −3 to 20 degrees). The FPA serves only to define whether there is an in-toeing or out-toeing gait.
Femoral Anteversion
Measuring the hip rotation with the child in prone position, the hip in neutral flexion or extension, thighs together, and the knees flexed 90 degrees indirectly assesses the anteversion (Fig. 667-4). Both hips are assessed at the same time. As the lower leg is rotated ipsilaterally, this produces internal rotation of the hip, whereas contralateral rotation produces external rotation. Excessive anteversion increases internal rotation, and, retroversion increases the external rotation.
Tibial Rotation
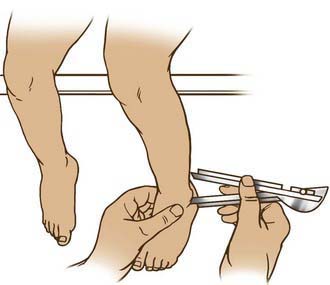
Tibial rotation is measured using the transmalleolar angle (TMA). The TMA is the angle between the longitudinal axis of the thigh with a line perpendicular to the axis of the medial and lateral malleolus (Fig. 667-5). In the absence of foot deformity, the thigh foot angle (TFA) is preferred (Fig. 667-6). It is measured with the child lying prone. The angle is formed between the longitudinal axis of the thigh and the longitudinal axis of the foot. It measures the tibial and hindfoot rotational status. Inward rotation is assigned a negative value, and outward rotation is designated a positive value. Inward rotation indicates internal tibial torsion, whereas outward rotation represents external tibial torsion. Infants have a mean angle of −5 degrees (range, −35 to 40 degrees) as a consequence of normal in utero position. In mid-childhood through adult life, the mean TFA is 10 degrees (range, −5 to 30 degrees).
Foot Shape and Position
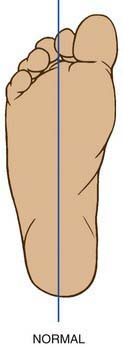
The foot is observed for any deformities in prone and standing position. The heel bisector line (HBL) is used to evaluate the foot adduction and abduction deformities. The HBL is a line that divides the heel in two equal halves along the longitudinal axis (Fig. 667-7). It normally extends to the 2nd toe. When the HBL points medial to the 2nd toe, the forefoot is abducted, and when the HBL is lateral to the 2nd toe, the forefoot is adducted.
Ruwe PA, Gage JR, Ozonoff MB, et al. Clinical determination of femoral anteversion: a comparison of established techniques. J Bone Joint Surg Am. 1992;74:820-830.
Thompson GH. Gait disturbances. In: Kliegman RM, editor. Practical strategies in pediatric diagnosis and therapy. ed 2. Philadelphia: WB Saunders; 2003:823-843.
667.3 Torsional Deformities
Metatarsus Adductus
Metatarsus adductus (Chapter 666.01) manifests with forefoot adduction and inversion of all metatarsals. Ten to 15% are associated with hip dysplasia. The prognosis is good, because the majority get better with nonoperative intervention. The feet, which are flexible and correctable up to neutral, are treated with stretching exercises. Those that are not completely correctable are treated with serial casting. Rigid deformities, which are not correctable by stretching, are treated with medial capsulotomy of the 1st metatarsal cuneiform joint and soft-tissue release by 2 yr of age. Osteotomies of the base of the metatarsal are usually done after 6 yr of age.
667.4 Coronal Plane Deformities
Genu varum and genu valgum are common pediatric deformities of the knee. The age-appropriate normal values for knee angle are presented in Figure 667-2. Tibial bowing is common during the 1st year, bowlegs are common during the 2nd year, and knock-knees are most prominent between 3 and 4 yr of age.
Genu Varum
Physiologic bowleg is a common torsional combination that is secondary to normal in utero positioning (Fig. 667-8). Spontaneous resolution with normal growth and development can be anticipated. Persistence of varus beyond 2 yr of age may be pathologic. The different causes are metabolic bone disease (vitamin D deficiency, rickets, hypophosphatasia), asymmetric growth arrest (trauma, infection, tumor, Blount), bone dysplasia (dwarfism, metaphyseal dysplasia), and congenital and neuromuscular disorders (Table 667-1). It is prudent to differentiate physiologic bowing from Blount disease (Table 667-2). Physiologic bowing should also be differentiated from rickets and skeletal dysplasia. Rickets has classic bone changes with trumpeting widening and fraying of the metaphysis and widening of the physis (Chapter 48).
Table 667-1 CLASSIFICATION OF GENU VARUM (BOWLEGS)
PHYSIOLOGIC
ASYMMETRIC GROWTH
METABOLIC DISORDERS
SKELETAL DYSPLASIA
Modified from Thompson GH: Angular deformities of the lower extremities. In Chapman MW, editor: Operative orthopedics, ed 2, Philadelphia, 1993, JB Lippincott, pp 3131–3164.
| PHYSIOLOGIC BOWING | BLOUNT DISEASE |
|---|---|
| Gentle and symmetric deformity | Asymmetric, abrupt, and sharp angulation |
| Metaphyseal-diaphyseal angle <11 degrees | Metaphyseal-diaphyseal angle >11 degrees |
| Normal appearance of the proximal tibial growth plate | Medial sloping of the epiphysis Widening of the physis Fragmentation of the metaphysis |
| No significant lateral thrust | Significant lateral thrust |
Tibia Vara
Idiopathic tibia vara, or Blount disease, is a developmental deformity resulting from abnormal endochondral ossification of the medial aspect of the proximal tibial physis leading to varus angulation and medial rotation of the tibia (Fig. 667-9). The incidence is greater in African-Americans and in toddlers who are overweight, have an affected family member, or started walking early in life. It has been classified into three types depending on the age at onset: infantile (1-3 yr), juvenile (4-10 yr), and adolescent (11 yr or older). The juvenile and adolescent forms are commonly combined as late-onset tibia vara. The exact cause of tibia vara remains unknown.
An anteroposterior standing radiograph of both lower extremities with patellas facing forward and a lateral radiograph of the involved extremity should be obtained (Fig. 667-10). Weight-bearing radiographs are preferred and allow maximal presentation of the clinical deformity. The metaphyseal-diaphyseal angle can be measured and is useful in distinguishing between physiologic genu varum and early tibia vara (Fig. 667-11). Langenskiöld has six stages on radiographs (Fig. 667-12). The differentiation is based on fragmentation of the epiphysis, beaking of the medial tibial epiphysis, depression of the medial tibial plateau, and formation of a bony bar. Occasionally, CT with three-dimensional reconstructions, or MRI, may be necessary to assess the meniscus, the articular surface of the proximal tibia including the posteromedial slope, or the integrity of the proximal tibial physis.
Cheema JI, Grissom LE, Harcke HT. Radiographic characteristics of lower-extremity bowing in children. Radiographics. 2003;23(4):871-880.
Davids JR, Blackhurst DW, Allen BLJr. Radiographic evaluation of bowed legs in children. J Pediatr Orthop. 2001;21:257-263.
Do TT. Clinical and radiographic evaluation of bowlegs. Curr Opin Pediatr. 2001;13:42-46.
Doyle BS, Volk G, Smith CI. Infantile Blount’s disease: long-term follow-up of surgically treated patients at skeletal maturity. J Pediatr Orthop. 1996;16:469-476.
Feldman MD, Schoenecker PL. Use of metaphyseal-diaphyseal angle in the evaluation of bowed legs. J Bone Joint Surg Am. 1993;75:1602-1609.
Henderson RC, Kemp GJ, Greene WB. Adolescent tibia vara: alternatives for operative treatment. J Bone Joint Surg Am. 1992;74:342-350.
Henderson RC, Kemp GJ, Hayes PRL. Prevalence of late-onset tibia vara. J Pediatr Orthop. 1993;13:255-258.
Johnston CEII. Infantile tibia vara. Clin Orthop. 1990;255:13-23.
Sabharwal S. Blount disease. J Bone Joint Surg Am. 2009;91:1758-1776.
Stevens PM, Maguire M, Dales MD, et al. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop. 1999;19:645-649.
Thompson GH. Angular deformities of the lower extremities in children. In: Chapman MW, editor. Operative orthopedics. ed 3. Philadelphia: JB Lippincott; 2001:4287-4335.
667.5 Congenital Angular Deformities of the Tibia and Fibula
Wallach DM, Davidson RS. Pediatric lower limb disorders. In: Dormans JP, editor. Core knowledge in orthopaedics: pediatric orthopaedics. Philadelphia: Mosby; 2005:197-223.
Wallach DM, Davidson RS. Pediatric lower limb disorders. In: Dormans JP, editor. Pediatric orthopaedics and sports medicine: the requisites in pediatrics. Philadelphia: Mosby; 2005:246-272.