Chapter 671 The Spine
Abnormalities of the spine may be present at birth (congenital), can develop during childhood or adolescence, or can result from traumatic injuries. Alterations in spinal alignment are commonly of cosmetic concern to the patient and family. Sequelae from progressive spinal deformities include pain, cardiopulmonary dysfunction, and a loss of sitting balance (nonambulators). Early detection helps to facilitate treatment and to identify and address coexisting visceral and/or neurologic problems that may be associated with a spinal deformity. A classification of common spinal abnormalities is presented in Table 671-1.
Table 671-1 CLASSIFICATION OF SPINAL DEFORMITIES
SCOLIOSIS
Idiopathic
Congenital
Neuromuscular
Myopathies
Syndromes
Compensatory
KYPHOSIS
Adapted from the Terminology Committee, Scoliosis Research Society: A glossary of scoliosis terms, Spine 1:57, 1976.
671.1 Idiopathic Scoliosis
Etiology and Epidemiology
Scoliosis is a complex, 3-dimensional deformity of the spine, with abnormalities in the coronal, sagittal, and axial planes. The diagnosis is based on a coronal plane curvature of >10 degrees using the Cobb method. Idiopathic scoliosis is a diagnosis of exclusion; other causes must be ruled out (see Table 671-1). The etiology of idiopathic scoliosis remains unknown and is likely multifactorial, involving both genetic and environmental components. Major theories have been based on genetic factors, metabolic dysfunction (melatonin deficiency, calmodulin), neurologic dysfunction (craniocervical, vestibular and oculovestibular), and biomechanical factors (asynchrony in spinal growth, anterior spinal overgrowth, and others). With regard to genetic factors, although several different modes of inheritance have been suggested (autosomal dominant, multifactorial, X-linked), a single locus has yet to be identified. Abnormalities identified in connective tissue, muscle, and bone appear to be secondary. Melatonin and calmodulin might have indirect effects, and subtle abnormalities in vestibular, ocular, and proprioceptive function suggest that abnormal equilibrium might also play a role.
Clinical Manifestations
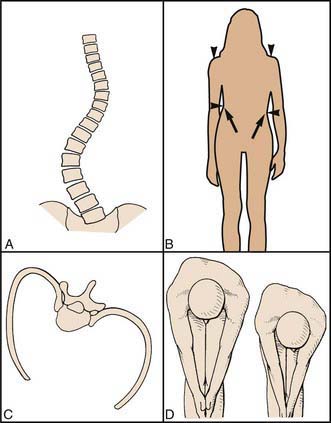
Patients usually present with a change in cosmetic appearance noted by family and/or friends or on a screening examination by a school nurse or primary care physician. The patient is evaluated in the standing position, from both the front and the side, to identify any asymmetry in the chest wall, trunk, and/or shoulders. Asymmetry of the posterior chest wall on forward bending (the Adams test) is the earliest abnormality (Fig. 671-1). Rotation of the vertebral bodies toward the convexity results in rotation and prominence of the attached ribs posteriorly. The anterior chest wall may be flattened on the concavity, due to inward rotation of the chest wall and ribs. Associated findings can include elevation of the shoulder, a lateral shift of the trunk, and an apparent leg-length discrepancy. The patient should also be evaluated from the side. The thoracic spine normally has a smooth, rounded kyphosis (20-50 degrees using the Cobb method from T3-T12) that extends down to the thoracolumbar junction, and the lumbar spine is normally lordotic (30-60 degrees using the Cobb method from T12-L5). Children normally have less cervical lordosis and more lumbar lordosis than do adults or adolescents. Typically, idiopathic scoliosis results in a loss of the normal thoracic kyphosis in the region of curvature (relative thoracic lordosis).
Radiographic Evaluation
Standing high-quality posteroanterior (PA) and lateral radiographs of the entire spine are recommended at the initial evaluation for patients with clinical findings that suggest a spinal deformity. On the PA radiograph, the degree of curvature is determined by the Cobb method, in which the angle between the superior and inferior end vertebra (tilted into the curve) is measured (Fig. 671-2). A line is drawn across the superior end plate of each end vertebra, and the angle between perpendicular lines erected from each of these is measured. Although the indications for performing MRI are variable, this modality is helpful when an underlying cause for the scoliosis is suspected based on age (infantile, juvenile curves), abnormal findings on the history and physical examination, and atypical radiographic features (curve patterns and/or specific features). Atypical radiographic findings include uncommon curve patterns such as the left thoracic curve, double thoracic curves, high thoracic curves, widening of the spinal canal, and erosive or dysplastic changes in the vertebral body or ribs. On the lateral radiograph, an increase in thoracic kyphosis or an absence of segmental lordosis might suggest the presence of an underlying diagnosis.
Treatment
Bracing
There are several options for braces (Fig. 671-3). The Milwaukee brace, employing longitudinal traction from the skull to the pelvis with lateral compression of the chest wall, can be adjusted for growth and thus is a good brace for patients with infantile or juvenile scoliosis. Underarm braces (the Boston or Wilmington braces) are less obvious and so are often preferred by adolescents. The Charleston brace provides a corrective force and is used only at night.
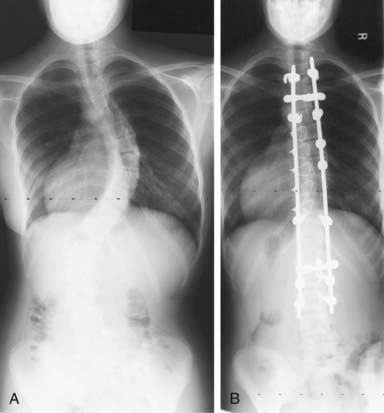
Surgery
The most common procedure is an instrumented posterior spinal fusion, and the typical spinal implant construct includes 2 rods anchored to the spine by hooks, wires, and/or screws (Fig. 671-4). In the last few years there has been significant interest in using a construct with pedicle screws at each level. Although correction of the axial deformity (rotation of the rib cage) is more pronounced with this technology, it remains unclear whether patient outcomes are improved. An anterior release and fusion, performed through a thoracotomy or thoracolumbar exposure, is indicated for isolated thoracolumbar and lumbar curves, to improve correctability of stiffer curves, and to prevent curve progression (“crankshaft”) from continued anterior growth of the spine in selected patients with considerable growth remaining. A construct with multiple pedicle screws can allow the surgeon to avoid an anterior approach in many larger or stiffer curves (more powerful correction) and in younger patients (stiff enough to resist anterior spinal growth and prevent crankshaft). Thoracoscopic surgery has also been used to perform an anterior release with or without instrumentation and fusion, but this technique has been used much less often since the advent of thoracic pedicle screws. For idiopathic thoracolumbar and lumbar curves, an anterior fusion with instrumentation (usually screws in the vertebral body connected to 1 or 2 rods) can be done as an alternative to save lumbar motion segments.
Barsdorf AI, Sproule DM, Kaufman P. Scoliosis surgery in children with neuromuscular disease. Arch Neurol. 2010;67:231-235.
Bunge EM, Juttmann RE, van Biezen FC, et al. Estimating the effectiveness of screening for scoliosis: a case-control study. Pediatrics. 2008;121:9-14.
de Lind van Wijngaarden RFA, de Klerk LWL, Festen DAM, et al. Scoliosis in Prader-Willi syndrome: prevalence, effects of age, gender, body mass index, lean body mass and genotype. Arch Dis Child. 2008;93:1012-1016.
Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence based review. Spine. 2007;32:S91-S100.
Gillingham B, Fan RA, Akbarnia BA. Early onset idiopathic scoliosis. J Am Acad Orthop Surg. 2006;14:101-112.
Kallmes D, Jarvik JG. Spinal augmentation research: free at last? Lancet. 2009;373:982-984.
Katz DE, Herring JA, Browne RH, et al. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010;92:1343-1352.
Kim YJ, Lenke LJ, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006;31:291-298.
Merola AA, Haher TR, Brkaric M, et al. A multi-center study of the outcomes of the surgical treatment of adolescent idiopathic scoliosis using the Scoliosis Research Society (SRS) outcome instrument. Spine. 2002;27:2046-2051.
Negrini S, Minozzi S, Bettany-Saltikov J, et al: Braces for idiopathic scoliosis in adolescents (review), Cochrane Database Rev (1):CD006850, 2010.
Richards BS, Vitale MG. Screening for idiopathic scoliosis in adolescents. An information statement. J Bone Joint Surg Am. 2008;90:195-198.
Tones M, Moss N, Polly DWJr. A review of quality of life and psychosocial issues in scoliosis. Spine. 2006;31:3027-3028.
Weinstein SL, Dolan LA, Cheng JCY, et al. Adolescent idiopathic scoliosis. Lancet. 2008;371:1527-1536.
Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis. JAMA. 2003;289:559-567.
Wright JG, Donaldson S, Howard A, et al. Are surgeon’s preferences for instrumentation related to outcomes? A randomized clinical trial of two implants for idiopathic scoliosis. J Bone Joint Surg Am. 2007;89:2684-2693.
671.2 Congenital Scoliosis
Congenital scoliosis results from abnormal growth and development of the vertebral column, likely due to intrauterine events at or about the 6th wk of gestation. There can be a partial or complete failure of formation (wedge vertebrae or hemivertebrae), a partial or complete failure of segmentation (unilateral unsegmented bars), or a combination of both (Fig. 671-5). One or more bony anomalies can occur in isolation or in combination.
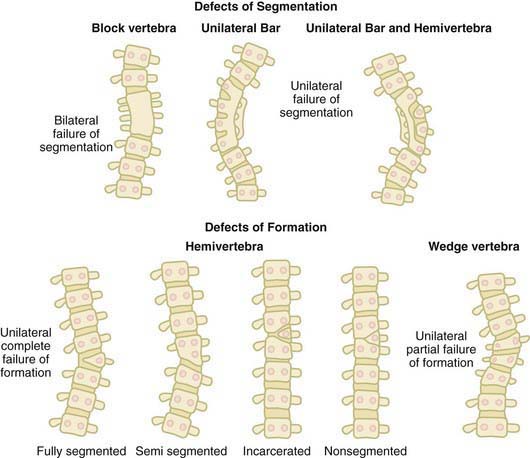
Figure 671-5 The defects of segmentation and formation that can occur during spinal development.
(From McMaster MJ: Congenital scoliosis. In Weinstein SL, editor: The pediatric spine: principles and practice, ed 2, Philadelphia, 2001, Lippincott Williams & Wilkins, p 163.)
Approximately 20-40% of patients have an intraspinal anomaly. Infants with cutaneous abnormalities overlying the spine might benefit from ultrasonography to rule out an occult spinal dysraphic condition. MRI is usually recommended during the course of treatment. Spinal dysraphism is the general term applied to such lesions (Chapters 585 and 598). Examples include diastematomyelia, split cord malformations, intraspinal lipomas (intradural or extradural), arachnoid cysts, teratomas, dermoid sinuses, fibrous bands, and tight filum terminale. Cutaneous findings that may be seen in patients with closed spinal dysraphism include hair patches, skin tags or dimples, sinuses, and hemangiomas. Most of these lesions become clinically evident through tethering of the spinal cord, the symptoms of which include back and/or leg pain, calf atrophy, progressive unilateral foot deformity (especially cavovarus), and problems with bowel or bladder function.
When multiple levels of the thoracic spine are involved, especially in the presence of fused ribs, a progressive 3-dimensional deformity of the chest wall can impair lung development and function, resulting in a thoracic insufficiency syndrome. This syndrome is best described as the inability of the chest wall to support normal respiration. A thoracic insufficiency syndrome may be seen in patients with several recognized conditions, such as Jarcho-Levin syndrome (spondylocostal or spondylothoracic dysplasia) and Jeune syndrome (asphyxiating thoracic dystrophy). There is interest in treating these difficult cases with an experimental technique called expansion thoracoplasty, in which the thoracic cage is gradually expanded over time by progressive lengthening of the chest wall on the concavity of the spinal deformity (or in some cases on both sides of the spine). The procedure involves an opening wedge thoracostomy, followed by placement of a vertical expandable titanium prosthetic rib. The implant is then distracted (lengthened) at regular intervals (Fig. 671-6). The primary goal is to gradually correct the chest wall deformity to improve pulmonary function, and a secondary goal is correction of an associated spinal deformity. This technique is currently not approved for the treatment of scoliosis in the absence of a thoracic insufficiency, and further study will help to refine (and possibly expand) the indications for the technique.
Batra S, Ahuja S. Congenital scoliosis: management and future directions. Acta Orthop Belg. 2008;74(2):147-160.
Campbell RM, Smith MD, Mayes TC, et al. The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am. 2003;85:399-408.
Campbell RAJr, Smith MD, Mayes TC, et al. The effect of opening wedge thoracostomy on thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am. 2004;86:1659-1674.
Karol LA, Johnston C, Mladenov K, et al. Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis. J Bone Joint Surg Am. 2008;90:1271-1281.
Kim YJ, Otsuka NY, Flynn JM, et al. Surgical treatment of congenital kyphosis. Spine. 2001;26:2251-2257.
Kose N, Campbell RM. Congenital scoliosis. Med Sci Monitor. 2004;10(5):RA104-110.
McMaster MJ, Singh H. The surgical management of congenital kyphosis and kyphoscoliosis. Spine. 2001;26:2146-2154.
Smith JT, Gollogly S, Dunn HK. Simultaneous anterior-posterior approach through a costotransversectomy for the treatment of congenital kyphosis and acquired kyphoscoliotic deformities. J Bone Joint Surg Am. 2005;87:2281-2289.
Vitale MG, Matsumoto H, Bye MR, et al. A retrospective cohort study of pulmonary function, radiographic measures, and quality of life in congenital scoliosis: an evaluation of patient outcomes after early spinal fusion. Spine. 2008;33:1242-1249.
671.3 Neuromuscular Scoliosis, Genetic Syndromes, and Compensatory Scoliosis
Compensatory Scoliosis
Leg-length inequality is common and is usually associated with a small compensatory lumbar curvature (Chapter 668). This is 1 cause of false-positive screening examinations. Pelvic tilt toward the short side is associated with a lumbar curve (convexity away from the short leg). There is little evidence to suggest that a small compensatory lumbar curve places the patient at risk of progression or back pain. Because children with leg-length inequality can also have idiopathic or congenital scoliosis, a standing radiograph may be obtained with a block under the foot on the short side (to correct the leg-length discrepancy) to level the pelvis. If the curvature disappears when the limb-length discrepancy is corrected, then a diagnosis of a compensatory curve is made. An alternative is a PA radiograph with the patient seated. In neuromuscular disorders such as polio or cerebral palsy, an adduction or abduction contracture of the hip (fixed infrapelvic contracture) may be compensated for by a lumbar scoliosis to maintain standing or sitting balance. For patients who ambulate, a 10-degree fixed contracture will result in up to 3-cm apparent leg-length discrepancy.
Jones KB, Sponseller PD, Shindle MK, et al. Longitudinal parental perceptions of spinal fusion for neuromuscular spine deformity in patients with totally involved cerebral palsy. J Pediatr Orthop. 2003;23:143-149.
Kotwicki T, Jozwiak M. Conservative management of neuromuscular scoliosis: personal experience and review of literature. Disabil Rehabil. 2008;30(10):792-798.
Mercado E, Alman B, Wright JG. Does spinal fusion influence quality of life in neuromuscular scoliosis? Spine. 2007;32:S120-S125.
Sarwark J, Sarwahi V. New strategies and decision making in the management of neuromuscular scoliosis. Orthop Clin North Am. 2007;38:485-496. v
671.4 Kyphosis (Round Back)
Structural Kyphosis
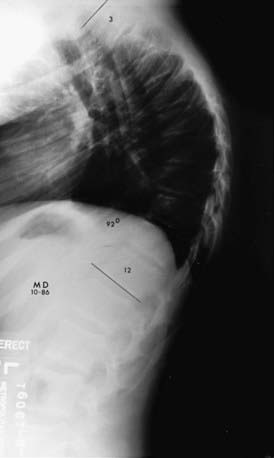
Radiographic Evaluation
Standing PA and lateral radiographs are obtained (Fig. 671-7). The recommended technique for the lateral radiograph involves folding the arms across the chest. A vertical plumb line dropped from C7 should intersect the anterosuperior corner of the sacrum for maintenance of sagittal spinal balance. A coexisting spondylolisthesis is rarely identified on the lateral radiograph. The standing PA radiograph often reveals a mild scoliosis, which is rarely progressive. An MRI is indicated in the presence of neurologic symptoms, and some surgeons routinely obtain an MRI before correcting a kyphosis.
Treatment
Skeletally immature patients with mild deformity might benefit from a hyperextension exercise program, but the effects of this strategy on the natural history remain to be documented. Patients with >1 yr of growth remaining and a kyphosis of >50-60 degrees might benefit from a bracing program. A Milwaukee brace (see Fig. 671-3) that extends up to the neck is recommended for curves with an apex above T7, but curves with a lower apex are often be treated by a thoracolumbar orthosis. The brace is recommended for 23 hr/day. On occasion, a serial casting (or stretching) program is instituted to gain flexibility before instituting the brace program. Although the goal of bracing is to prevent progression, a permanent improvement is observed in some patients. When bracing is effective in achieving permanent correction, radiographs show a reconstitution of anterior vertebral height (reversal of wedging). Skeletally mature patients with little or no pain and acceptable cosmesis are not treated.
Boseker EH, Moe JH, Winter RB, et al. Determination of “normal” thoracic kyphosis: a roentgenographic study of 121 “normal” children. J Pediatr Orthop. 2000;20:796-798.
Lowe TG. Evidence based medicine: analysis of Scheuermann kyphosis. Spine. 2007;32:S115-S119.
Lowe TG, Line BG. Evidence based medicine—analysis of Scheuermann kyphosis. Spine. 2007;32:S115-S119.
Papegelopoulos PJ, Klassen RA, Peterson HA, et al. Surgical treatment of Scheuermann’s disease with segmental compression instrumentation. Clin Orthop Rel Res. 2001;386:139-149.
Petcharaporn M, Pawelek J, Bastrom T, et al. The relationship between thoracic hyperkyphosis and the Scoliosis Research Society outcomes instrument. Spine. 2007;32:2226-2231.
Poolman RW, Been HD, Ubags LH. Clinical outcome and radiographic results after operative treatment of Scheuermann’s disease. Eur Spine J. 2002;11:561-569.
Swischuk LE, John SD, Allbery S. Disk degenerative disease in childhood: Scheurmann’s disease, Schmorl’s nodes, and the limbus vertebra: MRI findings in 12 patients. Pediatr Radiol. 1998;28:334-338.
671.5 Back Pain in Children
Back pain is a relatively common complaint in children and adolescents, and the differential diagnosis is extensive (Table 671-2). Traditionally, it was thought that the majority of back pain in childhood and adolescence had an organic basis, suggesting the need for an extensive evaluation (including imaging studies) in all patients. Although back pain in infants and toddlers is often associated with underlying pathology, the likelihood of establishing a diagnosis in older children and adolescents is much less, roughly similar to that of the adult population. A definitive diagnosis may be established in 22-36%. The prevalence rate (5-75%) increases with age, approaching that of adults by the age of 18 yr, and most episodes of back pain resolve within 6 wk. Back pain can also be referred from the hip, the sacroiliac joint, or a visceral source. There is some evidence to suggest that back pain is more common with greater weights in backpacks. A thorough history and physical examination, often supplemented by imaging modalities, is required to rule out an underlying pathologic process. The treatment of back pain is tailored to the underlying diagnosis.
Table 671-2 DIFFERENTIAL DIAGNOSIS OF BACK PAIN
INFLAMMATORY OR INFECTIOUS
RHEUMATOLOGIC
DEVELOPMENTAL
TRAUMATIC (ACUTE VERSUS REPETITIVE)
NEOPLASTIC
Vertebral Tumors
Benign
Malignant
Spinal cord, ganglia, and nerve roots
OTHER
Auerbach JD, Ahn J, Zgonis MH, et al. Streamlining the evaluation of low back pain in children. Clin Orthop Rel Res. 2008;466:1971-1977.
Balague F, Dudler J, Nordin M. Low-back pain in children. Lancet. 2003;361:1403-1404.
Bhatia NN, Chow G, Timon SJ, et al. Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop. 2008;28:230-233.
Bockowski L, Sobaniec W, Kulak W, et al. Low back pain in school-age children: risk factors, clinical features and diagnostic management. Adv Med Sci. 2007;52(Suppl 1):221-223.
Cohen SP, Argoff CE, Carragee EJ. Management of low back pain. BMJ. 2009;338:100-106.
Davis PJC, Williams HJ. The investigation and management of back pain in children. Arch Dis Child Educ Pract Ed. 2008;93:73-83.
Feldman DS, Straight JJ, Badra MI, et al. Evaluation of an algorithmic approach to pediatric back pain. J Pediatr Ortho. 2006;26:353-357.
Hangai M, Kaneoka K, Okubo Y, et al. Relationship between low back pain and competitive sports activities during youth. Am J Sports Med. 2010;38:791-796.
Jeffries LJ, Milanese SF, Grimmer-Somers KA. Epidemiology of adolescent spinal pain. A systematic overview of the research literature. Spine. 2007;32:2630-2637.
Jones GT, Macfarlane GJ. Epidemiology of low back pain in children and adolescents. Arch Dis Child. 2005;90:312-316.
Macias BR, Murthy G, Chambers H, et al. Asymetric loads and pain associated with backpack carrying by children. J Pediatr Orthop. 2008;28:512-517.
Mohseni-Bandpei MA, Bagheri-Nesami M, Shayesteh-Azar M. Nonspecific low back pain in 5000 Iranian school age children. J Pediatr Ortho. 2007;27:126-129.
Pellise F, Balague F, Rajmil L, et al. Prevalence of low back pain and its effect on health-related quality of life in adolescents. Arch Pediatr Adolesc Med. 2009:65-71.
Savigny P, Watson P, Underwood M. Early management of persistent non-specific low back pain: summary of NICE guidelines. BMJ. 2009;338:1441-1442.
Watson KD, Papageorgiou AC, Jones GT, et al. Low back pain in schoolchildren: the role of the mechanical and psychosocial factors. Arch Dis Child. 2003;88:12-17.
671.6 Spondylolysis and Spondylolisthesis
Radiographic Evaluation
The initial evaluation of the lumbar region should include high-quality anteroposterior, lateral, and oblique radiographs. The pars is best visualized on the oblique radiographs, and a pars defect has been termed the Scotty dog sign. Standing PA and lateral radiographs are obtained if findings suggestive of scoliosis or hyperkyphosis are also present (Figs. 671-8 and 671-9). In patients with normal plain films, a bone scan with SPECT images can help to diagnose a spondylolysis during the early stages (stress reaction), before a fracture or an established pseudarthrosis develops. A CT scan with thin cuts can establish the presence of a pars defect or a pseudarthrosis. If the bone scan shows no increased uptake in the region, and a CT scan demonstrates a pars defect, then the potential for healing is felt to be limited. Although MRI is most commonly indicated in the presence of signs or symptoms of cauda equina or nerve root involvement, it has been used more and more during the diagnostic phase.
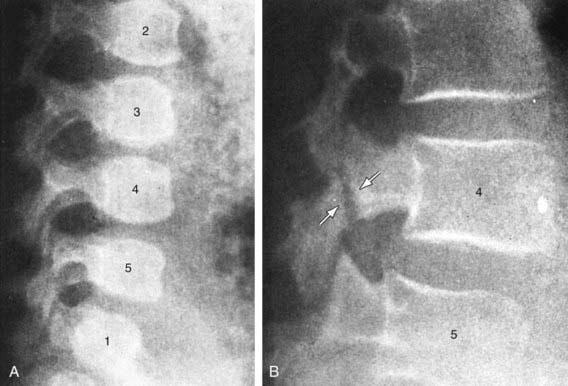
Figure 671-8 A, Normal spine at 9 mo of age. B, Spondylolysis in the L4 vertebra at 10 yr of age.
(From Silverman FN, Kuhn JP: Essentials of Caffrey’s pediatric x-ray diagnosis, Chicago, 1990, Year Book Medical Publishers, p 94.)
Grzegorzewski A, Kumar SJ. In situ posterolateral spine arthrodesis for grades III, IV, and V spondylolisthesis in children and adolescents. J Pediatr Orthop. 2000;20:506-511.
Helenius I, Remes V, Lamberg T, et al. Long-term health-related quality of life after surgery for idiopathic scoliosis and spondylolisthesis. J Bone Joint Surg Am. 2008;90:1231-1239.
Hu SS, Tribus CB, Diab M, et al. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90:656-671.
Klein G, Mehlman CT, McCarty M. Nonoperative treatment of spondylolysis and grade 1 spondylolisthesis in children and young adults: a meta-analysis of observational studies. J Pediatr Ortho. 2009;29:146-156.
Lenke LG, Bridwell KW. Evaluation and surgical treatment of high-grade isthmic dysplastic spondylolisthesis. Instr Course Lect. 2003;52:525-532.
Remes V, Lamberg T, Tervahartiala P, et al. Long-term outcome after posterolateral, anterior, and circumferential fusion for high-grade isthmic spondylolisthesis in children and adolescents: magnetic resonance imaging findings after average 17 year followup. Spine. 2006;31:2491-2499.
Sairyo K, Sakai T, Yasui N. Conservative treatment of lumbar spondylolysis in childhood and adolescence: the radiological signs which predict healing. J Bone Joint Surg Br. 2009;91:206-209.
671.7 Disk Space Infection
Both diskitis and vertebral osteomyelitis may be considered as age-dependent variations of infectious spondylitis. Diskitis is generally seen in children <5 yr of age, and vertebral osteomyelitis occurs in older children and adolescents. This spectrum may be explained on the basis of anatomy; the vertebral column in infants and younger children has vascular channels that communicate between the vertebral end plate and the vascular disk space, allowing organisms to seed the disk space (Table 671-3). Once these channels have closed, the infection remains in the vertebra.
Table 671-3 SPECTRUM OF NONTUBERCULOUS INFECTION OF THE SPINE
| SIGNS, SYMPTOMS, AND DEMOGRAPHICS | DISKITIS | VERTEBRAL OSTEOMYELITIS |
|---|---|---|
| Most common age | Younger than 7 yr Peak at 3 yr |
Older than 8 yr |
| Symptoms | Limp, back pain Refusal to walk |
Same as for diskitis |
| Location of lesion | Lumbar | Anywhere along spine |
| Febrile | Less likely (28%) | More likely (79%) |
| Laboratory values (complete blood Count, sedimentation rate) | Nonspecific elevation | Nonspecific elevation |
| Plain radiograph | Early: normal >20 days: disk space abnormal |
Early: normal 7-20 days: disk space and vertebrae abnormal |
| Magnetic resonance imaging | Localizes lesion | Localizes lesion Defined soft tissue involvement |
| Blood culture | Often negative | Often positive |
| Antibiotic therapy | Controversial | Yes |
From Slovis TR, editor: Caffey’s pediatric diagnostic imaging, ed 11, vol 1, Philadelphia, 2008, Elsevier.
The available evidence suggests that diskitis is a low-grade bacterial infection rather than an inflammatory process. Cultures of either the blood or disk space are positive in only 50-60% of patients, and Staphylococcus aureus (Chapter 174) is the most common organism isolated. Cultures are more likely to be positive if the symptoms have been present for <6 wk. Other organisms include Kingella kingae (Chapter 676), group A streptococcus (Chapter 176), and Escherichia coli (Chapter 192).
Clinical Manifestations
A high index of suspicion is required to establish the diagnosis of diskitis, especially in younger patients. The differential includes vertebral osteomyelitis (see Table 671-3). In addition to back pain and/or fever, patients can experience malaise, and toddlers can develop a limp or refuse to walk or sit. Spinal motion is voluntarily reduced to alleviate pain, and paraspinal muscle spasm is common. Flexion of the spine compresses the anterior elements of the spine and should increase any discomfort. This may be tested by asking the child to pick up an object from the ground. There may a loss of the normal lumbar lordosis. Neurologic manifestations are rare. Patients may be afebrile, and although a complete blood count might remain normal, the erythrocyte sedimentation rate and the C-reactive protein are usually elevated. Older children might have fever and abdominal pain.
Brown R, Hussain M, McHugh K, et al. Discitis in young children. J Bone Joint Surg Br. 2001;83:106-211.
Early S, Kay R, Tolo V. Childhood diskitis. J Am Acad Orthop Surg. 2003;11:413-420.
Fernandez M, Carroll CL, Baker CJ. Discitis and vertebral osteomyelitis in children: An 18-year review. Pediatrics. 2000;105:1299-1304.
Garron E, Veihweger E, Launay F, et al. Nontuberculous spondylodiscitis in children. J Pediatr Orthop. 2002;22:321-328.
Jansen BR, Hart W, Schreuder O. Discitis in childhood. 12-35-year follow-up of 35 patients. Acta Orthop Scand. 1993;64:33-36.
Kayser R, Mahlfeld K, Greulich M, et al. Spondylodiscitis in childhood: results of a long-term study. Spine. 2005;30:318-323.
Nussinovitch M, Sokolover N, Volovitz B, et al. Neurologic abnormalities in children presenting with diskitis. Arch Pediatr Adolesc Med. 2002;156:1052-1054.
Wenger DR, Bobechko WP, Gilday DL. The spectrum of intervertebral disc-space infection in children. J Bone Joint Surg Am. 1978;60:100-108.
Zimmerli W. Vertebral osteomyelitis. N Engl J Med. 2010;362:1022-1028.
671.8 Intervertebral Disk Herniation and Slipped Vertebral Apophysis
Chang CH, Lee ZL, Chen WJ, et al. Clinical significance of ring apophysis fracture in adolescent lumbar disc herniation. Spine. 2008;33:1750-1754.
Fairbank J. Prolapsed intervertebral disc. BMJ. 2008;336:1317-1318.
Parisini P, DiSilvestre M, Greggi T, et al. Lumbar disc excision in children and adolescents. Spine. 2001;26:1997-2000.
Shirado O, Yamazaki Y, Takeda N, et al. Lumbar disc herniation associated with separation of the ring apophysis: is removal of the detached apophysis mandatory to achieve satisfactory results? Clin Orthop Rel Res. 2005;431:120-128.
Smorgick Y, Floman Y, Millgram MA, et al. Mid- to long-term outcome of disc excision in adolescent disc herniation. Spine J. 2006;6:380-384.
671.9 Tumors
David A. Spiegel and John P. Dormans
Back pain may be the most common presenting complaint in children who have a tumor involving the vertebral column or the spinal cord. Other associated symptoms can include weakness of the lower extremities, scoliosis, and loss of bowel or bladder function. The majority of tumors are benign (Chapter 495). Lesions that may be observed in the anterior elements of the spine include aneurysmal bone cyst, eosinophilic granuloma, leukemia, and lymphoma; common tumors involving the posterior elements include osteoid osteoma and osteoblastoma. Malignant tumors involving the vertebral column may be osseous (osteosarcoma or Ewing sarcoma) or rarely are due to metastatic disease. Lesions in the soft tissues surrounding the spine are most commonly neurogenic, involving the spinal cord and sympathetic nerves (ganglioneuroma, ganglioneuroblastoma, neuroblastoma). In addition to high-quality plain radiographs, modalities including a bone scan (localization, look for other lesions), MRI (soft-tissue extension, neurologic compression) and CT (excellent bony detail) are performed in most cases before making a treatment plan. A biopsy is usually required to establish the diagnosis, and the treatment of tumors of the spinal column can require a multidisciplinary approach and should ideally be done in centers with experience in managing these lesions.