49 Therapeutic Exercises
Therapeutic exercises or exercise therapy is a major component in the management of various disorders. It can be defined as any prescribed and supervised exercise program, in which, during therapy sessions, the patients are required to carry out repeated voluntary dynamic movements or static muscle contractions, either whole body or region specific and either with or without external loading with the aim of relieving symptoms or improving function, by controlling inflammation, when present, restoring range of motion (ROM), restoring and/or improving muscular strength, power and endurance, and training to return to daily and recreational activities.1–4
Convened in 1999, the Philadelphia Panel, composed of clinical experts in the fields of medicine, research, and physical therapy set out to provide a structured and rigorous set of evidence-based guidelines for the conservative (nonsurgical) management of conditions associated with low back, knee, neck, or shoulder pain. A five-step process was established to put together these guidelines: defining rehabilitation interventions most frequently used in the care of low back, knee, neck, and shoulder pain, collecting the evidence, synthesizing the results, making recommendations based on the research, and grading the strength of the recommendations.5
The panel gathered evidence from randomized clinical trials and observational studies; the data were synthesized, and the relative clinical benefit between treatment and control groups was calculated for each condition for each intervention. The studies were also graded according to type and clinical importance of the findings. The grading scheme is summarized in Table 49-1. The panel deemed a 15% or greater improvement between treatment and control groups to be clinically important. In addition, the panel circulated feedback survey questionnaires to healthcare practitioners to verify their applicability and ease of use in clinical settings. Interventions with a grade of A or B were to be included in the guidelines.5
Table 49-1 Details of the Philadelphia Panel Classification System
| Grade | Clinical Importance | Study design type |
|---|---|---|
| A | 15% | RCT (single or meta-analysis) |
| B | 15% | CCT or observational study (single or meta-analysis) |
| C | 15% | RCT or CCT or observational (single or meta-analysis) |
| ID | NA | Insufficient or no data |
CCT, controlled clinical trial; NA, not applicable; RCT, randomized, controlled trial
From Harris GR, Susman JL: Managing musculoskeletal complaints with rehabilitation therapy: Summary of the Philadelphia Panel evidence-based clinical practice guidelines on musculoskeletal rehabilitation interventions. J Family Pract 51:1-7, 2002.
Briefly, the panel gave Grade A recommendation on the efficacy of therapeutic exercises, including stretching, strengthening, and mobility exercises for the treatment of subacute, chronic, postsurgery back pain, osteoarthritis of the knee, and chronic neck pain. Grade A recommendation means the intervention resulted in clinically significant improvement in pain and function. However, there are insufficient data on the benefit of therapeutic exercises for shoulder pain.5
These recommendations were made based on the available evidence at the time. The Philadelphia Panel also noted in its recommendation, many problems with the body of evidence in the medical literature—the main concern being the lack of standardization of outcome measurements used in different studies. Also noted was the inherent difficulty of studying rehabilitation interventions, where effectiveness could be compromised by psychosocial, physical, and occupational factors, as well as improbability of blinding either the therapist or the patient to the interventions.5
To address these issues, the panel recommends that future studies develop standards of measurement that are valid, reliable, and sensitive to changes in outcome; further, studies must specifically clarify the type and manner of intervention, intervention intensity and duration, and progression of the intervention according to patient-specific outcomes. Studies need to fully randomize large patient groups to minimize selection bias. Overall, the panel stressed the need for further large studies on rehabilitation interventions with the increased use of therapeutic exercises and other physical therapy interventions for the management of low back pain, knee pain, neck pain, and shoulder pain.5
Smidt and colleagues1 summarized and assessed available evidence on the effectiveness of exercise therapy for patients with disorders of the musculoskeletal and other systems. In their assessment of 98 reviews, they concluded that exercise therapy is effective for a wide range of chronic disorders. In particular, they found exercise therapy is effective for patients with knee osteoarthritis, subacute and chronic low back pain, cystic fibrosis, chronic obstructive pulmonary disease (COPD), and intermittent claudication. They also found indications that exercise therapy is effective for patients with ankylosing spondylitis, hip osteoarthritis, and Parkinson disease, and also for patients who have had stroke. They could not find sufficient evidence to support or refute effectiveness of therapeutic exercises for patients with neck pain, shoulder pain, repetition strain injury (RSI), rheumatoid arthritis, asthma, and bronchiectasis.
However, there is insufficient evidence to support or refute the effectiveness of specific types of therapeutic exercises for all disorders, and there is little or no research on how short-term effectiveness of the exercise therapies can be maintained long term. Conversely, they found no evidence that exercise therapy is harmful or that it provoked harmful side effects. They suggested that is could be due to the inadequate reporting of side effects in randomized controlled trials.1
In 2007, Taylor and colleagues,2 whose review included results from the Philadelphia Panel, Smidt and colleagues and 36 other studies found strong evidence that therapeutic exercises can benefit people across broad areas of physical therapy practice.2
Reviews published in the years of 2002 to 2005 that were assessed by Taylor and colleagues2 showed that exercise interventions that led to significant improvements were varied and diverse, but all the effective exercise programs tended to be intense. These results were found in people with musculoskeletal disorders (e.g., people with chronic back pain and people who have had lumbar disc surgery). Similarly, people with multiple sclerosis, coronary heart disease, and COPD, who participated in programs four to five times a week at relatively high intensity, showed significant improvements in their muscle strength and mobility for those with multiple sclerosis and for patients with heart disease or COPD, improved exercise capacity and less shortness of breath. There was no evidence that exercise of relative intensity caused exacerbation of symptoms such as increased fatigue in patients with multiple sclerosis, or disc reherniation in patients who have had lumbar disc surgery.2
Another common theme that emerged was that results were more favorable when therapeutic exercise was compared to a no treatment control group. However, like Smidt and colleagues, Taylor and coworkers did not find sufficient evidence that one type of exercise was superior to another. This finding was common in many areas of practice.1,2
However, Taylor and colleagues noted that a particularly useful finding for clinical practitioners, was that therapeutic exercise may be more effective when it is individualized or targeted. Studies showed that individualized exercises were more effective than standardized exercise programs wherein every patient is given the same regimen.2 Effective individualized exercise programs begin with sequential steps to help identify the needs of the patient—assess the patient, interpret the assessment, establish goals, develop and supervise the treatment plan, and reassess the progress of the program (see Table 49-2).3 When assessment has been completed and documented, the individualized exercise program begins immediately.
Table 49-2 The Rehabilitation Process
| 1. Record the patient’s subjective information—in particular the primary complaint; document objective data to establish measurable baseline information. |
| 2. Organize and interpret the assessment to identify primary deficits and weaknesses. |
| 3. Establish realistic short- and long-term goals, taking into consideration patient’s fitness and functional level prior to injury, severity of injury or disability, and patient’s motivation. |
| 4. Develop a treatment plan that incorporates rehabilitation interventions—therapeutic exercise programs and modalities that evidence has shown to be effective in the treatment of the patient’s injury or disability. |
| 5. Use periodic measurements to assess progress, or the lack thereof, refining and/or modifying the treatment plan when needed. |
From Anderson MK, Hall SJ, Martin M: Sports Injury Management, 2nd ed. Philadelphia, Lippincott Williams & Wilkins, 2000.
The Neck
The Evidence
Neck pain accounts for billions of dollars each year in economic loss due to lost workdays, treatment and disability, with about 70% of the population experiencing an episode of neck pain at some point in their lives. It is the second largest cause of time off from work, after low back pain. Acute neck pain is usually a result of injury or accident, most often road vehicle accidents associated with whiplash. Prognostic studies have suggested that chronic neck pain is associated with repetitive working conditions, and also with depression. Patient with neck pain are categorized into three widely accepted classifications: mechanical neck disorders (MND), including whiplash associated disorders, WAD), myofascial neck pain, and degenerative changes including osteoarthritis and cervical spondylosis; neck disorder with headache (NDH); and neck disorders with radicular findings (NDR). For these conditions, one of the most commonly used interventions is therapeutic exercise.6–8
Strengthening exercises are any exercise done by the patient that includes resistance, such as isometric, isokinetic, or isotonic exercise. It could include strength training with machines, free weights, or low-load endurance exercises to train muscle control.6,8
Proprioception is a specialized variation of the sensory modality of touch that encompasses the sensation of joint movement. Proprioceptive exercises are performed with the goal of reducing the proprioceptive deficits.3
Gaining popularity among clinicians in the treatment of neck pain are spinal stabilization exercises. Examples of cervicothoracic stabilization exercises are shoulder shrugs, shoulder circles and squares, and scapular retraction.4
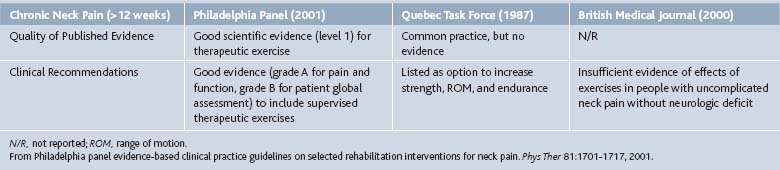
Rehabilitation specialists use concomitant treatment interventions within the same treatment session for a particular patient, such as mechanical traction, transcutaneous electrical nerve stimulation (TENS), and thermal therapy. Certain interventions, such as application of ultrasound and manual therapy are used for pain relief in the acute stage or as a treatment preparation before the main intervention.6 Table 49-3 outlines the strength of the evidence on the use of therapeutic exercises for acute neck pain.
Table 49-3 Strength of Published Evidence and Clinical Recommendations of Previous Evidence-Based Clinical Practice Guidelines on the Use of Therapeutic Exercises for Acute Neck Pain
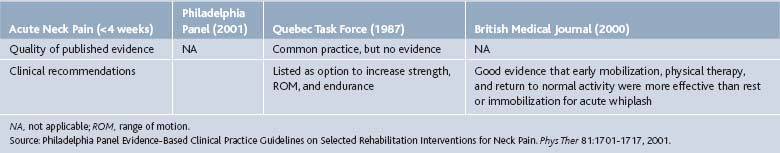
In its report of findings, the Philadelphia Panel found good scientific evidence (level I), with clinically important benefit on pain and function with supervised, isometric, or slow neck movement exercises. Based on the evidence, the panel recommends the inclusion of supervised exercise programs (including proprioceptive and traditional exercises) for the management of chronic neck pain. It was pointed out that the type of exercise, intensity, and progression needs to be clarified according to patient-specific classification of physical dysfunction, needs, treatment goals, and outcomes. However, the panel’s review did not include studies on the efficacy of therapeutic exercises for acute or subacute conditions (Table 49-4).6
Table 49-4 Strength of Published Evidence and Clinical Recommendations of Previous Evidence-Based Clinical Practice Guidelines on the Use of Therapeutic Exercises for Chronic Neck Pain
In another review, Kay and coworkers found limited evidence of benefit on active ROM exercises in whiplash-associated injuries. In studies assessing the use of strengthening exercises for subacute and chronic neck pain, two reviews found moderate evidence of benefit, with improvements in pain and function noted for patients with chronic neck with headache in the short and long term. The evidence on the use of strengthening exercises on patients with mechanical neck pain is unclear. The authors attributed this finding to several factors, including the location of focus of strengthening exercises and the types of strengthening exercises used in the studies that assessed the efficacy of strengthening exercises. However, Kay and colleagues did find moderate evidence of benefit on pain in chronic MND and NDH in the short term and long term when the stretching and strengthening program focused on the cervical or cervical and shoulder/thoracic region. In addition, a program of eye-fixation/proprioception exercises embedded in a complete exercise regimen shows moderate evidence of benefit for pain, function and global perceived effects for patients with chronic MND in the short term and on pain and function on patients with acute or subacute WAD with or without headache in the long term.7,8
Kay and coworkers also found strong evidence of benefit in a multimodal care approach of exercise combined with mobilizations or manipulations for subacute and chronic MND with or without headache in the short and long term. However, in the entire review, no explanation was given for this finding. The report did not specify if the benefit was for pain, function, or global perceived effect. Moreover, in the section on types of intervention that were included in this review, Kay and colleagues stated that studies were included if they used one or more type of exercise therapy, such as specific neck exercises, shoulder exercises, active exercise, stretching, strengthening and other types of exercise. The authors did not state that a multimodal approach that includes mobilization or manipulation would also be considered in the review.7
However, Gross and associates8 who reviewed conservative management of mechanical neck disorders, including mobilization and manipulation, did report strong evidence of benefit on pain, function, and perceived global effect with the use of the multimodal approach on patients with subacute and chronic MND, NDR, and NDH. Moffet and McLean4 found limited evidence for the use of any one specific exercise program and in evidence-based practice guidelines, no one specific program is recommended. Although the use of spinal stabilization exercises is gaining popularity in the treatment of neck pain, there is minimal evidence regarding its efficacy.4,7,8
Guidelines for Stretching to Improve Flexibility
Selected Exercises
The Back
Low back pain is extremely common to all the industrial world. Sixty to 90% of the adult population is at risk of developing LBP at some point in their lifetime. Of those who develop acute LBP, 30% develop chronic LBP. Its high prevalence as well as its impact on functional ability usually leads to personal and socioeconomic consequences. It is the largest cause of workers’ compensation in the United States and Canada.9–12
The severity of LBP can range from an acute disabling problem to a chronic mild discomfort. Usually affected are joints, ligaments, discs, and capsule. Any damage to these primary structures may affect the nerve roots or spinal cord, and may lead to secondary muscle spasm, tightness, or weakness. As a result of direct injury to the back muscles, a pain-spasm cycle could also occur. Many nonpharmacologic therapies are available for the treatment of LBP, and in many cases, patients were referred to physical therapy for exercise therapy and other interventions.9–12
Because of the complexity and the number of variables involved, low back disorder and/or disability can be very difficult to assess accurately and treat successfully. Using the most widely accepted method of classification for LBP, where patients are categorized into one of three groups—serious spinal pathology, neurologic involvement, or nonspecific LBP, would help guide clinicians in the accurate assessment of LBP and thus, create and implement an effective treatment plan. Moreover, the clinician must watch for “red flags” during assessment, so if need be, a prompt referral to a specialist for further investigation can be arranged (Table 49-5).4
Table 49-5 Red Flags to Look for When Assessing Patients with Low Back Pain
| Age of onset <20 or >55 years |
| Violent trauma |
| Constant progressive, nonmechanical pain (no relief with bed rest) |
| Thoracic pain |
| Past medical history of malignant tumor |
| Prolonged use of corticosteroids |
| Drug abuse, immune deficiency disorders, human immunodeficiency virus (HIV) |
| Systemically unwell |
| Unexplained weight loss |
| Widespread neurologic conditions (including cauda equina syndrome) |
| Structural deformity |
| Fever |
From Moffet J, McLean S: The role of physiotherapy in the management of non-specific back pain and neck pain. Rheumatology 45:371-378, 2006.
Nonspecific LBP is defined as pain between the gluteal fold and the uppermost lumbar vertebrae, including patients with postsurgery back pain. Because prognosis is typically dependent on the disease duration, nonspecific LBP is also classified into three widely accepted categories, acute (<4 weeks’ duration), subacute (4 to 12 weeks’ duration), and chronic (>12 weeks’ duration).11
Once red flags are ruled out and the patient assessment has been completed, the clinician must decide from among the various rehabilitation interventions that are available in the treatment of patients with nonspecific LBP. Among the most widely used intervention to treat nonspecific LBP is exercise therapy or therapeutic exercises. Exercise therapy encompasses a diverse mix of interventions that vary in type, intensity, frequency, and duration of exercise and the setting in which it is provided. Some of the more popular methods used are contradictory in theory and practice (Williams’ flexion and McKenzie’s extension exercises) and some have limited evidence in the literature.4,10,11
The Philadelphia Panel reviewed randomized controlled trials, nonrandomized controlled clinical trials or case control or cohort studies that evaluated therapeutic exercises and other rehab interventions in patients with nonspecific LBP. Outcomes weighed were functional status, pain, ability to work, patient global improvement, patient satisfaction, and quality of life.11
In its report, the panel found level I evidence that showed no clinically important benefit of stretching (including McKenzie) or strengthening exercises. The panel recommended there is poor evidence to include or exclude stretching or strengthening exercises alone as an intervention for acute LBP. This finding is consistent with other evidence-based guidelines, like the Compendium of the Best Available Evidence for Effective Health and the Agency for Health Care Policy and Research. However, the Quebec Task Force does recommend the prescription of general exercises as an option to increase strength, ROM, and endurance. In patients with subacute LBP, the Philadelphia Panel found good evidence to include extension, flexion and strengthening exercises as interventions (grade A for pain, function, and patient global improvement). For chronic LBP patients, the panel recommends stretching, strengthening, and mobility exercises. It found good scientific evidence (level I) that therapeutic exercises, in particular stretching and strengthening exercises, provided clinically important benefit for pain relief and functional status. In patients with postsurgery back pain, the panel found good evidence for strengthening and back extension exercises, with clinically significant improvements on pain and function.11
In a review commissioned by the American Pain Society and the American College of Physicians on nonpharmacologic therapies for LBP in adults, exercise therapy was found to be superior to usual care or no care for patients with acute LBP. There were no differences between exercise therapy and placebo or usual care for subacute LBP. For patients with chronic LBP, exercise therapy was associated with statistically significant but small effects on pain and function compared with other noninvasive interventions.12
In a review that considered 61 randomized, controlled trials to evaluate the effectiveness of exercise therapy in adults with nonspecific acute, subacute, and chronic LBP versus no treatment and other conservative treatments, analysis revealed no significant difference in short-term pain relief between exercise therapy and no treatment for acute LBP populations. Similarly, exercise therapy did not have a statistically significant positive effect on functional outcomes. In subacute LBP populations, evidence to support or refute the effectiveness of exercise therapy in reducing pain and improving function was deemed insufficient. However, it was noted that some evidence suggests that a graded-activity exercise program has some benefit in occupational settings. In chronic LBP patients, evidence strongly suggest that exercise is at least as effective as other conservative treatments, with statistically significant improvement in function and pain levels.13
In systematic reviews that assessed exercise therapy in general, and in those that studied specific types of exercise therapy and their efficacy in the treatment of LBP, findings are in agreement with the Philadelphia Panel, which found extension, strengthening, and flexion exercises effective for subacute and chronic LBP. A systematic review of McKenzie therapy concludes that the method results in greater decrease in pain and disability in the short-term than do other standard therapies. However, it was noted that there is insufficient data on long-term outcomes.14 In a study that compared the effects of spinal flexion and extension exercises on low-back pain severity and spinal mobility in patients with chronic LBP, it was reported that both the spinal flexion and spinal extension exercises provided significant reduction in LBP severity, with no statistically significant difference between treatment groups. In its conclusion, it was noted that both types of exercises can be used to reduce pain and increase spinal mobility.10
Alternatively, the efficacy of stabilization exercises alone or with other types of therapeutic exercises and rehab interventions in the treatment of nonspecific LBP is difficult to establish. A randomized controlled trial that evaluated the effect of stabilization exercises in reducing pain and disability, compared two patient groups, one received modalities, stretching and strengthening exercise, whereas the experimental group received stabilization exercises. The results revealed no statistically significant differences in reduction of pain intensity or increase of physical performance between both groups; however, there was a statistically significant difference between groups in the disability score in favor of the experimental group. However, the effect size was not reported. It must be noted that the sample size of the study is small (control, n = 20 and experimental, n = 20).15
An RCT studied the effectiveness of the Godelive Denys-Struft (GDS) method, which is based on the combination of individual manual therapy sessions and group sessions in which spinal stabilization exercises are performed along with exercises that work other muscles believed to help promote spinal stabilization, such as pelvic floor or diaphragm muscles. It was reported that at the end of the treatment sessions, the experimental group (GDS method) and the control group (conventional physiotherapy protocol) showed improvements in terms of three outcomes studied—pain, function, and quality of life. It also revealed that at follow-up 6 months after treatment, the control group had almost the same pain level as before treatment and also lost half of the improvements made in functional ability and quality of life. In its conclusion, it noted that the GDS method lead to greater improvements in the midterm in patient-perceived pain, functional ability, and quality of life than did the conventional treatment. However, it must be pointed out that the control group, defined as having received conventional physical therapy, actually received 15 sessions that consisted of the following: 14 40-minute sessions of TENS, plus 10 minutes of microwave treatment, and a single session in which patients were instructed on home exercises.16
Koumantakis and associates examined the usefulness of the addition of specific stabilization exercises to a general back and abdominal muscle exercise approach for patients with subacute or chronic nonspecific back pain by comparing a specific muscle stabilization-enhanced general exercise approach with a general exercise-only approach. They found that the general exercise program reduced disability in the short term to a greater extent than a stabilization-enhanced exercise approach in patients with recurrent nonspecific LBP. They concluded that stabilization exercises do not appear to provide additional benefit to patients with subacute or chronic LBP who have no clinical signs suggesting the presence of spinal instability.17
In summary, there is strong evidence on the usefulness of flexion, extension, and strengthening exercises in reducing pain and improving function in patients with subacute and chronic back pain. Extension and strengthening exercises are effective on patients with postsurgery back pain. However, there is limited evidence on the usefulness of therapeutic exercises, in general, and specific types of exercises for patients with acute LBP (Tables 49-6 to 49-9). Additionally, the growing popularity of stabilization exercises by itself or in combination with other types of interventions in clinical practices is not supported by evidence in the literature. More methodologically-sound randomized controlled trials are needed on the use of stabilization exercise for patients with nonspecific LBP.
Table 49-6 Strength of Published Evidence and Clinical Recommendations of Previous Evidence-Based Clinical Practice Guidelines on the Use of Therapeutic Exercises for Acute Back Pain
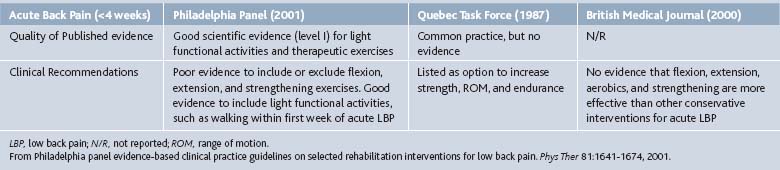
Table 49-7 Strength of Published Evidence and Clinical Recommendations of Previous Evidence-Based Clinical Practice Guidelines on the Use of Therapeutic Exercises for Subacute Low Back Pain
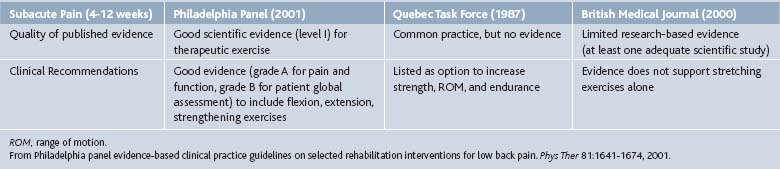
Table 49-8 Strength of Published Evidence and Clinical Recommendations of Previous Evidence-Based Clinical Practice Guidelines on the Use of Therapeutic Exercises for Chronic Back Pain
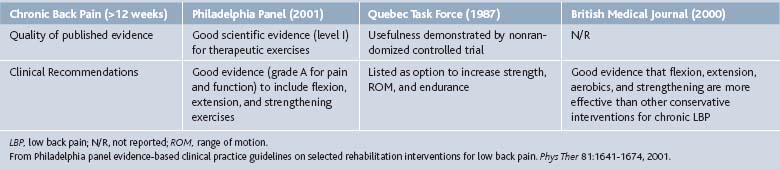
Table 49-9 Strength of Published Evidence and Clinical Recommendations of Previous Evidence-Based Clinical Practice Guidelines on the Use of Therapeutic Exercises for Postsurgery LBP (4-12 weeks)

Selected Exercises
Assisted Hamstring Stretching (Fig. 49-7)
Hamstring Curls (Figs. 49-8 and 49-9)
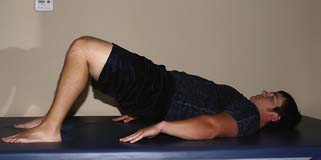
Resist Lumbar Bridging (Fig. 49-16)
Lumbar Bridging Bilateral on Ball (Figs. 49-17 and 49-18)
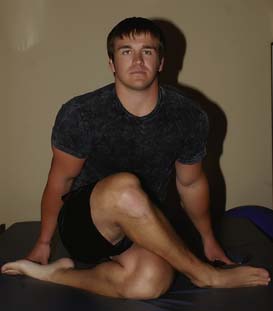
Piriformis Stretching—Supine (Fig. 49-20)
Piriformis Stretching—Long Sitting (Fig. 49-21)
Piriformis Self-Stretching (Fig. 49-22)
Posterior Hip Capsule and Piriformis Stretching (Fig. 49-23 to 49–25).
Iliopsoas Stretching in Supine Position(Fig. 49-26).
Self-Stretches
Rectus Femoris and Quadriceps Stretching (Figs. 49-29 to 49-31)
Stretch Lumbar with Rotation (Fig. 49-32)
Erector Spinae Assisted Stretching (Fig. 49-33)
AROM Lumbar Extension Prone High Level (Fig. 49-34)
The Knee
Chronic knee pain is one of the most common reasons for visits to a family practitioner. Acute knee pain usually follows injury or surgery. Chronic knee pain can be related to a disease such as osteoarthritis or associated with overuse or untreated injuries to muscles, ligaments, or tendons. Several etiologies of knee pain exist—chondromalacia patellae (patellofemoral pain syndrome), postsurgical conditions, and osteoarthritis.18 Osteoarthritis (OA) is the most common form of arthritis in Western populations. It primarily affects the articular cartilage and subchondral bone of a synovial joint and results in joint failure. Radiographic features are the formation of osteophytes at the joint margins, joint space narrowing, subchondral sclerosis, subchondral cyst formation, and chondrocalcinosis. It has been estimated that 40% to 80% of people with these radiographic changes will have symptomatic OA, especially in people older than 55 years. People with symptomatic OA of the knee complain of deep, aching pain. In early stages, pain is intermittent and mostly associated with joint use. As the disease progresses, the pain becomes more chronic and may also be present at rest and during the night, with the joint feeling stiff after a period of rest, resulting in pain and difficulty initiating movement. Patients may also experience crepitus or deep creaking sounds on movement and ROM often becomes limited, causing patients with the disease to experience increased difficulty and disability in walking, stair-climbing, and other daily functional activities. Physical disability arising from pain and loss of functional capacity reduces quality of life and increases the risk of further morbidity.19,20
Patellofemoral pain syndrome (PFPS) is a common complaint in adolescents and young adults. The symptom most frequently reported is a diffused peripatellar (around the knee cap) and retropatellar (behind the knee cap) localized pain, typically provoked by ascending or descending stairs, squatting and sitting with flexed knees for prolonged periods of time. Other common symptoms are crepitus and giving-way. However, the cause of PFPS is complicated, with several factors implicated.21
The European League Against Rheumatism (EULAR), in its 2003 recommendations on the management of knee osteoarthritis recommended that the treatment of knee OA should be tailored according to: knee risk factors (obesity, adverse mechanical factors, physical activity), general risk factors (age, comorbid conditions, polypharmacy), level of pain intensity and disability, sign of inflammation (effusion), and location and degree of structural damage. EULAR also reported that the optimal management of knee OA requires a combination of nonpharmacologic and pharmacologic treatment modalities.19 Current nonpharmacologic treatments for OA of knee and patellofemoral pain syndrome, as well as for patients who underwent knee arthroplasty, include a variable number of sessions of physical therapy.18–21 The therapist will use specific evaluative tools to determine an optimal treatment plan. These tools include: patient medical history and lifestyle, including occupational and leisure activities; sensory evaluation to determine presence of any pain or sensory loss; assessment of ROM, both passive and active to determine malalignment, laxity or tightness; measuring circumference at the knee to assess the presence of edema and atrophy; assessing quadriceps control for indications of muscle strength, evaluating gait patterns, which may reveal reduced motor control and assessing functional activities.22 The therapists will use various rehab interventions during treatment, but a major component will be therapeutic exercises. The aim of therapeutic exercises is to improve functional status by increasing muscle strength, improving flexibility, and reducing pain.18 The application of specific types of exercises, intensity and duration will depend on the patient’s unique circumstances, the goals of the treatment program, and other major factors.18,22 These factors include quadriceps inhibition or activation failure, obesity, passive knee laxity, knee alignment, fear of physical activity, and self-efficacy. The literature suggests that the inability of therapeutic exercises to address some of these factors might place barriers on the patient’s ability to achieve maximum benefits from a rehabilitation program.18,19,20
Of major concern throughout the rehabilitative process of any knee problem is the maintenance or improvement of quadriceps control. The quadriceps, like most muscles, are composed of both tonic and phasic extrafusal muscle fibers. The tonic fibers have a low threshold to stimulation and do not easily fatigue; however, these fibers tend to atrophy after prolonged immobilization or inactivity, resulting in an inability of the quadriceps to sustain an isometric contraction in the shortened range. The initial focus of treatment in such cases is to enhance the isometric activity by facilitating a shortened held resisted contraction. In patients with knee osteoarthritis, who have reduced functional performance, therapeutic exercises are thought to compensate for the arthrogenic impairment in the quadriceps femoris muscle sensorimotor function, improve diminished proprioceptive acuity, and increase postural stability.18 In patients with PFPS, resisted movement through range may aggravate this condition, whereas increased control of the vastus medialis is usually indicated and can be promoted by resisted isometric contractions in the shortened range of knee extension.21,22 Patients who have undergone surgical repair may require prolonged immobilization. In these cases, rotational motions of the knee are not indicated during the first stages of treatment.22
Pain is another major concern during the initial treatments. Procedures are always performed within the patient’s pain tolerance to prevent further trauma to the tissues. An increase in pain is usually indicative of an increase in stress to the inert or contractile tissues. Extra caution must be taken during ROM and strengthening exercises to prevent trauma.22
The exercise procedures are divided into three stages: initial, middle, and advanced. Depending on each patient’s unique circumstances, the therapist may begin ROM exercises or quadriceps control exercises. Increasing movement into knee flexion is also a goal of treatment and is promoted following the increasing of range into extension and the enhancement of quadriceps control. At the middle stage, postsurgery patients will have achieved full passive motion into extension and knee flexion to at least 90 degrees. For nonsurgical patients, for example, those with PFPS or knee OA, treatment may begin at this stage. At this point, isometric control in shortened range of knee extension is emphasized for all patients, with focus on direct activation of the quadriceps with a progressive increase in the amount of resistance. These activities will increase quadriceps isometric control, further increase ROM and increase power, strength, and endurance of the quadriceps and hamstrings. During the advanced stage, the patient should have good strength of the quadriceps and hamstrings and little difficulty with terminal extension. Strengthening exercises also improve gait and attenuate knee pain in activities of daily living among patients with osteoarthritis. At this point, the goals are to promote normal functional ability, improve eccentric control of the quadriceps, and promote advanced stages of motor control.18,22
For patients with PFPS, a systematic review of studies on the efficacy of therapeutic exercises, found evidence that suggests that exercise is effective, but the pooled results of the relevant studies are not straightforward, with some studies suggesting that exercise therapy provides significant pain reduction, whereas one study contradicts this finding. Regarding the improvement in function, two studies found no improvement, whereas one low-quality RCT reported positive results.21 The Philadelphia Panel found that there are insufficient data to support or refute the efficacy of therapeutic exercises for patellofemoral pain syndrome.18 However, there is sufficient evidence to support the efficacy of closed and open kinetic chain exercises for pain reduction and improved function.21
For patients who received exercise therapy after knee surgery, there is some evidence of its usefulness in reducing pain and improving function. A systematic review of the effectiveness of exercise therapy after knee arthroplasty found sufficient evidence to support the efficacy of functional exercises for improved function. The pooled results of the studies considered in the review found small to moderate standardized effect size in improved function over 3 to 4 months postoperatively and improved ROM and quality of life over the same period. However, none of the benefits were seen 1 year after surgery. It was noted that improved function is an important outcome in clinical practice, possibly more important than ROM, which is affected by factors beyond the therapists’ control, such as prosthetic design, preoperative knee motion, and surgical technique.23 RCTs that compared other rehab interventions with exercise therapy found that the control groups (exercise group) exhibited the same positive results as the experimental groups.24,25 Beaupre and colleagues (2001) found that all three groups—the exercise group, the CPM group, and the slider board group exhibited improved ROM in knee flexion and extension, with no statistically significant difference among groups; similarly, in patient-reported outcomes all three groups reported improvement in terms of pain, stiffness, and function.24 Similarly, Denis and coworkers found that adding CPM devices to exercise therapy did not have any additional benefit on active ROM in knee flexion or on any of the other secondary outcomes measured (ROM in knee extension, patient-reported pain, stiffness, and function).25
Exercise therapy for patients with knee osteoarthritis has strong evidence in the literature to support its application. The Philadelphia Panel found level I evidence that showed clinically important benefit of strengthening exercises on knee osteoarthritis pain. Its recommendation states that there is good evidence to include strengthening, stretching, and functional exercises for pain and patient global assessment.18 Similarly, a review of therapeutic exercises for people with knee OA concluded that there is platinum level evidence on the effectiveness of land-based therapeutic exercises relative to patient-reported outcomes. In its report of findings, land-based therapeutic exercises demonstrated small, but significant, benefits in terms of knee pain and physical function.20 A large-scale review of physical therapy interventions found high-quality evidence that therapeutic exercises reduce pain and improve function in patients with knee OA. It found therapeutic exercises to be effective in reducing pain and improving function. It also found that aerobic exercises and other exercises that promoted weight loss improved disability in patients with weight issues.26
The literature has sufficient data on usefulness of therapeutic exercises in patients with chronic knee pain, in particular, knee osteoarthritis, where the RCTs are typically of high quality. More research is needed on efficacy of therapeutic exercises for patients with patellofemoral pain syndrome and postsurgery knee patients. However, the Philadelphia Panel and other authors noted that in all studies on knee disability, the types of exercises, intensity, and progression need to be clarified according to physical dysfunction, needs, treatment goals, and outcomes. Also recommended is the need for an enormous research effort on rehabilitation interventions for knee pain, for prospective RCTs to identify predictors of patient responsiveness to therapeutic exercises, for multi-armed placebo-controlled RCTs to identify the optimal types of exercise and dosage for each type of knee dysfunction.18,20
The Hip
The hip is the second most common large weight-bearing joint to be affected by osteoarthritis (OA), a chronic joint condition characterized by pain, disability, and impairment. The prevalence of hip OA ranges from 3% to 11% in Western populations more than 35 years of age. It is often associated with significant pain, disability, and impaired quality of life. Main treatment goals are improving function, relieving symptoms, and improving quality of life. The optimal management of hip OA requires a combination of nonpharmacologic and pharmacologic treatment modalities. Physical rehabilitation interventions, including therapeutic exercise, is recommended.27,28
Exercise therapy aims to improve the patients’ overall function and to help them meet the demands of daily living. Because exercise therapy can vary in content, dosage, and mode of delivery, the therapist must base decisions on clinical judgment.28 The EULAR taskforce recommends that the following factors should be considered: hip risk factors (obesity, adverse mechanical factors, physical activity, dysplasia); general risk factors (age, sex, comorbid conditions, comedication) level of pain intensity, disability, and handicap; location and degree of structure damage; and wishes and expectations of the patient. The taskforce reports that these clinical markers used to guide clinical decisions are based on expert opinion and standard clinical practice only because there are no appropriate clinical trials to support the recommendation.27
Several reviews have found evidence on the usefulness of exercise therapy in hip OA to be limited. Although literature search yielded many results, most of the existing reviews studied knee and hip OA. The EULAR report points out that although available treatments for hip osteoarthritis are similar to knee OA, there are certain differences because the effect size of a specific treatment might vary according to the site of the OA involvement, owing to differences in anatomy, biomechanics, risk factors for development and progression, and accessibility to local treatments.27
Despite the paucity of evidence, the EULAR taskforce still recommends the use of exercise therapy in the treatment of hip OA, citing clear face-validity and expert opinion, as well as strong evidence of the usefulness of therapeutic exercises in other types of OA.27 Roddy and coworkers reported that there is insufficient data to conclude that strengthening exercises could reduce pain and improve function in people with hip OA.29 Pisters and colleagues, who studied the long-term effectiveness of exercise therapy in patients with hip or knee OA, reported strong evidence for no long-term effect on pain and self-reported function. However, it did report that moderate evidence exists for the effectiveness of additional posttreatment booster sessions in terms of long-term observed physical function. It must be noted that in its report of findings, the authors did not make the distinction between knee or hip OA.30 An umbrella review of nonpharmacologic and nonsurgical interventions, reported that there is insufficient evidence to make conclusions about the effect of exercise therapy on pain, disability, or health status.28 Roddy and colleagues also reported that there is no evidence in the literature to suggest that individualized, patient-centered exercise therapy is any more effective than group sessions. However, it was noted that although evidence may not support the practice, because RCTs tend to recruit homogeneous populations to whom standardized interventions are delivered with little room for individualization, individualized, patient-centered exercise regimens still have clear face-validity and are recommended in clinical guidelines.29
The Shoulder
The prevalence of shoulder pain accompanied by disability is approximately 20% in the general population. Conditions causing shoulder pain are common and contribute substantially to the musculoskeletal morbidity of the community. The shoulder is frequently injured in sports, and prevalence and disability tend to increase in age, the peak prevalence occurring in the 56 to 60 year age group.31,32
Shoulder disorders often result in substantial disability. Moving the shoulder allows for hand placement, therefore compromised shoulder mobility significantly affects ability to perform tasks of daily living. Moreover, shoulder pain is known to affect one’s ability to sleep. People with shoulder pain tend to score significantly higher than normal values in standardized tests that measure physical, social and emotional function, and pain. Most patients diagnosed with shoulder pain are referred to physical therapy.32
Physical therapy encompasses a broad range of interventions. The aim is to relieve pain, promote healing, reduce muscle spasms, increase joint range and strengthen weakened muscles, and, ultimately, to prevent and treat functional impairment.31,32 However, the Philadelphia Panel found the data on therapeutic exercises for shoulder pain to be insufficient. A systematic review of physical therapy interventions conducted in 2003, reported that supervised exercise therapy demonstrated significant benefit in the short and long term. In its report of findings, it was not indicated if the benefits were in terms of pain and/or function.31,32
Existing reviews noted the urgent need for more RCTs to determine whether therapeutic exercises are effective at reducing pain and improving long-term patient-important outcomes. It was noted that existing RCTs studied populations with mixed diagnoses (rotator cuff disease, adhesive capsulitis, calcific tendonitis). Studies often compared various interventions with other interventions, instead of using placebo as control group.31,32 The state of current research and the paucity of evidence on the efficacy of therapeutic exercises in the treatment of shoulder pain offer significant clinical challenge to practitioners. A good clinician must be able to choose appropriate interventions to produce optimal treatment outcomes, and with no sufficient evidence in the literature, must rely on clinical experience and training to develop individualized, patient-centered exercise regimens.
1. Smidt N., de Vet H.C., Bouter L.M., et al. Effectiveness of exercise therapy: a best-evidence summary of systematic reviews. Aust J Physiother. 2005;51:71-85.
2. Taylor N.F., Dodd K.J., Shields N., Bruder A. Therapeutic exercise in physiotherapy practice is beneficial: a summary of systematic reviews 2002-2005. Aust J Physiother. 2007;53:7-16.
3. Anderson M.K., Hall S.J., Martin M. Sports Injury Management, 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2000.
4. Moffet J., McLean S. The role of physiotherapy in the management of non-specific back pain and neck pain. Rheumatology. 2006;45:371-378.
5. Harris G.R., Susman J.L. Managing musculoskeletal complaints with rehabilitation therapy: summary of the Philadelphia Panel evidence-based clinical practice guidelines on musculoskeletal rehabilitation interventions. J Fam Pract. 2002;51:1042-1046.
6. Philadelphia panel evidence-based clinical practice guidelines on selected rehabilitation interventions for neck pain. Phys Ther. 2001;81:1701-1717.
7. Kay T.M., Gross A., Goldsmith C.H., et al. Exercises for mechanical neck disorders. Cochrane Database of Syst Rev. (Issue 3):2005.
8. Gross A.R., Goldsmith C., Hoving J.L., et al. Conservative management of mechanical neck disorders: a systematic review. J Rheumatol. 2007;34:1083-1102.
9. Hayden J.A., van Tulder M.W., Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142:776-785.
10. Elnaggar I.M., Nordin M., Sheikhzadhe A., et al. Effects of spinal flexion and extension exercises on low-back pain and spinal mobility in chronic mechanical low-back pain patients. Spine. 1991;16:967-972.
11. Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for low back pain. Phys Ther. 2001;81:1641-1674.
12. Chou R., Huffman L.H. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147:492-504.
13. Hayden J.A., van Tulder M.W., Malmivaara A.V., Koes B.W. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142:765-775.
14. Clare H.A., Adams R., Maher C.G. A systematic review of efficacy of McKenzie therapy for spinal pain. Austr J Physiother. 2004;50:209-216.
15. Ali T.A. Stabilization exercises for patients with low back pain 54 2006. (The Cochrane Controlled Trials Register [CCTR/CENTRAL]). In The Cochrane Library. Oxford: Update Software; 2009. Issue 1, Updated quarterly
16. Dîaz Arribas M.J., Ramos Sånchez M., Pardo Hervås P., Løpez P., et al. Effectiveness of the physical therapy Godelive Denys-Struyf method for nonspecific low back pain: Primary care randomized control trial. Spine. 2009;34:1529-1538.
17. Koumantakis G.A., Watson P.J., Oldham J.A. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. 2005;82:209-225.
18. Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for knee pain. Phys Ther. 2001;81:1675-1700.
19. Jordan K.M., Arden N.K., Doherty M., et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62:1145-1155.
20. Fransen M., McConnell S. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2008. Issue 4. Art. No.: CD004376. DOI: 10.1002/14651858.CD004376.pub2
21. Heintjes E.M., Berger M., Bierma-Zeinstra S.M.A., et al. Exercise therapy for patellofemoral pain syndrome. Cochrane Database of Systematic Reviews. 2003. Issue 4. Art. No. CD003472. DOI: 10.1002/14651858.CD003472
22. Sullivan P.E., Markos P.D., Minor M.A. An Integrated Approach to Therapeutic Exercise. In Theory and Clinical Application. Reston, VA: Reston Pub. Co.; 1982.
23. Minns-Lowe C.J., Barker K.L., Dewey M., Sackley C.M. Effectiveness of physiotherapy exercise after knee arthroplasty for osteoarthritis: systematic review and meta-analysis of randomized controlled trials. BMJ. 2007:335. 812
24. Beaupré L.A., Davies D.M., Jones C.A., Cinats J.G. Exercise combined with continuous passive motion or slider board therapy compared with exercise only: a randomized controlled trial of patients following total knee arthroplasty. Phys Ther. 2001;81:1029-1037.
25. Denis M., Moffet H., Caron F., et al. Effectiveness of continuous passive motion and conventional physical therapy after total knee arthroplasty: a randomized clinical trial. Phys Ther. 2006;86:174-185.
26. Jamtvedt G., Dahm K.T., Christie A., et al. Physical therapy interventions for patients with osteoarthritis of the knee: an overview of systematic reviews. Phys Ther. 2008;88:123-136.
27. Zhang W., Doherty M., Arden N., et al. EULAR evidence-based recommendations for the management of hip osteoarthritis: report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2005;64:669-681.
28. Moe R.H., Haavardsholm E.A., Christie A., et al. Effectiveness of nonpharmacological and nonsurgical interventions for hip osteoarthritis: an umbrella review of high-quality systematic reviews. Phys Ther. 2007;87:1716-1727.
29. Roddy E., Zhang W., Doherty M., et al. Evidence-based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee—the MOVE consensus. Rheumatology. 2005;44:67-73.
30. Pisters M.F., Veenhof C., Meeteren N.L.U., et al. Long-term effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: A systematic review. Arthritis Rheum. 2007;57:1245-1253.
31. Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for shoulder pain. Phys Ther. 2001;81:1719-1730.
32. Green S., Buchbinder R., Hetrick S.E. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003. Issue 2. Art. No. CD004258. DOI: 10.1002/14651858