25 Suprascapular Nerve Block
Anatomy of the Suprascapular Nerve
The suprascapular nerve is a mixed motor and sensory peripheral nerve originating from the upper trunk of the brachial plexus, receiving contributions predominantly from C5 and C6 fibers with approximately 22% of individuals also receiving contributions from C4.1 The suprascapular nerve gives motor innervation to the supraspinatus and infraspinatus muscles. Additionally, the nerve gives sensory and proprioceptive innervation to the glenohumeral joint, acromioclavicular joint, subacromial bursa, and the scapula (Fig. 25-1). Although the suprascapular nerve receives afferents from up to 70% of the shoulder joint, it rarely carries cutaneous afferent fibers. Cadaveric studies have found that as many as 15% of individuals have a cutaneous branch of the suprascapular nerve supplying the proximal, lateral one-third of the arm.2,3
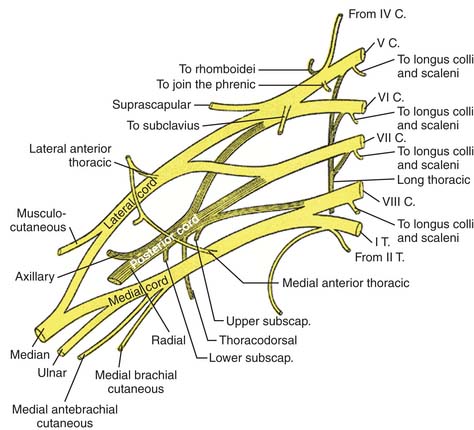
Figure 25-1 Brachial plexus.
(From Gray H: Anatomy of the Human Body. Philadelphia, Lea & Febiger, 1918).
After arising from the upper trunk of the brachial plexus, the suprascapular nerve courses through the posterior triangle of the neck, anterior to the trapezius muscle and posterior to the inferior belly of the omohyoid muscle (Fig. 25-2). The nerve then traverses through the suprascapular notch where it lies beneath the superior transverse scapular ligament and in close relation to the posterior border of the clavicle. Proximal to entering the suprascapular notch, the superior articular branch of the suprascapular nerve gives off sensory fibers to the coracoclavicular and coracohumeral ligaments, the acromioclavicular joint, and the subacromial bursa.3–6 Within the suprascapular notch, the suprascapular nerve gives rise to two motor nerves to the supraspinatus muscle.2 The nerve then passes through the notch and continues inferiorly, wrapping around the lateral margin of the scapular spine and through the spinoglenoid notch. Here, the suprascapular nerve sends a sensory branch to the posterior glenohumeral joint capsule. The nerve subsequently travels around the scapular spine, passing through a tunnel created by the spine of the scapula and spinoglenoid ligament (inferior transverse scapular ligament). The spinoglenoid ligament is a fibrous connective tissue band which originates from the lateral border of the scapular spine and inserts at the margin of the glenoid process.6 After passing through this space, the suprascapular nerve terminates by sending two to four motor branches to the infraspinatus muscle.
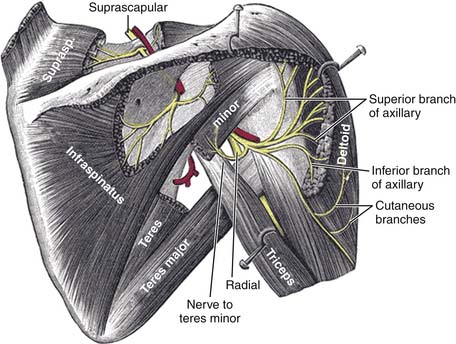
Figure 25-2 Course of suprascapular nerve on right side.
(From Gray, H: Anatomy of the Human Body. Philadelphia, Lea & Febiger, 1918).
Anatomic associations of the suprascapular nerve play an important role in source of injury. Proximally, the nerve’s close relation to the inferior border of the clavicle makes it potentially vulnerable to clavicular injuries. It is also hypothesized that anatomic variation in the shape of the suprascapular notch may predispose individuals to proximal suprascapular nerve entrapment. Cadaveric studies of adult scapulae have shown that the suprascapular notch can exist in six shapes. The U-shaped (48%) and V-shaped (3%) are most commonly associated with nerve entrapment.2,7 Additionally, morphologic deviations in the superior transverse scapular ligament, such as calcification and hypertrophy, are also associated with suprascapular nerve injury.2
The suprascapular nerve is prone to injury distally where it passes through the tunnel formed by the scapular spine and the spinoglenoid ligament. Adduction and internal rotation of the shoulder is thought to tense the spinoglenoid ligament and subsequently stretch the nerve.2,8 In cadaveric studies, the spinoglenoid ligament has been identified in variable prevalence (15% to 80% of individuals).2,9,10 Interestingly, the ligament has been shown to be present more frequently in males (87%) than in females (50%), representing the higher likelihood of volleyball shoulder in males.6
Pathophysiology
The most common location of injury to the suprascapular nerve is proximally at the suprascapular notch, and distally at the spinoglenoid notch. The mechanism of suprascapular nerve injury here is usually by repetitive overhead motions of the shoulder. In what is termed the sling effect, depression and retraction or hyperabduction of the shoulder causes the nerve to become apposed to the inferior margin of the superior transverse scapular ligament proximally or submitted to traction injury as it wraps around the scapular spine distally at the spinoglenoid notch.2 The sling effect underscores the importance of the scapula in overhead shoulder motions, such as throwing. These upper limb movements, causing scapular protraction and retraction, ultimately cause tension on the suprascapular nerve and sheer stress. Consequently, many suprascapular nerve injuries are in athletes using repetitive overhead motions that stress the shoulder.2
Alternative movements of the shoulder are also associated with distal suprascapular nerve injury. Abduction and external rotation causes the medial border of the infraspinatus tendon, inducing a compression injury at the spinoglenoid notch.2,11 Adduction or internal rotation of the upper limb is thought to cause traction of the suprascapular nerve at the spinoglenoid notch.2,12 Fast, repetitive, eccentric contraction of the infraspinatus muscle, in what is termed “volleyball shoulder”, causes injury to the suprascapular nerve at its terminal portion.13,14
Compression effects may also cause injury to the suprascapular nerve. Ganglion cysts are the most common source of mass effect and primarily arise secondary to trauma to the joint capsule (Fig. 25-3). Other masses, including sarcomas and bone cysts may cause a similar effect.2

Figure 25-3 Coronal T2-weighted magnetic resonance image of the right shoulder demonstrating a ganglion cyst (arrow).
(From Cummins CA, Messer TM, Nuber GW: Suprascapular nerve entrapment. J Bone Joint Surg Am. 2000;82[3]:415-424.)
Patients with suprascapular nerve injury are typically young male athletes between 25 and 35 years of age with usually insidious onset of dominant upper extremity pain. They present with dull, achy pain in the posterior aspect of the shoulder. Overhead motion of the extremity exacerbates these symptoms. Because the majority of the suprascapular nerve’s sensory fibers are located proximally, pain is more associated with injury to the proximal aspect of the nerve. Consequently, injury to the nerve distally at the spinoglenoid notch or volleyball shoulder causing isolated injury or atrophy to the infraspinatus are more likely to be insidious in onset and without any notable symptoms.13 Weakness may also manifest initially. However, many patients are asymptomatic and are incidentally found to have atrophy of the supraspinatus and infraspinatus muscles.2
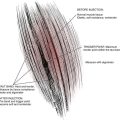
Physical examination of individuals with suprascapular nerve injury will show atrophy of the supraspinatus and infraspinatus muscles (Fig. 25-4). Patients with proximal lesions of the suprascapular nerve will present with tenderness to palpation between the clavicle and scapular spine. Distal suprascapular nerve lesions will manifest as tenderness to palpation at the spinoglenoid notch on physical examination. Patients may also have weakness in external rotation of the shoulder, a function of the infraspinatus and teres minor muscles. Also observed is a weakness in abduction, a function of the supraspinatus muscle.
Indications for Block
Suprascapular nerve blocks (Fig. 25-5) are indicated for neuropathy of the suprascapular nerve, pain from mass effects of malignancies and cysts, postoperative shoulder pain, or to assist with shoulder range of motion during rehabilitation of patients with adhesive capsulitis.15 Patients with inflammatory disease, including rheumatoid arthritis and spondyloarthropathies, will benefit from nerve blockade.16,17 Athletes with chronic shoulder pain from overuse injury may also benefit from suprascapular nerve block. Patients with severe osteoarthritis of the glenohumeral joint who are not candidates for total shoulder joint replacement and who do not benefit from intraarticular corticosteroid injections are candidates for suprascapular nerve blockade for pain relief. Additionally, injection of a local anesthetic into the suprascapular notch has been found by some authors to be helpful in diagnosing suprascapular nerve entrapment by exclusion.2
Techniques for Suprascapular Nerve Block
Suprascapular nerve blockade is accomplished by injecting local anesthetic solution around the suprascapular nerve at the suprascapular notch. The suprascapular notch is an ideal location for neural blockade, given the relative ease of accessibility for the operator. Additionally, at this level, the suprascapular nerve gives branches to the glenohumeral joint, the acromioclavicular joint, and the supraspinatus muscle.16
If done without fluoroscopy, the patient is placed in a sitting position with his or her back to the examiner and the hand of the affected side resting on the contralateral shoulder to help contour the shoulder and back in optimal position for a successful block. The procedure must be performed in a sterile manner and the skin must be cleansed with an antiseptic solution. The site of injection for nerve blockade is found by first identifying the spine of the scapula by palpation and drawing a line along the length of the scapular spine. The line should be in an oblique orientation, heading superiorly and laterally toward the acromion. At approximately the midpoint of this line, a second vertical line is drawn parallel to the vertebral spine. This line is intended to bisect the angle of the scapula superiorly and extend toward the tip of the scapula inferiorly. The upper outer quadrant formed by these two lines is further bisected with a third line. The injection site for suprascapular nerve blockade is approximately 2 cm along this third line.16,18,19 A subcutaneous wheal with lidocaine (Xylocaine) 1% solution is made to anesthetize the site of needle injection. A 22 gauge, 38 mm insulated block needle with a nerve stimulator is aligned parallel to the patient’s back at the point of injection. The needle is inserted through the skin toward the scapular spine. When contact with the spine is made, the block needle should be carefully directed anteriorly to enter into the suprascapular notch.19 A motor response by the supraspinatus and infraspinatus muscles to 0.3 to 0.5 mA and 0.1 msec confirms accurate needle position. When satisfactory needle position is obtained, the operator should always aspirate from the needle to ensure the needle is not in an intravascular space. Approximately 10 mL of 0.5% bupivacaine and 40 mg methylprednisolone or triamcinolone should be injected to fill the space around the nerve. The anesthetic agent should be injected slowly because rapid injection of anesthetic solution into this fixed space can cause trauma to the nerve.15,20 Because of the proximity of the suprascapular notch to the pleural cavity, pneumothorax may result if the block needle is placed too deep within the suprascapular notch.
Ultrasound guidance can also be used for suprascapular nerve blockade, either alone or with a combined nerve stimulator technique. The technique is similar to that described earlier. Perineural spread of local anesthetic will appear as a hypoechoic shadow on ultrasound. Figures 25-6 and 25-7 outline ultrasound-directed views of the suprascapular nerve during nerve blockade.
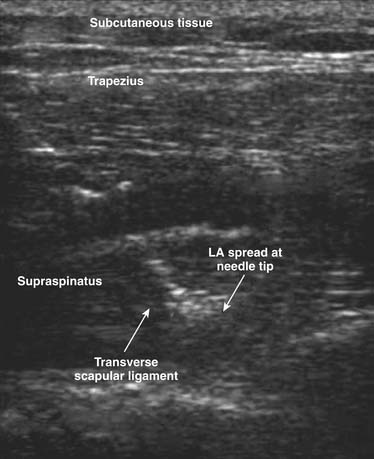
Figure 25-7 Real-time imaging of needle insertion for the ultrasound-guided suprascapular block
(From Harmon D, Hearty C: Ultrasound-guided suprascapular nerve block technique. Pain Physician. 10:743-746. 2007.)
For fluoroscopy-guided blocks, patients are placed in prone position with the fluoroscopy unit angled in a caudocranial direction. The suprascapular notch is first identified anterior to the spine of the scapula (Fig. 25-8). A subcutaneous wheal with lidocaine (Xylocaine) 1% solution is made to anesthetize the site of needle injection. A 25 gauge, 3.5 inch spinal needle is aligned parallel to the x-ray beam and positioned in the suprascapular notch, by first contacting the scapular spine and then by carefully directing the needle anteriorly to enter into the suprascapular notch.19 When satisfactory needle position is obtained, the operator should always aspirate from the needle to ensure it is not in an intravascular space, and 1 mL of nonionic contrast should be injected under continuous fluoroscopy to confirm spread along the suprascapular nerve and to rule out intravascular spread (Fig. 25-9). Approximately 10 mL of 0.5% bupivacaine and 40 mg methylprednisolone or triamcinolone should be injected to fill the contents of the suprascapular notch. Similar to the anatomic landmark approach, pneumothorax is a potential complication and the anesthetic agent should be injected slowly to prevent nerve trauma.
1. Lee H.Y., Chung I.H., Sir W.S., et al. Variations of the ventral rami of the brachial plexus. J Korean Med Sci. 1992;7:19-24.
2. Cummins C.A., Messer T.M., Nuber G.W. Suprascapular nerve entrapment. J Bone Joint Surg Am. 2000;82(3):415-424.
3. Ajmani M.L. The cutaneous branch of the human suprascapular nerve. J Anat. 1994;185:439-442.
4. Inouye Y. Conduction along the articular branch of the suprascapular nerve. Acta Neurol Scand. 1978;58:230-240.
5. Mestdagh H., Drizenko A., Ghestem P. Anatomical bases of suprascapular nerve syndrome. Ana Clin. 1981;3:67-71.
6. Lee B.C., Yegappan M., Thiagarajan P. Suprascapular nerve neuropathy secondary to spinoglenoid notch ganglion cyst: Case reports and review of literature. Ann Acad Med Singapore. 2007;36:1032-1035.
7. Rengachary S.S., Neff J.P., Singer P.A., Brackett C.E. Suprascapular entrapment neuropathy: A clinical, anatomical, and comparative study. Part 1: Clinical study. Neurosurgery. 1979;5:441-446.
8. Demirhan M., Imhoff A.B., Debski R.E., et al. The spinoglenoid ligament and its relationship to the suprascapular nerve. J Shoulder Elbow Surg. 1998;7:238-243.
9. Ticker J.B., Djurasovic M., Strauch R.J., et al. The incidence of ganglion cysts and other variations in anatomy along the course of the suprascapular nerve. J Shoulder Elbow Surg. 1998;7:472-478.
10. Cummins C.A., Anderson K., Bowen M., et al. Anatomy and histological characteristics of the spinoglenoid ligament. J Bone Joint Surg Am. 1998;80:1622-1625.
11. Sandow M.J., Ilic J. Suprascapular nerve rotator cuff compression syndrome in volleyball players. J Shoulder Elbow Surg. 1998;7(5):516-521.
12. Demirhan M., Imhoff A.B., Debski R.E., et al. The spinoglenoid ligament and its relationship to the suprascapular nerve. J Shoulder Elbow Surg. 1998;7:238-243.
13. Ferretti A., De Carli A., Fontana M. Injury of the suprascapular nerve at the spinoglenoid notch. The natural history of infraspinatus atrophy in volleyball players. Am J Sports Med. 1998;26(6):759-763.
14. Ferretti A., Cerullo G., Russo G. Suprascapular neuropathy in volleyball players. J Bone Joint Surg Am. 1987;69(2):260-263.
15. Weiss J.M., Lennard T.A., Silver J.K., Weiss L.D. Easy Injections. New York: Elsevier Health Sciences; 2007.
16. Shanahan E.M., Ahern M., Smith M., et al. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis. 2006;62:400-406.
17. Shanahan E.M., Ahern M., Smith M., et al. Suprascapular nerve block reduced chronic shoulder pain and disability in degenerative disease or rheumatoid arthritis. Evid Based Med. 2004;9:50.
18. Bockenek W.L., Walsh N.E., Gans B.M., DeLisa J.A. Physical medicine and rehabilitationPrinciples and practice. Philadelphia: Lippincott Williams & Wilkins; 2004.
19. Argoff C.E., Turk D.C., Wu C.L., et al. Raj’s Practical Management of Pain. New York: Elsevier; 2008.
20. Büttner J., Meier G. Peripheral Regional Anesthesia. New York: Thieme; 2007.