Parts and definitions31
6.2 Cells of the nervous system, synapse33
6.3 Brain and spinal cord33
6.4 Spinal nerves35
6.5 Segmentation, dermatomes, myotomes36
6.6 Autonomic nervous system37
6.7 Spinal cord in the vertebral canal and spinal meninges39
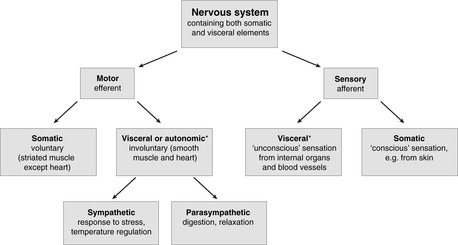
The brain and spinal cord constitute the central nervous system, cranial and spinal nerves the peripheral nervous system. Different descriptive terms are based on direction of impulse (sensory, motor), and nature of sensation or action (somatic, visceral; voluntary, involuntary). Cells of the nervous system are neurons and supporting cells (glial cells, Schwann cells). The central nervous system contains both nerve cell bodies (grey matter) and tracts of axons (white matter), disposed in the spinal cord according to function. Spinal nerves are attached to the spinal cord in such a way that a pair of nerves and the portion of cord to which they are attached constitute a segment. The autonomic (visceral) nervous system controls homeostasis and bodily functions of internal organs, visceral motor impulses forming the sympathetic and parasympathetic nervous systems. Within the vertebral canal the spinal cord is surrounded by spinal meninges. The cord is much shorter than the canal itself, so roots of spinal nerves originating from the low spinal cord must pass within the vertebral canal before they reach the intervertebral foramen through which they pass to the rest of the body.
You should:
• explain the terms central, peripheral, sensory, motor, somatic, visceral, voluntary, involuntary, and describe the relationships between them
• describe the basic organisation of the autonomic nervous system
• list the names and functions of different types of neurons and glial cells
• describe the basic organisation of the brain, spinal cord and spinal nerves
• describe the related concepts of segmentation, dermatomes and myotomes
• describe how the spinal cord is surrounded by spinal meninges, and the anatomy of lumbar puncture.
6.1. Parts and definitions
The nervous system consists of the brain, spinal cord and peripheral nerves. It is one of the means by which central control of bodily functions is maintained, and allows the body to respond to stimuli of various sorts. There are several ways of classifying the components of the nervous system (Fig. 6.1).
Geographical: central/peripheral
• Central nervous system. This is the brain and spinal cord.
• Peripheral nervous system. This is everything else, i.e.:
– cranial nerves arising from the brain: 12 pairs
– spinal nerves arising from the spinal cord: 31 pairs (usually).
Direction of nerve impulse: sensory or afferent/motor or efferent
A nerve impulse in a peripheral nerve may travel:
• towards the central nervous system: a sensory or afferent impulse; or
• away from the central nervous system: a motor or efferent impulse.
Nature of perception: somatic sensory/visceral sensory
• Somatic sensory impulses are those of which we are acutely aware, and which we are well able to localise (e.g. sharp pain, touch). These generally originate in body wall structures (rather than internal organs). These fibres may run in either cranial or spinal nerves.
• Visceral sensory impulses are either imperceptible, only vaguely localisable, or only become perceptible in disease. They arise from blood vessels or internal organs (viscera), may run in either cranial or spinal nerves and are also found in a network of nerves associated with the internal organs.
Type of action: voluntary motor/visceral (involuntary) motor
Voluntary motor impulses. These control skeletal muscle over which we have voluntary control. From various parts of the brain, nerve impulses pass down in the spinal cord to connect with neurons whose axons pass out of the central nervous system into peripheral nerves.
• The neuron or neurons entirely within the central nervous system are upper motor neurons.
• The neurons with cell bodies in the central nervous system, but whose axons pass into the peripheral nerves, are lower motor neurons. They are found in both cranial and spinal nerves.
Visceral (involuntary) motor or autonomic. These impulses control muscle over which we do not normally have voluntary control. These fibres may run in either cranial or spinal nerves, and are considered in more detail below and in section 6.6.
Autonomic (visceral) nervous system
The visceral components of the nervous system, visceral sensory and visceral motor, supply internal organs and blood vessels. They may be grouped together as the autonomic nervous system, although it is not an anatomically distinct entity. Some components are central, some peripheral: some are in cranial nerves, some in spinal nerves, and some in autonomic plexuses (networks) in and around internal organs.
I recommend that you use the term autonomic to include only visceral motor fibres: use the term visceral sensory for afferent impulses from internal organs and blood vessels.
6.2. Cells of the nervous system, synapse
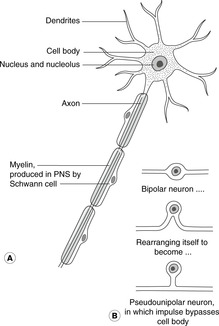
Neuron (Fig. 6.2)
Neurons are nerve cells. They consist of cytoplasm and a nucleus. The long cytoplasmic process that transmits impulses away from the cell body is the axon. The process that transmits impulses towards the cell body is the dendrite.
• Multipolar neurons. These are found throughout the central nervous system. Motor neurons in the spinal cord are multipolar (have more than one cytoplasmic process), one of the poles being the axon (Fig. 6.2A).
• Bipolar neurons. Peripheral sensory neurons are originally bipolar with one cytoplasmic process which conducts the nerve impulse from the receptor towards the cell body, and one which conducts the impulse from there to the central nervous system. For spinal nerves, and some cranial nerves, the bipolar cell rearranges its processes during development (Fig. 6.2B) to become pseudounipolar, presumably in the interests of speed of conduction (the impulse does not have to ‘wade’ through the cytoplasm of the cell body). The sensory neurons which remain truly bipolar are those of olfaction (smell), vision, hearing and balance where the receptors are close to the brain.
The cell bodies of sensory neurons in a peripheral nerve are all collected together in one site, a ganglion (swelling). In a spinal nerve the sensory ganglion is attached to the dorsal (posterior) root of the nerve (see below), and so is known as the dorsal (posterior) root ganglion; it is found in the region of the intervertebral foramen through which the nerve passes out of the vertebral canal. For a cranial nerve it is simply known as the sensory ganglion of that nerve, and is often given another name peculiar to itself.
Synapse
Neural pathways involve a chain of separate neurons. Junctional zones are called synapses: here the impulse at the end of one neuron stimulates the neuron to release chemicals (neurotransmitters) that cause electrical impulses to be generated in the succeeding neuron. Synapses are thus relay stations in the neural pathway.
Supporting cells: glial cells, Schwann cells
Supporting cells provide structural support and myelin. In the brain these are glial cells: oligodendrocytes for myelin production, astrocytes for structural support. In the spinal cord myelin is produced by Schwann cells. Glial cells give rise to the commonest brain tumours – gliomas.
6.3. Brain and spinal cord
Brain
The brain consists of:
• The brain stem: the central, midline portion made up of (from bottom up) medulla oblongata, pons and midbrain. It is continuous below with the spinal cord and above with the forebrain.
• The cerebellum, behind the pons.
• The forebrain: thalamic structures and right and left cerebral hemispheres.
Cranial nerves
There are 12 pairs of cranial nerves arising from the brain. They are usually designated by Roman numerals (I–XII), as in this text, and are concerned mainly with structures in the head and neck.
The cranial nerves and brain are considered in more detail in Chapters 14 and 15.
Spinal cord
The spinal cord is found within the vertebral (spinal) canal. It has a number of functions.
• It serves as a coordinating centre for each spinal cord segment, e.g. spinal reflexes.
• It receives sensory information from peripheral nerves and sends it on to the brain and to other places for the purposes of perception and for eliciting appropriate responses.
• It receives commands from the brain, and other centres, which it distributes to appropriate peripheral nerves.
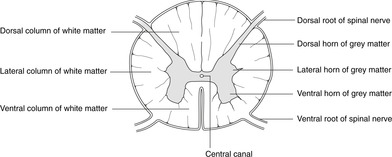
Grey and white matter (Fig. 6.3)
Neural tissue of the entire central nervous system consists of both axons and cell bodies. Axons are surrounded by myelin, a fatty substance which, like most fatty tissues, is almost white in colour. Thus, areas of the central nervous system that are rich in axons surrounded by myelin constitute the white matter. Areas of the central nervous system that largely consist of cell bodies rather than axons do not appear white, and these areas constitute the grey matter. In the spinal cord, grey matter is distributed in a butterfly shape around the central canal.
Regions of grey matter
These are described as horns because of their appearance on cross-section. There are, though, no structural barriers between the different areas.
• Ventral (anterior) horn. Cell bodies of lower motor neurons innervating voluntary muscle are found in the ventral grey horn, and so are called ventral (anterior) horn cells, often abbreviated to VHC or AHC. Disease of these cells, for example poliomyelitis, causes paralysis of voluntary muscle. The ventral horns are largest in those parts of the spinal cord that serve regions of the body with many muscles – the limbs: spinal cord segments C5–T1 for the upper limb and L2–S4 for the lower limb.
• Lateral horn. Cell bodies of motor neurons of the sympathetic system are found in the lateral horn. The lateral horn is present only in the thoracic and lumbar areas of the spinal cord.
• Dorsal (posterior) horn. The dorsal horn handles sensory impulses.
Regions of white matter: tracts
White matter is described as being disposed in columns around the grey matter: anterior, lateral and dorsal columns; again, there are no structural barriers between them. Within white matter, axons are arranged so that those of similar functions are grouped together to form a tract. These tracts are not sharply demarcated from each other: there may be some overlap between them.
Bundles of axons carrying impulses up to the brain form sensory tracts; bundles of axons carrying impulses down from the brain to neurons in the grey matter of the spinal cord form motor tracts. Their names usually reflect the journey of the impulses they carry: a tract beginning with spino- (e.g. spinothalamic, spinotectal) is a sensory tract, and a tract ending with -spinal (e.g. corticospinal, tectospinal) is a motor tract. The largest regions of white matter are the dorsal (posterior) columns: they contain heavily myelinated sensory fibres of large diameter (the degree of myelination and the large diameter giving a fast conduction speed).
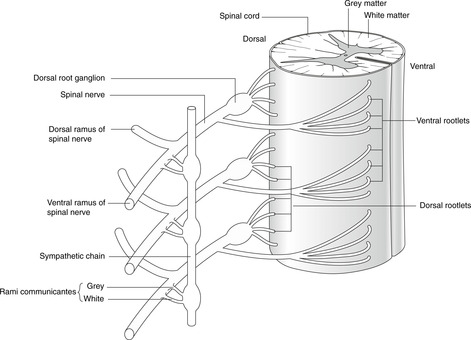
6.4. Spinal nerves
Note. In descriptions of the human nervous system, because humans stand erect, the terms dorsal and posterior are interchangeable, as are ventral and anterior. For the nervous system, I prefer dorsal and ventral to anterior and posterior.
Spinal nerves arise in pairs: 8 cervical, 12 thoracic, 5 lumbar and 5 sacral (forget about the coccygeal nerve). Each spinal nerve arises by a series of dorsal rootlets and ventral rootlets. As a general rule, dorsal rootlets convey sensory information into the spinal cord, and ventral rootlets convey motor information away from the spinal cord. These rootlets unite in or near the intervertebral foramen to form the spinal nerve. Nerves C1–7 emerge above the correspondingly numbered vertebrae; C8 nerve arises below vertebra C7 (remember, there are only seven cervical vertebrae), and thereafter the nerves emerge below the correspondingly numbered vertebra.
Dorsal root ganglion (Fig. 6.4)
As the dorsal rootlets converge, there is a swelling, the dorsal (posterior) root ganglion, which houses the cell bodies of all the sensory neurons in that particular nerve.
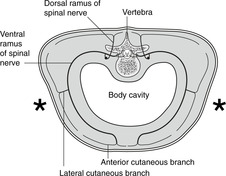
Branches of a typical spinal nerve (Figs 6.4, 6.5)
• Dorsal ramus. This supplies the dorsal one-third (about) of the body wall; dorsal rami do not contribute to the limbs.
• Ventral ramus. This supplies the ventral two-thirds (about) of the body wall including the limbs.
Beware of confusion!
Dorsal and ventral roots are not the same as dorsal and ventral rami. Dorsal roots convey sensory impulses; ventral roots convey motor impulses. Once these roots unite to form the nerve, all subsequent branches, including the rami, convey both sensory and motor impulses.
6.5. Segmentation, dermatomes, myotomes
The repeating pattern of spinal nerves reflects the pattern of somites in the embryo. Spinal nerves are called segmental nerves, and the area of the spinal cord from which they arise is known as a spinal cord segment: C5 spinal nerves arise from C5 segment of the spinal cord.
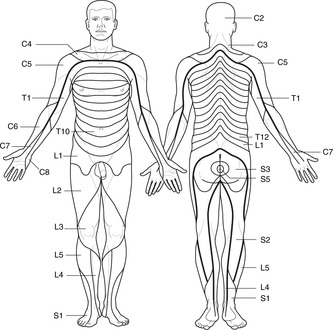
Dermatomes (Fig. 6.6)
The strip of skin supplied by one spinal nerve is the dermatome: the dermatome of C5 is supplied by C5 nerve which arises from C5 segment of the spinal cord. Dermatomes are useful clinically. If you find on examination of a patient that there is sensory loss that corresponds to an entire dermatome then you know that something is interfering with either the spinal nerve, the dorsal (sensory) rootlets, the dorsal root ganglion or the spinal cord itself. It is worth noting that there is sufficient overlap between dermatomes for damage to one spinal nerve to cause few if any sensory symptoms. Damage to two adjacent spinal nerves would be more apparent. Dermatome maps in different books differ. This is because people differ. The dermatome map given here is a kind-of average. Note that if you hold your upper limbs horizontal with the palms facing forwards, the sequence of dermatomes is more-or-less from above (cephalic) to below (basilic). This was once so also for the lower limb, but medial rotation of the lower limb during development complicates things (this is related to the reason why the elbows ‘point’ backwards but the knees forward).
Dermatomes bear no relation to Langer’s lines (Fig. 3.2, p. 17) despite their apparent similarity at first glance.
Shingles
Shingles illustrates the segmental arrangement of the nervous system and the dermatomes. A viral infection of a dorsal root ganglion causes pain and vesicular eruptions in the strip of skin innervated by the nerve on which the ganglion is situated.
Myotomes
The skeletal muscle supplied by one spinal cord segment is a myotome. Damage to ventral horn cells of spinal cord segment C5, or damage to the ventral roots of C5 nerve, will cause weakness or paralysis of muscles supplied by that nerve. Myotome distribution is different from dermatome distribution, and is considered in more detail in Chapters 12 and 13. It is worth noting here though that myotomes are distributed in a limb from proximal to distal rather than above to below as for dermatomes. Thus, in the upper limb, the muscles supplied by C5 are at or near the shoulder, and those supplied by T1 are in the hand. There is a comparable arrangement in the lower limb.
6.6. Autonomic nervous system
There are two parts: sympathetic and parasympathetic.
The sympathetic system prepares us for action:
• it is active when we are alert, fearful or stressed, dilating the pupil (mydriasis) and speeding the heart
• it is important in temperature regulation, supplying muscles that move cutaneous hair, regulate the calibre of cutaneous blood vessels, and provoke secretion of sweat (for cooling).
The parasympathetic system relaxes us for gut tube activity:
• it provokes salivary secretion, gastric activity and emptying, intestinal peristalsis, anal sphincter relaxation
• it constricts the pupil (miosis)
• it slows the heart
• and it has important reproductive functions.
There are two peripheral motor neurons to smooth muscle
Unlike motor impulses to voluntary muscle, autonomic (visceral motor) impulses to smooth muscle pass in two peripheral motor neurons with an intervening synapse, the two neurons being called presynaptic and postsynaptic. The synapses are found in autonomic ganglia, and the terms preganglionic and postganglionic are also used (more often, in fact).
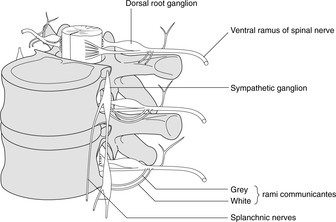
Layout of the sympathetic nervous system (Fig. 6.7)
Sympathetic impulses arise only from spinal cord segments T1 to L1 or 2, and so the term thoracolumbar is used to describe the sympathetic outflow from the cord. This limited origin demands that, in order for sympathetic impulses to reach all parts of the body, there must be a redistribution system. This is the sympathetic chain which is found on either side of the vertebral column: it certainly extends between T1 and L2, but it also extends higher than T1 so that impulses can pass to cervical spinal nerves and the head, and lower than L2 so that impulses can pass to nerves L3 and below.
In the spinal cord, sympathetic preganglionic impulses arise from the lateral horn cells between T1 and L1 or 2, an impulse passing into the spinal nerve of that segment and thence through a connection, the white ramus communicans, to the sympathetic chain. Once in the chain, several things may happen.
• The preganglionic impulse may synapse on the cell body of a postsynaptic (postganglionic) neuron, the axon of which passes back into the spinal nerve through the grey ramus communicans (grey because less myelinated than the white ramus) to be distributed in the territory of that same spinal nerve in which it emerged from the spinal cord.
• The preganglionic impulse may synapse on the cell body of a postsynaptic (postganglionic) neuron, the axon of which passes on to an adjacent segmental artery. By this means sympathetic impulses may pass to all branches of that artery.
• Having passed into the sympathetic chain, the preganglionic impulse may ascend or descend in the chain to gain another spinal nerve. This ‘new’ spinal nerve may be above T1 or below L2 – here is the sympathetic chain acting as the redistribution system referred to earlier. The preganglionic impulse synapses in the ganglion at the ‘new’ level and proceeds through the grey ramus of the ‘new’ level into the ‘new’ spinal nerve for distribution.
• The preganglionic impulse may pass through the ganglion without synapsing, into one of the branches of the sympathetic chain serving the thoracic and abdominal viscera. These are the cardiac and pulmonary branches and the splanchnic nerves. These impulses will synapse in a group of ganglia in plexuses in and around the aorta and its branches (cardiac, pulmonary, coeliac, superior mesenteric, renal, inferior mesenteric, hypogastric).
Layout of the parasympathetic nervous system
As in the sympathetic system, parasympathetic impulses traverse two peripheral motor neurons (pre- and postganglionic). Some arise from the brain stem and pass into cranial nerves III, VII, IX and X, and others arise from cell bodies in the sacral spinal cord and pass into spinal nerves S2, S3 and S4, with none arising between these two regions of the central nervous system. The word craniosacral is used to describe this pattern. The peripheral ganglia are in or on the destination organ, so postganglionic parasympathetic neurons are very short.
Visceral sensation
Sensory (e.g. pain) fibres from internal organs reach the central nervous system using either sympathetic or parasympathetic pathways (or both). However, as in the sensory system there is no peripheral synapse, the terms pre- and postganglionic fibres are irrelevant and wrong for visceral sensory nerves. The cell body of a visceral sensory neuron is in the sensory ganglion of whichever nerve delivers the impulse to the central nervous system, so sensory ganglia contain cell bodies of both somatic sensory and visceral sensory neurons.
Referred pain
Disease of internal organs and the gut tube may cause pain, which the patient interprets as arising from skin. This is because, to put it simply, the brain is confused into thinking the pain is coming from skin (which is where pain often comes from) rather than from an internal organ supplied by a neuron of the same spinal segment that supplies the skin. The internal pain is said to be ‘referred’ to a particular dermatome. The physiology of this is not understood.
Ganglion – beware!
You have met two types of ganglion in the preceding sections: a sensory ganglion in section 6.2 and an autonomic ganglion in section 6.6. Both consist of a collection of cell bodies in the peripheral nervous system, but one has synapses and the other does not.
• A sensory ganglion is simply the site at which the cell bodies of all the bipolar or pseudounipolar sensory neurons in that particular nerve are gathered together.
• An autonomic ganglion is the site of the synapse between preganglionic and postganglionic autonomic neurons.
• Ganglia are either sensory or autonomic: they are never both.
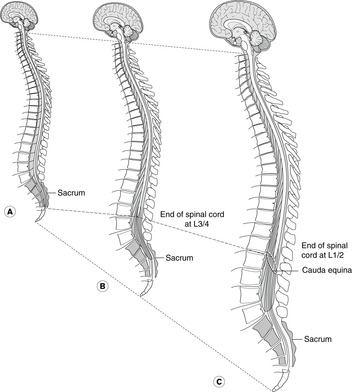
6.7. Spinal cord in the vertebral canal and spinal meninges
The vertebral (spinal) canal extends throughout the vertebral column, but the spinal cord in the adult is considerably shorter than this. This was not so in fetal life when the cord more nearly filled the canal, but as development proceeds the vertebral column grows more than the spinal cord so that by adulthood there is a considerable discrepancy. In the newborn, the end of the spinal cord is level with vertebra L3, but in the adult it is level with vertebra L2 or even L1. This means that while the origin of the cervical spinal nerves is roughly level with the cervical vertebrae, the thoracic, lumbar and sacral nerves originate higher than their companion vertebrae, the disparity increasing towards the sacral region. The sacral spinal cord (giving origin to sacral spinal nerves) is, in fact, level with the lower thoracic and upper lumbar vertebrae.
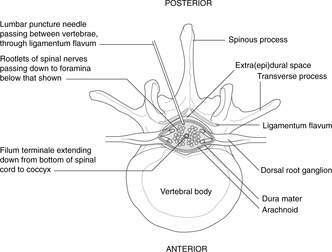
Cauda equina (Fig. 6.8)
As a result of this, lumbar and sacral spinal nerve roots must pass down in the vertebral canal for quite a distance before they reach the intervertebral foramen through which they pass, and after which they are numbered. The collection of these nerve roots occupying the vertebral canal below the bottom of the spinal cord is the cauda equina. It may be compressed by central herniation of the intervertebral disc (Ch. 5, p. 25), leading to cauda equina syndrome (Ch. 11, p. 15).
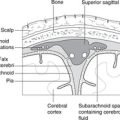
Meninges (Fig. 6.9)
The spinal cord is surrounded by the meninges (covering membranes) which are continuous with the meninges of the brain (see Ch. 14).
• Pia mater: on the surface of the spinal cord and inseparable from it (Greek: pia = tender).
• Arachnoid mater: joined to the pia by thin strands of tissue (Greek: arakhnes = spider).
• Dura mater: tough and fibrous (Latin: dura = hard), longitudinal fibres. At about the point where the spinal nerve passes through intervertebral foramen, the dura is continued along the nerve as a thick fibrous envelope, the perineurium. Nerve roots in the subarachnoid space lack this covering and so are more fragile than spinal nerves. In traumatic injury to the vertebral column, nerve roots are more often torn than nerves themselves.
The meninges are themselves supplied by sensory nerve fibres which are branches of cranial and spinal nerves, so inflammation of the meninges (meningitis) is painful.
Filum terminale
At the lower margin of the spinal cord, at about vertebral level L2, the pia mater surrounding the cord is prolonged down to attach to the coccyx in the vertebral canal, even though it contains no neural tissue. It is as if this prolongation of pia mater had been occupied by spinal cord in fetal life, but as the spinal cord apparently withdraws upwards during development and maturation, the sleeve of pia mater that contains it becomes empty. This ‘envelope’ of pia mater is the filum terminale and it is found amidst the nerve roots making up the cauda equina.
Subarachnoid space and cerebrospinal fluid
Between the pia and the arachnoid is the subarachnoid space containing cerebrospinal fluid. The pressure of the cerebrospinal fluid in the subarachnoid space keeps the thin arachnoid in contact with the dura such that the space between the arachnoid and dura, the subdural space, is not normally present. The arachnoid and the dura mater normally occupy the vertebral canal well into the sacrum, down to about vertebral level S2.
Denticulate ligament
This is a lateral extension of the pia mater extending from the cord in a coronal plane about midway between the dorsal and ventral nerve roots to meet the internal aspect of the arachnoid in a series of sawtooth-like projections. It helps to tether the spinal cord within the subarachnoid space.
Extradural or epidural space
Outside the dura mater, between it and the walls of the bony canal, is the extradural or epidural space. This contains connective tissue, fat and the internal vertebral venous plexus.
Surface anatomy
• Vertebral level (about) T11–L1/2: sacral region of spinal cord.
• Vertebral level L1/2: end of spinal cord in adult.
• Vertebral level L3/4: end of spinal cord at birth.
• Vertebral level S2: end of dural sac and subarachnoid space.
Lumbar puncture (Fig. 6.9)
The subarachnoid space below vertebral level L1/2 is occupied by cerebrospinal fluid and the cauda equina, but not by the spinal cord. This is the lumbar cistern of cerebrospinal fluid (a cistern is a region of the subarachnoid space), and into it needles may be inserted to sample the cerebrospinal fluid without risk of damaging the spinal cord itself. This is a lumbar puncture.
A hollow needle is inserted through the skin of the back, usually slightly off centre, and approaches the vertebral column from behind. The needle passes through the ligamentum flavum (a ‘give’ is felt) between adjacent vertebral laminae. The tip of the needle is now in the extradural space. It should be further advanced until it has pierced the dura and arachnoid together (another ‘give’), at which point clear cerebrospinal fluid should pass through the needle and a sample can be taken for analysis.
In the adult this is best done at vertebral level L3/4, the surface marking for which is a line drawn between the highest points of the right and left iliac crests. In the child, where the spinal cord is relatively longer with respect to the vertebral column, lumbar puncture would be performed one or two intervertebral spaces lower.
Epidural anaesthesia and spinal anaesthesia
A liquid anaesthetic agent may be injected into the extra(epi)dural space. This is an epidural anaesthetic and it will anaesthetise the spinal nerve roots it surrounds. It is normally performed as would be a lumbar puncture except that the needle is not advanced after the first ‘give’ (see above). It is particularly useful for procedures in the pelvis and perineum (supplied by lumbar and sacral nerves) where the patient is unfit for a general anaesthetic.
In spinal anaesthesia, the needle is inserted as in a lumbar puncture and the anaesthetic agent is injected into the subarachnoid space. The specific gravity of these agents is greater than that of the cerebrospinal fluid and so by altering the position of the patient the anaesthetic can be restricted to the lower region of the subarachnoid space. It produces a more profound anaesthesia and lasts longer than an epidural anaesthetic.