The big picture237
14.2 Skull bones and joints, cranial cavity238
14.3 Cervical vertebrae, joints and muscles of the neck243
14.4 Cranial nerves247
14.5 Neck257
14.6 Face, parotid, VII, scalp264
14.7 Anatomy of mastication268
14.8 Anatomy of swallowing and phonation273
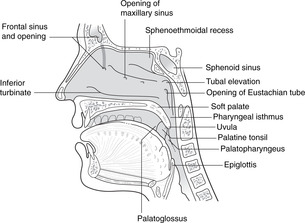
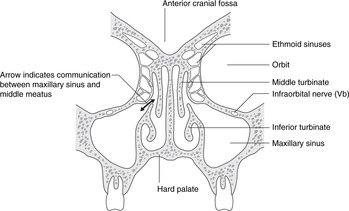
14.9 Nose, nasal sinuses and the sense of smell: cranial nerve I279
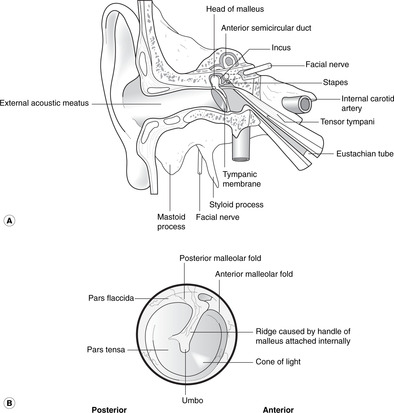
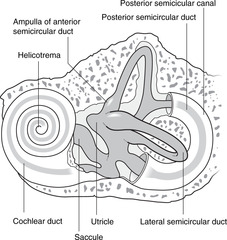
14.10 Ear, hearing and vestibular function: cranial nerve VIII282
14.11 Orbit, eye movements, vision, visual reflexes; cranial nerves II, III, IV, VI288
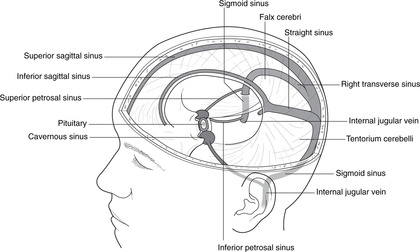
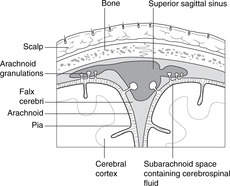
14.12 Inside the skull, haemorrhages295
14.13 Sympathetic impulses to the head299
14.1. The big picture
The head houses the brain, main sense organs and the upper end of the respiratory and alimentary systems. Twelve pairs of cranial nerves arise from the brain. Arterial blood comes from the common carotid and vertebral arteries. Veins drain principally to the internal jugular vein, and lymph to the deep cervical chain.
Skeleton
The skeleton of the head and neck serves several functions. Some of its components, the neurocranium, protect the brain and organs of the special senses. Some components, the viscerocranium, provide structural support for the cranial end of the gut tube and attachments for its muscles. Cervical vertebrae provide structural support for the head and muscle attachments for head and neck movements, and cartilages in the anterior neck provide a structural framework for the upper end of the respiratory system and attachments for muscles of phonation.
Nerves
• Cranial nerves. The 12 pairs of nerves that pass through or into the skull bones are probably the most important aspects of head and neck anatomy as far as the general physician is concerned. They serve various functions:
– special senses: olfaction, vision, balance, hearing
– sustenance: ingestion, digestion
– communication: facial expression, speaking.
A survey and analysis of the cranial nerves follows (section 14.4, p. 247) to provide a foundation for their various aspects that appear and reappear as the several regions and functions of the head and neck are considered. Cranial nerves are referred to by Roman numerals, I, II, III, etc.
• Cervical spinal nerves 1–8 supply structures in the neck and contribute to the innervation of the upper limb, upper thoracic skin and diaphragm. They are similar in form and function to other spinal nerves.
The brain attempts to integrate, coordinate and control these neural functions.
Arteries
• Carotid system. The right and left common carotid arteries bifurcate to give the internal and external carotid arteries of each side.
– External carotid arteries give branches in the neck to supply the neck, scalp, skull bones and cranial dura mater.
– Branches of the two carotid systems communicate, particularly in the scalp and around the orbit.
• Vertebrobasilar system. The vertebral arteries supply the cervical vertebrae and spinal cord. They enter the cranial cavity through the foramen magnum, uniting to form the basilar artery, which supplies the brain stem. It terminates by contributing to the arterial circle of Willis with the internal carotids.
• The arterial circle of Willis supplies the brain.
Veins
• Dural venous sinuses within the cranium: these form an intracranial network of veins that receive blood from the brain and drain to the:
• Internal jugular veins: deep veins in the neck, with tributaries from the face and neck.
• External and anterior jugular veins: superficial veins from the skull, face and superficial tissues.
• There are many communicating channels between the internal and external systems.
• Venous blood from the cranial cavity also drains through the foramen magnum to the internal vertebral venous plexus of the vertebral column.
Lymph nodes
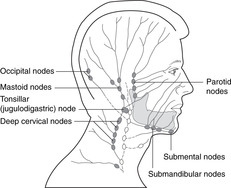
• Groups of lymph nodes, many palpable, are shown in Figure 14.1. In the head, lymph from a particular organ or region passes, in general, to whichever group of nodes is nearest. These then drain to the deep cervical chain and thence to the venous system at the union of the internal jugular and subclavian veins. The palpable lymph node at the top of the deep cervical chain, just behind the angle of the mandible, is the jugulodigastric or tonsillar node, so called because it is the node most commonly affected in tonsillitis. If you suffered as a child from frequent attacks of tonsillitis, you may have a permanently enlarged tonsillar node.
• The entrance to the gut tube is surrounded by Waldeyer’s ring of lymphoid tissue: tonsils, adenoids, and lingual tonsils. This is continuous with the upper end of the deep cervical chain and drains to it.
• Retropharyngeal nodes. Involvement of nodes between the vertebral column and the pharynx is dangerous. The nodes are deep and therefore impalpable, so if disease spreads to this group of nodes, it is likely to go undetected until it has also spread elsewhere, by which time it is likely to be too late for effective treatment. Retropharyngeal nodes are connected to the deep cervical nodes of both sides and so provide a pathway for lymphatic spread across the midline.
14.2. Skull bones and joints, cranial cavity
The skull is made up of several separate bones united by fibrous sutures. The only synovial joint in the skull is the temporomandibular joint at which the movements of chewing occur. The internal aspect of the cranium is divided into three cranial fossas. There are numerous named foramina to allow structures to pass through the cranium. The fetal skull is different from the adult skull in a number of ways apart from size.
Bones
There are two types of skull bones:
• Neurocranium: flat bones of the vault of the skull. These consist of two plates of cortical bone, inner and outer tables or diploë, between which is the diploic cavity containing marrow. This is a site of haemopoiesis and so has a rich blood supply.
• Viscerocranium: these are bones of the base of the skull surrounding the nasal cavity and sinuses, oral cavity, pharynx and larynx.
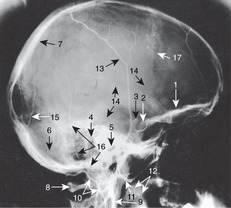
Study the bones of the skull (Fig. 14.2, Fig. 14.3, Fig. 14.4, Fig. 14.5 and Fig. 14.6). Most of them reach the external surface of the skull, so identify and palpate them on yourself. Four of them (see below) are worth studying in some detail.
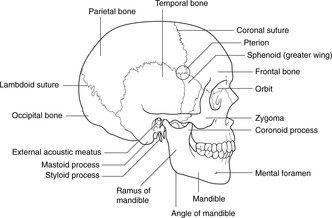 |
| Fig. 14.2 |
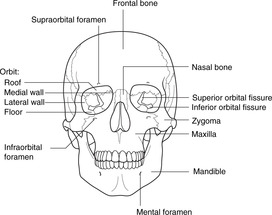 |
| Fig. 14.3 |
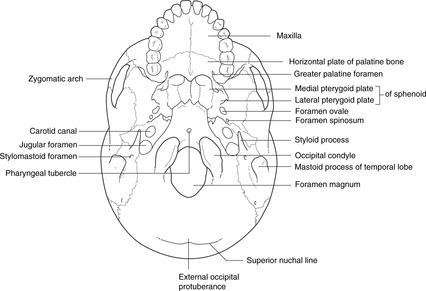 |
| Fig. 14.4 |
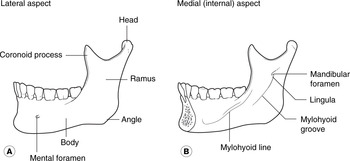
Mandible (Fig. 14.6)
The right and left mandibles fuse in the second year after birth.
• Body and ramus, lateral aspect:
– mental foramen
– angle.
• Body and ramus, medial (internal) aspect:
– angle
– mandibular foramen, lingula
– mylohyoid line and groove.
• Alveolar (teeth) sockets.
• Coronoid process.
• Neck, head (condyle), articular surface.
Occipital bone (Figs 14.4, 14.5)
• Basi-occiput: equivalent to the vertebral bodies below:
– foramen magnum
– condyles: convex, for the reciprocal surface of the atlas
– hypoglossal (condylar) canal
– pharyngeal tubercle.
• Squamous part, external aspect:
– external occipital protuberance
– superior nuchal lines.
• Squamous part, internal aspect:
– internal occipital protuberance, ridges for meningeal attachments.
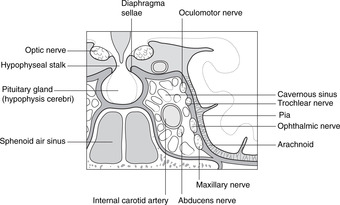
Sphenoid bone (Fig. 14.5)
• Body, articulating with the basi-occiput.
• Sphenoid air sinus.
• Pituitary fossa (sella turcica), dorsum sellae, clinoid processes.
• Greater wing, lesser wing, optic foramen, superior orbital fissure, foramen rotundum, foramen ovale, foramen spinosum, spine (inferior aspect).
• Lateral and medial pterygoid plates, hamulus (palpable in the mouth behind and medial to the third upper molar).
Temporal bone (Figs 14.2, 14.4, 14.5)
• Petrous temporal: ridge and apex.
• Internal acoustic (internal auditory) meatus.
• Mastoid process, mastoid antrum and air cells, middle ear cavity, orifice for Eustachian tube.
• Squamous temporal.
• External acoustic (external auditory) meatus.
• Articular (condylar) surface for the head of the mandible.
• Zygomatic process forming the zygomatic arch with the zygoma.
• Carotid canal, foramen lacerum.
• Styloid process.
• Stylomastoid foramen.
Pterion (Fig. 14.2). This is an area on the lateral side of the skull where the frontal, parietal, temporal and sphenoid bones meet. Its surface marking is about 4 cm above a point one-third of the way from ear to eye. Its importance will be pointed out later (p. 296).
Bones worth only a brief survey
• Parietal: diploë, grooves for meningeal vessels.
• Frontal: supraorbital margin and notch, frontal sinus.
• Zygoma: zygomatic arch formed by zygoma and temporal bone.
• Ethmoid: crista galli, perpendicular plate, cribriform plate, ethmoid sinuses, superior and middle turbinates.
Bones you need only to have heard of
• Vomer: a midline, unpaired, bone forming the posterior part of the nasal septum.
• Lacrimal bone: on the anteromedial aspect of the orbit, near the opening of the nasolacrimal duct.
• Inferior turbinate: the lowest of the three bones projecting into the nasal cavity from the lateral wall (the other two are parts of the ethmoid).
• Palatine: deep in the skull, forming the posterolateral palate and part of the lateral side of the nasal cavity.
• Nasal bone: the bony part of the nasal bridge, sometimes fractured.
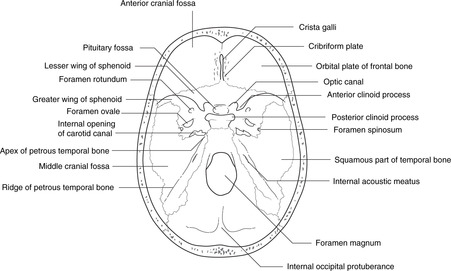
Internal aspect of the cranium, cranial fossas (Fig. 14.5)
• The floor of the internal aspect of the cranial cavity is divided into three cranial fossas:
– Anterior cranial fossa: anterior to the lesser wing of the sphenoid, related to the frontal lobes of the brain and the olfactory bulbs. Its features include the cribriform plate and crista galli of the ethmoid.
– Middle cranial fossa: between the lesser wings of the sphenoid and the ridge of the petrous temporal bones, related to the temporal lobes and cavernous (venous) sinus. Its features include the pituitary fossa, foramina for cranial nerves II–VI, the carotid canal, and foramen spinosum.
– Posterior cranial fossa: posterior to the ridge of the petrous temporal bone, related to the medulla, pons and cerebellum. It is covered by the tentorium cerebelli. Its features include foramina for cranial nerves VII–XII and the foramen magnum.
• The vault of the skull is formed by frontal, parietal, squamous temporal and squamous occipital bones. The internal aspect of the vault displays grooves for meningeal vessels supplying bones and dura, and ridges for dural attachments forming intracranial partitions and the edges of the dural venous sinuses.
• Cranial meninges, meningeal vessels and venous sinuses are described in section 14.12 (p. 296).
Skull foramina
Although not all these are important clinically, they are given here for the sake of completeness (Table 14.1). The list is not exhaustive.
| Bone | Name | Contents | Effect of damage at the foramen |
|---|---|---|---|
| Ethmoid | Cribriform plate | I | Post-traumatic anosmia and CSF rhinorrhoea |
| Sphenoid | Optic foramen | II, ophthalmic artery | Not likely, eye blindness |
| Superior orbital fissure | III, IV, Va, VI | Fractures may cause squints | |
| Foramen rotundum | Vb | Not likely | |
| Foramen ovale | Vc | Not likely | |
| Foramen spinosum | Middle meningeal artery | Not likely | |
| Sphenoid/temporal | Carotid canal | Internal carotid artery | Not likely |
| Mandible | Inferior alveolar | Inferior alveolar nerve and vessels | Mandibular fractures may damage this nerve (mental anaesthesia) |
| Mental | Mental nerve | Mental anaesthesia | |
| Temporal bone | Stylomastoid foramen | VII | Facial palsy, weakness |
| Internal acoustic meatus | VII, VIII | Deafness, balance disorders | |
| Occipital/temporal | Jugular foramen | IX, X, XI, internal jugular vein | Not likely |
| Occipital | Hypoglossal canal | XII | Not likely |
| Foramen magnum | Lower brain stem, vertebral arteries, XI, meninges | Trunk and limbs paralysis, death |
Joints and growth of the skull
Sutures (Fig. 14.2)
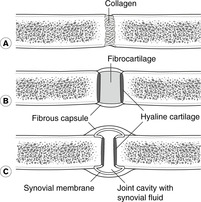
Sutures are fibrous joints (see section 4.2, p. 21), the most important being:
• coronal – between the frontal bone and the two parietal bones
• sagittal – between the two parietal bones
• lambdoid – between the parietal bones and the occipital bone.
Suture lines are irregular and sometimes contain islands of bone (sutural bones, of no significance). Once sutures have fused no movement is possible, but before that there may be a little and the edges of the sutures may overlap. This is particularly so during childbirth when the fetal skull is deformed as it passes through the mother’s pelvis. Growth at the sutures stops at about puberty, after which they are gradually obliterated from inside out. The metopic suture between the two frontal bones fuses during childhood (but may persist for longer), the sagittal suture fuses in the third decade, and those around the temporal bone may be present until old age.
Primary cartilaginous joints
The joint between the occipital and sphenoid bones is a primary cartilaginous joint (see section 4.2, p. 21). Fusion of these bones occurs when anteroposterior growth ceases after puberty, usually in the mid-20s.
Synovial joints
There is only one on each side, the temporomandibular joint (see p. 268).
Fetal and neonatal skull
Fontanelles
Until the bones are completely ossified, the defects between them are occupied by fibrous connective tissue. Two such areas are large at birth:
• posterior fontanelle, in the midline between the occipital and parietal bones; it closes in the first 6 months of postnatal life
• anterior fontanelle, in the midline between the frontal and parietal bones; it closes between 18 months and 2 years after birth. It is clinically useful:
– It can be used to assess intracranial pressure and the state of hydration. In a healthy baby it should be slightly convex and ‘give’ only a little to the touch, but if the child is dehydrated the fontanelle will be concave and feel ‘floppy’. In raised intracranial pressure it may bulge markedly.
– Through it, drugs can be injected into the subarachnoid space and samples of cerebrospinal fluid can be withdrawn more easily than by performing a lumbar puncture. Beware: a needle inserted in the midline will yield blood, not cerebrospinal fluid, because of the superior sagittal sinus: see Figure 14.37.
 |
| Fig. 14.37 |
Cephalhaematoma
A cephalhaematoma is a subperiosteal haemorrhage: the blood collects between the bone itself and the overlying periosteum. It may occur during birth, possibly as a result of the inept use during delivery of forceps or some other mechanical extraction device. The haematoma is limited to the shape of the underlying bone, because the periosteum is attached to the bone at the sutures.
Three of the more obvious differences between the neonatal skull and a mature skull are:
• Size: always state the obvious.
• Several protuberances of the skull bones form as a result of muscular attachments, of which a good example is the mastoid process, which develops postnatally as a result of the action of sternocleidomastoid. The lack of a mastoid process means that the facial nerve emerging from the stylomastoid foramen is superficial and vulnerable.
• As a proportion of the skull as a whole, the face is much smaller in the newborn, reflecting the fact that the child has not yet had to use its gut tube for sustenance.
14.3. Cervical vertebrae, joints and muscles of the neck
There are seven cervical vertebrae with special functional adaptations in C1 and C2 to allow for nodding and rotation. Elsewhere, features of cervical vertebrae are similar to those of other vertebrae. The cervical spine is more mobile than other regions of the vertebral column.
Vertebrae C3–7
Revise the features of a typical vertebra (see Fig. 5.1, p. 26). Vertebrae C3–7 are typical cervical vertebrae (see section 5.4, p. 26), the particular features of which are:
• triangular vertebral canal
• foramen in the transverse process (foramen transversarium) for vertebral vessels
• anterior and posterior tubercles on the transverse processes
• bifid posterior spinous process for the attachment of a tough nuchal ligament (ligamentum nuchae).
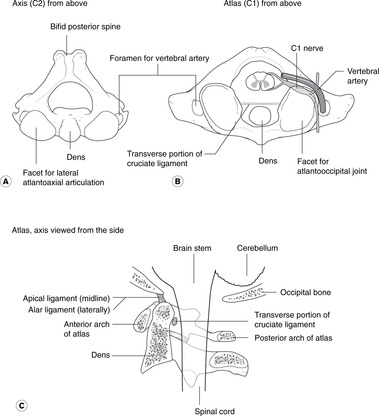
Vertebra C2, the axis (Fig. 14.8)
• Vertebra C2 can be thought of as a typical cervical vertebra with its body extended upwards to form the dens (tooth) or odontoid (tooth-like) process. This is a pivot around which vertebra C1 rotates. Embryologically, the dens is the body of C1, which has fused with C2, so there is no intervertebral disc between C1 and C2.
• There are large articular facets on the upper surface of the lateral sides of the body: these are the articulations for gliding movements with the atlas. Unlike facet joints elsewhere in the vertebral column, these are anterior to the emerging spinal nerves.
Vertebra C1, the atlas (Fig. 14.8)
Noteworthy features of the atlas are:
• it has no body (see above)
• anterior arch, the posterior surface of which has a facet for articulation with the dens
• posterior arch
• lateral masses where the anterior and posterior arches meet, palpable immediately behind the angle of the mandible (the atlas is surprisingly wide)
• inferior articular facets for reciprocal surfaces on the axis (see above)
• superior articular facets, concave, for the convex occipital condyles, for nodding movements
• groove for the vertebral artery (see below) on the superior surface.
The atlas is higher than you might think: it lies behind the mouth, so radiographs of the dens and atlas are taken through the open mouth (if the mouth were closed, teeth would obscure the radiographic view).
Joints of the cervical vertebral column
Joints below C2
These are as described in Chapter 5 (section 5.5, p. 27). There are symphyses with intervertebral discs in the midline and the facet joints laterally. The mobility of the cervical vertebral column means that there is considerable wear and tear on the facet joints and disease of them can cause cervical nerve root irritation and neck pain.
C2–1: atlanto-axial joints and ligaments (Fig. 14.8)
• In the midline. There is a synovial joint between the dens and the back of the anterior arch of the atlas (where facets may be seen), and a synovial bursa between the dens and the cruciate ligament behind it. The dens is kept in place by the cruciate ligament.
• Laterally. The lateral articular surfaces are flat to allow for gliding movements during rotation.
Cruciate ligament (Fig. 14.8). This cross-shaped ligament separates the dens from the spinal meninges. The horizontal component of the ligament is attached to the sides of the spinal canal, and the vertical component runs from the lower part of the body of C2 to the occipital bone above. There is a synovial bursa between the ligament and the posterior aspect of the dens.
Atlanto-occipital joints
These are synovial joints with reciprocally curved surfaces for nodding. They are anterior to the spinal nerves as they emerge from the intervertebral foramen.
Notochordal remnants
Midline structures in this region (dens, apical ligament) are derived form the notochord, and tumours of notochordal remnants, chordomas, occasionally develop here.
Movements of the cervical spine
Flexion and extension occur, as in the rest of the vertebral column. Lateral flexion and rotation are not limited by ribs, as they are in the thorax. The cumulative result of smaller movements between adjacent vertebrae adds up to great flexibility.
Muscles (Fig. 14.9)
 |
| Fig. 14.9 |
Flexion, lateral flexion
• Sternocleidomastoid. Attachments: sternum, clavicle–mastoid process. Nerve supply: accessory nerve (cranial XI). Sternocleidomastoid flexes the cervical spine and moves the chin upwards and away from the muscle. It is a good test of accessory nerve function: to test the right accessory nerve, ask the patient to rotate his head to the left against the resistance of your hand on his chin.
• Scalene muscles: lateral flexion. Nerve supply: branches from cervical nerves. These muscles arise from the transverse processes of C3–6, scalenus anterior passing to the first rib between the subclavian vein and artery, and scalenus medius passing to the first rib behind the subclavian artery (see section 10.4, p. 87).
• Prevertebral (longus) muscles run between anterior aspects of upper thoracic and cervical vertebrae and the skull. You need only know that they exist.
Extension
• Trapezius. Attachments: external occipital protuberance and nuchal ligament – spine and acromion of scapula. Nerve supply: accessory nerve (cranial XI). Trapezius extends the head and cervical spine and its role in shoulder abduction has been considered (section 12.3, p. 174). Shrugging the shoulders against resistance is a test of accessory nerve function.
• Postvertebral muscles (‘erector spinae’) muscles (see section 5.5, p. 27). Nerve supply: dorsal rami of spinal nerves.
• Small suboccipital muscles run between the atlas, the spinous process of the axis and the occipital bone and are supplied by branches of C1 and C2 nerves. They are responsible for movements that take place from minute to minute as we move our heads for listening, expressing emotion, talking, viewing and listening. You need know nothing of their detailed anatomy.
Greater occipital nerve, C2
The greater occipital nerve is the dorsal ramus of C2. It is a large sensory nerve which emerges posteriorly between vertebrae C1 and C2, and passes backwards between the suboccipital muscles before turning upwards to supply the skin of the back of the head and scalp as far forwards as the vertex. It has been suggested that compression of the nerve in the suboccipital region, perhaps by muscular tension, may be the cause of many headaches – a theory which has not been disproved – so perhaps there is something in the postural exercises advocated by adherents of the Alexander technique who maintain that certain relaxation exercises involving the cervical spine and skull can improve posture, lessen neck pain and generally promote a feeling of well-being.
14.4. Cranial nerves
You will need to return to this section repeatedly as you come across cranial nerves in other parts of the text.
Cranial nerves arise from the brain and are numbered I–XII roughly in the order that they arise. Some are simple, either motor nerves or sensory nerves; some are complex: mixed motor and sensory, with parasympathetic and other impulses travelling with them and their branches on what appears at first sight to be a haphazard basis. Despite the complexity of some cranial nerves (particularly V, VII), each cranial nerve has one or two functions that matter more than the others. In the clinical situation cranial nerves are often referred to by number alone (I, II, III, etc.).
You should:
• list the names and numbers of all 12 cranial nerves
• be able to refer to cranial nerves by number only
• list the most important function of each cranial nerve
• describe how to test each cranial nerve (this will not be possible until you have completed your study of the head and neck)
• describe the principal features of the course of each cranial nerve (this will not be possible until you have completed your study of the head and neck).
Functions, attachments and skull foramina of cranial nerves (Table 14.2)
A brief analysis
• Sensory nerves: I, II, VIII. These are nerves of the special senses.
• Motor nerves: III, IV, VI, XI, XII:
– III, IV and VI innervate muscles that move the eyeball.
– XI innervates sternocleidomastoid and trapezius.
– XII innervates tongue muscle.
• Mixed nerves: V, VII, IX, X. These nerves supply structures derived from embryonic branchial arches at the cranial end of the gut tube.
– Motor fibres are called branchiomotor: they are responsible for movements of the mandible, face, pharynx and larynx.
– Sensory components convey a mixture of cutaneous sensation (e.g. tactile, pain, temperature) and visceral sensation (e.g. taste) from the face, mouth, nose, pharynx and larynx, and in the case of X, visceral sensation from the thorax and abdomen.
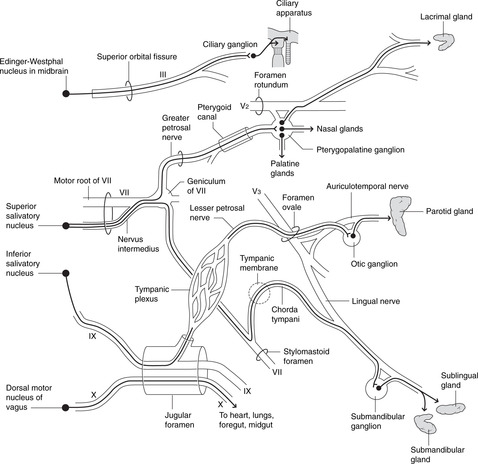
• Preganglionic parasympathetic fibres leave the brain stem in III, VII, IX and X but in order to reach their destinations those in III, VII and IX leave these nerves and hitch a lift with branches of V, with the ganglion (synapse) somewhere on the way. Parasympathetic fibres in X pass to the thorax and abdomen (see p. 257 and Fig. 14.14).
 |
| Fig. 14.14 |
• Sensory fibres in cranial nerves:
– Cutaneous and oral sensation (tactile, pain, temperature): most impulses reach the brain stem in V, with a few in X. In the brain stem they pass to the trigeminal sensory nuclei, so called (presumably) because the trigeminal nerve contributes most.
– Visceral sensation (e.g. taste, impulses from chemoreceptors): impulses reach the brain stem in VII, IX and X. In the brain stem the impulses pass to the nucleus of the solitary tract (tractus solitarius) in the medulla (see p. 257 and Fig. 14.15).
 |
| Fig. 14.15 |
| Nerve | Type | Main function (less important functions in brackets | Typical symptoms of damaged nerve |
|---|---|---|---|
| I Olfactory | Sensory | Smell | Anosmia |
| II Optic | Sensory | Vision | Visual impairment |
| III Oculomotor | Motor | Movements of eyeball, upper eyelid | Squints, ptosis |
| Parasympathetic: pupilloconstriction, accommodation | Dilated pupil, poor accommodation | ||
| IV Trochlear | Motor | Superior oblique (only) | Squint |
| V Trigeminal | Mixed | ||
| Va Ophthalmic | Sensory | Eyeball, anterior scalp, upper face | Sensory loss in affected area |
| Vb Maxillary | Sensory | Nasal cavity and sinuses, palate, upper teeth, mid-face | Sensory loss in affected area |
| Vc Mandibular | Motor | Muscles of mastication | Impaired chewing |
| Sensory | Chin, temple, oral cavity, tongue, temporomandibular joint, lower teeth, ear | Sensory loss in affected area | |
| VI Abducens | Motor | Lateral rectus (only) | Medial squint |
| VII Facial | Mixed | ||
| Motor | Muscles of facial expression | Facial palsy, weakness | |
| (Motor) | (Parasympathetic: lacrimal, nasal, palatine, submandibular, sublingual glands) | (Dry mouth) | |
| (Sensory) | (Taste, anterior tongue) | (Loss of taste) | |
| VIII Vestibulocochlear | Sensory | Balance and position in space, hearing | Disturbance of balance and/or deafness |
| IX Glossopharyngeal | Mixed | ||
| Sensory | Oropharynx, posterior tongue, carotid body and sinus | Not often involved in disease | |
| (Sensory) | (Taste, posterior tongue) | Loss of taste | |
| (Motor) | (Stylopharyngeus) | ||
| (Motor) | (Parasympathetic, parotid gland) | Dry mouth | |
| X Vagus | Mixed | ||
| Motor | Muscles of pharynx, larynx for swallowing, phonation | Impaired swallowing, hoarseness of voice (depends upon site of lesion) | |
| (Motor) | (Parasympathetic: cardiac muscle; muscles and glands of foregut and midgut) | Not much | |
| Sensory | Sensation from ear, pharynx, larynx | Abolition of cough reflex | |
| (Sensory) | (Sensation from heart, lungs, abdominal viscera) | ||
| (Sensory) | (Taste: epiglottic region) | Loss of taste, abolition of cough reflex | |
| XI Accessory | Motor | Sternocleidomastoid, trapezius | Limited head and neck movements and shoulder abduction beyond 90° |
| XII Hypoglossal | Motor | Tongue muscles | Impaired chewing and speaking |
Cranial nerve attachments and skull foramina (Table 14.3)
Cranial nerves I and II are attached to the cerebral hemispheres, and nerves III to XII to the brain stem (midbrain, pons and medulla). All nerves except IV arise from the ventral aspect.
| Brain attachment | Nerve | Foramen or canal (cranial bone in brackets) |
|---|---|---|
| Forebrain | ||
| Cerebral cortex, frontal lobes | I | Cribriform plate (ethmoid) |
| Diencephalon | II | Optic canal (sphenoid) |
| Midbrain | ||
| Upper, ventral aspect | III | Superior orbital fissure (sphenoid) |
| Lower, dorsal aspect | IV | Superior orbital fissure (sphenoid) |
| Hindbrain | ||
| Pons | V | |
| Va | Superior orbital fissure (sphenoid) | |
| Vb | Foramen rotundum (sphenoid) | |
| Vc | Foramen ovale (sphenoid) | |
| Pontomedullary junction, medial | VI | Superior orbital fissure (sphenoid) |
| Cerebellopontine angle | VII | Internal acoustic meatus, facial canal, stylomastoid foramen (temporal) |
| Cerebellopontine angle | VIII | Internal acoustic meatus (temporal) |
| Medulla | IX, X | Jugular foramen (between occipital and temporal) |
| Medulla, spinal cord | XI | Jugular foramen (between occipital and temporal): see text |
| Medulla | XII | Hypoglossal canal (occipital) |
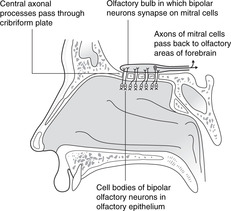
Olfactory nerve: I
The olfactory nerve is the nerve of smell. It transmits impulses from the olfactory epithelium of the nose to the brain and is described in more detail in section 14.9 (p. 279).
Optic nerve: II
The visual pathways are described in section 14.11 (p. 288).
Oculomotor nerve: III
The oculomotor nerve innervates muscles that move the eyeball and is described with the orbit and eyeball (section 14.11, p. 290).
Trochlear nerve: IV
The trochlear nerve innervates one of the muscles that move the eyeball and is described with the orbit and eyeball (section 14.11, p. 290).
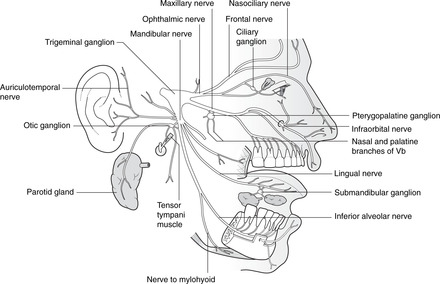
Trigeminal nerve: V (Fig. 14.10)
The trigeminal nerve conveys sensation from the face and anterior scalp, the oral and nasal cavities, the teeth and the meninges, and its mandibular division is motor to the eight muscles of the first branchial arch, known as the muscles of mastication.
 |
| Fig. 14.10 |
It arises from the pons and passes forwards to the trigeminal (sensory) ganglion in a slight depression on the petrous temporal bone. It then divides into the ophthalmic (Va), maxillary (Vb) and mandibular (Vc) nerves, each described separately below.
Clinical notes
• Shingles. The trigeminal ganglion, like all sensory ganglia, may harbour the herpes zoster virus causing shingles in the sensory distribution of the nerve. The virus may have been latent for years following chickenpox.
• Trigeminal neuralgia. This is severe pain in the distribution of one or more branches of V. Its cause is usually unknown and treatment difficult.
Ophthalmic nerve: Va
The ophthalmic nerve conveys sensation from the eyeball, the skin of the upper face and anterior scalp, the lining of the upper part of the nasal cavity and sinuses, and the meninges of the anterior cranial fossa.
Some peripheral branches convey parasympathetic fibres from elsewhere on their way to the ciliary and iris muscles, and the lacrimal gland.
Origin, course and branches.
From the trigeminal ganglion, Va passes in the lateral wall of the cavernous sinus and divides into the frontal (the largest), nasociliary and lacrimal (the smallest) branches, which pass through the superior orbital fissure into the orbit.
• Frontal nerve: supplies skin of forehead and scalp, and the frontal sinus. The nerve passes directly beneath the frontal bone and divides into supraorbital (larger, lateral) and supratrochlear (smaller, medial) nerves, which turn upwards at the supraorbital margin to the forehead and scalp.
• Nasociliary nerve: supplies the eyeball, upper part of the nasal cavity and neighbouring air cells, anterior nasal skin, and meninges. Its branches include:
– Long and short ciliary nerves conveying sensory fibres from the eyeball. They also convey parasympathetic impulses from III to the ciliary ganglion, and deliver postganglionic impulses to the ciliary body and constrictor pupillae.
– Anterior ethmoidal nerve, which supplies the upper part of the nasal cavity and associated sinuses. At the bridge of the nose it becomes superficial as the external nasal nerve supplying cutaneous sensation down to the nasal tip.
The ophthalmic nerve contains:
• Somatic sensory fibres: to the trigeminal sensory nuclei.
• In peripheral branches only, parasympathetic impulses from the Edinger–Westphal nucleus and III: to the ciliary ganglion (synapse) and eyeball (see p. 257).
• In peripheral branches only, parasympathetic impulses from the superior salivatory nucleus and pterygopalatine ganglion (synapse): to the lacrimal gland (see p. 257).
Clinical testing
• Test the cutaneous sensation of the forehead and anterior scalp.
• Corneal reflex. When the cornea is touched, usually with a wisp of cotton wool, the subject blinks. This tests Va and VII. The nerve impulses pass thus: cornea → nasociliary nerve → Va → principal sensory nucleus of V → brain stem interneurons → facial motor nucleus → VII → orbicularis oculi muscle. This reflex does not test II, III, IV or VI.
Maxillary nerve: Vb
The maxillary nerve conveys sensation from the malar skin (skin between lower eyelid and mouth), from the nasal cavity and sinuses, and from maxillary teeth. Some of its branches convey postganglionic fibres from the pterygopalatine ganglion to lacrimal, nasal and palatine glands.
Origin, course and branches
From the trigeminal ganglion, Va passes through the foramen rotundum to the pterygopalatine fossa where it divides into:
• Infraorbital nerve: to infraorbital skin, upper lip, maxillary sinus. This passes between orbit and maxillary sinus to emerge at the infraorbital foramen.
• Zygomatic nerve: enters the orbit through the inferior orbital fissure and divides into nerves that penetrate the zygoma to supply overlying skin. It also conveys postganglionic parasympathetic impulses from the pterygopalatine ganglion on their way to the lacrimal nerve and gland.
• Nasal branches: pass to the nasal cavity and sinuses. Branches also convey postganglionic impulses from the pterygopalatine ganglion to nasal glands.
• Greater and lesser palatine nerves: descend in similarly named canals to the palate. Branches also convey postganglionic impulses from the pterygopalatine ganglion to palatal glands.
• Superior alveolar (dental) nerves: pass directly through the maxilla to the maxillary teeth and sinus.
• Pharyngeal branch: passes posteriorly to the nasopharynx.
The nerve contains
• Somatic sensory fibres: to the trigeminal sensory nuclei.
• In peripheral branches only, parasympathetic impulses from the superior salivatory nucleus and VII: to lacrimal, nasal and palatal glands (see p. 235).
Clinical testing
Test the cutaneous sensation of the lower eyelid, cheek and upper lip.
Mandibular nerve: Vc
The mandibular nerve is a mixed sensory and motor nerve. It conveys sensation from:
• skin over the mandible, side of the cheek and temple
• oral cavity and contents including the anterior tongue
• external ear, tympanic membrane and temporomandibular joint
• meninges of the cranial vault.
It conveys motor fibres to the eight muscles derived from the first branchial arch:
• temporalis, masseter
• medial, lateral pterygoids
• mylohyoid, anterior belly of digastric
• tensor tympani, tensor palati.
As an aid to memory, note the four groups of two: 2 tensors, 2 pterygoids, 2 big chewing muscles, 2 in the floor of the mouth. These are sometimes known as the muscles of mastication, but this is misleading since effective mastication also requires muscles supplied by other nerves: buccinator (VII) and tongue (XII).
Some of the peripheral branches of Vc also convey parasympathetic impulses to the salivary glands, and taste fibres from the anterior portion of the tongue.
Origin, course and branches
• From the trigeminal ganglion, the mandibular nerve passes through the foramen ovale into the infratemporal fossa where it gives:
– branches to the muscles listed above.
• Inferior alveolar nerve: lower teeth, skin, mylohyoid, digastric. The inferior alveolar nerve passes between medial and lateral pterygoids and enters the mandibular foramen. It continues as the mental nerve emerging from the mental foramen of the mandible and supplies skin. Immediately before entering the mandibular foramen it gives the nerve to mylohyoid and anterior belly of digastric.
• Lingual nerve: tongue sensation. The lingual nerve passes between medial and lateral pterygoids and is joined by the chorda tympani, a nerve connecting the lingual nerve with VII. The lingual nerve is immediately below and medial to the third lower molar (wisdom) tooth and passes forwards in the floor of the mouth, crosses medially beneath the submandibular duct and supplies the anterior tongue and gums. Fibres it exchanges with the chorda tympani are taste fibres from the anterior tongue, and parasympathetic fibres to the submandibular ganglion.
• Auriculotemporal nerve: skin of temple, temporomandibular joint, external ear. The auriculotemporal nerve arises immediately beneath the foramen ovale by two rootlets ‘clasping’ the middle meningeal artery. It passes above (or through) the parotid gland, between the temporomandibular joint and the external acoustic meatus, and ascends on the side of the head close to the superficial temporal artery. For a short distance between its origin and the parotid gland it conveys parasympathetic impulses from the inferior salivatory nucleus to the otic ganglion for innervation of the parotid gland.
• Buccal nerve: skin and mucosa of cheek. The buccal nerve passes between the two heads of lateral pterygoid to the cheek. (It does not supply buccinator.)
• Muscular branches: deep temporal nerves to temporalis, and twigs to other muscles.
• Meningeal branches: branches in the infratemporal fossa re-enter the middle cranial fossa through the foramen ovale and other foramina.
The nerve contains
• Sensory fibres: to the trigeminal sensory nuclei.
• Branchiomotor fibres: from the trigeminal motor nucleus (pons).
• In peripheral branches only, taste fibres to the nucleus of the solitary tract: from the anterior portion of tongue via the lingual nerve, chorda tympani, VII.
• In peripheral branches only, parasympathetic impulses:
– from the superior salivatory nucleus and VII to the submandibular and sublingual glands (see p. 257)
– from the inferior salivatory nucleus and IX to the parotid gland (see p. 257).
First branchial arch
The mandibular nerve is the main nerve of the first branchial arch, which gives rise to a precursor of the mandible (Meckel’s cartilage), the spine of the sphenoid, the sphenomandibular ligament, the malleus and incus, and the eight muscles listed above. All these structures are related to mandibular nerve function in some way.
Clinical testing
• Sensory: test the cutaneous sensation of the chin and lower lip.
• Motor: feel the contractions of masseter and temporalis. Ask your patient to open the jaw against resistance (pterygoids, mylohyoid, anterior digastric).
Abducens nerve: VI
The abducens nerve innervates one of the muscles that move the eyeball and is described with the orbit and eyeball (section 14.11, p. 290).
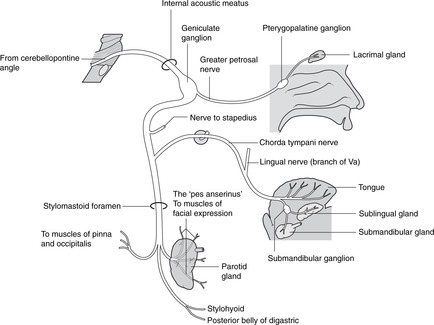
Facial nerve: VII (Fig. 14.11)
The facial nerve supplies the muscles of facial expression.
 |
| Fig. 14.11 |
Its intracranial portion also conveys:
• taste sensation from the anterior portion of the tongue and oral cavity, which is conveyed to the facial nerve by the chorda tympani
• parasympathetic fibres for the first part of their journey to the submandibular, sublingual, lacrimal, nasal and palatine glands.
Origin, course and branches
VII arises from the cerebellopontine angle by two adjacent roots, the motor root (larger, more medial) and the nervus intermedius (smaller, more lateral; sensory and parasympathetic fibres), so named because it is found between two larger nerves (the motor root of VII and VIII).
Intracranial course, within the cranial cavity and temporal bone
• The roots of VII enter the internal acoustic meatus (with VIII) and merge.
• The facial canal runs posteriorly along the medial wall of the tympanic (middle ear) cavity, and a branch passes to stapedius (attached to the stapes). The nerve turns downwards and laterally, and just before it emerges from the temporal bone it gives off the chorda tympani, which passes anteriorly across the tympanic membrane to the lingual nerve (Vc) in the infratemporal fossa.
• VII emerges at the stylomastoid foramen.
Extracranial course and branches
• Outside the stylomastoid foramen, small branches arise to supply the occipital belly of occipitofrontalis, stylohyoid and the posterior belly of digastric.
• VII enters the parotid gland in which it forms a plexus. Branches of VII are the most superficial structures passing through the gland.
• Five groups (usually) of branches emerge from the anterior border of the gland: temporal, zygomatic, buccal, mandibular and cervical. These supply the muscles of facial expression, including orbicularis oculi, orbicularis oris and buccinator.
The nerve contains:
• Branchiomotor fibres: from the facial motor nucleus.
• In the intracranial portion only, taste fibres to the solitary tract and nucleus: they carry taste sensation from the anterior portion of the tongue in the lingual nerve and gain the intracranial portion of VII through the chorda tympani.
• In the intracranial portion only, preganglionic parasympathetic impulses from the superior salivatory nucleus: to lacrimal, nasal and palatine glands, and to the submandibular and sublingual glands (see p. 257).
• Somatic sensory fibres: to the trigeminal sensory nuclei from a small and variable area of skin near or in the ear.
Second branchial arch, otic vesicle and facial nerve
Clinical notes
• The most important thing about the intracranial course of VII is its relationship to the temporal bone and middle ear. It can be affected in ear disease (see p. 285).
• The most important thing about the extracranial course of VII is its relationship to the parotid gland. It can be affected in parotid disease (see p. 266).
• Geniculate herpes. The herpes zoster virus may lie dormant in the geniculate ganglion (after chickenpox) and at a later stage cause a vesicular eruption in the small area of skin around the external acoustic meatus supplied by the facial nerve. There may also be signs on the anterior portion of the tongue because of involvement of taste fibres with cell bodies in the geniculate ganglion. The inflammation may spread to involve the motor fibres in VII, and a lower motor neuron lesion arising thus is known as Ramsay Hunt’s syndrome.
Clinical testing
• Observe the face. Normal facial movements (lips, eyelids, emotions) and the presence of normal facial skin creases indicate an intact nerve.
• Test strength by trying to force apart the tightly closed eyelids; this should be difficult.
• Test the corneal reflex; see Va above.
Vestibulocochlear nerve: VIII
The vestibulocochlear nerve is the nerve of equilibration (vestibular) and hearing (cochlear) and is described in section 14.10 (pp. 287–288).
Glossopharyngeal nerve: IX
The main function of the glossopharyngeal nerve is the sensory supply of the oropharynx, posterior third of the tongue, Eustachian tube and middle ear.
Its other functions are:
• motor to stylopharyngeus
• sensory from the middle ear, carotid sinus and carotid body
• conveying parasympathetic fibres part of the way to the parotid gland.
Origin, course and branches
• IX arises from the medulla by rootlets lateral to the olive, above those of X.
• It leaves the posterior cranial fossa through the jugular foramen. Superior and inferior sensory ganglia containing cell bodies of sensory fibres are situated in and near the jugular foramen.
• The tympanic branch is given off in the jugular foramen. This contains parasympathetic impulses from the inferior salivatory nucleus (for the parotid gland) and sensory fibres from the ear.
• IX descends in the neck giving a branch to the carotid body, then enters the pharynx between superior and middle constrictors. Branches contribute sensory fibres to the pharyngeal plexus.
The nerve contains
• Visceral sensory fibres: to the nucleus of the solitary tract.
• Branchiomotor fibres: from the nucleus ambiguus to stylopharyngeus.
• In the proximal part of the nerve only, parasympathetic impulses from the inferior salivatory nucleus: to the parotid gland (see p. 257).
Third branchial arch
The glossopharyngeal nerve is the nerve of the third branchial arch that gives rise to part of the hyoid bone and the stylopharyngeus muscle. Arterial components of the third arch form part of the common and internal carotid arteries, thus explaining the carotid sinus innervation.
Clinical testing
Gag reflex. Sensation supplied by the glossopharyngeal nerve is different in quality to that supplied by the trigeminal. Put your finger on the anterior part of your tongue (Vc) and then on the posterior part (IX) to demonstrate this. The gag reflex is mediated by IX (afferent limb) and X (efferent limb), so it tests both nerves.
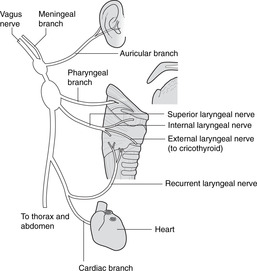
Vagus nerve: X (Fig. 14.12)
The vagus is a mixed motor and sensory nerve supplying the gut tube as far as the transverse colon. This includes the pharynx and larynx for swallowing and phonation, and these are its most important functions.
 |
| Fig. 14.12 |
It also supplies parasympathetic and sensory fibres to the heart, tracheobronchial tree and abdominal viscera, and conveys a few cutaneous sensory fibres from the posterior part of the external acoustic meatus and the tympanic membrane.
Origin, course and branches
The vagus is the most extensively distributed cranial nerve, its name reflecting both the distribution and the type of sensation it conveys (Latin: vagus = vague, indefinite, wandering).
• X arises from the medulla by rootlets lateral to the olive, below those of IX.
• It leaves the posterior cranial fossa through the jugular foramen. Superior and inferior sensory ganglia for cell bodies of sensory fibres are situated in and near the jugular foramen.
• The auricular branch passes through a canal in the temporal bone and conveys sensory fibres from the posterior part of the external acoustic meatus and tympanic membrane.
• X descends in the carotid sheath between the internal jugular vein and the carotid arteries. It gives pharyngeal branches, and the superior laryngeal nerve.
• Cardiac (slowing the heart rate) and tracheal (sensory) branches arise in the root of neck and upper thorax. It enters the thorax and, on the left side, crosses the arch of the aorta.
• Recurrent laryngeal nerves arise in the mediastinum: that on the left is related to the ligamentum arteriosum, that on the right to the subclavian artery. Both recurrent nerves re-ascend between the trachea and oesophagus to supply laryngeal muscles and give sensory fibres to the larynx below the vocal cords, the trachea and the oesophagus.
• The vagus forms the oesophageal plexus and enters the abdomen through the oesophageal hiatus in the diaphragm. See Chapters 10 and 11.
The motor function of the vagus in the neck is branchiomotor: in the thorax and abdomen it is parasympathetic.
• Branchiomotor fibres: from the nucleus ambiguus to pharyngeal and laryngeal muscles.
• Parasympathetic fibres: from the dorsal motor nucleus of vagus to the heart and thoracoabdominal viscera (foregut and midgut, see p. 257).
• Somatic sensory fibres: to the trigeminal sensory nuclei. From the posterior wall of the external acoustic meatus and the posterior portion of the external surface of the tympanic membrane, fibres pass in the auricular branch of X to the main trunk in the jugular foramen.
• Visceral sensory fibres: to the nucleus of the solitary tract from taste buds in the epiglottic area, visceral sensory fibres from gut tube derivatives and aortic baro- and chemoreceptors.
Fourth and sixth branchial arches
The vagus is the nerve of the fourth and sixth branchial arches. Structures derived from these include the pharyngeal and laryngeal cartilages and muscles. The sixth arch artery on the left gives rise to the ductus arteriosus (ligamentum after birth) around which the left sixth arch nerve, the recurrent laryngeal, is trapped in embryonic life. The sixth arch artery on the right degenerates, so the right recurrent laryngeal nerve is related to the most caudal persisting branchial arch artery, the fourth, which becomes the right subclavian.
An alternative view of the vagus
The vagus controls the entry into the gut tube (swallowing), and mediates sensation of most of the gut tube. This includes the bronchial tree, another gut tube derivative. The heart develops from cells initially found in the wall of the yolk sac, from which the gut tube develops. Sustenance is a common theme here, whether the absorption of nutrients from the yolk sac (gut tube) or their propulsion round the body by the force of cardiac contractions. Perhaps the ‘big picture’ is that the vagus is the nerve of sustenance – the yolk sac nerve.
Clinical testing
• If speech is normal, there is no need to test X at all since it supplies the muscles that move the vocal cords causing phonation.
• Say ‘aah’. Observing the elevation of the palate when a subject says ‘aah’ tests motor function in fibres from the nucleus ambiguus in X.
• Gag reflex – see IX above.
Accessory nerve: XI
The accessory nerve has two parts: cranial and spinal. Oddly enough, when clinicians refer to the eleventh cranial nerve, or accessory nerve, they mean the spinal accessory.
• Cranial accessory. This arises from a caudal extension of the nucleus ambiguus by rootlets below and in series with those of IX and X. It joins X, from which it is functionally indistinguishable (its name means accessory vagus). This book considers the cranial accessory no more and neither need you.
• Spinal accessory: this is the one to remember (Fig. 14.9). This is motor to the muscles bounding the posterior triangle of the neck: sternocleidomastoid and trapezius.
Origin and course: there are two foramina
• Rootlets from the upper four or five segments of the spinal cord (in series with those of IX, X and cranial XI) emerge between the ventral and dorsal spinal nerve roots.
• The spinal accessory ascends through the foramen magnum to enter the posterior cranial fossa and briefly runs with cranial XI before it (the cranial) joins the vagus.
• XI descends through the jugular foramen into the neck and passes deep to sternocleidomastoid, which it supplies.
• XI enters the posterior triangle of the neck about one-third of the way down the posterior border of sternocleidomastoid and passes across to enter trapezius about one-third of the way up its anterior border.
The nerve contains
• Motor fibres: cell bodies are in the lateral part of the ventral grey horn of cervical cord segments 1–5.
Clinical testing
• Ask your patient to move his chin up to one side against resistance (contralateral sternocleidomastoid).
• Ask your patient to shrug his shoulders (trapezius) against resistance.
• Ask your patient to put his hand on his head (trapezius: shoulder abduction beyond 90°).
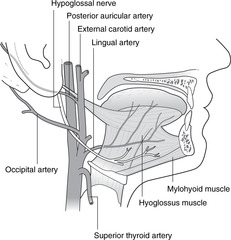
Hypoglossal nerve: XII (Fig. 14.13)
The hypoglossal nerve supplies the muscles of the tongue. Movements of the tongue are important in chewing, in the initial stages of swallowing, and in speech.
 |
| Fig. 14.13 |
It also conveys fibres from C1 which contribute to the innervation of the strap muscles.
Origin, course and branches
• It passes through the hypoglossal (condylar) canal in the occipital bone.
• It receives motor fibres from C1 and descends to the submandibular region.
• It turns forwards, lateral to the external carotid artery and hooks beneath the origin of the occipital artery.
• It gives a branch to the ansa cervicalis, which carries some fibres from C1 to the strap muscles; other C1 fibres remain with XII to supply geniohyoid.
• It enters the tongue from below passing lateral to hyoglossus and supplies the muscles of the tongue.
The nerve contains:
• Motor fibres: from the hypoglossal nucleus in the floor of the fourth ventricle in the medulla, to the tongue muscles.
Clinical testing
• Ask your patient to protrude the tongue. If it deviates to one side, then the nerve of that side is damaged – the tongue is pushed to the paralysed side by muscles of the functioning side.
• Ask the patient to push the tongue into the cheek, then palpate the cheek to feel tone and strength of tongue muscles.
Parasympathetics and taste in cranial nerves
Parasympathetic and taste components in cranial nerves, although one is efferent and the other afferent, share some peripheral pathways connecting branches of one cranial nerve to another (e.g. chorda tympani, petrosal nerves). These pathways provide material for nit-picking examinations, and are of embryological interest, but from a functional point of view they are insignificant. They may have to be interrupted, for example in ear surgery, and although food and drink may lose some savour, and the patient may subsequently suffer from a dry mouth, this could never be described as life-threatening.
Parasympathetic components (Fig. 14.14)
• Edinger–Westphal nucleus–III–ciliary ganglion (synapse)–branches of Va–iris, ciliary body.
• Superior salivatory nucleus–VII–greater petrosal nerve–pterygopalatine ganglion (synapse)–branches of Vb–lacrimal, nasal, palatine glands.
• Superior salivatory nucleus–VII–chorda tympani–submandibular ganglion (synapse)–branches of Vc–submandibular, sublingual glands.
• Inferior salivatory nucleus–IX–lesser petrosal nerve–otic ganglion (synapse)–branches of Vc–parotid gland.
• Dorsal motor nucleus of the vagus–X–gut tube derivatives and heart (synapses in or near destination).
Taste fibres (Fig. 14.15)
• Taste sensation from palate–branches of Vb–greater petrosal nerve–VII (cell bodies in geniculate ganglion)–solitary tract of brain stem.
• Taste sensation from anterior tongue and mouth–branches of Vc–chorda tympani–VII (cell bodies in geniculate ganglion)–solitary tract of brain stem.
• Taste sensation from posterior tongue–IX (cell bodies in sensory ganglia of IX)–solitary tract of brain stem.
• Taste sensation from pharynx–X (cell bodies in sensory ganglia of X)–solitary tract of brain stem.
Clinical testing
• Pupillary light reflex: this tests parasympathetic fibres from the Edinger–Westphal nucleus (see section 14.11, pp. 294, 295).
• Salivary glands. Ask your patient to suck something bitter (e.g. a lemon) to provoke salivary secretion. This is more usually done to try to locate the position of a calculus in the duct of a salivary gland, usually the submandibular.
• Taste. Testing taste is possible but hardly worth the trouble.
14.5. Neck
Fascial sheets surround various structures in the neck and are important in the spread of disease. Bones and cartilages in the anterior neck form the visceral skeleton of the larynx. Arteries and veins travel anterior to, or through the vertebral column. The neck is divided into posterior and anterior triangles.
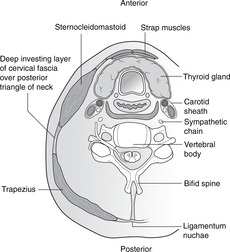
Fascial layers (Fig. 14.16)
• The investing layer of cervical fascia encloses the deep structures like a sleeve. It is attached posteriorly to the nuchal ligament and splits around trapezius and sternocleidomastoid. Cutaneous nerves are superficial to it.
• The carotid sheath is a vertical fascial tube deep to the investing layer of fascia. It contains the common and internal carotid arteries, the internal jugular vein, the vagus nerve and the deep cervical chain of lymph nodes.
• The prevertebral ‘space’ is the area between the prevertebral muscles and the pharynx/oesophagus containing loose connective tissue and lymph nodes. It allows disease to spread from one side of the neck to the other. The cervical sympathetic chain is found here, immediately posterior to the carotid sheath.
• The pretracheal fascia in front of and to the sides of the trachea encloses the thyroid gland and with the investing layer of cervical fascia anteriorly forms sheaths around the strap (infrahyoid) muscles of the neck.
• Platysma muscle is directly subcutaneous. When it contracts it raises ridges in the skin of the neck and is useless except for those who shave. It is supplied by VII and is a now-redundant muscle of ‘facial’ expression.
 |
| Fig. 14.16 |
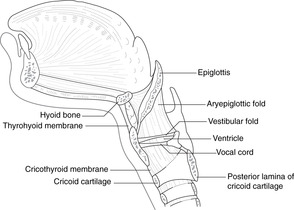
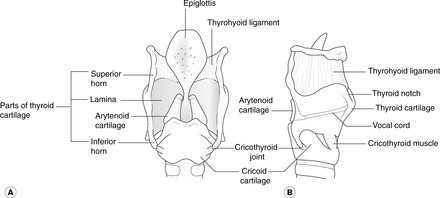
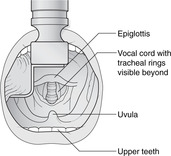
Visceral skeleton of the neck
• Hyoid bone. This is palpable immediately underneath, almost inside, the mandible at the top of the neck. The greater horns (cornua) extend backwards from the sides of the body (be careful when palpating these – too much pressure will fracture the bone).
• Thyroid cartilage. Right and left laminae join in the midline to form the thyroid prominence or Adam’s apple. Superior horns extend up towards the hyoid bone, and inferior horns articulate with the cricoid cartilage below.
• Cricoid cartilage. This is a cartilaginous ring at the top of the trachea. It has a lamina posteriorly and facets for synovial joints with the inferior horns of the thyroid cartilage at the sides.
• Membranes attach these cartilages to each other so that they move as one.
– thyrohyoid membrane, palpable between hyoid bone and thyroid cartilage
– cricothyroid membrane, palpable between thyroid and cricoid cartilages. Laryngotomy is performed here.
Vertebral levels of the visceral skeleton of the neck
Despite movement during swallowing, these vertebral levels are worth remembering:
• hyoid bone: about C2
• thyroid cartilage, upper margin of lamina (surface marking of bifurcation of common carotid artery): about C3
• vocal cords: about C4
• thyroid cartilage, lower margin of lamina: about C5
• cricoid cartilage (surface marking of beginning of trachea and oesophagus): C6.
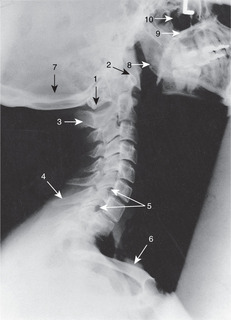
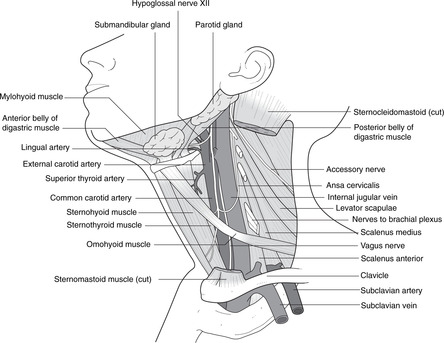
Arteries of the neck (Figs 14.17, 14.18)
 |
| Fig. 14.17 |
Internal carotid artery
This has no branches in the neck, but enters the skull through the carotid canal. It is called internal because it passes into the cranium, not because of its position in the neck.
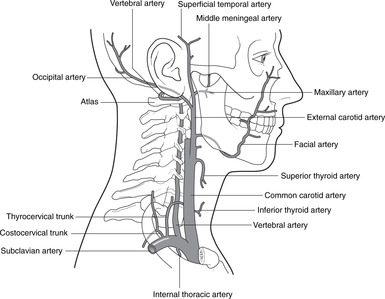
External carotid artery (Fig. 14.18)
This gives branches as follows:
• Superior thyroid: to thyroid gland, larynx, pharynx. This may arise from the bifurcation or even from the common carotid artery.
• Ascending pharyngeal (not important).
• Lingual: to the tongue.
• Facial: to the face. The lingual and facial may arise by a common trunk.
• Occipital: to the back of the head. The occipital comes off the posterior border at about the same level as the lingual and facial arise anteriorly, and at its origin is intimately related to XII.
• Posterior auricular: to the region around the ear.
• The two terminal branches, arising behind the neck of the mandible, are:
– superficial temporal: to the side of the head and scalp, usually visible and palpable
– maxillary: to the mandible, maxilla, cheek, nasal cavity, skull bones and cranial meninges.
Carotid pulse
Press posteriorly lateral to the upper border of the thyroid cartilage. You are compressing the common carotid artery against the anterior aspect of the transverse process of vertebra C3. Do not push too hard, and do not palpate both sides together.
Superficial temporal pulse
Place your fingers about 2 cm above the middle of a line joining the top of the pinna to the side of the orbit.
Vertebral artery
This is a branch of the first part of the subclavian artery. It ascends through the foramina transversaria of vertebra C6 (usually) to C1, then turns medially, grooving the upper surface of the atlas behind the atlanto-occipital joint facet, pierces the meninges and enters the subarachnoid space. It passes through the foramen magnum, ascends on the anterior aspect of the brain stem and unites with its opposite number to form the basilar artery.
• Branches in the neck supply deep neck structures and give twigs through intervertebral foramina to the spinal cord.
• Branches in the cranium supply the spinal cord, brain stem, vital centres, vestibular apparatus and the posterior cerebral cortex.
Veins of the neck
Internal jugular vein
This emerges from the jugular foramen of the skull and descends in the carotid sheath with the common carotid artery and X. It terminates behind the sternoclavicular joint where it joins the subclavian to form the brachiocephalic vein. It receives tributaries from the face and thyroid gland.
External jugular vein
This is formed behind the angle of the mandible from superficial veins of the face and passes obliquely towards the midpoint of the clavicle. It receives tributaries from superficial neck tissues and terminates by joining the subclavian vein either directly or indirectly.
Anterior jugular veins
These are situated near the medial (anterior) border of sternocleidomastoid and form a venous arch that drains to the brachiocephalic veins.
Surface markings of neck veins
• Internal jugular: ear lobe (roughly)–sternoclavicular joint. It is deep to sternocleidomastoid, so is neither visible nor palpable.
• External jugular: angle of mandible to midpoint of clavicle. This is superficial and is visible throughout its length.
Jugular venous pulsation
A routine part of the examination of the cardiovascular system is an assessment of jugular venous pulsation. The height of the column of blood in the jugular veins reflects pressure changes in the right side of the heart. The internal jugular veins are more accurate in this respect than the external as there are no valves between the right atrium and internal jugulars. In a healthy person the top of the column of blood should be at the sternal angle although the pulsations may be just visible above the clavicle. In heart failure the column of blood will be taller, so the pulsations will be visible higher than normally. In superior vena cava obstruction the pulsations will be lost and the vein will be engorged. Exaggerated pulsations will be visible in tricuspid disease.
Words: jugular, carotid
Veins are jugular (Latin: throat, yoke); arteries are carotid (Greek: drowsiness). Compression of the arteries for long enough would certainly cause something like drowsiness: this method of inducing anaesthesia was prevalent before drugs were introduced for this purpose.
Nerves of the neck
See dermatome map (see Fig. 6.6, p. 36).
• Posterior skin is supplied by dorsal rami of cervical nerves.
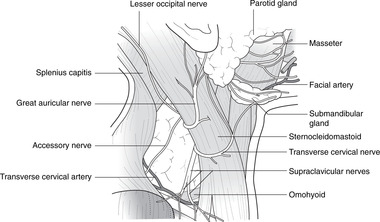
Cervical plexus C2–4
• Sensory branches emerge from behind the central region of the posterior border of sternocleidomastoid. They are:
– lesser occipital (C2, 3)
– great auricular (C2, 3)
– transverse (or anterior) cutaneous of the neck (C2, 3)
– supraclavicular nerves (C3, 4), passing down and laterally over the clavicle to meet the dermatome of T2 over the second rib (C5–T1 dermatomes are in the upper limb)
– branches to the phrenic nerve C3–5 for thoracic viscera and central diaphragmatic sensation.
• Muscular branches:
– to the phrenic nerve C3–5 for the diaphragmatic muscle
– to the strap (infrahyoid) muscles attached to the hyoid bone and thyroid cartilage. Fibres from C1 travel briefly with XII, and then join fibres from C2 and C3 to form the ansa cervicalis, which supplies the strap muscles. It may have to be cut in surgery: we can live without both it and the muscles it supplies
– from C4 to levator scapulae, rhomboids, etc., of no clinical importance.
Posterior triangle of the neck (Fig. 14.19)
 |
| Fig. 14.19 |
Boundaries
• Posterior border of sternocleidomastoid
• Anterior border of trapezius
• Middle portion of clavicle.
The apex of the triangle is at the mastoid process. The external jugular vein and supraclavicular nerves run over the triangle, and deep to them the roof of the triangle is formed by the investing layer of cervical fascia between sternocleidomastoid and trapezius.
Contents
• Upper trunk of the brachial plexus inferomedially
• Apex of the lung extending above the middle third of the clavicle for about 2 cm.
• Lymph nodes around the edges of the triangle
• Accessory nerve (XI). Its approximate surface markings are: one-third of the way down sternocleidomastoid to two-thirds of the way down trapezius.
At risk in the posterior triangle:
• The accessory nerve (XI) is easily damaged and is at risk in malignant involvement of lymph nodes, careless biopsy of enlarged lymph nodes, and stab wounds. It would result in weakness of trapezius with impaired shoulder abduction, leading to difficulty in hair grooming, etc.
• Stab wounds may damage the brachial plexus (upper trunk injury leading to Erb’s palsy) and the apex of the lung (leading to a pneumothorax).
Anterior triangle of the neck
Boundaries
Contents
• Superficial: anterior jugular veins, cutaneous branches of cervical plexus.
• Strap muscles: thyrohyoid, sternohyoid, sternothyroid, omohyoid. Nerve supply: cervical plexus C1–3 through ansa cervicalis. Their names give their attachments, omo- (Greek: shoulder) -hyoid coming from the upper border of the scapula just medial to the scapular notch. Sternohyoid overlies both sternothyroid and thyrohyoid; sternothyroid is immediately anterior to the thyroid gland.
• Larynx and trachea (described in section 14.8, p. 273).
• Thyroid gland.
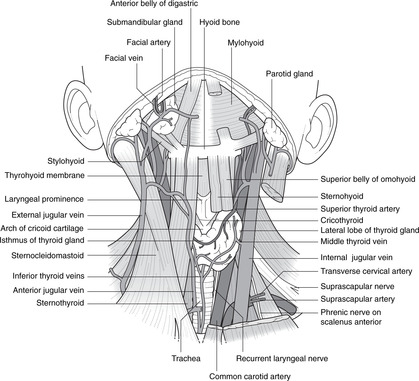
Thyroid gland (Fig. 14.20)
The thyroid gland has two lateral lobes and a central isthmus. The isthmus overlies tracheal rings 2–4 and the lateral lobes extend up to about the middle of the thyroid cartilage. Note that the bulk of the thyroid gland is significantly lower than the thyroid cartilage.
 |
| Fig. 14.20 |
Relations, enlargement of the thyroid gland
The thyroid gland is enclosed within the pretracheal fascia, and immediately above the gland, thyrohyoid muscle is attached to the thyroid cartilage. This means that when the gland enlarges (goitre) its expansion above is limited by this attachment. At the sides, expansion is limited by the fusion of the pretracheal fascia with the carotid sheath, so that apart from some generalised swelling, gross enlargements of the gland expand inferiorly where there is nothing to stop the gland growing down into the mediastinum (mediastinal goitre). Such mediastinal masses may compress the jugular and brachiocephalic veins leading to venous engorgement of the neck and face.
Arteries
• Inferior thyroid: from the thyrocervical trunk of the first part of the subclavian artery. It loops behind the carotid sheath before turning upwards once more to branch as it enter the lower pole of the lateral lobe.
• Superior thyroid: from the external carotid artery.
The territories of both arteries communicate with each other and across the midline with their opposite numbers. There is often a posterior anastomotic artery between branches of the superior and inferior thyroid arteries.
• Thyroidea ima artery: from the brachiocephalic artery or aortic arch; infrequent (less than 10%).
Relationship of arteries to the laryngeal nerves
• The superior thyroid artery is closely related near its origin to the superior laryngeal nerve (branch of X). Section of the nerve would anaesthetise the laryngeal mucosa and abolish the cough reflex, so increasing the risk of food or a foreign body entering the trachea.
• The inferior thyroid artery is closely related to the recurrent laryngeal nerve (branch of X) as it enters the gland. Section of this would result in paralysis of the muscles that move the vocal cords on that side. Any patient for thyroid surgery should have the vocal cords inspected beforehand so that, in the event of any suspicion of the surgeon having damaged the nerve during surgery, there is a record of their preoperative state.
Veins
• Inferior thyroid veins: numerous vessels drain into the brachiocephalic veins.
• Middle and superior thyroid veins, usually one each on each side, pass anterior to the common carotid artery and drain into the internal jugular vein.
Development, thyroglossal cysts, ectopic thyroid tissue
The thyroid gland develops as an exocrine downgrowth from the foramen caecum of the tongue, its duct, the thyroglossal, closing with increasing vascularisation of the gland. The attachment of the duct to the gland may be marked by a pyramidal lobe on the upper aspect of the isthmus. Ectopic thyroid tissue can be found at the foramen caecum (lingual thyroid) or along the course of the duct. Thyroglossal cysts may develop in the track of the duct and cause sufficient trouble for them to require excision. In such cases it is usually necessary to remove the central part of the hyoid bone as well, since the thyroglossal duct may be attached to its posterior surface before continuing its downwards journey.
How do you distinguish between a thyroglossal cyst and, say, a sebaceous cyst that just happens to be in the midline? The thyroglossal cyst will be pulled up when the patient swallows or protrudes the tongue.
Parathyroid glands
There are usually two small parathyroid glands on each side, but their position is not constant. The superior parathyroids are on, or in, the posterior surface of the lateral lobes of the thyroid gland, often somewhere near the anastomotic artery joining the inferior and superior thyroid arteries. The inferior parathyroids are close to the lower pole of the thyroid gland and supplied by branches of the inferior thyroid artery.
14.6. Face, parotid, VII, scalp
Muscles of facial expression are supplied by VII. This is intimately related to the parotid gland on the side of the face. Sensory nerves of the face and anterior scalp are branches of V; those of the posterior scalp are from spinal nerve C2. Vessels and nerves of the scalp are superficial to the epicranial aponeurosis, and bleeding after scalp injuries is usually profuse.
You should:
• explain how and why diseases of the parotid gland can affect VII
• list the principal muscle groups supplied by VII
• describe the main cutaneous nerves supplying the face and scalp
• explain why scalp injuries bleed profusely, and why they may result in subaponeurotic haematomas and black eyes.
Muscles of facial expression
The muscles of facial expression are attached to the deeper layers of the skin. They mimic emotion and so are called the mimetic muscles, and they are used in speech and for eye protection. They are all supplied by the facial nerve (VII).
There are many individual muscles, some with charming names, but it is not necessary to know most of them. Think of them collectively as the muscles of facial expression, and know the names of:
• orbicularis oculi
• orbicularis oris
• buccinator.
(You have already met platysma: it is unimportant.)
Some muscles supplied by VII remain deep, attached to the temporal bone, and are involved in movements of the pharynx: posterior belly of digastric (mastoid process–hyoid–mandible); stylohyoid (styloid process–hyoid).
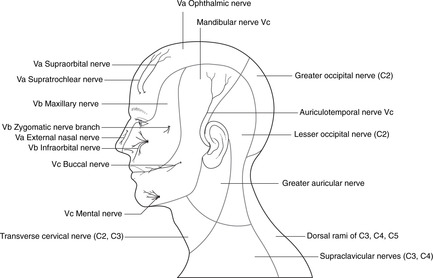
Cutaneous innervation of the face (Fig. 14.21)
 |
| Fig. 14.21 |
Note the following:
• Eyes and above: Va.
• Between palpebral fissure and mouth, and malar (over the cheekbone) skin: Vb.
• Chin and ‘beard area’ except skin over the angle of the mandible: Vc (from top down: auriculotemporal, buccal, and mental branches).
• Neck, skin over angle of mandible and area between ‘beard area’ and ear: cervical plexus C2, 3.
Miscellanea
• Trauma to the infraorbital margin may cause sensory loss in infraorbital skin as a result of damage to the infraorbital nerve (branch of Vb).
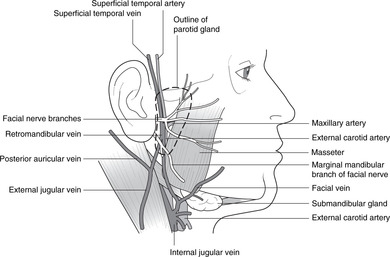
Parotid gland and VII (Fig. 14.22)
The parotid salivary gland lies at the side of the face behind the mandible, which it may overlap. It lies superficially and parotid swellings (e.g. mumps, tumours) produce an obvious retromandibular bulge. It is partially enclosed by the investing layer of cervical fascia, the superficial layer fusing with the fascia over masseter, and the deep layer having a free anterior edge (known misleadingly and inaccurately as the stylomandibular ligament).
 |
| Fig. 14.22 |
The parotid duct emerges from the anterior border of the gland and passes forwards on masseter. It then turns medially, penetrates buccinator and opens into the mouth opposite the second upper molar tooth. The duct is found by palpating the anterior border of a tensed masseter. Detached islands of secretory tissue may be found scattered along the duct.
Other structures that pass through the substance of the gland are the retromandibular vein, the auriculotemporal nerve and the termination of the external carotid artery (sometimes).
Parasympathetic supply
Secretomotor impulses to the gland come from the inferior salivatory nucleus and travel by way of IX, the lesser petrosal nerve and the otic ganglion (see p. 257 and Fig. 14.14).
Facial nerve
The single most important thing about the parotid gland is its relationship to the branches of the facial nerve. The single most important thing about the extracranial facial nerve is its relationship to the parotid gland.
The facial nerve emerges from the skull at the stylomastoid foramen in the temporal bone, behind the ear. It immediately turns forwards and superficially to enter the parotid gland in which it forms a complex and variable plexus. It is superficial in the gland. This means that the nerve is liable to damage (trauma, parotid tumour) leading to a facial palsy.
Branches of VII emerge from the anterior margin of the gland usually in five groups, the pattern being known as the pes anserinus (Latin: foot of the goose):
• zygomatic: to orbicularis oculi and upper face
• buccal: to buccinator, orbicularis oris and mid-face
• marginal mandibular: to orbicularis oris and the corner of the mouth
• cervical: to platysma.
Watch out particularly for the marginal mandibular nerve that passes on or just below the lower margin of the mandible. It is superficial even to the palpable facial pulse, and is thus liable to injury from, for example, trauma or careless incisions. Damage would result in weakness of the muscles of the corner of the mouth resulting in drooling of saliva.
Facial palsy, Bell’s palsy
A lower motor neuron lesion of VII is called a facial palsy. It may be a lesion of the cell bodies in the facial motor nucleus, or of the nerve itself, and the muscle fibre(s) supplied by the affected neuron(s) will be paralysed. Facial wrinkles disappear, and there will be facial asymmetry so it is usually easy to spot. Bell’s palsy is a facial palsy of unknown cause.
Facial nerve in the newborn baby
The mastoid process is almost non-existent in a newborn baby and the stylomastoid foramen is superficial. The facial nerve may be damaged here as a result of manipulation of the baby’s head during birth. This is serious: VII supplies buccinator, which the baby needs for feeding.
Frey’s syndrome
After parotidectomy, cut ends of postganglionic parasympathetic fibres begin to grow. If these sprouting fibres find their way into Schwann cells sheaths occupied before surgery by sympathetic fibres, stimuli normally producing salivation will instead induce sweating over the site of the parotid.
Scalp
The layers of tissue forming the scalp are:
• skin
• connective tissue containing vessels and nerves
• aponeurosis of occipitofrontalis muscle (epicranial aponeurosis or galea aponeurotica)
• loose areolar tissue.
Add the ‘p’ for periosteum of the cranial bones and the initial letters spell ‘scalp’. The areolar tissue gives a natural cleavage plane between the aponeurosis and the bone.
Occipitofrontalis muscle and its aponeurosis
This forms a helmet over the vault of the skull. Occipital muscle fibres are attached to the superior nuchal line, and anteriorly, frontalis is attached to the skin of the forehead: these fibres crease the skin. Laterally, the aponeurosis is attached to the superior temporal line, and some people have muscles fibres here so are able to wiggle their pinnas. The muscle fibres are supplied by VII: occipitofrontalis is a mimetic muscle.
Vessels and cutaneous nerves of the scalp
These are in the connective tissue layer, superficial to the aponeurosis.
• Arterial blood. There is a profuse supply to the scalp from:
– the supraorbital artery from the orbit (a branch of the ophthalmic and internal carotid)
– branches of the external carotid artery at the sides and back, in order from the front: superficial temporal, posterior auricular, occipital.
The rich anastomosis means that scalp wounds bleed profusely, and from the point of view of the casualty officer trying to stem the flow, this is not helped by the tension exerted on the margins of the wound by occipitofrontalis pulling in both directions at once.
• Venous blood drains externally to internal and external jugular veins (see above) and by connections through the orbit, diploic cavities and elsewhere to intracranial venous sinuses.
• Cutaneous nerves of the scalp (see Fig. 14.21):
– anterior to the vertex: Va (supraorbital and supratrochlear branches)
– posterior to the vertex: greater occipital nerve, dorsal ramus of C2
– at the sides there are small areas supplied by: zygomatic (Vb), auriculotemporal (Vc) and lesser occipital (C2, 3 from cervical plexus) nerves.
Supraorbital injury
Trauma to the supraorbital margin or frontal bone may damage the supraorbital and/or supratrochlear nerves causing sensory loss in the scalp.
Temporal fascia
This is attached to the superior temporal line. It is tough and may be used for fascial grafts elsewhere in the body.
14.7. Anatomy of mastication
Movements of mastication occur at the temporomandibular joint. Muscles of mastication are supplied by Vc. The infratemporal fossa, deep to the mandible, contains the maxillary artery and some of these muscles. Sensory nerves to the oral cavity are branches of Vb and Vc. Muscles on the tongue are supplied by XII and it receives sensory fibres through Vc and IX. The submandibular and sublingual glands are in the floor of the mouth. The tonsils are at the posterior limit of the oral cavity, at the oropharyngeal isthmus.
You should:
• describe how the mandible moves, and the nerve supply of the muscles that move it
• describe which other muscles are required for chewing
• describe the sensory innervation of the oral cavity and teeth
• describe the innervation and lymph drainage of the tongue
• describe the position of the submandibular and sublingual salivary glands
• describe the position and significance of the tonsils.
Temporomandibular joint and mandibular movements
The temporomandibular joint is divided into two separate synovial cavities by a fibrocartilaginous disc. The sensory supply to the joint comes from the auriculotemporal nerve (Vc), which is why pain from the joint, like that from the teeth and tongue, can be referred to the skin of the external acoustic meatus and tympanic membrane (they are all supplied in whole or in part by branches of Vc).
The mandibles are tethered by the attachment of the sphenomandibular ligament extending from the spine of the sphenoid to the lingula of the mandible, and the two mandibles move by pivoting on an axis passing through the lingula, adjacent to the mandibular foramen on each side.
As the mouth opens, the head of the mandible moves forwards, and this is how lateral pterygoid acts as a depressor of the mandible: it exerts forward traction on the head, neck and joint capsule. You will be able to deduce what happens when the mandible closes. Protraction is the action that results in the entire mandible being pulled anteriorly; retraction is the opposite. Masticatory movements involve mandibular depression, elevation, protraction, retraction and side-to-side grinding.
Muscles (Fig. 14.23)
• Temporalis. Attachments: a wide area of temporal bone and fascia–coronoid process and anterior border of ramus of mandible, passing deep to the zygomatic arch.
• Masseter. Attachments: zygomatic arch–lateral aspect of angle of mandible.
• Lateral pterygoid. Attachments: lateral side of lateral pterygoid plate of sphenoid–head and neck of mandible, joint capsule, articular disc. It is a ‘front-to-back’ muscle.
• Medial pterygoid. Attachments: medial side of lateral pterygoid plate of sphenoid–medial aspect of angle of mandible. It is a ‘top-to-bottom’ muscle.
• Mylohyoid. Attachments: mylohyoid line on medial aspect of mandible–median raphe between hyoid bone and midpoint of posterior surface of mandible.
• Digastric, anterior belly. Attachments: hyoid–digastric fossa of mandible; below mylohyoid.
These muscles are all supplied by Vc.
Movements
• Elevation. The mandible is suspended from the skull by a muscular sling formed internally by medial pterygoid and laterally by masseter. From directly above, temporalis is a powerful elevator of the mandible.
• Depression. This is brought about in two ways:
– by anterior traction on the head of the mandible by lateral pterygoid
– by inferior traction on the mandible by the anterior belly of digastric and mylohyoid.
• Grinding. Lateral and rotatory movements are produced by muscles of the two sides working cooperatively. For example, moving the mandible to the left involves the left masseter and the right medial pterygoid.
• Protraction: lateral pterygoid, anterior fibres of temporalis.
• Retraction (not powerful): posterior fibres of temporalis.
Infratemporal fossa (Fig. 14.23)
The area beneath and in front of the temporal bone, bounded also by the ramus of the mandible, the maxilla and the pterygoid plates of the sphenoid, is the infratemporal fossa. It contains the pterygoid muscles and venous plexus, and branches of Vc and the maxillary artery.
Mandibular nerve
The mandibular nerve enters the roof of the fossa through the foramen ovale. The inferior alveolar and lingual nerves descend between the two pterygoid muscles, and the buccal nerve aims laterally for the skin of the cheek, passing between the two heads of lateral pterygoid. From its origin at the foramen ovale, the auriculotemporal nerve passes laterally directly underneath the skull. In the fossa, the chorda tympani emerges from the temporal bone and joins the posterior aspect of the lingual nerve.
Maxillary artery, pterygoid venous plexus
• The maxillary artery is one of the terminal branches of the external carotid artery and arises posterior to the neck of the mandible. It runs medially and forwards, and disappears medially through the slit between the lateral pterygoid plate of the sphenoid and the maxilla, the pterygomaxillary fissure (see below). It has several branches, the two most important being:
– the middle meningeal, which ascends to the foramen spinosum (usually passing between the roots of the auriculotemporal nerve)
– the inferior alveolar, which joins the nerve of the same name and enters the mandibular foramen.
• The pterygoid venous plexus in and around lateral pterygoid communicates with facial veins superficially and through skull foramina with intracranial venous sinuses.
Fissure, fossa, foramen …
Pterygopalatine fossa
The relations of the pterygopalatine fossa are as follows: the maxillary sinus is anterior, the inferior orbital fissure is anterosuperior, the nasal cavity is medial, the foramen rotundum (Vb enters here) and the pterygoid canal are posterior, the infratemporal fossa is lateral (the maxillary artery enters here) and the palatine canals are inferior. In the fossa the maxillary nerve and artery divide into their terminal branches. These pass to:
• the nose
• the maxillary sinus and skin of the cheek
• upper teeth
• palate
• nasopharynx.
Pterygopalatine ganglion
The pterygopalatine fossa also contains the pterygopalatine ganglion, a parasympathetic ganglion on the pathway from the superior salivatory nucleus to nasal, palatine and lacrimal glands (Fig. 14.14). The ganglion is attached to one or more branches of the maxillary nerve and because of this you might be misled into thinking that it is an integral part of the maxillary nerve. It is not: any sensory fibres belonging to the maxillary nerve that approach the ganglion, for example those from the palate, pass through the ganglion without taking any part in its morphology. It is purely a parasympathetic ganglion that has attached itself to branches of the maxillary nerve for the convenience of distributing its postganglionic fibres. It receives preganglionic fibres from the nerve of the pterygoid canal (from the superior salivatory nucleus and VII).
Mouth (Fig. 14.24)
• The vestibule is the area external to the teeth and gums. The midline fold between the inner aspect of the upper lip and gum is the frenulum.
• The oral cavity is the area internal to the teeth, alveolar processes and gums. The midline fold between the inner aspect of the lower gum and the tongue is the frenulum of the tongue.
• The muscles of the wall of the mouth are:
– orbicularis oris, which forms the oral sphincter
– buccinator, which forms the muscle of the cheek.
These are muscles of facial expression and are supplied by VII.
Buccinator is attached posteriorly to the pterygomandibular raphe, which is attached to the hamulus of the sphenoid and the mandible just behind the third lower molar tooth.
• The parotid duct opens opposite the second upper molar tooth. The submandibular duct opens on either side of the frenulum of the tongue and the sublingual ducts open nearby.
• The sensory innervation of buccal skin and mucosa is from branches of Vc, particularly the buccal.
• The arterial supply is from branches of the external carotid, particularly the facial, and venous drainage is to the facial vein and tributaries of the external jugular.
Teeth
• The primary or ‘milk’ dentition. In each half jaw there are 2 incisors, 1 canine, 2 molars. The first to erupt is the medial incisor at about 7 months, and the last at 2 years is the second molar.
• The adult dentition. In each half jaw there are 2 incisors, 1 canine, 2 premolars and 3 molars. The first to erupt is the first molar at about 6 years, the penultimate is the second molar at about 12 years, and the last the third molar in early adulthood as the mandible is settling down to its full size.
• The arterial supply to the teeth is from superior and inferior alveolar branches of the maxillary artery.
• The sensory innervation of the teeth:
– maxillary teeth: superior alveolar nerves (Vb)
– mandibular teeth: inferior alveolar nerve (Vc).
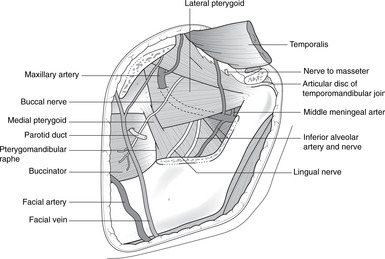 |
| Fig. 14.24 |
Tongue and floor of the mouth (Fig. 14.25)
The tongue has two parts: the oral, or anterior two-thirds; and the pharyngeal, or posterior one-third. The boundary is the sulcus terminalis, visible on the dorsum (superior surface) of the tongue as a V-shaped sulcus with its apex pointing backwards. The foramen caecum, at the apex of the sulcus, marks the site of origin of the thyroglossal duct forming the thyroid gland.
The anterior portion of the tongue is covered by papillae of various shapes. The posterior part has lymphoid follicles, often visible, which are parts of Waldeyer’s ring of lymphoid tissue guarding the oropharyngeal isthmus, and large circumvallate papillae arranged in line with and in front of the sulcus terminalis. Taste buds are present in all areas.
Muscles of the tongue
• Intrinsic muscles alter the shape of the tongue.
• Extrinsic muscles move the tongue bodily:
– hyoglossus, attached to the length of the greater horn of the hyoid bone
– genioglossus, attached to the mandible; and
– styloglossus, attached to the styloid process.
If the extrinsic muscles are paralysed, the tongue falls back and may block the airway.
Nerves of the tongue
• Motor to all tongue muscles: hypoglossal nerve (XII). It descends in the neck to the level of the hyoid bone, then passes lateral to the internal carotid artery hooking under the origin of the occipital artery. It approaches the tongue from below and passes lateral to hyoglossus.
• Motor to anterior belly of digastric and mylohyoid: Vc.
• Sensory innervation of the anterior two-thirds of the tongue:
– ‘ordinary’ sensation (tactile, pain, temperature, etc.): lingual nerve (branch of Vc), with cell bodies in the trigeminal ganglion
– taste sensation: lingual nerve, chorda tympani, VII, with cell bodies in the geniculate ganglion (of VII).
• Sensory innervation of the posterior one-third of the tongue: IX for all types of sensation, with cell bodies in the sensory ganglion of IX. The quality of sensation from this area is different from that in the anterior portion: anything more than a brief touch elicits the gag reflex (see p. 254).
• For sensory innervation, the boundary between the anterior two-thirds and posterior one-third is an imaginary line in front of the circumvallate papillae, which are supplied by IX.
• The lingual nerve (branch of Vc), having descended between the pterygoid muscles, where it is joined by the chorda tympani, lies adjacent to the third lower molar tooth.
– In the floor of the mouth the submandibular ganglion is attached to the nerve, which then enters the tongue lateral to hyoglossus.
– The lingual nerve passes forwards from lateral to medial under the submandibular duct.
Arteries
Arterial blood comes from the lingual artery, which enters the tongue from behind, lateral to hyoglossus.
Lymph drainage of the tongue
• From the tip: to submental nodes, in the midline below the middle of the mandible.
• From the body: to submandibular nodes, with the midline portion of the tongue draining to both sides.
• From the posterior third: to the deep cervical chain.
The message is: if you have a patient with a tongue tumour, check the nodes on both sides of the neck.
Submandibular and sublingual glands (Fig. 14.25)
The submandibular salivary gland lies beneath and medial to the angle of the mandible. The posterior border of mylohyoid indents the anterior surface of the gland, partially dividing it into superficial (below) and deep (above) portions. The submandibular duct passes forwards, lateral to hyoglossus, to open into the mouth on either side of the frenulum of the tongue. The duct is prone to blockage by submandibular stones, largely because the duct is long and the secretions sticky, the gland being rich in mucous secretory acini. In its course in the floor of the mouth the duct is intimately related to the lingual nerve (see above).
Sublingual salivary glands are scattered along the submandibular duct, into which some of them open, others opening directly into the oral cavity.
Secretomotor impulses to both glands originate in the superior salivary nucleus and pass by way of VII, the chorda tympani, lingual nerve and the submandibular ganglion (see Fig. 14.14).
Facial pulse
The facial pulse is palpable as the artery crosses the mandible. The facial artery has a tortuous course (to allow for mandibular movements) and passes through the submandibular gland.
Inferior alveolar nerve
The inferior alveolar nerve in the mandibular canal may be damaged by a mandibular fracture leading to sensory loss distally. This can be assessed by testing sensation over the chin (mental nerve, a continuation of the inferior alveolar).
Oral anaesthesia
Injection of local anaesthetics into the oral mucosa on the medial side of the mandible, aiming for the inferior alveolar nerve, can also involve the nearby lingual nerve causing numbness of the tongue and oral mucosa. In wisdom tooth extractions, the buccal nerve may also be involved giving numbness of the cheek.
Referred pain to the ear
Any area supplied by the mandibular nerve may give referred pain to the ear. Beware of patients with cotton wool in the external acoustic meatus – look in the mouth for the disease (e.g. oral or lingual cancer).
Palate and tonsillar bed
• The hard palate is formed by parts of the maxilla and palatine bone.
• The soft palate is muscular and formed by tensor palati, levator palati, palatoglossus and palatopharyngeus, the last two forming the palatoglossal and palatopharyngeal arches, visible in the mouth.
– Tensor and levator palati: base of lateral pterygoid plate–soft palate (details not necessary).
• The palatal arches (faucial arches, or fauces):
– The palatoglossal arch (with the uvula), the more anterior of the two, passes from the palate to the tongue and marks the posterior limit of the oral cavity.
– The palatopharyngeal arch, the more posterior of the two, passes from the palate to the side of the pharynx, and marks the anterior boundary of the oropharynx.
– The region between the two arches is the oropharyngeal isthmus.
• The tonsillar bed is at the side of the tongue between the two arches. Its principal artery is the tonsillar artery (a branch of the facial), which enters from below. Infection of the palatal mucosa above the tonsillar bed between the arches may lead to an abscess in these peritonsillar tissues and cause bulging of the arches. This is a quinsy. An incision is required to drain the pus.
• The motor innervation of these muscles is X except for tensor palati, which is Vc.
• The sensory innervation is from palatine branches of Vb and, in the tonsillar bed, branches of IX.
• The lymph drainage passes to the tonsillar (jugulodigastric) node at the top of the deep cervical chain.
Nerves of ingestion and chewing: functional considerations
Opening the mouth depends upon the mandibular and facial nerves: the mandibular nerve supplies the muscles that open the jaw, and the facial supplies the muscles that part the lips. Chewing is served by the same nerves together with the hypoglossal: in simple language, the facial keeps the lips closed, the mandibular innervates the muscles that chew and grind the food, and both facial and hypoglossal nerves maintain the food in the occlusal plane by innervating buccinator and the tongue. Furthermore, in a baby before weaning, the facial and hypoglossal nerves supply the principal muscles of sustenance producing the necessary sucking forces: buccinator and the tongue. This is why damage to the facial nerve in a baby is serious.
Sensory components of ingestion and chewing are also served by the trigeminal and facial nerves. Both the mandibular and maxillary nerves sense the position and consistency of the food and regulate the force of contraction of the muscles, and taste perception in the mouth is served by various branches of the trigeminal and the facial nerves.
As we chew, it is necessary that the strength of contraction in muscles like masseter and temporalis is monitored. Were these muscles to exert undue force, and they are very powerful muscles, teeth and gums would be damaged. Proprioceptive impulses from the upper jaw are carried in branches of Vb and from the lower jaw in branches of Vc. The fibres which carry them are unique in that their cell bodies are not in a peripheral (in this case the trigeminal) ganglion: they have been ‘sucked’ into the brain stem to form the nucleus itself: the mesencephalic trigeminal sensory nucleus. Onward connections from this nucleus are not clear, but some pass to the trigeminal motor (mandibular) nucleus for direct control of the motor impulses to the muscles.
14.8. Anatomy of swallowing and phonation
The pharynx is divided into, from above down, nasopharynx, oropharynx and hypopharynx (laryngopharynx). Its walls are formed by constrictor muscles. The larynx opens from the anterior pharyngeal wall and contains the vocal cords. All movements of the pharynx and larynx, for swallowing and phonation, are supplied by the nucleus ambiguus of the brain stem, principally through cranial nerve X. The anatomy of the laryngeal skeleton is important for intubation and access to the airway in an emergency.
You should:
• describe the basic construction of the pharynx and larynx
• describe the anatomy of vocal cord movements
• describe the motor and sensory innervation of the pharynx and larynx, and the areas to which pain may be referred
• describe the lymph drainage of the pharynx and larynx
• describe the surface anatomy of the larynx, particularly with regard to laryngotomy and tracheostomy.
Pharynx
Parts of the pharynx (Fig. 14.26)
• Nasopharynx: above the level of the palate (see section 14.9, p. 281).
• Oropharynx: between the levels of the palate and the tip of the epiglottis. This is anterior to vertebrae C1, 2. Its anterior boundary is the palatopharyngeal arch.
– The mucosal fold in the midline between the posterior surface of the tongue and the base of the epiglottis is the median glosso-epiglottic fold. The small recess on each side is the vallecula.
• Hypopharynx, or laryngopharynx: between the tip of the epiglottis and the cricopharyngeal sphincter (vertebral level C6) at the top of the oesophagus.
– The larynx opens from the anterior wall of the hypopharynx.
– The piriform fossas are the lateral portions of the hypopharynx, on either side of the laryngeal opening. They are the pathways taken by swallowed material on its way from mouth to oesophagus, thus avoiding the laryngeal opening.
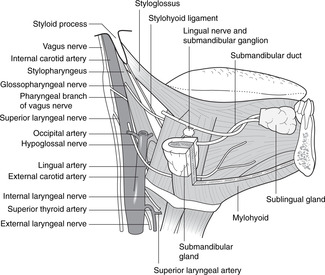 |
| Fig. 14.26 |
Walls of the pharynx
The constrictor muscles form the walls of the pharynx and are attached posteriorly to the median pharyngeal raphe. This hangs down from the pharyngeal tubercle underneath the basi-occiput just anterior to the foramen magnum, and blends inferiorly with the posterior wall of the hypopharynx and oesophagus.
The constrictors are arranged as three overlapping units: superior, middle and inferior. Between muscle and pharyngeal epithelium is the pharyngobasilar fascia, which is attached to the base of the skull and the medial pterygoid plates. Fibres of the constrictors pass down and laterally to attach to various skeletal elements in front. From above down:
• Superior constrictor: this is attached to the lower half of the medial pterygoid plate, the pterygomandibular raphe and the adjacent lingula. It continues forwards as buccinator. It is not attached to the upper part of the medial pterygoid plate: the Eustachian tube opens here.
• Middle constrictor: this is attached to the side of the body and lesser horn of the hyoid bone.
• Inferior constrictor: this is attached to the lateral surface of the thyroid and cricoid cartilages.
• Cricopharyngeus is part of the inferior constrictor that forms a sphincter at the level of the cricoid cartilage (vertebral level C6), controlling entry to the oesophagus.
• Other muscles, details are not important:
– Palatopharyngeus has no skeletal attachments. Part of it passes up to the nasopharynx to surround the orifice of the Eustachian tube (see p. 281).
– The movements of the pharynx are assisted by other muscles from above, such as stylohyoid (VII), stylopharyngeus (IX), and styloglossus (XII).
• Killian’s dehiscence. This is a potential weak spot in the posterior wall of the pharynx where the obliquely orientated fibres of the inferior constrictor and the transverse cricopharyngeus fibres leave a triangular defect. A pharyngeal diverticulum may arise here.
Nerves
The pharyngeal plexus in the pharyngeal wall receives fibres as follows:
• Motor: fibres from the nucleus ambiguus in X supply all pharyngeal muscles, unless otherwise stated.
• Sensory:
– nasopharynx: fibres from Vb and IX
– oropharynx: fibres from IX and X; scattered taste buds in the epiglottic region are supplied by X
– hypopharynx and below: fibres from X.
– note the progression from above down: Vb in nasopharynx, IX in oropharynx, X in hypopharynx, with much overlap.
Blood and lymph vessels
Arteries
Blood supply is from local branches of the external carotid artery: ascending pharyngeal, superior thyroid, lingual, facial.
Veins
Venous blood drains to tributaries of the internal and external jugular veins.
Lymph
Lymph drainage is to the deep cervical chain and retropharyngeal nodes.
Swallowing
Once the bolus of food has been propelled to the posterior third of the oral cavity by buccinator (VII) and the tongue (XII):
• The soft palate rises to close off the nasopharynx (palatal muscles, X).
• The Eustachian tube orifice opens (X).
• The laryngeal entrance is reduced in size to minimise the likelihood of material entering it. This involves narrowing of the laryngeal entrance (laryngeal muscles, X), elevation of the larynx (stylo-muscles, VII, IX, X; posterior digastric, VII, mylohyoid Vc, etc.) and the epiglottis momentarily flips down during the act of deglutition.
• The cricopharyngeal sphincter opens (X).
I think I have something stuck in my throat
Foreign bodies, such as fish or chicken bones, sometimes become impaled in the vallecula. These are easy to get at. More often, they are arrested in the piriform fossa or at the cricopharyngeal sphincter, with the patient requiring anaesthesia for laryngoscopy. A lateral radiograph of the neck may display such a foreign body, but remember that calcification of the laryngeal cartilages may confuse you. Often, when a patient thinks there is something stuck, it is simply that a sharp object has scratched the mucosa on the way down and the patient is misled by the dull visceral pain of a scratch.
Earache and pharyngeal tumours
The vagus supplies a large area of pharyngeal mucosa and also skin of the posterior wall of the external acoustic meatus and posterior tympanic membrane. Pharyngeal tumours may present as earache (referred pain).
Vagal reflexes
Irritation of the skin on the posterior wall of the external acoustic meatus (supplied by the vagus) can cause coughing, vomiting, or syncope (as a result of reflex bradycardia).
Larynx
Parts of the larynx (Fig. 14.27, Fig. 14.28 and Fig. 14.29)
Revise the anatomy of the hyoid bone, thyroid and cricoid cartilages (section 14.5, p. 257).
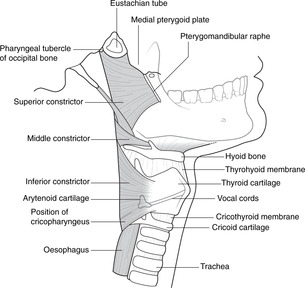 |
| Fig. 14.27 |
Parts of the larynx, described from superior to inferior, are:
• Resting on the (posterior) lamina of the cricoid cartilage are the right and left pyramidal-shaped arytenoid cartilages. The mucosal ridges that connect these to the base of the epiglottis are the aryepiglottic folds and they form the upper margin of the laryngeal opening (or aditus).
• The vocal cords (true vocal cords, or vocal folds) are below the vestibular folds, at about vertebral level C4, just below the level of the thyroid prominence.
• The two vocal cords as a unit constitute the glottis, and the aperture between them is the glottic aperture.
• The subglottic area of the larynx is below the vocal cords and extends down to the cricoid cartilage at vertebral level C6, at which point the trachea begins.
Vocal cords and movements: a simplified account
From the anterior (vocal) process of each arytenoid, a fibrous bands extends forwards, attached in front to the posterior surface of the lamina of the thyroid cartilage. This is covered by laryngeal epithelium and forms the vocal cord. The two cords oscillate against one another, setting up a vibrating column of air above – phonation – which is transmuted into speech by movements of other head and neck structures.
The sides of the glottic aperture are formed by the vocal cords (anterior two-thirds) and the medial border of the arytenoid cartilage from which they extend (posterior one-third). The cords can be abducted in two ways:
• The arytenoid cartilages can simply be pulled apart, creating a triangular-shaped glottic aperture.
• The arytenoid cartilages can swivel on the lamina of the cricoid at the synovial cricoarytenoid joints. If the lateral processes of the arytenoids are pulled backwards, their anterior processes and vocal cord attachments swing laterally to produce a diamond-shaped aperture.
The movements of adduction are the opposite of these.
The tension of the vocal cords affects the pitch of the voice. If the cords are stretched, the pitch rises. This occurs when the thyroid cartilage is tilted forwards on the cricoid.
Muscles that move the vocal cords:
• Abduction: posterior cricoarytenoid.
• Adduction: lateral cricoarytenoid, thyroarytenoids.
• Tensing: cricothyroid (Fig. 14.28), and muscle fibres attached to the cords themselves.
Nerves
• Motor: X. All muscles are supplied by the recurrent laryngeal nerve, except for cricothyroid, which is supplied by the external branch of the superior laryngeal nerve.
• Sensory: X. Laryngeal mucosa above the cords is supplied by the internal branch of the superior laryngeal nerve, and below by the recurrent laryngeal nerve.
Blood and lymph vessels
Arteries
The larynx is supplied by laryngeal branches of the superior and inferior thyroid arteries.
Veins
Blood drains to tributaries of the thyroid and internal and external jugular veins.
Speaking
Noise production – phonation
The vocal cords create the narrow slit through which air is directed to make a sound, much as in an oboe, recorder or organ pipe. Muscles which move the cords are supplied by the recurrent laryngeal nerve (X). Pitch is modulated principally by tensing (cricothyroid) and relaxing the vocal cords through the superior and recurrent laryngeal nerves (X). It is unnecessary to learn individual laryngeal muscles or their attachments: it is enough to know of their innervation.
Making the noise intelligible – articulation
The pharyngeal muscles (X), the tongue (XII), the muscles of facial expression (VII), mandibular movements (Vc) and the palate (X, V) all modify the crude noise produced by the larynx to create speech.
Movements of the pharynx and larynx: swallowing and phonation
The cell bodies of peripheral motor neurons supplying the muscles of the pharynx and larynx are in the nucleus ambiguus in the medulla. You will be able to imagine what the effect would be of a lesion of the nucleus ambiguus: profound swallowing and speech disorders – bulbar and pseudobulbar palsies (see Ch. 15, p. 328).
Laryngeal tumours
Tumours which are restricted to the cords are likely to be detected early because of voice changes, and the combination of an early presentation with no local lymphatics means that survival rates are good. In contrast, tumours of the subglottis are not good. This area has lymphatics (to local deep cervical nodes) and a tumour here will not only spread, but also will present late. It will have to grow large before it is visible beyond the vocal cords on laryngoscopy, and it may not cause voice changes.
Laryngotomy (tracheotomy), tracheostomy
• Emergency: laryngotomy. The problem is usually that the glottic aperture is blocked (foreign body, swollen cords, etc.), so there is no point inserting a hollow needle above the cords. Insert the needle in the midline of the cricothyroid membrane, below the thyroid prominence. (This is sometimes called tracheotomy – wrongly, since the needle is inserted into the larynx not the trachea).
• More permanent: tracheostomy. Divide the isthmus of the thyroid gland (much lower than a laryngotomy) and remove part of the anterior tracheal wall (in the region of tracheal rings 2–4). Note that stoma means orifice, -tomy means cut (as in anatomy).
Referred pain and laryngeal tumours
The vagus supplies a large area of laryngeal mucosa, whether by the internal or the recurrent laryngeal nerves. As with pharyngeal tumours, and for the same reason, laryngeal tumours often present as earache.
Laryngoscopy and insertion of airway
Look at Figures 14.30–14.31 and see why it is necessary to extend the patient’s neck. If the patient is unconscious, it’s helpful to remember ABC: airway, breathing, circulation – in that order.
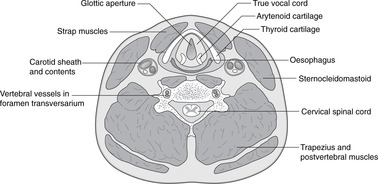 |
| Fig. 14.30 |
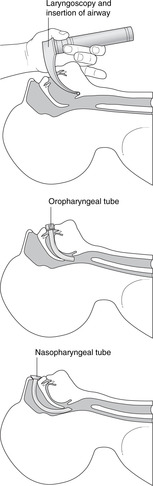 |
| Fig. 14.31 |
If the patient has had a stroke that affects cranial nerve XII (which supplies the tongue muscles), keeping the tongue out of the way can be a problem. Remember to press on the cricoid cartilage to keep the oesophagus closed, thus preventing stomach contents from appearing on the scene.
Insertion of tube
Study Figures 14.30 and 14.31. Be careful not to damage the vocal cords – pass the oropharyngeal or nasopharyngeal tube between the cords, not through them – as you insert the tube into the trachea.
Mediastinal tumours
Because of the thoracic course of both recurrent laryngeal nerves, mediastinal tumours may present as voice changes. This is more common on the left than the right because the nerve is lower on the left.
14.9. Nose, nasal sinuses and the sense of smell: cranial nerve I
The nasal cavity is divided by three turbinate bones (conchae) into inferior, middle and superior meatuses, and, at the top, the sphenoethmoidal recess. Nasal sinuses open into the lateral wall of the nasal cavity, ethmoid sinuses separating the nasal cavity from the orbit. The nasal cavity receives arterial blood mainly from the maxillary artery and is innervated mainly by the maxillary nerve. Olfactory mucosa is confined to the sphenoethmoidal recess. This is separated from the anterior cranial fossa by the cribriform plate of the ethmoid bone, sometimes fractured in head injuries.
External nose
The skeleton of the external nose is mainly cartilaginous. The overlying skin is supplied laterally by branches of Vb and in the midline by the external nasal nerves (continuations of the anterior ethmoidal branches of Va), which become superficial at the junction of cartilage and nasal bone, easily palpable. Fractures of the nasal bridge may damage this nerve resulting in sensory loss in skin down to the nasal tip.
Nasal cavity (Figs 14.24, 14.32, 14.33)
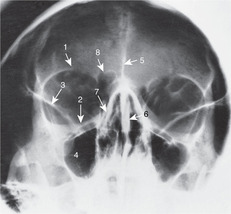 |
| Fig. 14.33 |
The nasal septum separates the two cavities. The anterior portion is cartilaginous, the central portion is formed by the perpendicular plate of the ethmoid, and the posterior portion, separating the two choanae, is formed by the vomer. A deformed or deviated nasal septum may interfere with nasal breathing and the cartilaginous portion can be removed in whole or in part by an operation called a submucous resection (SMR). The floor of the cavity is formed by the palatal shelf of the maxilla and the palatine bone, and the roof by the cribriform plate of the ethmoid.
Superior, middle and inferior turbinates (or conchae) project into the nasal cavity from the lateral wall. The superior and middle turbinates are parts of the ethmoid, but the inferior turbinate is a separate bone. The epithelium of the turbinates is highly vascular, almost erectile, for the purpose of humidifying inspired air, and is frequently the site of inflammatory reactions to allergens. The turbinates divide the nasal cavity into four parts as follows:
• inferior meatus, below the inferior turbinate
• middle meatus, between inferior and middle turbinates
• superior meatus, between middle and superior turbinates
• sphenoethmoidal recess, between the superior turbinate and the cribriform plate of the ethmoid.
Openings on the lateral wall of the nose
• Into the inferior meatus: nasolacrimal duct, anteriorly, draining tears from the orbit.
• Into the middle meatus: frontal and maxillary sinuses, respectively at the anterior and posterior ends of a crescentic groove, the hiatus semilunaris. Behind this is the sphenopalatine foramen, which admits branches of the maxillary artery and nerve from the pterygopalatine fossa. This is covered by mucosa in the live specimen.
• Into the middle and superior meatuses: numerous ethmoid air cells.
• Into the sphenoethmoidal recess: sphenoid air sinus. This cavity in the body of the sphenoid bone is immediately in front of and below the pituitary fossa and a transnasal or trans-sphenoidal approach to the pituitary may be used.
Arteries and nerves
• Upper third of nasal cavity and ethmoid sinuses: ethmoidal branches of the ophthalmic artery and Va.
• Lower two-thirds of nasal cavity and maxillary sinus: branches of the maxillary artery and Vb. These come mainly through the sphenopalatine foramen.
• Anteriorly, branches of the facial artery enter.
• For the septum, the pattern is as for the lateral wall. Structures entering through the sphenopalatine foramen gain access to the septum by passing across on the roof of the nasal cavity.
Venous drainage
This is to local venous networks including facial veins and the pterygoid venous plexus. About a centimetre inside the naris on the septum, close enough for a finger to reach, is Little’s area, the site of a rich venous anastomosis between tributaries of facial veins and veins draining deeply. It is often the site of bleeding and is frequently cauterised (often unnecessarily).
Lymph drainage
This is mainly to retropharyngeal nodes and the deep cervical chain, with the anterior region draining to superficial facial lymph vessels and the submandibular nodes.
Maxillary sinus (antrum) (Fig. 14.34)
This, the largest of the nasal sinuses, is in the maxilla between the upper teeth and the orbit. The infraorbital nerve (Vb) runs in its roof and supplies it. Its floor is intimately related to the roots of the maxillary teeth, particularly the second molar. In young children, this area is occupied by the as yet unerupted permanent dentition and the maxillary sinus is rudimentary.
Nasopharynx
The nasal cavities open into the nasopharynx through the two choanae. Its features are:
• the opening of the Eustachian tube
• the fossa of Rosenmüller, of no significance in itself except as the site of the adenoids (nasopharyngeal tonsils). These are components of Waldeyer’s lymphoid ring, which may be particularly large in children and block the Eustachian tube orifice.
The sensory innervation of the nasopharynx is from branches of Vb that pass back from the pterygopalatine fossa, and from branches of IX. It is included here as a reminder that it is part of the upper respiratory tract, as are the Eustachian tube and tympanic cavity, which are described in section 14.10 (pp. 284–285).
Maxillary sinus washout
The orifice between the maxillary sinus and the middle meatus is high on the medial wall of the sinus and it is said that the sinus is therefore badly drained. (This may be so when we stand, but not when we are lying or reading with our head dependent, and neither is it badly sited in quadrupeds.) It is sometimes thought appropriate to wash out the sinus. This is done by forcing a cannula through the bony lateral wall of the inferior meatus, and injecting fluid at pressure, which then, with the head in a dependent position, flows out through the natural orifice together with whatever was in the sinus beforehand.
Sinus cancers and proptosis
Epithelial cancers of the lining of the ethmoid and maxillary sinuses may invade the orbit causing proptosis (protruding eyes). Diplopia (double vision) results as the eyes become increasingly displaced.
Maxillary sinus pain
Infections of the maxillary sinus may cause referred pain to other structures supplied by Vb, e.g. upper teeth, infraorbital skin.
Fistula
Dental procedures on maxillary teeth may sometimes result in a permanent opening being established between the oral cavity and the maxillary sinus. This is an oro-antral fistula and it is a nuisance since pieces of food lodge in the sinus, become infected and give off offensive odours.
Olfaction, cranial nerve I (Fig. 14.33)
Olfactory epithelium is confined to the sphenoethmoidal recess, underneath the cribriform plate of the ethmoid.
• Olfactory receptors are the peripheral processes of bipolar sensory neurons, the cell bodies being deeper in the epithelium.
• Central axonal processes of the bipolar cells pass through the cribriform plate of the ethmoid and penetrate the meninges before entering the olfactory bulb. In the bulb they synapse on secondary sensory neurons forming the olfactory tract, which tract passes back on the inferior surface of the frontal lobe and gives onward connections to the temporal lobe, limbic system and elsewhere. What is usually referred to as the first cranial nerve, the olfactory tract, is not properly a nerve at all since it is part of the central nervous system. There are, in fact, many olfactory nerves on each side, not just one.
Anosmia, CSF rhinorrhoea
Head injuries which fracture the cribriform plate may tear olfactory axons resulting in post-traumatic anosmia. Such injuries may also lead to cerebrospinal fluid dripping from the nasal cavity (CSF rhinorrhoea) as a result of also tearing the dura mater and arachnoid.
Thanks for the memory
Olfaction and taste are two aspects of the same thing and both neural systems share common links. These include those to the limbic system of the brain, which is why smells and tastes can evoke memories, emotions and sexual responses, and also why there is some basis to aromatherapy and the ritual use of aromatics such as incense.
Clinical testing of I
It is hardly worth the trouble; you might just as well rely on the subjective opinion of the patient, which is, after all, what matters.
14.10. Ear, hearing and vestibular function: cranial nerve VIII
The ear is in three parts: external, middle and internal. The external and middle ears, separated by the tympanic membrane, conduct sound waves to the inner ear by means of the ossicular chain. The middle ear is part of the upper respiratory tract. The inner ear contains the auditory and vestibular organs in a common hydraulic system, so inner ear disease often leads to both auditory and vestibular symptoms.
You should:
• describe the organisation of the three parts of the ear, the tympanic membrane and the ossicles
• describe the innervation of the external ear and middle ear
• explain why respiratory tract disease may spread to the ear and cause deafness
• understand why disease of the external ear and middle ear causes conductive deafness
• describe the basic organisation of the inner ear
• explain why disease of the inner ear causes sensorineural deafness
• explain why inner ear disease may cause both auditory and vestibular symptoms.
Parts of the ear
The complex evolutionary history of what we call the ear has resulted in a three-part structure: external ear, middle ear and inner ear.
• The external ear consists of the pinna (or auricle), which focuses sound waves from the environment into the external acoustic meatus and on to the tympanic membrane. This membrane (commonly known as the ear drum) has air on each side, air on the medial side being in the middle ear cavity, which is a lateral extension of the nasopharynx.
• The middle ear or tympanic cavity contains the ossicles, three small bones that transmit vibrations from the tympanic membrane to the inner ear in the petrous temporal bone.
• The inner ear is an enclosed hydraulic system within the petrous temporal bone. The vibrations in the fluid of the inner ear act upon hair cells that send electrical impulses to the brain in the cochlear portion of the eighth cranial nerve.
• The inner ear has another, more important, function. It contains vestibular organs for registering movement of the head with respect to gravity. These movements, too, are picked up by hair cells with nerve impulses being conveyed to the brain in the vestibular portion of the eighth cranial nerve. In this regard, you may be able to understand why the petrous bone is rock-like (for protection), and why it is important that it is firmly fixed to the sphenoid and occipital bones, indeed fused in adult life, so that the right and left vestibular organs do not vary in position relative to each other.
The frequency of general medical consultations about the ear justifies consideration of the clinical anatomy of the ear in some detail.
External ear
Pinna or auricle
The elastic cartilages of the pinna are arranged in a number of curved ridges which include the helix (outer rim) and the tragus (the small flap ‘guarding’ the external acoustic meatus anteriorly). The lobule (ear lobe) is fatty and apparently functionless except in some people as a hook to hang things on.
• Sensory nerves: cervical plexus C2, 3 except for the concavity (the concha) opposite the tragus, which is supplied by the auricular branch of X.
• Arteries, veins, lymph: as for the external acoustic meatus (see below).
External acoustic meatus (Fig. 14.35)
Laterally (about two-thirds), the external meatus is a cartilaginous tube; medially it is a bony canal in the temporal bone. It curves forwards and downwards as it approaches the tympanic membrane, so in the adult it can be straightened by pulling the pinna up and back: this gives a better view when you use an otoscope. In a young child, pull the pinna down and back (this is because the external meatus is shorter, there is virtually no bony portion, and the orientation of the cartilaginous part is different). The cross-sectional diameter of the meatus, and the diameter of the tympanic membrane, are much the same in the child as in the adult.
The meatus is lined by skin secreting cerumen, modified sebum with protective properties for the delicate meatal skin. Epithelial cells migrate externally as they are replaced by new ones and the combination of discarded cells and cerumen is wax. This is a naturally regulated process and never requires assistance from cotton buds. Unless you are examining someone’s ear, never put anything in the external acoustic meatus that is any smaller than an elbow.
• Sensory innervation:
– anterior three-quarters (roughly): branches of the cervical plexus laterally, and auriculotemporal nerve (Vc) medially
– posterior quarter: auricular branch of X.
• Arteries: posterior auricular and other branches of the external carotid artery.
• Veins: to tributaries of the external jugular vein.
• Lymph: to parotid and mastoid nodes and the deep cervical chain.
Tympanic membrane (Fig. 14.35)
This is a three-layered structure.
• The outer layer is modified skin, continuous with that of the external acoustic meatus and sharing the pattern of cell renewal and disposal. Should this pattern fail, or be disrupted by cotton buds, disease results.
• The middle layer is connective tissue through which the chorda tympani passes.
• The inner layer is respiratory epithelium of the middle ear cavity.
The membrane is arranged as a shallow cone with the apex, umbo, pointing medially. It faces slightly downwards and laterally, the anterior wall of the external meatus being longer than the posterior. This apparently trivial detail is responsible for the cone of light that you see when using an otoscope.
Sensory nerves:
• Anterior three-quarters: branches of the auriculotemporal nerve (Vc).
• Posterior quarter: auricular branch of X.
Arteries, veins, lymph. Blood supply and blood and lymph drainage are as for the middle ear (see below).
Features of the tympanic membrane visible externally
• The membrane is divided approximately one-quarter of the way down into a smaller upper sector, the pars flaccida, and a larger lower sector, the pars tensa, the dividing line being the anterior and posterior malleolar folds. Disease in the pars flaccida should be treated seriously because of what lies behind it.
Middle ear cavity, mastoid antrum, ossicles, oval window
Imagine that you are miniaturised in the nasopharynx. The orifice of the Eustachian (pharyngotympanic, auditory) tube is level with the posterior end of the inferior turbinate. The cartilaginous walls of the tube project into the nasopharynx somewhat, and the tubal orifice is surrounded by fibres of an extension of palatopharyngeus muscle (called salpingopharyngeus) which is responsible for opening the orifice during swallowing.
• You proceed along the Eustachian tube laterally, upwards and backwards, through the temporal bone. The tube opens into the middle ear or tympanic cavity, very narrow (1–2 mm) from side to side, but quite tall. On its lateral wall you see the tympanic membrane with the malleus attached to its medial surface and the chorda tympani running from front to back (or back to front) near the top of the membrane, lying between the membrane and the respiratory epithelium. Above, you see the ossicular chain.
• Continue backwards through an orifice into a smaller chamber with a large number of air cells opening from it. This is the mastoid antrum, the entrance into it is the aditus of the mastoid antrum, and the many small cells are the mastoid air cells in the mastoid process of the temporal bone. Now return to the main chamber.
• The upper part of the tympanic cavity contains the ossicles. It is quite extensive and its roof is formed by a thin plate of bone, the tegmen tympani, separating it from the middle cranial fossa and the temporal lobe of the brain. The handle of the malleus, attached to the tympanic membrane, is continuous above with the body of the malleus, and this articulates (a synovial joint) with the body of the incus. The long process of the incus descends medially to articulate with the stapes at the incudostapedial joint (also synovial). The stapes is stirrup-shaped: the neck, which articulates with the incus, gives two crura (there used to be an artery between them) with a medially facing footplate attached to their ends. The footplate fits into the oval window (fenestra ovalis, fenestra vestibuli) in the medial wall of the middle ear, which, were it not closed by the footplate of the stapes, would allow us to proceed through it into yet another cavity in the temporal bone, the inner ear. Vibrations of the tympanic membrane and ossicular chain cause the footplate of the stapes to move back and forth in the oval window, the edges being sealed by connective tissue.
• The inner ear is a closed, fluid-filled system and so when the footplate of the stapes moves medially there must be a compensatory mechanism in the inner ear to take account of the fact that fluids are not compressible. A secondary membrane bulges laterally into the middle ear cavity when the footplate of the stapes moves medially, and vice versa. This is the round window (fenestra rotundum, fenestra cochleae) situated below the oval window.
• Two muscles are attached to the ossicles:
– Tensor tympani runs from the bone near the Eustachian tube to the handle of the malleus. It is supplied by Vc and if you try chewing whilst listening to someone, you will see, or rather hear, what it does.
– Stapedius is attached to the neck of the stapes. It arises from the medial wall of the middle ear cavity and dampens the movements of the stapes. It protects the delicate inner ear hair cells from being mechanically overstimulated. Before considering its nerve supply, the single most important relationship of the middle ear cavity needs to be mentioned: the facial nerve.
• The facial nerve passes from the posterior cranial fossa into the internal acoustic meatus, at the lateral end of which it turns backwards into the facial canal. This is separated from the middle ear cavity by only the thinnest (at most 1 mm) of bony partitions, absent in some people. The facial canal then turns laterally and down towards the stylomastoid foramen, forming the lower border of the aditus into the mastoid antrum. It gives a branch to supply stapedius, and just before emerging at the stylomastoid foramen it gives off the chorda tympani.
• Other relationships of the middle ear cavity:
– The tegmen tympani, which may be very thin (1 mm or less), separates the middle ear cavity from the middle cranial fossa and the temporal lobe of the brain.
– The internal carotid artery and internal jugular vein are very close to the floor.
Nerves and vessels of middle ear and Eustachian tube
• Sensory nerves to the mucosa: mainly branches of IX.
• Arteries: direct branches of the internal carotid (through the roof of the carotid canal), pharyngeal vessels.
• Veins: to the internal jugular vein.
• Lymph: to the deep cervical chain.
Vagal reflexes
Irritation of the skin on the posterior wall of the external acoustic meatus (supplied by the vagus) can cause coughing (X: bronchial tree sensation), vomiting (X: alimentary canal sensation), or syncope (reflex bradycardia).
Conductive deafness
Deafness resulting from diseases of the external and/or middle ear is called conductive deafness because the conduction of mechanical impulses to the footplate of the stapes is defective. It may be caused by:
• A blocked external acoustic meatus (e.g. inspissated wax, foreign body, inflammation).
• A perforated tympanic membrane reducing the effective area for the reception of sound waves.
• Dislocation of the ossicular chain (e.g. after a head injury).
• Synovial joint disease (e.g. rheumatoid arthritis) of the ossicular chain.
• Reduced ossicular movement as a result of the middle ear cavity being full of mucus, overproduced by its lining respiratory epithelium. This is glue ear. It may be caused by the pharyngeal orifice of the Eustachian tube being blocked by enlarged adenoids.
• Fixation of the footplate of the stapes in the oval window as a result of calcification at the margins.
All these causes of deafness are treatable.
Facial nerve
Because of the proximity of the middle ear cavity to the facial canal, a middle ear infection may cause a lesion of VII.
Hyperacusis
If stapedius is inactive (e.g. as a result of lesion of VII), movements of the stapes are not dampened, and sounds are distorted and echoing. This is hyperacusis.
Brain abscess
Because of the proximity of the middle ear cavity to the middle cranial fossa and temporal lobes, a middle ear infection may give rise to a temporal lobe abscess.
Inner ear (Fig. 14.36)
The inner ear has two parts: the osseous labyrinth and the membranous labyrinth.
Bony labyrinth
The bony (osseous) labyrinth is a single cavity in the petrous temporal bone containing perilymph, which would drip out through the oval and round windows were the windows not occluded. The cavity has three parts:
• The vestibule is the central ovoid part.
• The two and a half turns of the cochlea extend anteriorly, coiled around the central modiolus.
• The anterior (or superior), lateral and posterior semicircular canals extend from the vestibule posteriorly. They are disposed at right angles to each other for the purposes of registering movements in all planes.
Membranous labyrinth
The membranous labyrinth is a fluid-filled tube within the bony labyrinth. It contains endolymph and does not communicate with perilymph.
Hearing
Within the bony cochlea is the membranous cochlear duct, echoing the shape of the bony cochlea around it. The cochlear duct is wedge-shaped in cross-section and is attached to the walls of the bony cochlea so that the perilymph-containing area does not surround the cochlear duct, but is above and below it in, respectively, the scala vestibuli and the scala tympani. The membranous cochlear duct between is the scala media. The scala vestibuli and scala tympani communicate at their origin from the vestibule and at the apex of the cochlea, the helicotrema. The partition between the scala media (cochlear duct) and the scala tympani is the basilar membrane and the sensory hair cells form the organ of Corti resting on this membrane.
• The side wall of the scala media is composed of epithelial cells and melanocytes making up the stria vascularis, which produces endolymph.
• Vibrations of the footplate of the stapes set up vibrations in perilymph which in turn impinge upon endolymph, the basilar membrane and the organ of Corti.
Vestibular function
The membranous labyrinth within the bony vestibule is more complex in its anatomy than that of the cavity around it.
• It has two chambers, saccule and utricle, joined by connecting ducts from which the endolymphatic duct extends through the temporal bone. This terminates in the endolymphatic sac lying between the dura and the bone in the posterior cranial fossa. This is the pressure-release chamber for endolymph.
• Semicircular ducts (membranous) open from the utricle and are disposed in more or less the same way as the semicircular canals in which they are situated (anterior or superior, lateral and posterior).
• At several sites in the walls of the utricle and saccule, and in a dilatation (ampulla) at the base of each semicircular duct, hair cells extend into a gelatinous cap which ‘floats’ in the endolymph and moves in response to postural changes, thus distorting the hairs of the hair cells.
• The precise functions of the vestibular components of the membranous labyrinth are not clear.
Arteries and veins of middle ear and Eustachian tube
• Arteries: labyrinthine artery (from vertebrobasilar system through internal acoustic meatus), direct branches of the internal carotid (through the temporal bone).
• Veins: to internal jugular vein.
VIII: auditory pathways and reflexes
• From the organ of Corti, nerve impulses pass in bipolar neurons with cell bodies in the cochlear (spiral) ganglion in the modiolus (central pillar) of the cochlea. The central processes of these axons form the cochlear portion of VIII, which joins the vestibular portion at the lateral extremity of the internal acoustic meatus to form the eighth cranial nerve.
• VIII passes medially alongside VII in the meatus, across the posterior cranial fossa and is attached to the brain stem at the cerebellopontine angle, the most lateral of the nerves attached at that site.
• Axons pass to the cochlear nuclei of the lateral medulla.
• Secondary sensory neurons pass bilaterally to the midbrain (for auditory reflexes), medial geniculate bodies, and thence to the auditory cortex in the upper part of the temporal lobe (see Ch. 15).
• Some secondary sensory neurons pass elsewhere, e.g. to the medial longitudinal fasciculus (see below).
Auditory reflexes. When a loud noise is heard:
• Extrinsic ocular muscles turn the eyes towards the source of the sound. Connections responsible for this include those to the nuclei of III, IV and VI in the medial longitudinal fasciculus.
• There may be a sudden inspiration and/or exclamation (startle reflex). This illustrates connections to the spinal cord and nucleus ambiguus from the midbrain.
• There may be tensing of the tympanic membrane by tensor tympani and stabilisation of the stapes, which directly impinges on the cochlea, by stapedius. This illustrates connections to the trigeminal motor nucleus (for tensor tympani) and the facial motor nucleus (for stapedius).
• You may be awoken because of connections to the brain stem reticular formation.
VIII: vestibular pathways
• From the hair cells of the utricle, saccule and semicircular ducts, nerve impulses pass in bipolar neurons with cell bodies in the vestibular ganglion adjacent to the vestibule in the petrous temporal bone. The central processes of these axons form the vestibular portion of VIII, which joins the cochlear portion at the lateral extremity of the internal acoustic meatus to form the eighth cranial nerve.
• VIII passes medially alongside VII in the meatus, across the posterior cranial fossa and is attached to the brain stem at the cerebellopontine angle, the most lateral of the nerves attached at that site. Most axons pass directly to the cerebellum.
One closed system
The cochlear duct is continuous with the saccule, utricle and semicircular ducts: they form an enclosed endolymph-containing system derived from the otocyst. Cochlear disorders, therefore, may affect the vestibular system, and vice versa.
Sensorineural deafness
Sensorineural deafness results from disease of the cochlea, the vestibulocochlear nerve or the auditory pathway. It includes the deafness of old age (presbyacusis). It is clinically distinguishable from conductive deafness and is largely untreatable except by hearing aids, although cochlear implants may work if the fault is in the cochlea.
Nystagmus
The vestibular system (including the cerebellum) is connected to the nuclei of cranial nerves III, IV and VI and the spinal cord neurons by the medial longitudinal fasciculus, a brain stem tract. Disorders of the vestibular system may therefore result in jerky eye movements: nystagmus. A patient who has nystagmus when looking straight ahead most definitely needs to be investigated. Nystagmus at the extremes of lateral vision is not necessarily abnormal.
Travel sickness
Travel sickness illustrates the connections from the vestibular pathways and cerebellum to the vomiting centre in the medulla.
Ménière’s disease
Prosper Ménière described a condition consisting of attacks of deafness, vertigo and tinnitus (noises in the head). It arises from an endolymph disorder and its symptoms reflect the endolymphatic continuity between cochlea, saccule, utricle and semicircular ducts.
Endolymph and Dalmatian dogs
Endolymph production from the stria vascularis requires melanocytes. Pigment disorders (such as albinism) and deafness are associated: did you know that Dalmatian dogs, with their extensive albino patches, are hard of hearing?
Cerebellopontine angle tumours
These cause signs and symptoms of damage to VII and VIII and possibly cerebellar signs. An acoustic neuroma is a tumour of Schwann cells on VIII. If it extends into the internal acoustic meatus it will compress VII and VIII causing a nerve deafness and an ipsilateral facial palsy.
Clinical testing of VIII
• Simple tuning fork tests and audiometry distinguish between external and middle ear deafness (conductive) and inner ear and nerve deafness (sensorineural).
• Vestibular function can be tested by:
– electrical neurophysiological testing
– a long-established and still performed test, the caloric test, which involves irrigating the external acoustic meatus with warm and cold water. Convection currents affect the lateral semicircular duct (the nearest to the tympanic membrane), which provokes nystagmus. The duration of this can be measured and compared with results from a normal subject.
• But the best and easiest way to test the function of the vestibulocochlear nerve is to send the patient to the ENT clinic with, of course, a polite request.
14.11. Orbit, eye movements, vision, visual reflexes; cranial nerves II, III, IV, VI
The bony orbit contains the eyeball and muscles that move it. The muscles are innervated by cranial nerves III, IV and VI. Within the eyeball, the anterior chamber contains aqueous humour produced by the ciliary body and absorbed at the canal of Schlemm. Visual impulses are generated in the retina and transported to the brain by the optic nerve (II). This is a brain outgrowth and is surrounded by meninges and CSF throughout its course from the back of the eyeball to the brain. One of the most commonly performed clinical tests is the pupillary light reflex.
Orbit (Fig. 14.3)
The bony orbit contains the visual apparatus together with the nerves, vessels and lacrimal apparatus that maintain it, the muscles that move it, and the orbital fat pad that cushions it.
The orbital walls are formed by the frontal bone, the zygoma, the maxilla and the ethmoid. Of the other bones that contribute to the walls, the sphenoid contributes to the posterior walls, and it surrounds all the important structures that enter or leave. The involvement of the orbit in facial and anterior cranial fossa fractures is obvious, and its involvement in tumours of the ethmoid and maxillary sinuses has been mentioned above.
• Superior orbital margin. The supraorbital nerve (from Va) and artery (from the maxillary) may be damaged by injuries to this region. Nerve damage would result in sensory changes in the skin of the anterior scalp.
• Medial wall of the orbit. The ethmoidal nerves (from Va) and artery (from the ophthalmic) pass from orbit to ethmoid sinuses and nose. Nerve damage would result in sensory changes in the upper nasal mucosa and skin of the dorsum of the nose. This part of the orbital wall is very thin (it is called the lamina papyracea, sheet of paper) and easily damaged.
• Inferior orbital margin. The infraorbital nerve (from Vb) and artery (from the maxillary) may be damaged by injuries to this region. Nerve damage would result in sensory changes in the skin of the maxillary region and upper lip.
Foramina
• Superior orbital fissure (in the sphenoid). This transmits, from lateral to medial:
– lacrimal nerve (branch of Va)
– frontal nerve (branch of Va)
– IV
– III, superior division
– nasociliary nerve (branch of Va)
– III, inferior division
– VI.
It also transmits several veins draining to the cavernous and other dural venous sinuses.
• Inferior orbital fissure (between maxilla and sphenoid). This transmits the infraorbital and zygomatic nerves (branches of Vb) and veins draining to the pterygoid venous plexus.
• Optic foramen (in the sphenoid): transmits II, and the ophthalmic artery (branch of internal carotid).
Extrinsic ocular muscles
The muscles that move the eyeball are all supplied by cranial nerves III, IV and VI. Most of them arise from a fibrous ring at the back of the orbit so placed that it includes within it the optic foramen and the medial portion of the superior orbital fissure (including III, the nasociliary nerve and VI).
• The muscles (with innervation) that are attached to the fibrous ring are:
– superior rectus (III)
– lateral rectus (VI)
– inferior rectus (III)
– medial rectus (III).
Muscles are named according to their position and they are attached to the sclera of the eyeball, a few millimetres behind the corneoscleral junction (nearer the front of the eyeball than the back). The action of each muscle is largely predictable, but the lines of pull of superior and inferior rectus muscles are not directly anteroposterior, so the muscles have secondary actions. Superior rectus, for example, is certainly an elevator, but also adducts and medially rotates (intorts).
• Superior and inferior oblique muscles approach the eyeball from the anteromedial corner of the orbit. Inferior oblique (III) is attached to the maxilla anteromedially. Superior oblique (IV) is attached at the back of the orbit near the optic foramen outside the common tendinous ring. Its belly runs forwards in the upper medial part of the orbit, and its tendon passes around a fibrous ‘pulley’ at the front, then turning back and laterally to approach the eyeball from above, more or less mirroring that of inferior oblique below.
– Inferior oblique turns the eye up and out.
– Superior oblique turns the eye down and out.
• Levator palpebrae superioris is above superior rectus, between it and the frontal bone. Its fibres are attached to the subcutaneous tissues of the upper eyelid, the superior tarsal plate; and to the skin of the forehead and upper eyelid by fibres passing amongst the circular fibres of orbicularis oculi. It elevates the upper eyelid and acts with superior rectus – when you look up your eyelid rises – and is supplied by the same nerve (III, superior division). It also receives sympathetic innervation, so when the sympathetic pathways are interrupted the upper eyelid droops (ptosis, see Horner’s syndrome, p. 300).
Eyelids (palpebrae) and lacrimal apparatus
• The eyelids contain fibrous tarsal plates that provide firmness to the lids and protect the eye when the palpebral fissure is closed. The tarsal plates contain tarsal glands opening by ducts at the palpebral margin of the eyelids. These ducts may become blocked leading to cyst formation.
– Levator palpebrae superioris is attached to the superior tarsal plate and pulls it up. The superficial tissues of the eyelids also contain the circular fibres of orbicularis oculi muscle, a muscle of facial expression supplied by VII.
– The space between the eyelids and the eyeball, which extends back for about 10 mm behind the edge of the cornea, is the conjunctival sac into which tears drain. It is lined by conjunctiva, a secretory mucosa with a function similar to that of synovium.
• The lacrimal gland is a small exocrine gland at the upper outer part of the orbit. It is arranged around the edge of the anterior portion of levator palpebrae superioris. Its secretomotor innervation originates in the superior salivatory nucleus and passes by way of VII, the pterygopalatine ganglion and branches of Vb and Va (Fig. 14.14). Numerous ducts open into the conjunctival sac, tears lubricating and protecting the eyeball, then passing medially over the surface of the eyeball to the lacrimal canaliculi, then draining through the nasolacrimal duct into the inferior meatus of the nasal cavity. Infection of the lacrimal canaliculi and/or ducts may block them, leading to tears dripping down the cheeks.
Sensory nerves and vessels of the orbit
• Sensory nerve supply: branches of Va.
• Arteries: almost exclusively from the ophthalmic artery. Some branches supply the nasal cavity (ethmoidals) and scalp (supraorbital and supratrochlear).
• Veins: to the cavernous (venous) and other dural sinuses, the pterygoid venous plexus and facial veins.
Moving the eye: cranial nerves III, IV, VI
III: Oculomotor nerve
• From the midbrain, III passes forwards in the cranial cavity to the lateral wall of the cavernous sinus. It enters the orbit through the superior orbital fissure and supplies levator palpebrae superioris (also supplied by sympathetic fibres), superior rectus, medial rectus, inferior rectus and inferior oblique.
• It conveys parasympathetic impulses for pupilloconstriction and focusing of the lens.
The nerve contains:
• Motor fibres: from the oculomotor nucleus in the periaqueductal grey matter of the midbrain.
• Parasympathetic impulses: from the Edinger-Westphal nucleus (adjacent to the above) in the midbrain to the ciliary ganglion (synapse), proceeding to the eyeball in branches of Va.
IV: Trochlear nerve
From the dorsal aspect of the midbrain, IV passes round the side of the midbrain then forwards to the lateral wall of the cavernous sinus. It passes through the superior orbital fissure and supplies superior oblique.
The nerve contains motor fibres: from the trochlear nucleus in the periaqueductal grey matter of the lower midbrain. Axons pass dorsally, decussating before emerging.
VI: Abducens nerve
From the pontomedullary junction, VI passes up to the apex of the petrous temporal bone and through (rather than in the lateral wall of) the cavernous sinus on the internal carotid artery. It passes through the superior orbital fissure and supplies lateral rectus.
The nerve contains motor fibres: from the abducens nucleus in the upper medulla, close to the facial motor nucleus.
Trochlear
IV is the thinnest and most fragile nerve and is vulnerable to trauma. Section of the nerve would result in the affected eye being turned medially.
Nuclei of VI and VII
The nucleus of VI and the axons of VII are closely related in the medulla. A brain stem lesion may cause facial weakness in association with a paralysis of the ipsilateral lateral rectus muscle of the eye.
Abducens
VI has the longest intracranial course of any cranial nerve and therefore it is often the first cranial nerve to be affected by intracranial disease. So, if you could only test one cranial nerve as part of a neurological investigation, VI would be it. Damage would result in a medial or convergent squint (the eye abductor being paralysed).
VI passes over the apex of the petrous temporal bone and may be affected by infections of the bone (petrositis) causing weakness of lateral rectus with medial deviation of the ipsilateral eye. This is Gradenigo’s syndrome: rare but interesting.
Cavernous sinus thrombosis
This may result from an infection of any part of the head that drains through veins communicating with it (e.g. face, ear, etc.). It would affect III, IV, Va, and VI, but VI is usually affected first because it passes through the sinus.
Clinical testing of III, IV, VI
• Eye movements. With his head stationary, ask your patient to keep both eyes on an object moving not too quickly (e.g. finger or pen) as it describes a large square with both diagonals. Should any abnormality be observed, or the patient report double vision, each eye may be tested more carefully. Or, if you want it done properly, send your patient to an optician or ophthalmologist.
• Testing III and VI. Ask your patient to look to one side: this tests medial rectus of one side (III) and lateral rectus of the other (VI).
• Testing IV. Although the superior oblique turns the eye down and out, these movements can be performed by other muscles in combination, so simply asking your patient to do this will not adequately test IV. Superior oblique is the only muscle that depresses the eye that has first been adducted, so this is a better test of IV.
• Look for a squint. A lesion of the main trunk of the oculomotor, trochlear or abducens nerves will be obvious.
• Nystagmus. Do not forget the connections of the nuclei of III, IV and VI with the medial longitudinal fasciculus (see section 14.10, above).
Eyeball (Fig. 14.37)
The eyeball is maintained in position by:
• the lateral check ligament – from the sclera near the lateral rectus attachment to the lateral orbital margin
• the medial check ligament – from the sclera near the medial rectus attachment to the medial orbital margin
• the suspensory ligament – between the two check ligaments like a sling
• the rectus muscles
• the orbital fat pad.
Coats of the eyeball
• Outer coat: sclera and cornea. This fibrous layer is protective and provides attachment for the rectus and oblique muscles. The change of orientation at the corneoscleral junction is the limbus.
• Middle coat: choroid, ciliary body, iris, collectively known as the uvea. It contains rich networks of blood vessels.
• Inner coat: retina, described later.
Parts of the eyeball
• In front of the lens:
– anterior chamber: between cornea and iris
– posterior chamber: between iris and lens.
Aqueous humour is secreted into the posterior chamber by the ciliary body and flows through the pupil to the anterior chamber. Here it passes through small defects at the iridocorneal angle (between iris and cornea) to the sinus venosus sclerae, or canal of Schlemm, which is a circumferential venous channel that drains to anterior ciliary veins. Any alteration on the iridocorneal angle, such as may be caused by inflammation of the iris (iritis), might interfere with the passage of aqueous humour into the canal of Schlemm. This causes a rise in intra-ocular pressure, and is one of the causes of glaucoma.
• Iris:
– radial smooth muscle fibres (dilator pupillae) are supplied by the sympathetic nervous system
– annular smooth muscle fibres (sphincter pupillae) are supplied by parasympathetic impulses from the Edinger–Westphal nucleus and III.
• Ciliary body: smooth muscle fibres (for accommodation) are supplied by parasympathetic impulses from the Edinger–Westphal nucleus and III.
• Lens: attached to the ciliary processes of the ciliary body by the suspensory ligament of the lens.
• Behind the lens: occupied by vitreous humour.
Vessels and sensory nerves of the eyeball
• Arteries: from branches of the ophthalmic artery:
– posterior and anterior ciliary vessels
– the central artery of the retina passes up the centre of the optic nerve to the retina (see below).
• Veins: drain to the venous network of the orbit.
• Sensory innervation (pain, tactile, etc.): nasociliary nerve (Va). The cornea is extremely sensitive. Local anaesthetic drops are used to abolish sensation for ocular procedures (e.g. minor surgery, measurement of intra-ocular pressure). The corneal reflex (p. 251) tests Va and VII.
• Pupillary dilatation results from sympathetic activity, or a loss of parasympathetic activity (fear, surprise, distant vision, lesion of III, darkness, drugs, death).
• Pupillary constriction results from parasympathetic activity, or a loss of sympathetic activity (Horner’s syndrome, bright lights, near vision).
• Unequal pupils may signify a unilateral lesion in the autonomic pathways.
Retina, optic nerve (II), optic tract (Fig. 14.38)
The retina and optic nerve are formed by the optic vesicle, an outgrowth of the embryonic brain containing an extension of the ventricular system. The optic vesicle is subsequently invaginated to form the two-layered retina with a potential space, formerly the cavity, between the layers. The cavity in the optic nerve is obliterated but its position is occupied by the central artery and vein of the optic nerve, the artery being a branch of the ophthalmic artery that enters the nerve in the orbit.
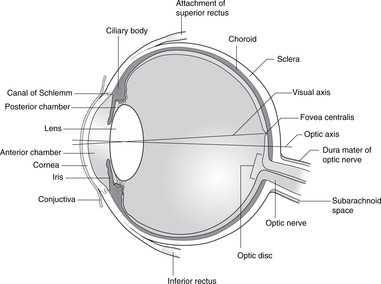 |
| Fig. 14.38 |
Optic disc, macula
• The optic nerve is attached to the inferomedial part of the eyeball, and the head of the optic nerve is marked on the retina by the optic disc, a pale area surrounded by the much pinker retina. In the centre of the optic disc is the blind spot (no light-sensitive cells) and this is the point at which the central artery and vein give into (usually) four branches disposed as an X on the retinal surface. All this is obvious on retinoscopy, particularly the sharp margin between the pale optic disc and its pink surroundings.
• About 4 mm lateral to the optic disc is the fovea centralis, the most light-sensitive part of the retina, which with its surrounding area constitutes the macula. The eye is usually positioned so that light rays from the object in the centre of the view fall upon the macula.
Retinal layers
• The outer layer of the retina, adjacent to the choroid, is the pigment layer. This extends on to the posterior aspect of the ciliary body and iris. It contains melanocytes and is reflective.
• The inner layer is the neural layer. In the postnatal eye it stops short of the ciliary body at the ora serrata.
• Rods and cones are in the deepest parts of the neural layer with processes in contact with the pigment layer. Light rays must penetrate the full thickness of the retina before reaching these light-sensitive components: because of this the retina is described as inverted (unlike that of some other vertebrates).
• Rods and cones excite bipolar cells (the primary sensory neurons), which synapse in the retina on ganglion cells.
• Axons of ganglion cells pass on the surface of the retina to the optic disc of the eyeball and then turn posteriorly, piercing the sclera to enter the optic nerve.
Optic nerve, chiasma, tract
• At the external surface of the eyeball the optic nerve acquires meningeal coverings as befits part of the brain: it is surrounded by meninges, subarachnoid space and CSF.
• The optic nerve passes through the optic canal.
• In the anterior cranial fossa the optic nerve meets its opposite number to form the optic chiasma in the anterior wall of the third ventricle of the brain, anterior to the pituitary gland. At the chiasma, fibres from the nasal portion of each retina cross to the optic tract of the opposite side, fibres from the temporal portion of the retina passing to the optic tract of the same side. Light rays from the temporal (lateral) visual field fall on the nasal retina; light rays from the nasal (medial) visual field fall on the temporal retina.
• Some optic tract axons bifurcate sending branches to the midbrain for visual reflexes.
• The optic tract extends from the chiasma to the lateral geniculate body with onward connections to the visual cortex in the occipital lobe (see Ch. 15).
Papilloedema
Since the optic nerve is surrounded by meninges and cerebrospinal fluid in the subarachnoid space, if pressure in the subarachnoid space rises, it will compress the optic nerve. This in turn compresses the central artery and vein, the vein being occluded before the artery because venous blood pressure is lower and venous walls are thinner. Blood will be able to enter the retina through the central artery but not leave through the central vein. This leads to venous engorgement and swelling of the head of the optic nerve which bulges into the vitreous, and a blurring of the edge of the optic disc. This is papilloedema. It is a reliable sign of raised intracranial pressure and is visible on retinoscopy, the only investigation where the clinician can directly inspect the central nervous system.
Retinal detachments
The two layers of the optic vesicle that give rise to the neural and pigment layers of the retina are contiguous rather than firmly attached. The potential space between them can open up in certain conditions, e.g. poor vascular perfusion. This is called retinal detachment, and it causes blindness.
Multiple sclerosis
In the optic nerve, which is a brain outgrowth, myelin is produced by oligodendrocytes. The nerve may thus be affected in demyelinating diseases such as multiple sclerosis. This is not so for other cranial nerves in which myelin is manufactured by Schwann cells.
Visual field defects
• Section of one optic nerve causes blindness in the ipsilateral eye. This is not common.
• Destruction of the crossing fibres in the chiasma, for example by an expanding pituitary tumour, causes blindness in the nasal retina of both eyes which gives a bitemporal hemianopia (field loss).
• Pressure on the lateral aspect of the chiasma (e.g. an internal carotid artery aneurysm) affects fibres from the temporal retina of the ipsilateral eye, giving an ipsilateral nasal hemianopia: this is uncommon. Bilateral internal carotid artery aneurysms would cause a binasal hemianopia: even more uncommon.
• Destruction of the pathway behind the chiasma would interrupt pathways from the temporal retina of the ipsilateral eye and the nasal retina of the contralateral eye. This would cause blindness in the same side of both visual fields: a homonymous hemianopia.
Clinical testing of II
So-called testing of the optic nerves usually means testing visual acuity and the visual fields. Visual acuity is tested with charts using print in standard sizes. Visual field assessments may be done by confrontation tests in which the examiner compares the patient’s visual fields with his own by moving the fingers in and out of the field of vision. They assume that the examiner’s visual fields are normal.
Visual reflexes
Pupillary light reflex (Fig. 14.39)
A light shone into either eye causes both pupils to constrict. This reflex is a crude test of brain stem function. It involves the optic nerve, optic chiasma, optic tract, midbrain and oculomotor nerve (parasympathetic components), ciliary ganglion and iris muscle. The reflex is described as consensual because commissural connections mean that when light is shone into one eye both pupils respond. The reflex does not involve cortical activity and may be performed on an unconscious subject: only at the deepest levels of unconsciousness is there no response. Fixed dilated pupils are those which do not respond to light: they are a likely indicator of brain death.
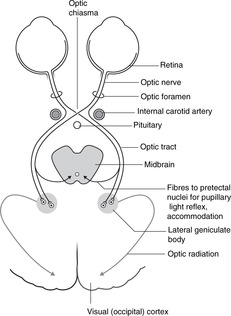 |
| Fig. 14.39 |
Accommodation reflex
Focusing on a near object and then looking away (or vice versa) results in changes of the size of the pupil (near: constricted; far: dilated) and the lens (near: fatter; far: thinner). In the accommodation reflex there is some degree of perception, unlike the pupillary light reflex, and thus the cerebral cortex is involved. There is also some voluntary control since you can decide to focus on a particular object. The precise pathways are not fully understood, but those given below are probable.
Retina → optic nerve → optic chiasma → optic tract → lateral geniculate bodies → visual cortex → frontal cortex → midbrain
Edinger–Westphal nuclei → III → ciliary ganglion → ciliary and iris muscles.
Argyll Robertson pupil (note: no hyphen). This is a pupil that accommodates but does not react to light. A comparison of the pathways for the accommodation reflex, which functions normally, and the pupillary light reflex, which does not, indicates that the lesion could be in (a) the fibres that pass from the optic tract to the midbrain, or (b) the midbrain.
14.12. Inside the skull, haemorrhages
You should:
• describe the layout of the cranial meninges and venous sinuses
• describe the principal arteries supplying skull bones, meninges and brain
• describe venous return from the cranial cavity
• explain the anatomy of extradural, subdural, subarachnoid and intracerebral haemorrhages
• list the principal cisterns of the cranial subarachnoid space.
Arteries
Meningeal arteries, extradural haemorrhage
Grooves are visible on the internal aspect of the skull bones. These are for meningeal veins and accompanying arteries that run between the dura and the periosteum of the skull bones. Although called meningeal, in fact these vessels are more important for supplying skull bones and diploic cavities than meninges. Several arteries give meningeal branches, but one in particular is important: the middle meningeal artery. It is a branch of the maxillary artery and enters the middle cranial fossa through the foramen spinosum. The anterior division of the artery passes deep to the pterion where the cranium is thinnest and an injury at this site may tear the artery causing an extradural haemorrhage. This may become quite large before it causes symptoms, and the interval between the injury and the appearance of symptoms is called the lucid interval. This is why patients with head injuries are often admitted to hospital for a brief period.
Internal carotid artery
At the top of the neck, the internal carotid artery enters the carotid canal in the temporal bone. In the canal the artery passes medially before turning upwards once more to enter the cranial cavity at the side of the sphenoid air sinus.
In the middle cranial fossa, the artery runs through the cavernous (venous) sinus, in and above which it describes an S-shaped course with VI on its lateral wall for a short distance. Above the sinus it gives off the ophthalmic artery to the orbit and eye and divides into its terminal branches, the anterior and middle cerebral arteries, as part of the arterial circle of Willis.
Vertebral artery
Having emerged from the transverse foramina of the cervical vertebrae, the vertebral arteries pass medially between vertebra C1 and the occipital bone, penetrate the dura and ascend through the foramen magnum. On the front of the brain stem they unite to form the basilar artery, which supplies the brain stem and inner ear. It terminates in the circle of Willis by dividing into the right and left posterior cerebral arteries.
Meninges, venous sinuses, subdural and subarachnoid haemorrhages (Fig. 14.40)
The meninges form sacs around the brain, the outer layer being the dura mater, the middle layer the arachnoid mater, and the inner layer, inseparable from the brain itself, the pia mater. Between the arachnoid and the pia is the subarachnoid space, which, like the spinal subarachnoid space with which it is continuous, contains cerebrospinal fluid. The arachnoid is a thin layer, loosely adherent to the inner aspect of the dura.
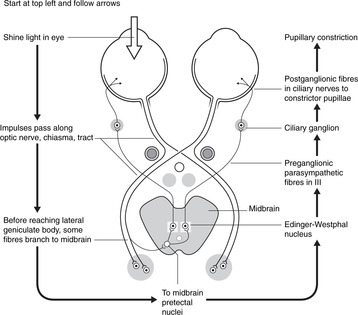 |
| Fig. 14.40 |
There is no cranial equivalent of the spinal extradural space. Unlike the spinal dura, the cranial dura is firmly adherent to the periosteum of the skull bones except at certain sites where they part company to enclose large endothelial venous channels, the venous sinuses. These are the principal collecting channels for venous blood from the brain. The margins of their attachment are clearly visible on the inside of the skull.
Beware. Regrettably, some people call the dura the ‘meningeal layer of dura’ and the periosteum of the skull bones the ‘periosteal layer of dura’. This terminology has nothing to recommend it.
Falx cerebri, tentorium cerebelli
From the larger venous sinuses at several sites, a double layer of dura projects into the cranial cavity. These dural folds form:
• The falx cerebri in the midline, which partially separates the cranial cavity into right and left halves and lies between the two cerebral hemispheres. It is attached to the ethmoid bone in front, the vault of the skull above and behind, and has a free inferior edge.
• The tentorium cerebelli, which is a more or less horizontally arranged sheet extending back from the ridge of the petrous temporal bone and the clinoid processes to the internal occipital protuberance. It forms a complete diaphragm over the posterior cranial fossa except for the tentorial notch, an anterior defect, through which the brain stem and surrounding nerves and vessels pass.
Venous sinuses
• The superior sagittal sinus is in the midline at the attachment of the falx cerebri to the skull vault. Blood in it drains posteriorly and at the internal occipital protuberance it normally turns to the right, becoming the transverse sinus. This passes forwards in the lateral attachment of the tentorium cerebelli to the edge of the petrous temporal bone. Here it curls down as the right sigmoid sinus, passes through the jugular foramen and becomes the right internal jugular vein.
• The inferior sagittal sinus is in the midline in the inferior free margin of the falx cerebri. Blood in it drains posteriorly and is joined at the tentorium/falx junction by blood from the great cerebral vein emerging from the back of the brain stem. These unite to form the straight sinus, which passes back in the attachment of the falx and the tentorium, and at the internal occipital protuberance normally turns to the left, becoming the left transverse sinus. The pattern then mirrors that on the right side, eventually forming the left internal jugular vein. Sometimes the pattern is reversed with the superior sagittal sinus turning left and the straight sinus turning right. At the internal occipital protuberance, the venous channels may communicate: this is the confluence of sinuses. The right-sided venous channels (from the superior sagittal sinus) are usually bigger than the left, with the right internal jugular vein bigger than the left. Indeed, the left internal jugular vein may even be absent altogether.
Arachnoid granulations (Fig. 14.41)
The dural walls of the sinuses, particularly the superior sagittal sinus, possess small defects which allow the underlying arachnoid to billow through into the sinus. These are the arachnoid granulations where only arachnoid and the endothelium of the sinuses separate cerebrospinal fluid from venous blood: they are the sites of reabsorption of cerebrospinal fluid. If the sinuses become thrombosed, reabsorption will be prevented and the pressure of cerebrospinal fluid in the subarachnoid space will rise.
Diaphragma sellae, pituitary fossa (Figs 14.5, 14.42)
This midline fossa directly above the sphenoid (nasal) sinus is guarded by the anterior and posterior clinoid processes, to which is attached the diaphragma sellae, a sheet of dura pierced by the pituitary stalk and isolating the pituitary gland below from the subarachnoid space above. There is neither subarachnoid space nor cerebrospinal fluid below the diaphragma, a fact that surgeons are glad of when performing transnasal approaches to the pituitary (see section 14.9, p. 280).
Cavernous sinus (Fig. 14.42)
Venous blood from the cranial cavity also passes through the foramen magnum to join the internal vertebral venous plexus of the spinal column. This is important if the internal jugular veins become blocked or if they have to be ligated.
Sensory innervation of the dura
Sensory fibres from several nerves innervate the dura. These may be given off as they leave the skull, or they may re-enter the skull through small foramina. The dura is sensitive to pain and stretching. Meningeal branches of the following nerves supply the dura:
• anterior cranial fossa: ethmoidal nerves Va; branches of Vb
• middle cranial fossa: branches of Vb, Vc
• posterior cranial fossa: branches of X and C1, 2.
Intracranial haemorrhages
Subdural. The walls of the venous sinuses are pierced by numerous small veins which pass directly from the brain substance into the sinuses. With advancing years, the brain shrinks so these veins become stretched, rendering them more susceptible in the old than in the young to tearing as a result of sudden jolts of the head. In such cases, the veins rupture immediately before entering the venous sinuses so blood seeps between the dura and arachnoid (which are normally in contact). This is a subdural haemorrhage.
Subarachnoid. Subarachnoid haemorrhages occur when an artery in the subarachnoid space (e.g. an artery of the circle of Willis or one of its branches) ruptures, discharging blood into the cerebrospinal fluid. It is sudden and often fatal, and is the commonest cause of sudden death in young adults.
Cerebral. And, for the sake of completeness, (intra) cerebral haemorrhages are bleeds of arteries within the brain substance. These may be either imperceptible in their effects, or have devastating effects depending not just on size but also on what structures are damaged or deprived of a blood supply. These are responsible for what is usually called a stroke.
The anatomy of both extracranial and intracranial haemorrhages is summarised in Table 14.4.
| Position | Usual nature (arterial or venous) | Things to remember |
|---|---|---|
| Extracranial | ||
| Subaponeurotic | Either | Scalp wound which also tears the epicranial aponeurosis, unlimited except by occipitofrontalis attachment, periorbital tracking |
| Subperiosteal | Either | Birth injuries, assumes shape of underlying bone |
| Intracranial | ||
| Extradural | Arterial | Head injury, pterion, middle meningeal artery |
| Subdural | Venous | Old people |
| Subarachnoid | Arterial | Anyone, often (?usually) fatal |
| Cerebral | Arterial | Arterial, stroke, usually disabling |
Cranial subarachnoid space, cisterns
• The cranial subarachnoid space extends laterally for a short distance as each cranial nerve passes through its skull foramen. This is for no more than a millimetre or so except for two nerves:
– the trigeminal, where the extension of subarachnoid space partially encloses the trigeminal sensory ganglion and is known as the trigeminal (Meckel’s) cave
– the vestibulocochlear, where the extension passes for some distance into the internal acoustic meatus.
14.13. Sympathetic impulses to the head
Sympathetic impulses do not emerge from the central nervous system in cranial nerves, but only in thoracolumbar segments of the spinal cord.
• Preganglionic impulses to the head arise in the lateral grey horn of spinal cord segments T1 and/or T2. They pass into the spinal nerve(s) and white rami communicantes to the sympathetic chain at the T1 ganglion, adjacent to the neck of the first rib. Preganglionic axons for cranial structures do not synapse here, but ascend in the chain behind the carotid sheath and synapse (usually) in the superior cervical ganglion immediately below the base of the skull.
• Postganglionic fibres reach their target organs by one or more of the following pathways:
– With arteries and their branches. Fibres pass to the neighbouring carotid and vertebral arteries forming a plexus in their walls, and are distributed with their branches to intracranial structures, the eye, orbit and skin.
– Cavernous sinus. As the internal carotid artery passes through the cavernous sinus, postganglionic sympathetic fibres may pass to VI (on the artery) or in fibrous strands to the lateral wall and III, IV and Va, providing another route to the orbit and eye and through branches of Va to the scalp.
– Deep petrosal nerve. The deep petrosal nerve leaves the plexus around the internal carotid artery in the carotid canal, and joins the greater petrosal nerve to form the nerve of the pterygoid canal. It enters the pterygopalatine fossa and is distributed in branches of Vb to the nose, pharynx, palate and face.
Single best answer questions
For each numbered question, only ONE of the options lettered a–d is correct.
16. Concerning the neck and thyroid gland:
a. a branchial cyst moves upwards when the tongue is protruded.
b. the accessory nerve lies deep in the posterior triangle and is not easily damaged.
c. the bifurcation of the common carotid artery is at about the level of the hyoid bone.
d. the isthmus of the thyroid gland usually overlies the thyroid cartilage.
17. Blood in the inferior thyroid artery comes from which of the following arteries:
a. axillary.
b. external carotid.
c. internal carotid.
d. subclavian.
18. Concerning the scalp:
a. a subaponeurotic haematoma may track in all directions except anteriorly.
b. branches of the ophthalmic nerve supply as far back as the vertex.
c. it is supplied with blood only from branches of the internal carotid artery.
d. vessels and nerves lie deep to the epicranial aponeurosis.
19. In the oral cavity and pharynx:
a. calculi are more likely in the parotid duct than in the submandibular duct.
b. enlarged adenoids may block the Eustachian tube.
c. the parotid duct opens opposite the third lower molar tooth.
d. the submandibular duct is intimately related to the facial nerve.
21. In the nasal cavity and sinuses:
a. Little’s area is on the lateral wall of the nasal cavity.
b. the maxillary sinus opens into the inferior meatus.
c. the Eustachian tube opens into the middle meatus.
d. the sphenoid sinus is immediately below the pituitary fossa.
22. Concerning the larynx and associated structures:
a. during quiet breathing the vocal cords are fully abducted.
b. the piriform fossa is part of the larynx.
c. the sensory nerve supply of the larynx is entirely from branches of the vagus nerve.
d. the true vocal cords are at the level of the cricoid cartilage.
23. Concerning the visual apparatus:
a. the ophthalmic artery is a branch of the external carotid artery.
b. a lesion of the sixth cranial (abducens) nerve causes lateral deviation of the eyeball.
c. alteration of the iridocorneal angle may hinder reabsorption of aqueous humour.
d. the posterior chamber of the eye is posterior to the lens.
24. An intact pupillary light reflex demonstrates the integrity of the:
a. pons.
b. midbrain.
c. Va.
d. optic tract.
25. An intact corneal reflex depends upon the integrity of the:
a. facial motor nucleus and trigeminal ganglion.
b. lateral geniculate body.
c. trigeminal motor nucleus and geniculate ganglion.
d. oculomotor nerve.
26. Section of the left facial (seventh cranial) nerve at the stylomastoid foramen:
a. prevents parotid secretion on the left side.
b. abolishes the pupillary light reflex on the left side.
c. causes hyperacusis on the left side.
d. paralyses orbicularis oris on the left side.
27. The hypoglossal (twelfth cranial) nerve:
a. if sectioned, causes deviation of the protruded tongue away from the side of the lesion.
b. carries sensory fibres from tongue muscles.
c. passes through the parotid gland.
d. is vulnerable in carotid artery surgery.
28. The anterior fontanelle:
a. lies between parietal and occipital bones.
b. is not present at birth.
c. closes within 6 months of birth.
d. overlies the superior sagittal sinus.
29. Which cranial nerve arises as stated:
a. III: midbrain interpeduncular fossa.
b. V: dorsal midbrain.
c. VI: cerebellopontine angle.
d. X: medulla, medial to olive.
30. The cavernous sinus:
a. contains the external carotid artery.
b. is intimately related to cranial nerves Vc, VII.
c. is intimately related to cranial nerves III, IV, Va and VI.
d. is inferior to the sphenoid sinus.
Matching item questions
Questions 31–35: cranial nerves
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. maxillary nerve (Vb)
b. mandibular nerve (Vc)
d. glossopharyngeal nerve (IX)
e. vagus nerve (X)
31. smiling.
32. mastication.
33. blinking.
34. parotid salivation.
35. toothache from the upper molars.
Questions 36–40: haemorrhages
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. injury to the pterion
b. venous bleed
c. adopts shape of underlying bone
d. blood from vertebral artery
e. extracranial haemorrhage
36. subperiosteal haemorrhage.
37. extradural haemorrhage.
38. subdural haemorrhage.
39. subaponeurotic haemorrhage.
40. subarachnoid haemorrhage.
Questions 41–46: blood vessels
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. branch of axillary artery
b. branch of common carotid artery
c. branch of external carotid artery
d. branch of internal carotid artery
e. branch of subclavian artery
41. facial artery.
42. inferior thyroid artery.
43. internal thoracic artery.
44. maxillary artery.
45. superior thyroid artery.
46. vertebral artery.
Questions 47–52: venous sinuses
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. inferior sagittal sinus
b. sigmoid sinus
c. straight sinus
d. superior sagittal sinus
e. transverse sinus
47. becomes internal jugular vein.
48. between confluence and sigmoid sinus.
49. formed by union of inferior sagittal sinus and great vein (of Galen).
50. in inferior margin of falx cerebri.
51. in junction of falx and tentorium cerebelli.
52. underlies anterior fontanelle in a baby.
Questions requiring short answers
53. Thugs wielding a knife attack a young lady. She is stabbed in the middle and lower parts of the posterior triangle of the neck. Which structures are at risk of damage? Give surface markings, and symptoms that would result from damage to any nerves you name.
54. A patient has a swelling between the left mandible and the ear, which is increasing in size. After a few weeks, the patient notices difficulty in closing the lips for whistling, and before long starts to dribble from the left corner of the mouth. Explain what is going on, giving as much information as you can about any nerve you name.
55. Give the lymph drainage and innervation of the tongue.
56. Briefly describe or draw the anatomy of the submandibular gland and duct. At operation, the surgeon must be careful of certain nerves when (a) making the incision; and (b) handling the duct. Name the nerves, give their function, and explain the results of damage.
57. Describe the blood supply of the scalp and explain why scalp lacerations can lead to a black eye.
58. A blow on the head results in clear fluid dripping from the nose. Explain what has been fractured and/or torn, what is the fluid and what may be a permanent symptom as a result of this injury.
60. A patient presents with a cough and hoarse voice. A chest radiograph reveals a left-sided tumour in the region of the pulmonary artery and aortic arch. Briefly describe the anatomy of this region and explain the voice change. Add a note on relevant embryology.
61. What is the middle ear? What major nerve could be affected by a severe middle ear infection? How would you recognise this?
62. Give the sensory innervation of the external aspect of the tympanic membrane and explain why earache may occur in the absence of ear disease.
Single best answers
16. c.
17. d. By means of the thyrocervical trunk.
18. b.
19. b.
20. d.
21. d.
22. c.
23. c.
24. b.
25. a.
26. d.
27. d.
28. d.
29. a.
30. c.
Matching item answers
31. c.
32. b.
33. c.
34. d.
35. a.
36. c.
37. a.
38. b.
39. e.
40. d.
41. c.
42. e. By way of thyrocervical trunk.
43. e.
44. c.
45. c.
46. e.
47. b.
48. e.
49. c.
50. a.
51. c.
52. d.
Short answers
53. The following structures are at risk of damage: XI, apex of lung, upper trunk of brachial plexus, branches of thyrocervical trunk, possibly even subclavian vessels. Surface markings of XI are: one-third of way down sternocleidomastoid – one-third of way up trapezius. Damage to this nerve would result in paralysis of trapezius, inability to abduct the shoulder beyond about 90° (although that might be the least of her problems). Pneumothorax and blood loss might be more urgent.
54. VII is the thing that matters. Parotid tumour invades branches of VII causing lower motor neuron lesion of VII and facial paralysis or weakness. You could mention other structures that pass through the parotid if you wish, and give other details of VII (cerebellopontine angle, internal acoustic meatus, temporal bone, middle ear).
55. The important things are:
• Lymph drainage: from the tip to the submental nodes; from the sides to the submandibular nodes of that side with the central portion to both sides; from the posterior tongue to both sides
• Innervation: deep cervical chain.
56. You should include the lingual nerve and its relation to the duct. Damage to it would mean loss of all sensation on the anterior tongue, and loss of some salivation in the sublingual glands (would one notice?).
57. There is no bony attachment of the epicranial aponeurosis anteriorly, so there is nothing to stop blood tracking down into the periorbital tissues. It might take a few days.
58. The cribriform plate of ethmoid has been fractured with tearing of the dura and arachnoid mater, so CSF drips out (rhinorrhoea). The olfactory nerve filaments may also be torn, so there may be post-traumatic anosmia (not post-traumatic amnesia as a student once told me, though you might have this as well!).
59. The thing is that the vocal cords are at the level of the middle of the thyroid cartilage. It is usually the vocal cords that are the site of obstruction, so at laryngotomy you need to make a hole below them. It is no use making a hole in the thyrohyoid membrane, above the cords: use the cricothyroid membrane, which is, unfortunately, slightly more difficult to find than the thyrohyoid membrane.
60. There has been damage to the recurrent laryngeal nerve, which arises in the mediastinum. Revise the mediastinum.
61. The middle ear or tympanic cavity is an extension of the upper respiratory tract from the nasopharynx, and includes the Eustachian tube, middle ear proper and mastoid antrum. It contains the ossicles and is bounded laterally by the tympanic membrane. The facial nerve (VII) is closely related to it, and a facial weakness or palsy might be caused by a severe middle ear infection that affects the nerve.
62. Sensory innervation of the external aspect of the tympanic membrane: Vc (about three-quarters), X (about one-quarter). Referred pain can arise from structures supplied by Vc (lower teeth, tongue, mouth); and from structures supplied by X (larynx, pharynx, trachea). Earache in a patient with normal tympanic membranes might result from disease of the mouth, tongue, pharynx, or larynx because of common innervation by branches of mandibular (mouth, tongue) and vagus (larynx, pharynx) nerves.