Chapter 73 Support of the failing liver
The Failing Liver
A failing liver is a serious condition that warrants a multimodal approach. The best option for a failing liver from either acute liver failure (ALF) or decompensated liver failure, is liver transplantation (Burroughs et al, 2006). However, the rapidity of progression and variable course of ALF, which includes progression to hepatic coma and the possibility of cerebral herniation, limit the effectiveness of transplantation. Furthermore, the downside of orthotopic liver transplantation is lifelong immunosuppression, and the side effects of these drugs include nephrotoxicity, diabetes mellitus, and infections.
The incidence of ALF in the United States is 2000 to 3000 persons per year (Ostapowicz et al, 2002), but the number is much higher for patients with acute decompensation of chronic liver failure (>200,000). The outcome of ALF varies by etiology: those with favorable prognoses are acetaminophen overdose, hepatitis A, and ischemia, with approximately 60% spontaneous survival (Lee et al, 2008). Etiologies with poor prognoses are drug-induced ALF, hepatitis B, and idiopathic cases, with approximately 25% spontaneous survival.
Medical Therapy
Once a patient is diagnosed with ALF, medical management must be initiated in a coordinated, systematic fashion (see Chapter 72). The goals of medical management are to 1) facilitate recovery, 2) reduce ongoing liver injury with N-acetyl cysteine, 3) prevent systemic manifestations such as cerebral edema, 4) correct hemodynamic instability, and 5) start preparing for liver transplantation if necessary. Treatment measures are initiated according to the severity of hepatic encephalopathy (HE).
For patients in stage I HE, evidenced by behavior changes with no changes in consciousness, baseline laboratory values are obtained for serum electrolytes, Mg2+, Ca2+, lactate, arterial blood gases, liver function tests, lactate dehydrogenase (LDH), ammonia, complete blood count (CBC), albumin, and coagulopathy panel. Twice-daily glucose checks are also recommended. Vitamin K is administered to help prevent or correct coagulopathy (Pereira et al, 2005), and lactulose is given orally for at least two loose stools per day because elevated blood ammonia can be detrimental. Ulcer prophylaxis is also started (Macdougall et al, 1977). Therapeutic measures are initiated when indicated, such as N-acetyl cysteine for acetaminophen overdose (Smilkstein et al, 1988).
If a patient progresses to stage II HE—with disorientation, delayed mentation, and asterixis—the measures for stage I HE are continued, and the patient is transferred to the intensive care unit (ICU) for a multidisciplinary evaluation from a critical care intensivist or hepatologist in consultation with a neurologic intensivist and a liver transplant surgeon. The patient’s level of consciousness is scored using both the Glasgow Coma Scale and the Mayo Clinic FOUR (Full Outline of UnResponsiveness) score (Wijdicks et al, 2005). Laboratory work obtained for stage I HE patients is continued on a routine schedule.
A head computed tomographic (CT) scan or a magnetic resonance image (MRI) scan is obtained to evaluate brain edema and rule out other causes for mental status change, such as hematoma. Depending on the clinical picture, either enteral or parenteral nutrition is begun, with a protein load not to exceed 0.5 g/kg/day and with caloric intake based on Harris-Benedict guidelines: ideal body weight plus 20%. Branched-chain amino acids (HepatAmine) are used at the discretion of dietetics, and antifungal and antiviral prophylaxes are considered because of the high incidence of opportunistic infections in the setting of ALF (Rolando et al, 1996). If these patients require sedation, we advocate the use of the short-acting agent propofol (Wijdicks et al, 2002).
As patients progress to stage III HE, endotracheal intubation is performed to protect the airway and initiate mechanical ventilation. Goals of ventilatory support are to maintain a PaO2 greater than 70 mm Hg, preferably using an FiO2 less than 40%. Mannitol is used to control intracranial pressure, with a goal serum osmolality of 310 to 320 mEq/L (Canalese et al, 1982); it is discontinued if oliguria develops. Simple maneuvers are initiated to lower intracranial pressure (ICP), such as keeping the head of the bed elevated between 30 and 45 degrees, limiting endotracheal suctioning, decreasing stimuli from lighting, and controlling agitation with propofol. IV fluids are adjusted to maintain serum Na+ between 140 and 150 mEq/L. Vasopressors are used to increase the mean arterial pressure (MAP) if the cerebral perfusion pressure (CPP) falls below 60 mm Hg. Vasodilators are used to decrease MAP if the CPP is above 100 mm Hg. More invasive monitoring systems are also instituted, including an arterial line and an ICP monitor (Vaquero et al, 2005). Prior to ICP monitor placement, a coagulation profile is obtained and INR is corrected to 1.5 or less with fresh frozen plasma. If correction requires large volumes of fresh frozen plasma, we consider the addition of recombinant Factor VII (Shami et al, 2003). The cerebral perfusion pressure (CPP = MAP − ICP) is maintained between 60 and 100 mm Hg. If the CPP falls below 60 mm Hg or the ICP rises above 20 mm Hg for more than 5 minutes, the patient is hyperventilated to a PaCO2 of 25 to 30 mm Hg (Strauss et al, 1998). Hyperventilation is only maintained short term.
Intracranial hemorrhage must be excluded if ICP remains high. Ultrasounds to assess hepatic mass and vasculature are obtained every 2 days. Hemodynamic instability often occurs secondary to a systemic inflammatory response (Rolando et al, 2000) or intravascular depletion. Intravascular volume is monitored with a Foley catheter for continuous urine output assessment and either a central venous or pulmonary artery catheter and is maintained for adequate end-organ perfusion. Human 5% albumin is the volume expander. Continuous venovenous hemodialysis is preferred in renal failure and ALF because of the risk of hypothermia and reduced CPP during intermittent hemodialysis (Davenport et al, 1993).
Hypothermia (33° to 35° C) is considered if cerebral edema is refractory to other therapies (Jalan et al, 2004). The duration has not been standardized, although some centers discontinue hypothermia before transplantation because of the risk of bleeding. Other centers continue hypothermia for 24 hours after transplantation because of late risks of cerebral edema.
Nonbiologic Liver Support
Plasma Exchange and Hemodiafiltration
Plasma exchange was a natural outgrowth of the less effective blood-exchange transfusion technique. The goals of plasma exchange in ALF are to reduce the level of circulating toxins and to replace deficient essential factors, such as clotting factors produced by the liver. Plasma exchange is achieved by apheresis, with removal of the patient’s jaundiced plasma and replacement with normal plasma. The results of early clinical trials were discouraging; encephalopathy often improved temporarily, but patient survival was not affected. Therapeutic gains, such as reduction in serum bilirubin and partial recovery from coma, were short lived and seen predominantly in patients with drug-induced ALF (Freeman et al, 1986; Lepore et al, 1972; Sabin et al, 1968). The overall survival rate of ALF patients treated by plasma exchange remained less than 50% (Takahashi et al, 1991). In addition, a significant complication rate was reported with plasma exchange, including chemical toxicity, viral infections, and death from lung and brain complications (Brunner et al, 1987). However, the effects of repeated, high-volume plasma exchange in patients with ALF have been studied under nonrandomized conditions (Kondrup et al, 1992).
In 1999, Clemmesen and colleagues investigated the effect of repeated, high-volume (15% of body weight) plasma exchange in 23 patients: 14 patients with ALF and 9 with decompensated cirrhosis (Table 73.1). The etiologies of ALF were acetaminophen in 8, hepatitis in 3, and nonhepatitis (A, B, C) in 3. Of the patients with acetaminophen intoxication, 25% died, and 21% were bridged to transplantation.
Table 73-1 Overview of Important Biologic and Nonbiologic Extracorporeal Liver Support Device Trials
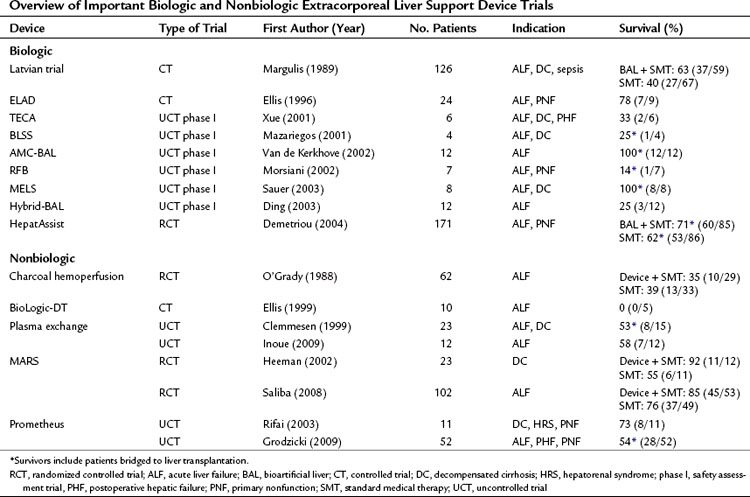
In Japan, where the option of liver transplantation is limited by the low rate of cadaveric organ donation, a dual approach that combines hemofiltration with plasma exchange has become popularized as a treatment of ALF (Inoue et al, 2009). In this Japanese study, all patients regained consciousness, and no patient developed brain edema or hepatorenal syndrome during plasma exchange and hemodiafiltration treatment. The median number of treatment sessions was 21 (range, 4 to 30), and 4 of 7 patients (57%) with indeterminate etiology and 1 of 5 patients (20%) with acute hepatitis B infection survived.
Historic Blood Purification Options
Throughout the 1960s and 1970s, it was believed that small (<5 kD) dialyzable molecules caused coma in ALF (Kiley et al, 1956; Opolon, 1979). As a result, numerous attempts were made to treat ALF patients with hemodialysis (Kiley et al, 1958; Merrill et al, 1950) and charcoal hemofiltration (O’Grady et al, 1988) for removal of these small toxins. Although case reports and controlled studies of both therapies have shown reversal of hepatic encephalopathy and improved survival (Gimson et al, 1982; O’Grady et al, 1988), neither therapy has been proven successful in prospective randomized trials of either ALF or decompensated cirrhosis.
MARS
MARS was developed by Stange and collegues (1993) in the early 1990s. Briefly, MARS is a two-circuit system composed of a blood circuit and a secondary albumin circuit; these are separated by a high-flux dialyzer membrane with a pore size and nominal molecular weight cutoff (MWCO) of approximately 50 to 60 kD. The pore size of this membrane makes it impermeable to albumin but permeable to smaller water and nonpolar waste substances. On the opposing side of this membrane is an albumin circuit that consists of supraphysiologic levels (>10%) of human albumin dialysate. Waste removal occurs by the concentration gradient between the patient’s blood and the albumin dialysate in the secondary circuit. The high concentration of albumin is believed to facilitate removal of nonpolar molecules known to bind to albumin. Detoxification of these nonpolar waste molecules occurs when the albumin passes over adsorbent columns, including an anion exchange resin column and an activated charcoal column (Steiner et al, 2004). The secondary circuit also provides conventional low-flux dialysis for detoxification of water-soluble molecules.
One of the earlier MARS trials was an uncontrolled trial of 13 patients who had not responded to standard medical treatment of decompensated liver failure (Stange et al, 1999). The etiologies of liver cirrhosis were hepatitis C in one patient and alcohol abuse in the rest; the precipitating events were unknown in 10 cases. This early uncontrolled study showed an overall survival of 69% (9 of 13). A prospective, controlled trial of the MARS system (n = 12) versus standard medical therapy (n = 11) was performed by Heemann and colleagues (2002) in patients with decompensated cirrhosis. The authors concluded that albumin dialysis was associated with a significant improvement in 30-day survival (11 of 12 survived with MARS, 6 of 11 survived in the control group). An editorial to this study raised concerns regarding stratification, standard medical care before randomization, and the inclusion criteria (Kamath, 2002). A larger randomized controlled trial of the MARS system plus standard medical therapy (n = 39) versus standard medical therapy alone (n = 31) in the treatment of hepatic encephalopathy in advanced cirrhosis was reported by Hassanein and colleagues (2007). In contrast to previous reports on MARS, mostly from European centers, this trial was conducted mostly at centers in the United States. This trial demonstrated that the use of MARS therapy was associated with an earlier and more frequent improvement of grades 3 and 4 hepatic encephalopathy compared with standard medical therapy alone. This 5-day trial did not attempt to assess the role of MARS therapy on survival or cirrhotic patients. A trial that did evaluate survival was reported by Saliba and colleagues (2008). This randomized prospective trial of MARS in the treatment of ALF included 102 patients randomized to MARS therapy (n = 53) or standard medical treatment alone (n = 49). Survival at 6 months was greater after MARS treatment (84.9% vs. 75.5%); however, this difference did not reach a significant level by log rank test.
Along with hepatic encephalopathy, MARS has been shown to improve other secondary end points associated with a failing liver, including renal dysfunction, jaundice, and hemodynamic parameters such as systemic vascular resistance and mean arterial pressure (Schmidt et al, 2003). One prospective randomized controlled trial showed significant improvement in survival in patients with hepatorenal syndrome (Mitzner et al, 2000). MARS therapy has been associated with prolonged relief of intractable pruritus in patients with cholestatic liver disease (Pares et al, 2004). In addition, in a study by Novelli and colleagues (2007), MARS therapy was associated with an improvement in Model of End-Stage Liver Disease (MELD) scores at 1 and 3 months after treatment.
A meta-analysis of MARS use evaluated patients with ALF or decompensated cirrhosis in four randomized clinical trials involving 67 patients and two nonrandomized trials involving 61 patients. This meta-analysis failed to show a significant survival benefit with MARS treatment (Khuroo et al, 2004). As a result, many clinicians are still hesitant to use MARS therapy on their patients with liver failure because a reproducible survival benefit has not been shown.
Prometheus
Prometheus is another form of albumin dialysis for supporting a failing liver. Prometheus functions by fractionating the plasma component of blood, in which the fractionated plasma is detoxified as it passes through two adsorption columns. Prometheus and MARS differ in the MWCO of their blood-separation membranes. MARS uses a 50- to 60-kD MWCO membrane that does not allow passage of albumin from the blood, whereas Prometheus uses a membrane with a 250-kD MWCO that allows the passage of albumin. Therefore greater potential removal of albumin-bound toxins from the patient’s blood is possible with the Prometheus system (Rifai et al, 2003). There have been concerns of dropping the patient’s albumin levels using Prometheus (Krisper et al, 2007) and concerns of losing clotting factors, presumably because of reduction in protein C and protein S concentrations after the fractionation and adsorption process (Meijers et al, 2007). As with MARS, a survival advantage of Prometheus over standard medical therapy has not yet been shown in a prospective randomized trial.
Biologic Liver Support
Ex Vivo Liver Perfusion
In 1965, Eiseman and colleagues reported the use of xenoliver (porcine) cross-perfusion to treat eight comatose patients. None of these patients survived, but transient clinical improvement, such as awakening from the comatose state, was reported. Later, in 1967, Burnell and colleagues reported the use of human-human cross-circulation in the treatment of three patients with fulminant hepatic failure. Moreover, livers from a variety of species—porcine, dog, and bovine—have been used (Abouna et al, 1970; Chari et al, 1994; Eiseman et al, 1965). Evident after the treatments were symptoms of hyperacute rejection—gastrointestinal bleeding, hemolysis, and thrombocytopenia—and less specific symptoms such as fever and nausea that would subside after each session. Human organs found not to be suitable for transplantation were used in a cross-perfusion setting reported in 1993; in this study, two of three patients were successfully bridged to transplantation, but the last patient did not improve clinically (Fox et al, 1993).
Hepatocyte Transplantation
Transplantation of liver cells, specifically hepatocytes, is promising for patients with inherited liver disorders such as tyrosinemia (Grompe et al, 1994) and hyperbilirubinemia Crigler-Najjar syndrome (Fox et al, 1998), which eventually lead to liver failure.
The possibility of treating liver insufficiencies with hepatocyte transplantation has been investigated over the years. The infusion of purified glucocerebridase in patients with enzyme disorders such as Gaucher disease have been attempted (Brady et al, 1974). Allogeneic hepatocyte transplantation to animals with enzyme deficiencies is a promising option. Studies in 1976 and 1977 showed conjugation of bilirubin in Gunn rats with deficiency in the enzyme uridine diphosphate glucoronyltransferase after alloinfusion of functional hepatocytes in the portal vein (Matas et al, 1976) and both the portal vein and intramuscularly (Groth et al, 1977). Later, a group at University of Minnesota (Sutherland et al, 1977) transplanted hepatocytes both intraportally and intraperitoneally in rats to support the recovery of hepatic necrosis (i.e., acute liver failure induced by dimethylnitrosamine).
Experimental models of liver failure and genetic defects of liver metabolism indicate that transplanted hepatocytes can assume the full range of functions of intact whole livers (Arkadopoulos et al, 1998). Intraportal infusions of hepatocytes in humans succeeded the intraportal infusion of purified enzymes. A limiting factor of enzyme therapy has been only short-term efficacy; the indications for hepatocyte transplantation with functionally intact hepatocytes have been liver failure (Habibullah et al, 1994), as a bridge to liver transplantation because of a failing liver (Strom et al, 1997), treatment of ornithine transcarbamylase deficiency (Horslen et al, 2003), and allogeneic hepatocyte transplantation in humans via the portal vein for Crigler-Najjar syndrome type 1 (Fox et al, 1998). These disorders have been partially corrected by hepatocyte transplantation, and these attempts have shown a proof of principle for cell transplantation therapy despite the effects being only short term (Strom et al, 2006).
Extracorporeal Hepatocyte Systems
To achieve these effects, an artificial liver should be able to lower blood levels of substances toxic to the brain, liver, and other organs, and it should provide whole liver functions that are impaired or lost. The concept of an artificial liver was developed by Sorrentino (1956), who demonstrated more than 50 years ago that fresh liver tissue homogenate converts urea from ammonium chloride and metabolizes ketone bodies, barbiturates, and salicylic acid. However, it was not until the mid-1970s that Wolf and Munkelt (1975) placed hepatoma cells in the extrafiber space of the hollow-fiber cartridge and showed that an extracorporeal device was capable of performing liver-specific functions, such as conjugating bilirubin.
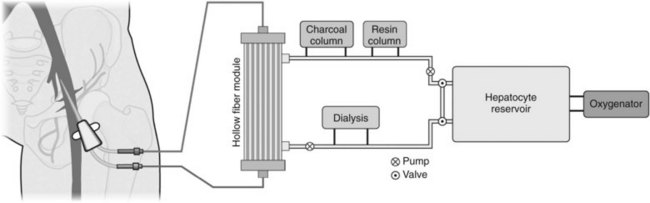
The first clinically applied BAL support was by Matsumura and colleagues (1987) in California, and the first BAL recipient was a 45-year-old patient in hepatic failure because of an inoperable bile duct carcinoma. The device contained isolated rabbit hepatocytes separated from the patient’s blood by a dialysis membrane. Figure 73.1 depicts a schematic overview of a generic BAL.
Clinical Trials of Bioartificial Liver Devices
Nine BAL devices have been evaluated in clinic trials (see Table 73.1). The different systems differ in perfusion rate, cell source, and duration of treatment (continuous vs. intermittent).
Latvian Hybrid Bioreactor Trial
A controlled study with 126 patients from Latvia in the former Soviet Union compared two groups: one group received standard medical treatment (n = 67), and a second group received standard medical treatment and BAL therapy (n = 59) (Margulis et al, 1989). The indications were liver failure caused by viral and toxic etiologies and decompensated alcoholic cirrhosis and sepsis. The device contained pig hepatocytes in liquid suspension along with activated charcoal granules. The 20-mL device was perfused through an external Scribner atrioventricular shunt (i.e., no external pump was applied). The results from this trial are admirable: 63% survival in the BAL-treated group as opposed to 41% in the control group. Of note, there was a selection bias, with 44% comatose patients in the control group as opposed to 33% in the BAL-treated group.
HepatAssist System
The first BAL device to be evaluated in a randomized prospective trial was the HepatAssist System (Circe Biomedical, Lexington, MA) (Demetriou et al, 2004). This was the first biologically based liver-assist device to be tested in an FDA-approved phase II/III trial. This trial enrolled a total of 171 patients, 86 controls and 85 BAL treated. The 30-day survival was 71% for the BAL group and 62% for the control group that received standard medical treatment. A trend was seen toward a better survival in the BAL group, although this difference did not reach statistical significance. Significant improved survival was found in a subgroup of patients with known etiology of ALF treated with BAL. Side effects of ALF included thrombocytopenia, renal failure, and increased intracranial pressure. These were higher in the controls, but the difference did not reach statistical significance. The authors of this proof-of-concept xenogeneic study concluded that the HepatAssist System was safe with regard to zoonosis; all the patients tested negative for porcine endogenous retrovirus after treatment. The HepatAssist System used a hollow-fiber–based configuration with membrane pore size of approximately 0.15 µm to separate the patient’s plasma from 7 billion primary porcine hepatocytes in the device. The plasma circuit of the BAL also included a charcoal column and an oxygenator. The future of this system may include a scaled-up version of the device loaded with 14 billion cryopreserved hepatocytes (approximately 140 g) under the new name HepaLife (www.hepalife.com).
Extracorporeal Liver-Assist Device
After several early case reports, the extracorporeal liver-assist device (ELAD) was evaluated by Ellis and colleagues (1996) in a controlled trial of patients with ALF. Two groups of patients were studied: those judged to still have a potentially recoverable lesion (group 1, 17 patients) and patients who already fulfilled criteria for transplantation (group 2, 7 patients). Patients were randomly allocated to BAL treatment or control. The etiologies of ALF were acetaminophen overdose in 17 cases, non-A non-B fulminant viral hepatitis in 5 cases, and hepatotoxicity from antituberculous chemotherapy in 2 cases. Of those who received BAL treatment, 7 (78%) of 9 survived compared with 6 (75%) of 8 in the control group (group 1). Only 1 (33%) of 3 patients from group 2 who received BAL treatment survived compared with one 1 (25%) of 4 in the control group. Biologic activity in the ELAD device was provided by a human hepatoblastoma cell line (C3A) loaded in a hollow-fiber cartridge. Later, Millis and colleagues (2002) reported a study of five ALF patients whose etiologies of liver failure were idiopathic, adverse drug reactions to leukemia treatment, and autoimmune hepatitis. This ELAD device differed from the device used by Ellis and colleagues in 1996 in that four cartridges loaded with hepatoma cells were used by Millis, whereas Ellis only used one cartridge. All patients in the Millis study were successfully bridged to transplantation, and the 30-day mortality rate was 20% (1 patient died). Each ELAD cartridge contained approximately 100 g of C3A cells within the extracapillary space of the hollow-fiber cartridges (a total of 400 g). The membrane used to generate the ultrafiltrate from the patient’s blood had a MWCO of 120 kD.
The most recent trial of ELAD (Vital Therapies, San Diego, CA) was reported as an abstract in 2007 (Duan et al, 2007). In that study, 54 patients with decompensated cirrhosis participated in a randomized controlled trial in which ELAD was tested at two different centers in China. The end point was 30-day survival. A significant difference was reached between the control group, with 47% (9 of 19) survival, and the ELAD-treated group, with 86% (30 of 35) survival. A third generation of ELAD will be evaluated in upcoming trials and will include a total of 440 g of C3A cells and increased fiber porosity, from 120 kD to 0.2 µm (www.vitaltherapies.com).
TECA-Hybrid Artificial Liver Support System
The TECA-Hybrid Artificial Liver Support System was tested in a clinical trial (a phase I safety trial) that included six comatose patients with liver failure; isolated primary porcine hepatocytes were used (Xue et al, 2001). The indications were variable and included ALF, decompensated cirrhosis, and postoperative hepatic failure after resection for biliary cancer. The survival rate was at least 33% (2 of 6), and none of the patients was listed for transplantation. The authors applied a hollow-fiber configuration in which plasma circulated inside the hollow fibers with the primary porcine hepatocytes on the outside of the hollow fibers.
Bioartificial Liver Support System
The Excorp Medical (Minneapolis, MN) Bioartificial Liver Support System (BLSS) was evaluated in four patients, two with ALF and two with decompensated cirrhosis (Mazariegos et al, 2001). The etiologies behind ALF were acetaminophen toxicity and adverse effects of chemotherapy, but the etiologies behind the decompensated cirrhosis were Wilson disease and alcoholic hepatitis. One patient was bridged to auxilliary liver transplantation, but the other three did not survive (25% survival). The device contained approximately 120 g primary porcine hepatocytes in a hollow-fiber cartridge perfused with the patient’s whole blood.
Radial Flow Bioreactor
A radial flow bioreactor was evaluated in a phase I clinical trial with seven grade III and IV comatose patients (Morsiani et al, 2002). The etiologies included primary biliary cirrhosis, viral hepatitis, primary nonfunction, and liver trauma. Six of seven patients were bridged to transplantation (86% survival rate). Two of seven died, including the patient with liver trauma and subsequent liver transplantation. The trial applied isolated primary porcine hepatocytes (up to 230 g) contained in a radial flow bioreactor.
Modular Extracorporeal Liver Support System
The modular extracorporeal liver support (MELS) system was evaluated in a phase I trial in 2003 that included eight patients with liver failure as a result of etiologies such as hepatitis B (two patients), drug toxicity (two patients), and unknown causes (three patients) (Sauer et al, 2003). The trial demonstrated safety; all 8 patients were successfully bridged to transplantation, and all were alive at the 3-year follow-up. The MELS device is a complex system of four independently functioning hollow-fiber capillary compartments that contain approximately 500 g of primary porcine hepatocytes. The MELS system is the only device clinically tested that has included human hepatocytes (Sauer et al, 2002).
Amsterdam Medical Center Bioartificial Liver
The Amsterdam Medical Center Bioartificial Liver (AMC-BAL) was evaluated in a phase I safety trial conducted in Italy (van de Kerkhove et al, 2002, 2004). The trial enrolled 12 patients; 11 successfully bridged to orthotopic liver transplantation (OLT). One patient survived after BAL treatments without OLT, and four patients died within 1 month after OLT of disease and transplant-related problems. The configuration of AMC-BAL is a three-dimensional, nonwoven, hydrophilic polyester matrix rolled like a mat with oxygen-carrying fibers in between. The patient’s plasma is in direct contact with the primary isolated porcine hepatocytes, a configuration that differs from devices that separate the patient’s blood and plasma from the cells by a semipermeable hollow-fiber membrane. The AMC-BAL cartridge houses 10 billion hepatocytes.
Hybrid Bioartificial Liver
Ding and colleagues (2003) evaluated their hybrid BAL in a phase I safety trial (Ding et al, 2003). The device was evaluated in 12 patients with ALF. The main etiology was hepatitis B infection after acute decompensation of underlying liver disease. Nine of 12 patients showed clinical and biochemical improvement. The reported mortality rate was 25%, but the length of the follow-up period was not mentioned. The principle of the BAL was detoxification of plasma with an apheresis unit and a hollow-fiber bioreactor loaded with 10 billion primary porcine hepatocytes.
Future Directions
As of today, the BAL devices that have reached clinical testing have been inoculated with hepatocytes from either primary or transformed sources. The trials performed so far have shown safety and proof of concept; however, efficacy data to convincingly demonstrate support of a patient with a failing liver are still missing. Limitations of the first-generation BAL systems have included excess device complexity (Uchino et al, 1988), insufficient hepatocytes to support a failing liver (Margulis et al, 1989), or loss of differentiated function (Matsushita et al, 2003). To address these limitations, a number of research efforts are currently underway. Various novel configurations have been undertaken to improve hepatocyte viability and functional activity in the quest to improve device efficacy. For example, promising reports have shown that combining different cell types of the liver in cocultivation with hepatocytes is a promising option because it more closely mimics the liver environment in vivo (Auth et al, 1998; Bhatia et al, 1999; Nedredal et al, 2007). As another example, Nyberg and colleagues (2005) have developed a novel method of forming hepatic spheroids through gentle oscillation in a rocked bioreactor. Compared with traditional monolayer systems, spheroids show superior function in albumin production, phase I and phase II metabolism, and ureagenesis. In addition, the spheroidal reservoir grown in a bioreactor is capable of supporting 250 to 500 g of primary hepatocytes. This cell mass is increased several times over most first-generation devices. A calculated value of greater than 150 g viable hepatocytes is needed in a BAL to effectively detoxify ammonia, assuming a clinical production rate of 400 µmol/h of ammonia (Nedredal et al, 2009).
Improved detoxification through enhanced mass transfer is another important aspect of future BAL designs. Optimal mass transfer is achieved with the use of semipermeable membranes with an MWCO that provides efficient waste removal and an effective immunologic barrier to protect the nonautologous cells in the BAL. A recent study showed optimal mass transfer with a 400-kD cutoff membrane compared with a 70-kD membrane (Nedredal et al, 2009). Membranes with cutoffs greater than 400 kD, including membranes used for apheresis, may allow immune-mediated damage of xenogeneic hepatocytes in the BAL (Nyberg et al, 2003, 2004).
An abundant source of metabolically active hepatocytes is essential to any successful BAL system. Porcine hepatocytes have been used with limited acceptance because of immunologic concerns and theoretical risks of zoonosis (Cascio et al, 2001; Patience et al, 1997). Meanwhile, immortalized human hepatocytes have yet to be shown to express a full battery of hepatocyte functions that includes ammonia detoxification and normal phase I and phase II activities, along with theoretical risks of malignant spread to an immunocompromised transplant recipient (Mavri-Damelin et al, 2007). These risks of transformed cells have led researchers to explore alternative options for expansion and for hepatocyte-like cells in vitro (Kulig et al, 2004) and hepatocytes in vivo, because efforts to proliferate primary hepatocytes in vitro have been of limited success.
One alternative system for expansion of human hepatocytes in vivo uses u-plasminogen activator–transgenic severe combined immunodeficiency mice (uPA/SCID mice) (Okamura et al, 2006; Sandgren et al, 1991, 1995; Tateno et al, 2004). These transgenic mice express u-plasminogen activator (uPA) under the transcriptional control of a hepatotoxic albumin promoter (Sandgren et al, 1991). Taking advantage of their immunodeficient state, human hepatocytes can be successfully transplanted into these mice without rejection. As the recipient murine hepatocytes die, healthy, unaffected human hepatocytes expand unopposed within the mouse liver, yielding chimeric human/mouse livers (Rhim et al, 1995). This system has led to engraftment levels exceeding 50%. Critics of the SCID-mouse system point to difficulties in animal husbandry, renal disease in the transgenic mice, and difficulties in controlling the mutant phenotype, leading to a narrow window for human hepatocyte transfer (Tateno et al, 2004).
In response to concerns over the SCID-mouse system, an alternative approach has been used to expand human hepatocytes with other transgenic mice. Using immunodeficient Rag2−/−/Il2rg−/− mice, researchers sought to generate an essential hepatocyte deficit and a selective pressure for the stable engraftment of human hepatocytes (Azuma et al, 2007). Fumarylacetoacetate hydrolase (Fah) is an essential enzyme in tyrosine catabolism. Mice deficient for Fah develop tyrosinemia and liver disease in the absence of the protective drug 2-(2-nitro-4-trifluoromethylbenzoyl)-1,3-cyclohexanedione, better known as NTBC (Grompe et al, 1995). Fah−1−/Rag2−/−Il2rg−/− triple-knockout mice were shown to be a successful model of stable engraftment and proliferation of human hepatocytes for the treatment of Fah deficiency (Overturf et al, 1998). Animals in this system are easily bred, devoid of renal disease, and are transplantable at a range of ages.
Interesting and promising approaches to hepatocyte production have been made with stem cells (Campard et al, 2008; Basma et al, 2009). Embryonic stem cells are pluripotent, meaning they have the potential to differentiate into most cell types and therefore could be a source of human hepatocytes. This would also increase the possibility of obtaining unlimited numbers of human hepatocytes and thus further the development of cell-based therapies for liver diseases. The potential uses for stem cells are numerous (Fausto, 2004; Karp, 2009). Drawbacks to stem cell–produced hepatocytes are the limited number of approved human cell lines; the lack of recognition of how to control the development of immature stem cells to mature, phenotypic, liver-specific cell types; and the possibility of teratoma formation.
Novel systems for in vivo (Azuma et al, 2007; Sandgren et al, 1991) and in vitro expansion of human hepatocytes are still early in development (Dalgetty et al, 2009; Yu et al, 2007). Critical to any system used to expand human hepatocytes is the ability to produce a large quantity of stable, healthy cells with normal hepatocyte phenotypes. In this regard, in vivo systems appear to be more advanced than in vitro systems; however, in vivo systems are currently limited by the number of hepatocytes that can be expanded from a mouse—approximately 5 g. Therefore cloning studies are underway to extend in vivo systems of human hepatocyte expansion to larger animal models with the prospect of overcoming scale-up limitations. Large animals with humanized livers may someday be a practical source of hepatocytes for cell-based BAL devices.
Abouna GM, et al. Long-term hepatic support by intermittent multi-species liver perfusions. Lancet. 1970;2:391-396.
Arkadopoulos N, et al. Transplantation of hepatocytes for prevention of intracranial hypertension in pigs with ischemic liver failure. Cell Transplant. 1998;7:357-363.
Auth M, et al. Maintained function of primary human hepatocytes by cellular interactions in coculture: implications for liver support systems. Transpl Int. 1998;11:S439-S443.
Azuma H, et al. Robust expansion of human hepatocytes in Fah−/−/Rag2−/−/Il2rg−/− mice. Nat Biotechnol. 2007;25:903-910.
Basma H, et al. Differentiation and transplantation of human embryonic stem cell–derived hepatocytes. Gastroenterology. 2009;136:990-999.
Bhatia S, et al. Effect of cell-cell interactions in preservation of cellular phenotype: cocultivation of hepatocytes and nonparenchymal cells. FASEB J. 1999;13:1883-1900.
Brady RO, et al. Replacement therapy for inherited enzyme deficiency: use of purified glucocerebrosidase in Gaucher’s disease. N Engl J Med. 1974;291:989-993.
Brunner G, et al. Benefits and dangers of plasma exchange in patients with fulminant hepatic failure. Oda, T, Shiokawa, Y, Inoue, N. Therapeutic Plasmapheresis. 1987:187-191.
Burnell JM, et al. Acute hepatic coma treated by cross-circulation or exchange transfusion. N Engl J Med. 1967;276:935-943.
Burroughs AK, et al. 3-month and 12-month mortality after first liver transplant in adults in Europe: predictive models for outcome. Lancet. 2006;367:225-232.
Campard D, et al. Native umbilical cord matrix stem cells express hepatic markers and differentiate into hepatocyte-like cells. Gastroenterology. 2008;134:833-848.
Canalese J, et al. Controlled trial of dexamethasone and mannitol for the cerebral oedema of fulminant hepatic failure. Gut. 1982;23:625-629.
Cascio S. Novel strategies for immortalization of human hepatocytes. Artif Organs. 2001;25:529-538.
Chari RS, et al. Treatment of hepatic failure with ex vivo pig-liver perfusion followed by liver transplantation. N Engl J Med. 1994;331:234-236.
Clemmesen JO, et al. Hepatic blood flow and splanchnic oxygen consumption in patients with liver failure: effect of high-volume plasmapheresis. Hepatology. 1999;29:347-355.
Dalgetty DM, et al. Progress and future challenges in stem cell-derived liver technologies. Am J Physiol Gastrointest Liver Physiol. 2009;297:G241-G248.
Davenport A, et al. Improved cardiovascular stability during continuous modes of renal replacement therapy in critically ill patients with acute hepatic and renal failure. Crit Care Med. 1993;21:328-338.
Demetriou A, et al. Prospective, randomized, multicenter, controlled trial of a bioartificial liver in treating acute liver failure. Ann Surg. 2004;239:660-670.
Ding YT, et al. The development of a new bioartificial liver and its application in 12 acute liver failure patients. World J Gastroenterol. 2003;9:829-832.
Duan ZP, et al. Interim results of randomized controlled trial of ELAD(TM) in acute on chronic liver disease. Hepatology. 2007;46:274A.
Eiseman B, et al. Heterologous liver perfusion in treatment of hepatic failure. Ann Surg. 1965;162:329-345.
Ellis A, et al. Pilot-controlled trial of the extracorporeal liver assist device in acute liver failure. Hepatology. 1996;24:1446-1451.
Ellis AJ, et al. Temporary extracorporeal liver support for severe acute alcoholic hepatitis using the BioLogic-DT. Int J Artif Organs. 1999;22:27-34.
Fausto N. Liver regeneration and repair: hepatocytes, progenitor cells, and stem cells. Hepatology. 2004;39:1477-1487.
Fox I, et al. Treatment of the Crigler–Najjar syndrome type I with hepatocyte transplantation. N Engl J Med. 1998;338:1422-1426.
Fox IJ, et al. Successful application of extracorporeal liver perfusion: a technology whose time has come. Am J Gastroenterology. 1993;88:1876-1881.
Freeman JG, et al. Plasmapheresis in acute liver failure. Int J Artif Organs. 1986;9:433-438.
Gimson AE, et al. Earlier charcoal haemoperfusion in fulminant hepatic failure. Lancet. 1982;2:681-683.
Grodzicki M, et al. Results of treatment of acute liver failure patients with use of the Prometheus FPSA system. Transplant Proc. 2009;41:3079-3081.
Grompe M, et al. A single mutation of the fumarylacetoacetate hydrolase gene in French Canadians with hereditary tyrosinemia type I. New Engl J Med. 1994;331:353-357.
Grompe M, et al. Pharmacological correction of neonatal lethal hepatic dysfunction in a murine model of hereditary tyrosinemia type I. Nature Genetics. 1995;10:453-460.
Groth CG, et al. Correction of hyperbilirubinemia in the glucuronyltransferase-deficient rat by intraportal hepatocyte transplantation. Transplant Proc. 1977;9:313-316.
Habibullah C, et al. Human fetal hepatocyte transplantation in patients with fulminant hepatic failure. Transplantation. 1994;58:951-952.
Hassanein T, et al. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Hepatology. 2007;46:1853-1862.
Heemann U, et al. Albumin dialysis in cirrhosis with superimposed acute liver injury: a prospective, controlled study. Hepatology. 2002;36:949-958.
Horslen SP, et al. Isolated hepatocyte transplantation in an infant with a severe urea cycle disorder. Pediatrics. 2003;111:1262-1267.
Inoue K, et al. Artificial liver support system using large buffer volumes removes significant glutamine and is an ideal bridge to liver transplantation. Transplant Proc. 2009;41:259-261.
Jalan R, et al. Moderate hypothermia in patients with acute liver failure and uncontrolled intracranial hypertension. Gastroenterology. 2004;127:1338-1346.
Kamath P. Is there life in MARS? Hepatology. 2002;36:1017-1019.
Karp SJ. Clinical implications of advances in the basic science of liver repair and regeneration. Am J Transplant. 2009;9:1973-1980.
Khuroo M, et al. Molecular adsorbent recirculating system for acute and acute-on-chronic liver failure: a meta-analysis. Liver Transpl. 2004;10:1099-1106.
Kiley JE, et al. Removal of blood ammonia by hemodialysis. Proc Soc Exp Biol Med. 1956;91:489-490.
Kiley JE, et al. Ammonia intoxication treated by hemodialysis. N Engl J Med. 1958;259:1156-1161.
Kondrup J, et al. High-volume plasma exchange in fulminant hepatic failure. Int J Artif Organs. 1992;15:669-676.
Krisper P, et al. Technology insight: artificial extracorporeal liver support—how does Prometheus compare with MARS? Nat Clin Pract Nephrol. 2007;3:267-276.
Kulig K, et al. Hepatic tissue engineering. Transpl Immunol. 2004;12:303-310.
Lee W, et al. Acute liver failure: summary of a workshop. Hepatology. 2008;47:1401-1415.
Lepore MJ, et al. Plasmapheresis with plasma exchange in hepatic coma. II. Fulminant viral hepatitis as a systemic disease. Arch Intern Med. 1972;129:900-907.
Macdougall BR, et al. H2-receptor antagonists and antacids in the prevention of acute gastrointestinal haemorrhage in fulminant hepatic failure: two controlled trials. Lancet. 1977;1:617-619.
Margulis M, et al. Temporary organ substitution by hemoperfusion through suspension of active donor hepatocytes in a total complex of intensive therapy in patients with acute hepatic insufficiency. Resuscitation. 1989;18:85-94.
Matas AJ, et al. Hepatocellular transplantation for metabolic deficiencies: decrease of plasms bilirubin in Gunn rats. Science. 1976;192:892-894.
Matsumura K, et al. Hybrid bioartificial liver in hepatic failure: preliminary clinical report. Surgery. 1987;101:99-103.
Matsushita T, et al. Apoptotic cell death and function of cryopreserved porcine hepatocytes in a bioartificial liver. Cell Transplantation. 2003;12:109-121.
Mavri-Damelin D, et al. Ornithine transcarbamylase and arginase I deficiency are responsible for diminished urea cycle function in the human hepatoblastoma cell line HepG2. Int J Biochem Cell Biol. 2007;39:555-564.
Mazariegos G, et al. Safety observations in phase I clinical evaluation of the excorp medical bioartificial liver support system after the first four patients. ASAIO J. 2001;47:471-475.
Meijers BK, et al. Major coagulation disturbances during fractionated plasma separation and adsorption. Am J Transplant. 2007;7:2195-2199.
Merrill JP, et al. The use of an artificial kidney. II. Clinical experience. J Clin Invest. 1950;29:425-438.
Millis JM, et al. Initial experience with the modified extracorporeal liver-assist device for patients with fulminant hepatic failure: system modifications and clinical impact. Transplantation. 2002;74:1735-1746.
Mitzner S, et al. Improvement of hepatorenal syndrome with extracorporeal albumin dialysis MARS: results of a prospective, randomized, controlled clinical trial. Liver Transpl. 2000;6:277-286.
Morsiani E, et al. Early experience with a porcine hepatocyte–based bioartificial liver in acute hepatic failure patients. Int J Art Organs. 2002;25:192-202.
Nedredal GI, et al. Significant contribution of liver nonparenchymal cells to metabolism of ammonia and lactate, and cocultivation augments the functions of a bioartificial liver. Am J Physiol Gastrointest Liver Physiol. 2007;293:G75-83.
Nedredal GI, et al. Optimization of mass transfer for toxin removal and immunoprotection of hepatocytes in a bioartificial liver. Biotechnol Bioeng. 2009;104:995-1003.
Novelli G, et al. Molecular adsorbents recirculating system treatment in acute-on-chronic hepatitis patients on the transplant waiting list improves model for end-stage liver disease scores. Transplant Proc. 2007;39:1864-1867.
Nyberg S, et al. Membrane barrier of a porcine hepatocyte bioartificial liver. Liver Transpl. 2003;9:298-305.
Nyberg S, et al. Cytotoxic immune response to a xenogeneic bioartificial liver. Cell Transplant. 2004;13:783-791.
Nyberg SL, et al. Rapid, large-scale formation of porcine hepatocyte spheroids in a novel spheroid reservoir bioartificial liver. Liver Transpl. 2005;11:901-910.
O’Grady J, et al. Controlled trials of charcoal hemoperfusion and prognostic factors in fulminant hepatic failure. Gastroenterology. 1988;94:1186-1192.
Okamura K, et al. Generation of hybrid hepatocytes by cell fusion from monkey embryoid body cells in the injured mouse liver. Histochem Cell Biol. 2006;125:247-257.
Opolon P. High-permeability membrane hemodialysis and hemofiltration in acute hepatic coma: experimental and clinical results. Artif Organs. 1979;3:354-360.
Ostapowicz G, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947-954.
Overturf K, et al. Ex vivo hepatic gene therapy of a mouse model of hereditary tyrosinemia type I. Hum Gene Ther. 1998;9:295-304.
Pares A, et al. Extracorporeal albumin dialysis: a procedure for prolonged relief of intractable pruritus in patients with primary biliary cirrhosis. Am J Gastroenterol. 2004;99:1105-1110.
Patience C, et al. Infection of human cells by an endogenous retrovirus of pigs. Nature Medicine. 1997;3:282-286.
Pereira SP, et al. Pharmacokinetics and efficacy of oral versus intravenous mixed-micellar phylloquinone (vitamin K1) in severe acute liver disease. J Hepatol. 2005;42:365-370.
Rhim JA, et al. Complete reconstitution of mouse liver with xenogeneic hepatocytes. Proc Natl Acad Sci U S A. 1995;92:4942-4946.
Rifai K, et al. Prometheus: a new extracorporeal system for the treatment of liver failure. J Hepatol. 2003;39:984-990.
Rolando N, et al. Bacterial and fungal infection in acute liver failure. Semin Liver Dis. 1996;16:389-402.
Rolando N, et al. The systemic inflammatory response syndrome in acute liver failure. Hepatology. 2000;32:734-739.
Sabin S, et al. Treatment of hepatic coma in cirrhosis by plasmapheresis and plasma infusion (plasma exchange). Ann Intern Med. 1968;68:1-7.
Saliba F, et al. Randomized controlled multicenter trial evaluating the efficacy of albumin dialysis with MARS(r) in patients with fulminant and subfulminant liver failure. Hepatology. 2008;48:94A.
Sandgren E, et al. Complete hepatic regeneration after somatic deletion of an albumin-plasminogen activator transgene. Cell. 1991;66:245-256.
Sandgren EP, et al. Hepatocarcinogenesis in transgenic mice. Prog Clin Biol Res. 1995;391:213-222.
Sauer IM, et al. Primary human liver cells as source for modular extracorporeal liver support: a preliminary report. Int J Artif Organs. 2002;25:1001-1005.
Sauer IM, et al. Clinical extracorporeal hybrid liver support: phase 1 study with primary porcine liver cells. Xenotransplantation. 2003;10:460-469.
Schmidt L, et al. Systemic hemodynamic effects of treatment with the molecular adsorbents recirculating system in patients with hyperacute liver failure: a prospective controlled trial. Liver Transpl. 2003;9:290-297.
Shami VM, et al. Recombinant activated Factor VII for coagulopathy in fulminant hepatic failure compared with conventional therapy. Liver Transpl. 2003;9:138-143.
Smilkstein M, et al. Efficacy of oral N-acetylcysteine in the treatment of acetaminophen overdose. N Engl J Med. 1988;319:1557-1562.
Sorrentino F. Prime richerche per la realizzatione di un fegato artificiale. Chirurgia Patologica Sperimentale. 1956;4:1401-1414.
Stange J, et al. Dialysis against a recycled albumin solution enables the removal of albumin-bound toxins. Artif Organs. 1993;17:809-813.
Stange J, et al. Molecular adsorbent recycling system (MARS): clinical results of a new membrane-based blood purification system for bioartificial liver support. Artif Organs. 1999;23:319-330.
Steiner C, et al. Binding of bilirubin and bromosulphthalein to albumin: implications for understanding the pathophysiology of liver failure and its management. Liver Transpl. 2004;10:1531-1538.
Strauss G, et al. Hyperventilation restores cerebral blood flow autoregulation in patients with acute liver failure. J Hepatol. 1998;28:199-203.
Strom S, et al. Hepatocyte transplantation as a bridge to orthotopic liver transplantation in terminal liver failure. Transplantation. 1997;63:559-569.
Strom S, et al. Hepatocyte transplantation: clinical experience and potential for future use. Cell Transplant. 2006;15:S105-110.
Sutherland DE, et al. Hepatocellular transplantation in acute liver failure. Surgery. 1977;82:124-132.
Takahashi T, et al. Artificial liver: state of the art. Dig Dis Sci. 1991;36:1327-1340.
Tateno C, et al. Near completely humanized liver in mice shows human-type metabolic responses to drugs. Am J Pathol. 2004;165:901-912.
Uchino J, et al. A hybrid bioartificial liver composed of multiplated hepatocyte monolayers. ASAIO Trans. 1988;34:972-977.
van de Kerkhove MP, et al. Phase I clinical trial with the AMC-bioartificial liver. Int J Artif Organs. 2002;25:950-959.
van de Kerkhove MP, et al. Clinical application of bioartificial liver systems. Ann Surg. 2004;240:216-230.
Vaquero J, et al. Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopathy. Liver Transpl. 2005;11:1581-1589.
Wijdicks E, et al. Propofol to control intracranial pressure in fulminant hepatic failure. Transplant Proc. 2002;73:1965-1968.
Wijdicks EF, et al. Validation of a new coma scale: the FOUR score. Ann Neurol. 2005;58:585-593.
Wolf C, Munkelt BE. Bilirubin conjugation by an artificial liver composed of cultured cells and synthetic capillaries. Trans Am Soc Artif Intern Organs. 1975;21:16-27.
Xue YL, et al. TECA hybrid artificial liver support system in treatment of acute liver failure. World J Gastroenterol. 2001;7:826-829.
Yu J, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917-1920.