Stoma care

Specific investigations
Second-line therapies
Third-line therapies
Synchronous panniculectomy with stomal revision for obese patients with stomal stenosis and retraction.
Katkoori D, Samavedi S, Kava B, Soloway MS, Manoharan M. BJU Int 2009; 105: 1586–9.
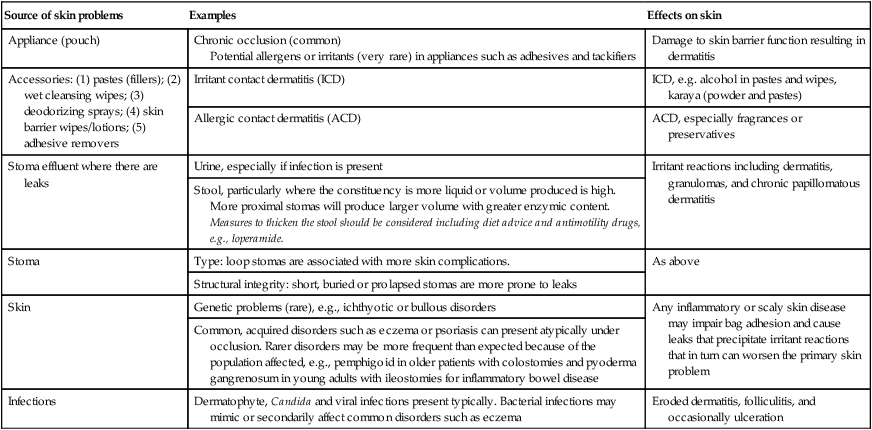
Table 225.1
Peristomal skin disorders according to primary source
| Source of skin problems | Examples | Effects on skin |
| Appliance (pouch) | Chronic occlusion (common) Potential allergens or irritants (very rare) in appliances such as adhesives and tackifiers |
Damage to skin barrier function resulting in dermatitis |
| Accessories: (1) pastes (fillers); (2) wet cleansing wipes; (3) deodorizing sprays; (4) skin barrier wipes/lotions; (5) adhesive removers | Irritant contact dermatitis (ICD) | ICD, e.g. alcohol in pastes and wipes, karaya (powder and pastes) |
| Allergic contact dermatitis (ACD) | ACD, especially fragrances or preservatives | |
| Stoma effluent where there are leaks | Urine, especially if infection is present | Irritant reactions including dermatitis, granulomas, and chronic papillomatous dermatitis |
| Stool, particularly where the constituency is more liquid or volume produced is high. More proximal stomas will produce larger volume with greater enzymic content. Measures to thicken the stool should be considered including diet advice and antimotility drugs, e.g., loperamide. | ||
| Stoma | Type: loop stomas are associated with more skin complications. | As above |
| Structural integrity: short, buried or prolapsed stomas are more prone to leaks | ||
| Skin | Genetic problems (rare), e.g., ichthyotic or bullous disorders | Any inflammatory or scaly skin disease may impair bag adhesion and cause leaks that precipitate irritant reactions that in turn can worsen the primary skin problem |
| Common, acquired disorders such as eczema or psoriasis can present atypically under occlusion. Rarer disorders may be more frequent than expected because of the population affected, e.g., pemphigoid in older patients with colostomies and pyoderma gangrenosum in young adults with ileostomies for inflammatory bowel disease | ||
| Infections | Dermatophyte, Candida and viral infections present typically. Bacterial infections may mimic or secondarily affect common disorders such as eczema | Eroded dermatitis, folliculitis, and occasionally ulceration |




 Change appliance
Change appliance Absorbent powders
Absorbent powders Antibiotics
Antibiotics Topical corticosteroids
Topical corticosteroids Sucralfate
Sucralfate Tacrolimus ointment or pimecrolimus cream
Tacrolimus ointment or pimecrolimus cream Intralesional corticosteroids
Intralesional corticosteroids Topical cromolyn sodium
Topical cromolyn sodium Oral dapsone
Oral dapsone Cyclosporine
Cyclosporine Tumor necrosis factor-blocking drugs
Tumor necrosis factor-blocking drugs Collagen injections
Collagen injections Lipectomy
Lipectomy Stoma revision surgery
Stoma revision surgery