Splinting Techniques
Splints are used frequently in the emergency department (ED) for temporary immobilization of fractures and dislocations and for definitive treatment of soft tissue injuries.1,2 Patients with a variety of nontraumatic musculoskeletal disorders (e.g., gout, inflammatory joint diseases, infections, burns) also benefit from short-term immobilization. Immobilization is the mainstay of fracture therapy, but though intuitively beneficial, it is difficult to find firm scientific data that support the use of splinting for soft tissue injuries.3,4 Although the general principle of immobilizing sprains and contusions is strongly supported by custom and personal preference, its exact influence on healing, number of complications, and ultimate return to normal activity is not known. In most studies of ankle sprains, for example, the function and pain of the injured joint are similar at 6 weeks’ follow-up, regardless of whether treatment consisted of ad lib walking, a simple elastic bandage, a posterior splint, or a formal cast.5,6 A systematic review of 22 clinical trials comparing various treatments of acute lateral ankle sprains (cast, splint, or early mobilization with support) found no favorable effect of immobilization.7 The current data support functional management for most acute ankle sprains.7
Patients are routinely seen in the ED with injuries that are amenable to splinting to relieve pain and augment healing (see Review Box 50-1). Although a strict standard of care cannot be promulgated, the use of short-term splinting in the ED for acutely painful conditions remains a common practice. Emergency clinicians have virtually abandoned the use of circumferential casts in favor of premade commercial immobilizing devices or splints constructed of plaster of paris or fiberglass. The impetus for this change is primarily related to the complications occasionally associated with circumferential casts, liability issues, and ease of application brought about by new technology. In most instances, properly applied splints provide short-term immobilization equal to that of casts while allowing continued swelling and thus reducing the risk for ischemic injury. Other obvious advantages of splints are that patients can take them off when immobilization is no longer needed or can remove them temporarily to bathe, exercise the injured part, or perform wound care.
Most splinting techniques are handed down from house staff or experienced clinicians, but the procedure is often suboptimal and haphazard.8 This chapter presents guidelines for adequate immobilization of injuries commonly encountered by emergency clinicians. Details of the construction and application of commonly used custom-made plaster splints are provided.
Indications and Contraindications
Theoretically, immobilization facilitates the healing process by decreasing pain and protecting the extremity from further injury. Other benefits of splinting are specific to the particular injury or problem being treated (Fig. 50-1). For example, in the treatment of fractures, splinting helps maintain bony alignment. Splinting deep lacerations that cross joints reduces tension on the wound and helps prevent wound dehiscence. Immobilizing tendon lacerations may facilitate the healing process by relieving stress on the repaired tendon. The discomfort of inflammatory disorders such as tenosynovitis or acute gout is greatly reduced by immobilization. Deep space infections of the hands or feet, as well as cellulitis over any joint, should similarly be immobilized for comfort. Limiting early motion may also reduce edema and theoretically improve the immune system’s ability to combat infection. Hence, selected puncture wounds and mammalian or human bites of the hands and feet may be immobilized until the risk for infection has passed. Splinting large abrasions that cross joint surfaces prevents movement of the injured extremity and reduces the pain produced when the injured skin is stretched. Finally, victims of multiple trauma should have fractures and reduced dislocations adequately splinted while other diagnostic and therapeutic procedures (e.g., fluid resuscitation, airway control, computed tomography scans, tube thoracostomy) are completed. Immobilization decreases blood loss, minimizes the potential for further neurovascular injury, reduces the need for opioid analgesia, and may decrease the risk for fat emboli from long-bone fractures.
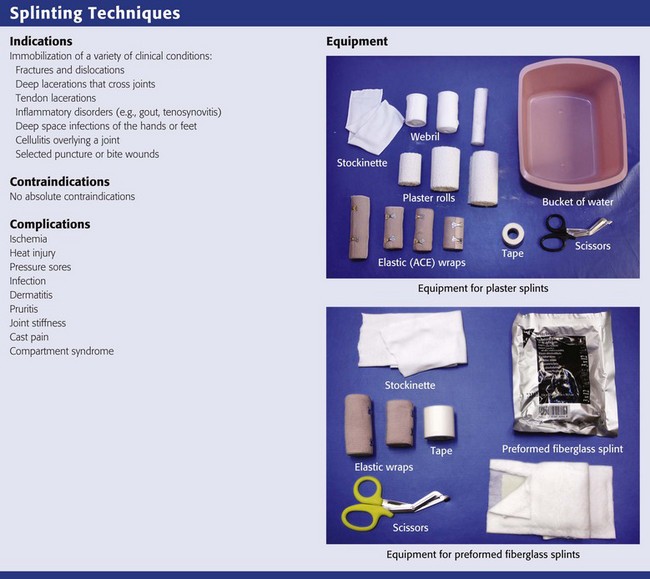
Equipment (see Review Box 50-1)
Plaster of Paris
Plaster of paris is the most widely used material for ED splinting.9 Its name originated from the fact that it was first prepared from the gypsum of Paris, France. When gypsum is heated to approximately 128°C, most of the water of crystallization is driven off and a fine white powder is left behind—plaster of paris. When water is added to the plaster, the reaction is reversed, and the plaster recrystallizes or “sets” by incorporating water molecules into the crystalline lattice of the calcium sulfate dehydrate molecules.
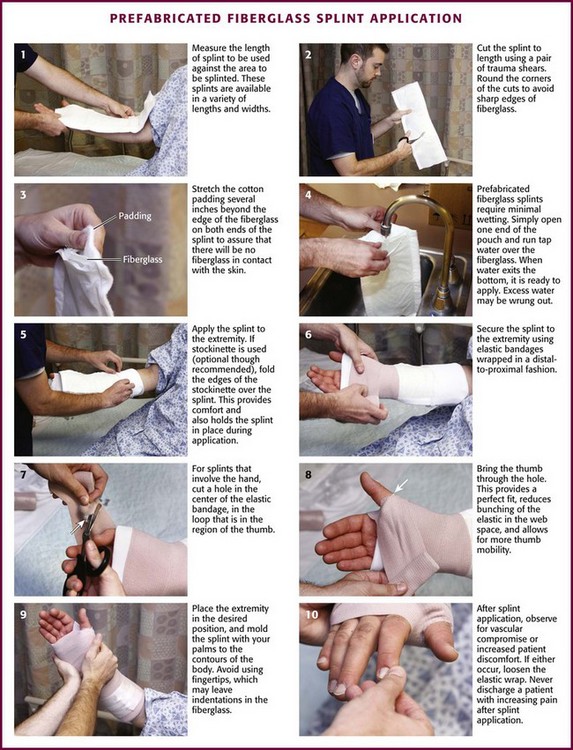
Prefabricated Splint Rolls
Prefabricated splint rolls composed of layers of fiberglass between polypropylene padding (e.g., Ortho-Glass, 3M Scotchcast One-Step) are now commonplace in many EDs. Fiberglass splint rolls offer the same time-saving aspect as prefabricated plaster splint rolls but require only 3 minutes to set, thus making application faster. In addition, splints made of prefabricated fiberglass rolls cure more rapidly (20 minutes), have no messy residue (i.e., they can be hydrated in a conventional sink without a special trap), can be washed and reapplied, and are stronger and lighter than splints constructed of prefabricated plaster rolls. Another advantage is the polypropylene padding, which wicks moisture away from the skin better than polyester, nylon, or cotton padding does.10 Prefabricated fiberglass splint rolls are more expensive than both simple plaster rolls and prefabricated plaster splint rolls and, like prefabricated plaster splints, lack some of the versatility and custom-fit qualities of self-made plaster splints.
Protective and Miscellaneous Equipment
Elastic Bandages
Patients often use or request an elastic bandage for many soft tissue injuries. Although applying an elastic bandage to an injured part is popular, it is of minimal benefit alone. The downside is that the bandage may be wrapped too tightly and cause additional injury or distal swelling (Fig. 50-2).
General Procedure of Custom Splint Application
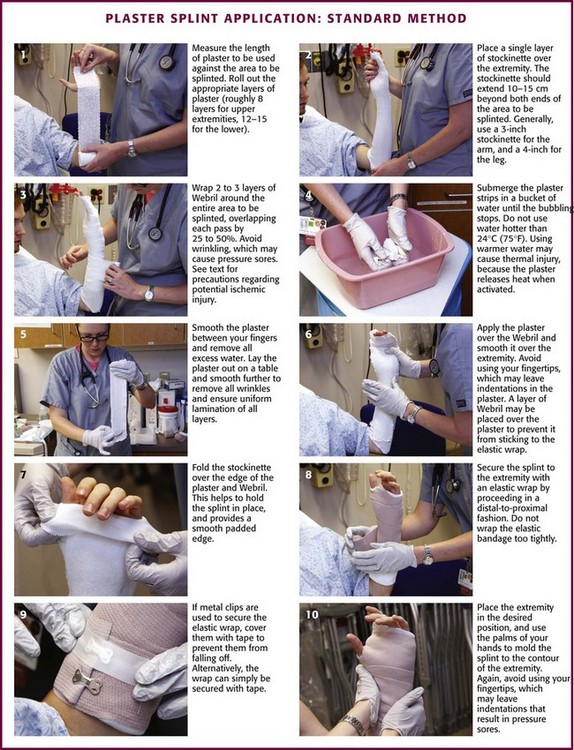
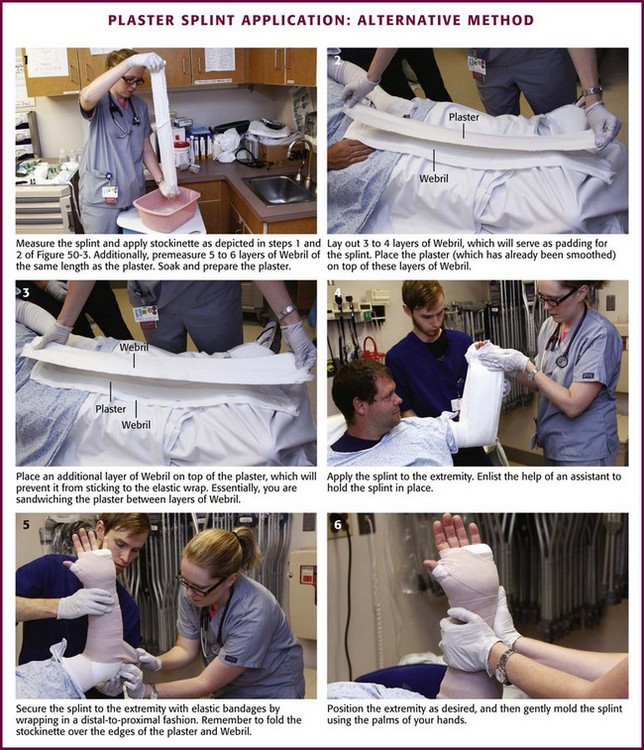
This following text refers to the application of custom-made plaster splints unless otherwise stated (Figs. 50-3 and 50-4). If periodic wound care is required, apply a more easily removable splint (e.g., OCL, Ortho-Glass, Velcro-type splint described below) in lieu of the standard splint (Fig. 50-5). Address the issue of removability before the splint is applied. In addition, use of Webril (Curity) cast padding is described, but other suitable cast padding may be substituted. Caveats for proper ED splinting are listed in Box 50-1.
Padding
Following placement of padding between the fingers and toes in self-made splints, use a stockinette over the skin as the first protective layer (see Fig. 50-3, step 2). Extend the stockinette at least 10 to 15 cm beyond the area to be splinted at both ends of the extremity. Later, after the plaster has been applied, fold the stockinette back over the ends of the splint to create smooth, padded rims and to help hold the splint in place when applying elastic bandages (see Fig. 50-3, step 7). To avoid pressure damage, do not pull the stockinette too tightly over bony prominences such as the heel. In addition, prevent wrinkling over flexion creases by slitting and overlapping the stockinette at bony prominences. One may also use two separate pieces of stockinette (one at each end of the splint) to produce the smooth padded rims. As a general rule, use 3-inch-wide stockinette for the upper extremity and 4-inch-wide stockinette for the lower extremity.
After the stockinette has been properly positioned, wrap Webril around the entire area that will be exposed to plaster. Apply at least two or three layers of Webril, with each turn overlapping the previous turn by 25% to 50% of its width (see Fig. 50-3, step 3). Make sure that the Webril extends 2.5 to 5.0 cm beyond the ends of the splint so that it, too, can be folded back over the splint to help create smooth, well-padded edges. Place extra padding over areas of bony prominence, such as the radial condyle or the malleoli (Box 50-2). Although this can be done with Webril, Mother’s Cotton adds an additional measure of protection without the worry of wrinkling or ischemic injury. If significant swelling is anticipated, use three or four layers of Webril. Be careful to avoid wrinkling because this can result in significant skin pressure when a tight splint is worn for a long period. Prevent wrinkles by proportionately stretching or even tearing the side of the Webril that must wrap around the larger portion of an extremity. Joints that must be immobilized in a 90-degree position, such as the ankle, make continuous Webril wrapping difficult. To avoid wrinkles around the ankle, place the joint in the proper position before padding. Wrap the Webril around the malleolar and midtarsal regions first, and then cover the bare calcaneal region with overlapping vertical and horizontal Webril strips until the entire heel region is evenly padded. Use the same approach in similar areas such as the elbow. Choose a width of Webril appropriate for the extremity to be splinted. In general, use the 2-inch width for the hands and feet, the 3- or 4-inch width for the upper extremity, and the 4- or 6-inch width for the lower extremity.
A final caveat when using Webril is to be aware of the potential for ischemic injury. This rare complication is most likely to occur in an extremity that continues to have significant swelling after the patient is released from the ED. Ischemia may result because the concentrically placed Webril can become a constricting band. If this situation is anticipated, it can easily be prevented. Cut through the Webril along the side of the extremity that is opposite the plaster splint. Then, secure the splint to the extremity in the usual manner. Alternatively, place two or three layers of Webril (the same diameter as the plaster) directly over the wet plaster (see Fig. 50-4). Position the Webril-lined splint over the area to be immobilized and secure it in place with an elastic bandage.
Plaster Preparation
The choice of plaster setting time depends on the nature of the injury and the expertise of the clinician. Use extra-fast–setting plaster when rapid hardening is desired to help maintain alignment of an acutely reduced fracture. However, for the majority of ED splints, plaster with slower setting times (e.g., Specialist Plaster Bandage Fast Setting) is recommended.11 Plaster that sets more slowly is easier for some clinicians to use because it affords more leeway in applying and molding the splint. Furthermore, plaster with a longer setting time produces less heat, thus reducing both patient discomfort and the risk for serious burns.12 Table 50-1 lists the setting times for commonly used plaster. These setting times can be adjusted by adding different substances to the plaster during the production process (Box 50-3). Given plaster with equal setting times, the most important variable affecting the rate of crystallization is water temperature. Warm water hardens a splint faster than cold water does and should not be used when extra time is needed for splint application.
TABLE 50-1
Setting Times of Fast- and Extra-Fast–Drying Plaster
| PLASTER | SETTING TIME (min) |
| Fast drying | 5-8 |
| Extra-fast drying | 2-4 |
The thickness of a splint depends on the size of the patient, the extremity that is injured, and the desired strength of the final product. An ankle splint may crack quickly and become useless if only eight layers are used, but this thickness may be ideal for a wrist splint. In general, it is best to use the minimum number of layers necessary to achieve adequate strength. Thicker splints are heavier and more uncomfortable. It is also important to note that plaster thickness is a major determinant of the amount of heat given off during the setting process. More than 12 sheets of plaster create an increased risk for significant burns, especially when using extra-fast–drying plaster, when using dipping water with a temperature higher than 24°C, or when a pillow is placed under or around the extremity for support during the setting process (Box 50-4). For an average-sized adult, splint the upper extremities with 8 sheets of plaster and the lower extremities with 12 to 15 sheets. Such layering usually provides the strength necessary for adequate immobilization while reducing the patient’s discomfort and the risk for significant burns. In a 136-kg (300-lb) patient, however, up to 20 layers may be required to make a durable ankle splint.
Keep the dipping water clean and fresh. Reusing water that has been used previously for wetting plaster increases the amount of heat given off during crystallization and causes the plaster to set more quickly. As a rule of thumb, keep the temperature of the water around 24°C. This temperature allows a workable setting time and has not been associated with increased risk for significant burns. As the temperature of the dipping water approaches 40°C, the potential for serious burns increases, even with splint thicknesses consisting of fewer than 12 plies. It is interesting to note that water temperature has been shown to be only a minor consideration in heat production in some studies (see Box 50-4).
Splint Application (see Fig. 50-3)
Molding the wet splint to conform to the body’s anatomy is probably the most important, yet the most frequently overlooked step to ensure adequate immobilization. The act of molding may cause some pain, so be sure to forewarn the patient. Mold with the palm or flat side of the fingers to avoid putting ridges or indentations in the underlying plaster. Complete all manipulation of the wet plaster before it reaches a thick, creamy consistency. Any movement after this time, which is known as the critical period, results in an imperfect crystalline network of calcium sulfate molecules and greatly weakens the ultimate strength of the splint. While the plaster is setting, do not wrap a pillow or blanket around the extremity for support. This leads to inadequate ventilation around the splint and greatly increases the amount of heat produced (see Box 50-4).
Upper Extremity Splints
Long Arm Posterior Splint
Indications.: Use a long arm posterior splint (Figs. 50-6 and 50-7) to immobilize injuries to the elbow and proximal end of the forearm. It completely eliminates flexion and extension of the elbow but does not entirely prevent pronation and supination of the forearm. Therefore, it is not recommended for immobilization of complex or unstable distal forearm fractures unless used in conjunction with a long arm anterior splint (see later in this section). Alternatively, a double “sugar-tong” splint can be applied (see later in this section).
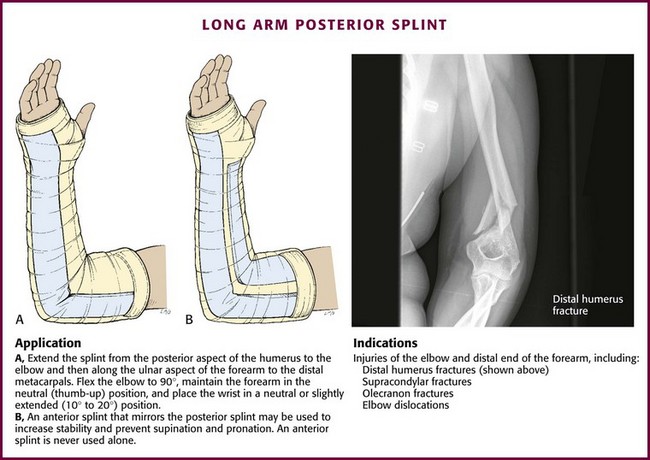
Figure 50-6 Long arm posterior splint.
Construction.: Construct a long arm posterior splint with 8 to 10 layers of 4- or 6-inch-wide plaster. Start the splint on the posterior aspect of the proximal end of the arm. Extend it down the arm to the elbow and then along the ulnar aspect of the forearm and hand to the level of the metacarpophalangeal (MCP) joints.
Application.: Apply a stockinette and Webril as described previously. Cut a hole in the stockinette to expose the thumb, and place extra padding over the olecranon to prevent pressure injury. Position the arm with the elbow flexed to 90 degrees, the forearm neutral (thumb upward), and the wrist neutral or slightly extended (10 to 20 degrees). Ask an assistant to hold the wet splint in place, particularly when applying both a posterior and an anterior splint. Once the splint has been properly positioned, fold the ends of the stockinette and Webril back and secure the splint in place with 2-, 3-, or 4-inch elastic bandages. Finally, fold the sides of the splint up to create a gutter configuration and carefully mold the plaster around the extremity with the palms of the hand. The fingers and thumb should remain free to prevent stiffness from unnecessary immobilization.
Long Arm Anterior Splint
Indications.: A long arm anterior splint is never used alone but, rather, as an adjunct to a long arm posterior splint to improve immobilization by increasing stability and preventing pronation and supination of the forearm (see Fig. 50-6B).
Construction.: Construct a long arm anterior splint in the same manner as described for a long arm posterior splint. It mirrors the posterior splint by running down the anterior aspect of the arm to the antecubital fossa, where it continues along the radial aspect of the forearm to the distal end of the radius.
Application.: Use stockinette, Webril, and positioning similar to the way it was described for application of a long arm posterior splint. When using both an anterior and a posterior long arm splint, have an assistant available to hold the wet splint in place. Place the anterior splint first and then position the posterior splint. Once both splints have been properly positioned, fold the ends of the stockinette and Webril back and secure the splint in place with 2-, 3-, or 4-inch elastic bandages. Finally, fold up the sides of the splint to create a gutter configuration and carefully mold the plaster around the extremity with the palms of the hands. Keep the patient’s fingers and thumb free to prevent stiffness from unnecessary immobilization.
Double Sugar-Tong Splint
Indications.: Use a double sugar-tong splint (Fig. 50-8) like a long arm posterior splint to immobilize injuries to the elbow and forearm. However, because it prevents pronation and supination of the forearm, it is preferable for some distal forearm and elbow fractures.
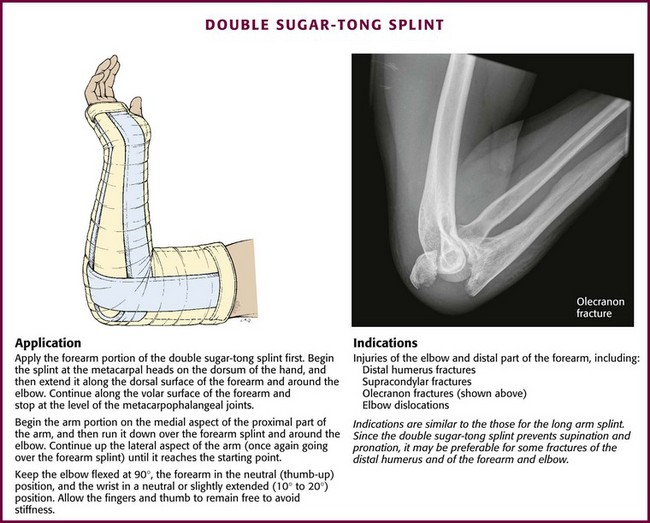
Figure 50-8 Double sugar-tong splint.
Construction.: The splint consists of two separate pieces of plaster, a forearm splint and an arm splint. Construct each piece with eight layers of 3- or 4-inch plaster. The forearm portion of the splint runs from the metacarpal heads on the dorsum of the hand along the dorsal surface of the forearm around the elbow. It continues along the volar surface of the forearm to the palm of the hand and stops at the level of the MCP joints. The arm portion of the splint begins on the anterior aspect of the proximal end of the humerus. It runs down the arm over the forearm splint and around the elbow. It then continues up the posterior aspect of the arm, once again going over the forearm splint, until it reaches the starting point.
Application.: Use a stockinette, Webril, and positioning similar to the way it was described for the application of a long arm posterior splint. Secure the two splints in place with 2-, 3-, or 4-inch elastic bandages starting with the forearm splint at the hand. Once the forearm splint is secured in place, wrap the arm portion of the splint beginning at its proximal end. Keep the patient’s fingers and thumb free to prevent stiffness.
Forearm and Hand Splints
Indications.: Use a volar splint (Fig. 50-9) to immobilize a variety of soft tissue injuries to the hand and wrist. It is also used for temporary immobilization of triquetral fractures, lunate and perilunate dislocations, and second through fifth metacarpal head fractures. For these more serious injuries, some clinicians prefer to add a dorsal splint to create a more stable bivalve effect (see Fig. 50-9B). Because a volar splint does not completely eliminate pronation and supination of the forearm, it may not be ideal for distal radial and ulnar fractures, although many clinicians use this splint for nondisplaced or minimally displaced distal ulnar and radial fractures.
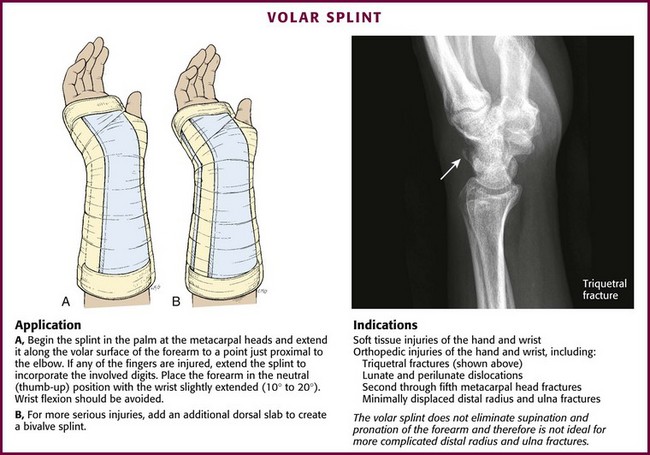
Figure 50-9 Volar splint.
Construction.: Construct the splint with 8 to 10 layers of 3- or 4-inch-wide plaster. The splint begins in the palm at the metacarpal heads and extends along the volar surface of the forearm to just proximal to the elbow. If there is an injury to any of the fingers, extend the splint to incorporate the involved digit or digits.
Application.: Apply a stockinette and Webril as described previously. Cut a hole in the stockinette to expose the thumb. If the splint is going to incorporate one or more digits, insert a piece of Webril or gauze between the digits to prevent skin maceration. Place the forearm in the neutral position (thumb upward) with the wrist extended slightly (10 to 20 degrees). Avoid wrist flexion. After properly positioning the wet plaster, fold back the ends of the stockinette and Webril and use a 3- or 4-inch elastic bandage to secure the splint in place. Fold the sides of the splint up around the forearm to create a gutter effect, and carefully mold the plaster to conform to the contours of the palm and wrist. Some clinicians prefer to extend the splint to the fingertips and then fold the wet plaster back toward the palm, which allows the fingers to “grasp” the rounded distal end when at rest. With either method, keep the thumb and fingers free to move unless they are injured and are being intentionally immobilized by the splint.
Sugar-Tong Splint
Indications.: Use a sugar-tong splint (Fig. 50-10) for fractures of the distal end of the radius and ulna. The advantage of this splint over a volar splint is prevention of pronation and supination of the forearm. In addition, it immobilizes the elbow, which is desirable for the first few days after a distal forearm fracture.
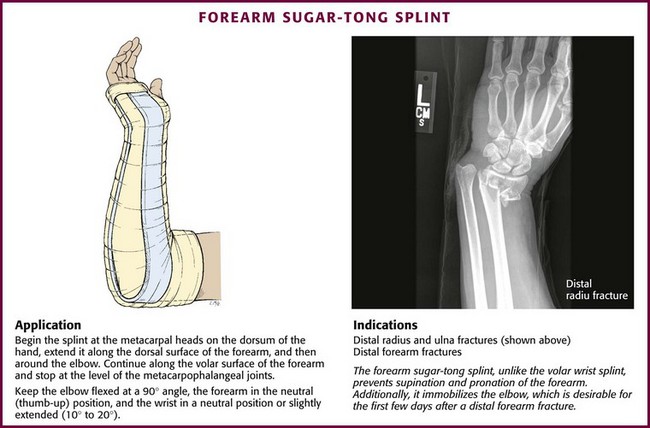
Figure 50-10 Forearm sugar-tong splint.
Thumb Spica Splint
Indications.: Use a thumb spica splint (Fig. 50-11) to immobilize injuries and fractures of the scaphoid, lunate, thumb, and first metacarpal. It is also used for the treatment of de Quervain’s tenosynovitis. Traditionally, a thumb spica splint or cast was thought to be a requirement for properly immobilizing scaphoid fractures; however, there is no totally agreed standard. Clay and coworkers13 stated that the optimal method of casting scaphoid fractures has not been definitively established. They were unable to prove a difference in patient comfort, recovery of function, or incidence of nonunion between a Colles cast and a traditional scaphoid cast that included the thumb.
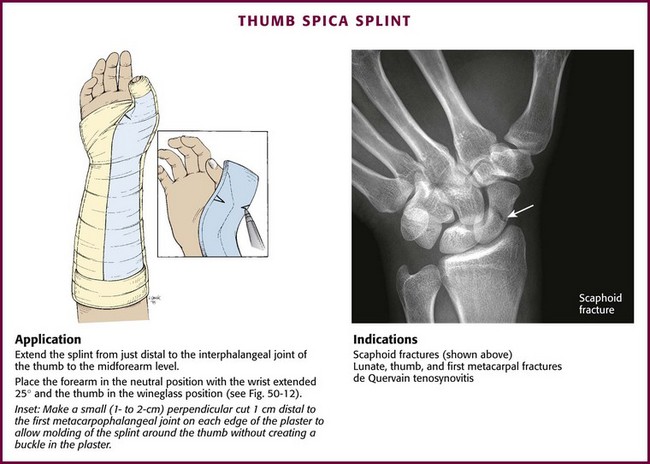
Figure 50-11 Thumb spica splint.
Construction.: Construct the splint with eight layers of 3-inch-wide plaster. Extend the splint from just distal to the interphalangeal joint of the thumb to the midforearm level.
Application.: Place the forearm in the neutral position with the wrist extended 25 degrees and the thumb in the wineglass position (Fig. 50-12). Apply a stockinette and Webril from the base of the palm to the midforearm level. It is difficult to place a stockinette around the thumb. Instead, cut a hole in the stockinette to expose the thumb, and then pad the exposed thumb with small vertical strips of Webril or wrap it with 2-inch Webril. Place the dry plaster over the radial aspect of the forearm from just beyond the thumb interphalangeal joint to the midforearm level. Once in position, mark the location of the first MCP joint and make a small (1- to 2-cm) perpendicular cut 1 cm distal to the mark on each edge of the plaster (see Fig. 50-11 inset). This allows the splint to be molded around the thumb without creating a buckle in the plaster. If the plaster distal to the cut notches is too wide to mold around the thumb without overlapping, trim the edges to the desired width. Wet the plaster and secure it in place with a 2- or 3-inch elastic bandage. It is important to carefully mold the wet plaster around the thumb and palm and to maintain the thumb in the wineglass position while the plaster is drying.
Ulnar Collateral Ligament Injury (Gamekeeper’s or Skier’s Thumb): Forced abduction with hyperextension of the thumb is the usual mechanism for injury to the ulnar collateral ligament. This is a rather disabling injury that requires early recognition since improper treatment can result in chronic pain, pinch weakness, and loss of stability of the thumb. Characterized by MCP joint pain, tenderness of the ulnar side, and laxity of this joint with valgus stressing, this is not a simple sprain. Although immobilization with a thumb spica splint or figure-of-eight thumb splint may suffice as definitive treatment (Fig. 50-13), surgery is often recommended for more advanced injuries. Splinting in the ED with referral to a consultant is prudent for all significant thumb soft tissue injuries consistent with an ulnar collateral ligament injury.
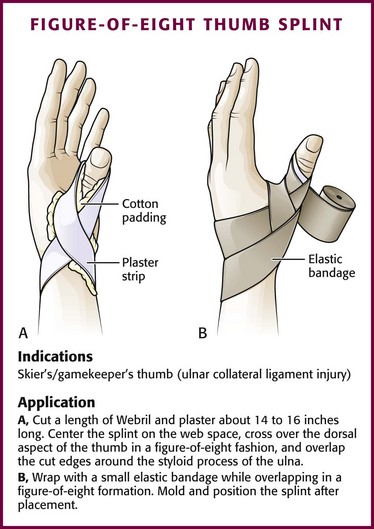
Figure 50-13 Figure-of-eight thumb splint.
Ulnar Gutter Splint
Indications.: Use an ulnar gutter splint (Fig. 50-14) to immobilize fractures and serious soft tissue injuries of the little and ring fingers and fractures of the neck, shaft, and base of the fourth and fifth metacarpals.
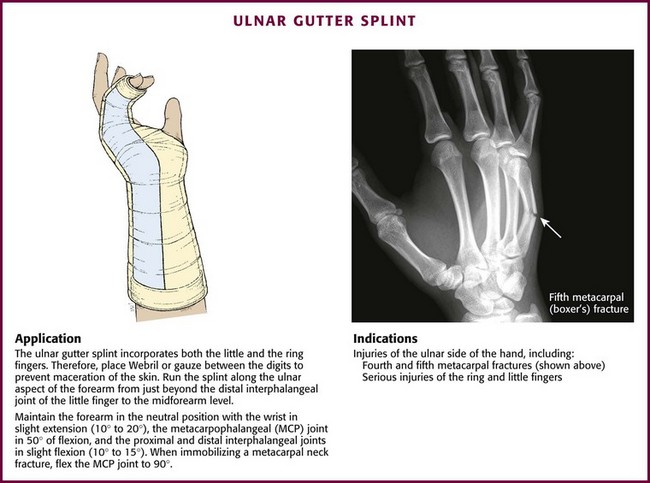
Figure 50-14 Ulnar gutter splint.
Construction.: Make the splint with six to eight layers of 3- or 4-inch plaster. It incorporates both the little and the ring fingers. It runs along the ulnar aspect of the forearm from just beyond the distal interphalangeal joint of the little finger to the midforearm level.
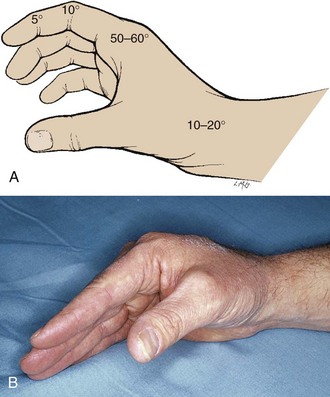
Application.: Apply a stockinette and Webril as usual. Place additional Webril or gauze between the little and ring fingers to prevent maceration of the skin. Position the forearm in the neutral position with the wrist in slight extension (10 to 20 degrees), the MCP joints in 50 degrees of flexion, and the proximal and distal interphalangeal joints in slight flexion (10 to 15 degrees). When immobilizing a metacarpal neck fracture (i.e., boxer’s fracture), flex the MCP joint to 90 degrees. Once in proper position, fold the sides of the splint up to form a gutter. Finally, fold the ends of the stockinette and Webril back to help hold the splint in place while it is secured to the extremity with a 2- or 3-inch elastic bandage.
Radial Gutter Splint
Indications.: Use a radial gutter splint (Fig. 50-15) to immobilize fractures and serious soft tissue injuries of the index and long fingers and fractures of the neck, shaft, and base of the second and third metacarpals.
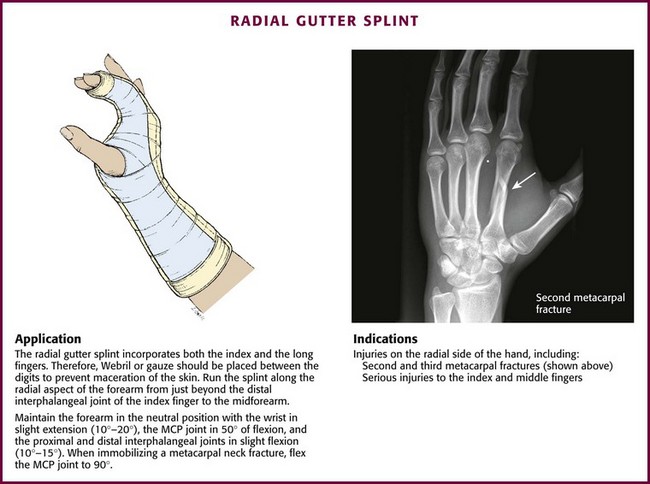
Figure 50-15 Radial gutter splint.
Construction.: Make the splint with six to eight layers of 3- or 4-inch plaster. It runs along the radial aspect of the forearm from just beyond the distal interphalangeal joint of the index finger to the midforearm level.
Application.: Apply a stockinette (with a hole cut to expose the thumb) and Webril as described previously. Insert an additional piece of Webril or gauze between the index and long fingers to prevent maceration of the skin. Place the hand and fingers in the position of function or in the intrinsic position (see Fig. 50-12). Neither position has been proved to be superior for the first few weeks of splinting, which makes them both acceptable for initial immobilization in the ED. In the position of function, the forearm is in the neutral position with the wrist in slight extension (10 to 20 degrees), the MCP joints in 50 to 60 degrees of flexion, and the proximal and distal interphalangeal joints in slight flexion (5 to 10 degrees) (see Fig. 50-12A). When immobilizing a metacarpal neck fracture, the intrinsic position is often used, with the MCP joint flexed to 90 degrees and the fingers extended (see Fig. 50-12B).
Finger Splints
Use finger splints for sprains, fractures, tendon repairs, or infections. Minor finger sprains can often be managed with dynamic splinting (e.g., buddy taping) (Fig. 50-16A) or a commercially available foam splint with aluminum backing (one-surface splint) (see Fig. 50-16B), but fractures, tendon repairs, and some soft tissue injuries benefit from formal splinting (e.g., thumb spica and ulnar and radial gutter splints). Specific conditions, such as mallet finger, require a specialized splint (plaster or Stack splint) (see Fig. 50-16C). When complete immobilization of a finger is required (e.g., unstable phalangeal fractures), an “outrigger” finger splint that incorporates the wrist may be used (see Fig. 50-16D). Both the position of function and the intrinsic position are acceptable for initial splinting.
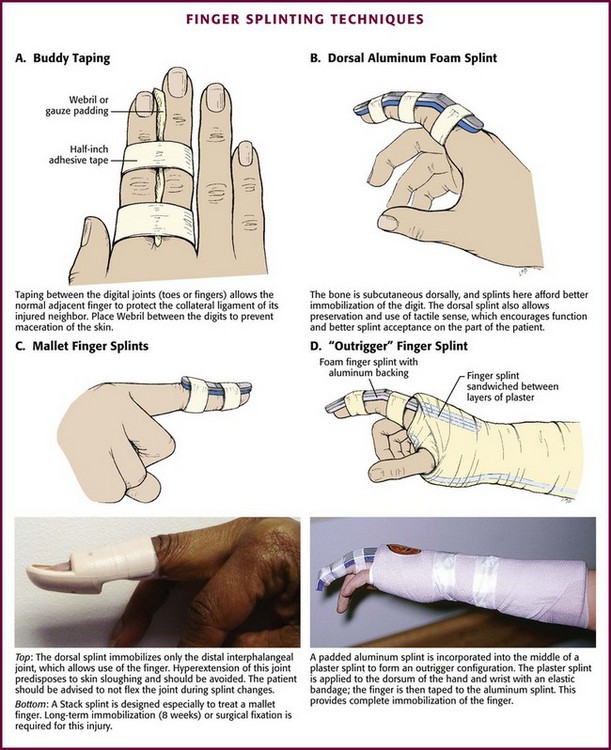
Figure 50-16 Finger splinting techniques
Pitfalls of Hand Dressings and Splints
The two most common problems with hand dressings and splints are putting them on too tightly and leaving them on too long (Table 50-2). One must be especially careful to avoid wrapping elastic bandages too snugly. Before discharge from the ED, instruct patients to loosen an elastic bandage if it feels too tight, and be sure that they have access to emergency follow-up care. It is often advisable to start patients on a regimen of early protected motion. This means that the patient removes the splint for a specified period, performs a prescribed exercise, and then replaces the splint. A splint is not an all-or-none device, and the patient is generally weaned from it slowly before it is discarded entirely. A stiff hand is a nonfunctional one, and stiffness is often a consequence of prolonged immobilization. It is important for patients to be made aware of their responsibility for the injured hand.
TABLE 50-2
Useful Estimates of Splint Times for Various Hand Problems
| INJURY | SPLINT TYPE | IMMOBILIZATION TIME* |
| Mallet finger | FIN | 8 wk |
| Boutonnière deformity | FIN | 6 wk |
| Distal phalanx—soft tissue | FIN | 1-2 wk |
| Extensor tendon | DHWF | 3 wk |
| Sprain-strain† | ||
| Interphalangeal joint | FIN | 1-2 wk |
| Wrist | DHWF | 1-2 wk |
| Hand burn | DHWF | 5-7 wk |
| Infection | ||
| Digit | DHWF | 5-7 day |
| Hand | DHWF | 5-7 day |
| Severe hand contusion | DHWF | 5-7 day |
| Fracture | ||
| Distal phalanx | FIN | 2-3 wk |
| Middle phalanx | FIN | 2-3 wk |
| Proximal phalanx | DHWF | 2-3 wk |
| Metacarpal | DHWF | 2-3 wk |
| Carpal tunnel | DHWF | Night only |
| de Quervain’s disease | DHWF | 2-3 wk |
| Trigger finger | FIN | Night only |
DHWF, digit-hand-wrist-forearm; FIN, finger.
*These are average times only. Every patient is treated as an individual when a splint is used. Clinical judgment is critical.
†Diagnosis of a sprain should be made only after a thorough effort has been made to rule out a fracture or dislocation. This is particularly true in the wrist.
Sling, Swathe and Sling, and Shoulder Immobilizer
Use a sling to maintain elevation and provide immobilization of the hand, forearm, and elbow (Fig. 50-17). It is most often used in conjunction with a plaster splint or cast. A number of commercial slings are available to choose from. Many of them are fairly economical and simple to use, whereas others are more expensive and do not allow the versatility of a simple, inexpensive triangular muslin bandage. When applying a sling, make it long enough to adequately support the wrist and hand. A sling that is too short will allow the wrist and hand to hang down (ulnar deviate) and can result in ulnar nerve injury.
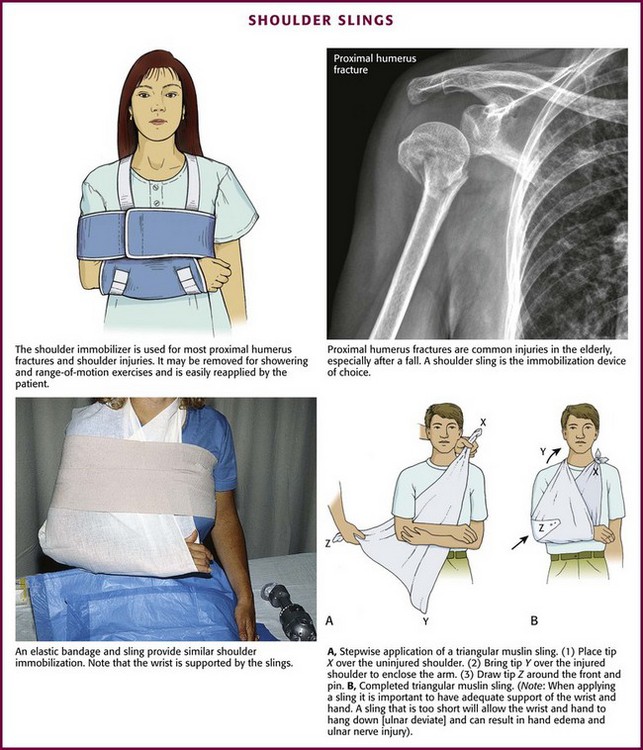
Figure 50-17 Shoulder slings.
Figure-of-Eight Clavicle Strap
In the past, clavicle fractures were often treated with an uncomfortable and complex figure-of-eight bandage. Despite its early popularity, this device never proved to be superior to a simple sling (in terms of cosmesis, functional outcome, or pain relief).14,15 Moreover, use of a figure-of-eight clavicle strap may actually promote nonunion or increase the deformity at the fracture site. When compared with a simple sling, a figure-of-eight clavicle strap is very uncomfortable, prohibits bathing, often causes chafing and discomfort in the axilla, and may predispose to axillary vein thrombosis.4 Thus, most emergency clinicians have abandoned the figure-of-eight dressing in favor of a simple sling, which is sufficient to treat most clavicular fractures.
Lower Extremity Splints
Knee Immobilizer
Indications.: A knee immobilizer (Fig. 50-18) is commonly used for mild to moderate ligamentous and soft tissue injuries involving the knee. It is removable and extremely easy to apply, which makes it popular among patients and clinicians alike. In most EDs it has replaced the more bulky plaster splint. Its use should be restricted to injuries that do not require immediate surgical intervention, traction, or casting. For these injuries, in which temporary but more complete immobilization is needed, use a plaster knee splint because it provides better stabilization and costs much less than a knee immobilizer. The exact scientific benefit of a knee immobilizer is poorly studied and difficult to document. However, it clearly helps relieve pain and, at least theoretically, hastens healing.
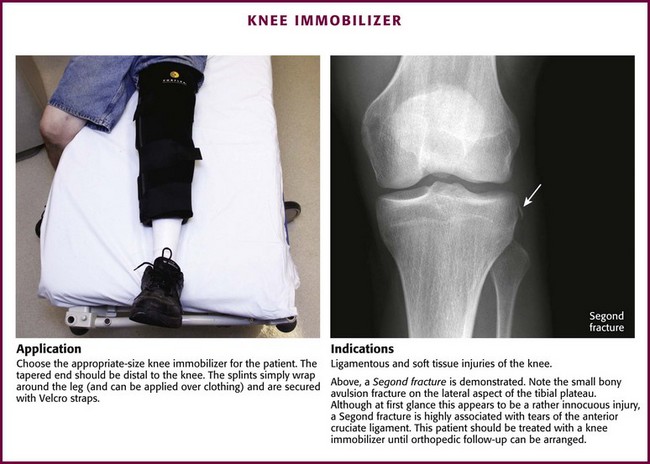
Figure 50-18 Knee immobilizer.
Application.: Knee immobilizers are available in small, medium, large, and extra-large sizes. To choose the appropriate size, place the knee immobilizer next to the injured leg so that the tapered end lies distal to the patient’s knee; if present, the cutout patellar area on the anterior aspect of the splint lies adjacent to the knee joint. In this position, the splint should extend distally to within a few inches of the malleoli and proximally to just below the buttocks crease. To apply the knee immobilizer, slide the open splint under the injured leg, wrap it around the extremity, and secure it in place with the Velcro straps. A knee immobilizer can be applied directly over clothing, thus obviating the need to remove or cut the patient’s pants.
Posterior Knee Splint
Indications.: In many EDs the knee immobilizer has virtually replaced the plaster knee splint for mild to moderate injuries to the knee. However, a plaster knee splint can be particularly useful in patients whose extremities are too large for a knee immobilizer, in the treatment of angulated fractures, or for temporarily immobilizing injuries that require immediate operative intervention or orthopedic referral. The posterior (gutter) knee splint (Fig. 50-19) is the type most commonly applied, but as alternatives, two parallel splints can be placed along each side of the leg and foreleg to create a bivalve effect (see Fig. 50-19B), or a long leg U-splint can be applied (see later). A bilateral knee splint is slightly more difficult to apply than a posterior knee splint, but it may provide better immobilization of the lateral and medial collateral ligaments and can be used for injuries to these structures.
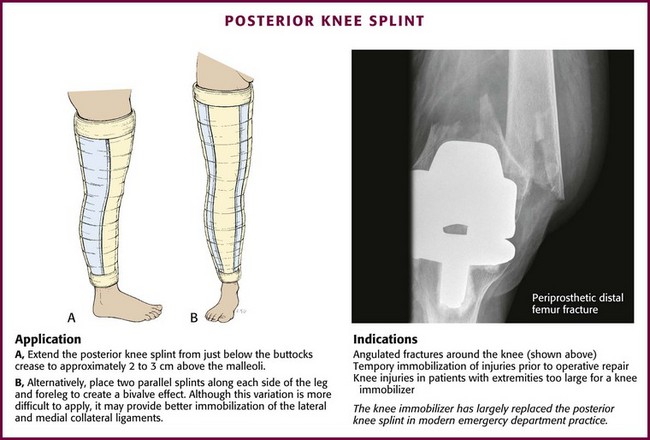
Figure 50-19 Posterior knee splint.
Construction.: Construct a posterior knee splint with 12 to 15 layers of 6-inch plaster. It should run from just below the buttocks crease to approximately 5 to 8 cm above the malleoli. The sides of the splint are folded upward to form a gutter configuration.
Application.: Apply a stockinette in the usual manner, and wrap the leg with 4- or 6-inch Webril. Have an assistant elevate the leg and hold the splint in place while securing it to the extremity with 4- or 6-inch elastic bandages. If no aide is available, place the patient in the prone position and have him use his toes to elevate the lower part of the leg off the bed to allow sufficient room to wrap the Webril and elastic bandages around the injured extremity. Lay the splint along the posterior surface of the extremity, and secure it in place with 4- or 6-inch elastic bandages.
Jones Compression Dressing
Indications.: A Jones compression dressing is commonly used for short-term immobilization of soft tissue injuries of the knee. It immobilizes and compresses the knee, thereby reducing both pain and swelling. However, because it does allow slight flexion and extension of the knee, it should not be used for injuries that require strict immobilization. In addition, it is difficult to maintain the splint for more than a few days.
Application.: To apply a Jones dressing, place the patient supine on the stretcher. If available, ask an assistant to elevate the patient’s leg to facilitate wrapping. If no help is available, place a pillow under the patient’s heel to lift the extremity off the stretcher. Wrap Webril around the extremity from the groin to a few inches above the malleoli. Use two or three layers of Webril and overlap the previous turn by 25% to 50%. Complete the dressing by wrapping 6-inch elastic bandages (two are usually required) around the Webril. If more support is required, repeat the process with another two or three layers of Webril held in place by additional elastic bandages.
Ankle Splints
Indications.: A posterior ankle splint (Fig. 50-20) is one of the most common splints applied in the ED. As noted in the introductory section, the entire concept of splinting an acutely sprained ankle has been questioned, with no firm evidence to support better outcomes with splinting or casting versus functional management (early mobilization with an external support). Nonetheless, an acutely sprained ankle is painful, and if nothing else, splinting for a few days helps alleviate the pain.
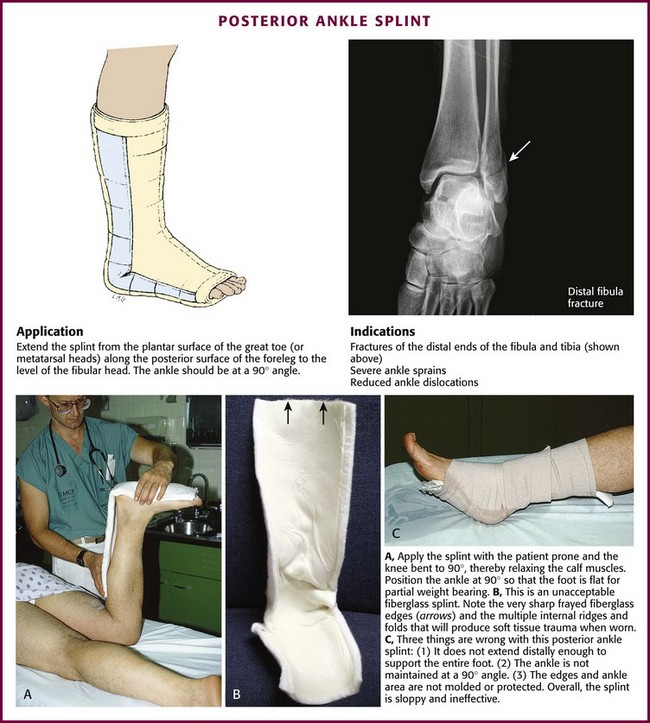
Figure 50-20 Posterior lower leg splint.
Use a posterior splint primarily to immobilize severe ankle sprains, fractures of the distal ends of the fibula and tibia, and reduced ankle dislocations. It can also be used for fractures of the tarsal and metatarsal bones or for other foot conditions that require immobilization. With particularly severe or unstable injuries, an additional anterior splint may be used to provide extra immobilization resembling that of a formal cast (Fig. 50-21). For severe lateral or bilateral ligamentous injuries, add a U-splint or stirrup splint (see later) to the posterior splint for increased immobilization. With minor soft tissue injuries, patients may have partial weight bearing on ankle splints after 24 hours. If the patient will be bearing weight, wearing a cast shoe over the splint makes it easier to walk and increases the longevity of the splint. Generally, though, walking on the splint is prohibited if immobilization for more than 2 or 3 days is desired.
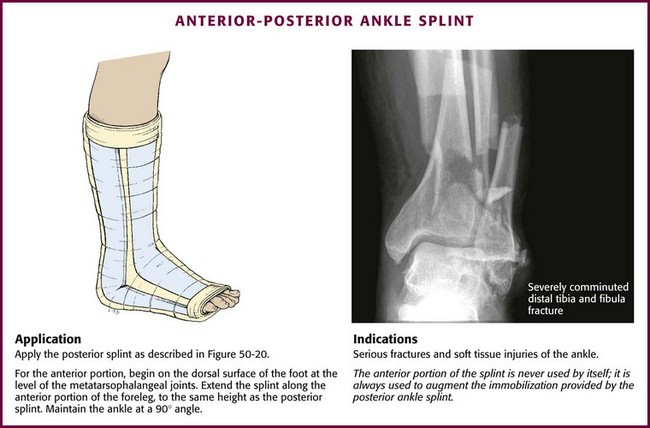
Figure 50-21 Anterior-posterior ankle splint.
Construction.: Make the posterior splint with 4- or 6-inch-wide plaster strips. It should extend from the plantar surface of the great toe or metatarsal heads along the posterior surface of the foreleg to the level of the fibular head. If it hurts to move the toes, incorporate them into the splint (after padding is placed between the digits). It is a common mistake to apply a posterior splint that does not extend far enough to support the ball of the foot. Use 15 to 20 layers if partial weight bearing is allowed because this splint frequently breaks or cracks when walked on.16
Application.: The easiest way to apply a posterior splint is to place the patient in the prone position with the knee and ankle flexed at a 90-degree angle. Failure to place the ankle in a 90-degree angle results in a plantar-flexed splint. A supine patient may help maintain the ankle in a 90-degree angle by pulling up on the foot with a wide stockinette stirrup. Flexing the knee to a 90-degree angle relaxes the gastrocnemius muscle and facilitates ankle motion. With the knee and ankle in the proper position, apply a stockinette and pad the foot and leg with Webril as described earlier. Use extra padding over bony prominences, particularly the malleoli. To prevent skin maceration, place pieces of Webril or gauze between the toes if they are to be included in the splint. Lay the wet plaster over the plantar surface of the foot and secure it in place by folding back the ends of the stockinette and Webril and wrapping with one or two 4-inch-wide elastic bandages. Carefully mold the wet plaster around the malleoli and instep to ensure maximum comfort and immobilization. Leave the toes partially exposed for later examination of color and capillary refill.
Anterior-Posterior Splint
Indications.: An anterior splint is never used by itself, but it can augment a posterior splint to create a bivalve effect (see Fig. 50-21). Use it for serious fractures and soft tissue injuries of the ankle.
Construction.: Cut a piece of plaster several centimeters shorter than the one used for the posterior splint, but since this splint does not bear weight, only 8 to 10 layers are required.
Application.: Position the patient and apply padding as described for a posterior splint. After the wet posterior splint has been applied, place the anterior splint over the anterior aspect of the ankle and foreleg parallel to the posterior splint. Hold the two in place with elastic bandages as described earlier for a posterior splint alone. An assistant is needed to apply an anterior-posterior splint because it is extremely difficult to hold both splints in place while wrapping the elastic bandages. Once secured, carefully mold both splints over the instep and ankle joint.
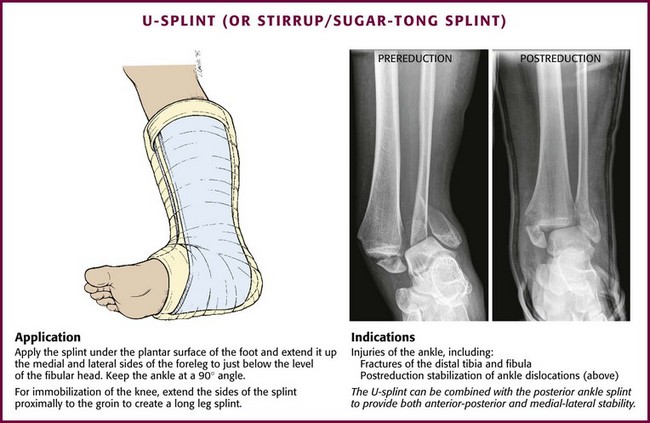
U-Splint (Stirrup Splint)
Indications.: Use a U-splint or stirrup splint (Fig. 50-22) primarily for injuries to the ankle. It functions like a posterior splint, and either one provides satisfactory ankle immobilization. In one study that compared these splints in normal volunteers, the U-splint allowed less plantar flexion and broke less often with plantar flexion than did the posterior splint.16 Also, because it actually covers the malleoli, a U-splint may protect the medial and lateral ligaments from further injury better than a posterior splint can.
Construction.: Construct a U-splint of 4- or 6-inch-wide plaster strips. The splint passes under the plantar surface of the foot from the calcaneus to the metatarsal heads and extends up the medial and lateral sides of the foreleg to just below the level of the fibular head.
Application.: Position the patient and pad the extremity as described for a posterior splint. Lay the wet plaster across the plantar surface of the foot between the calcaneus and the metatarsal heads with the sides extending up the lateral and medial aspects of the foreleg. Secure it in place with 4-inch elastic bandages. Wrap the elastic bandage around the extremity starting at the metatarsal heads and continuing around the ankle in a figure-of-eight configuration. Once the ankle has been wrapped, use another 4- or 6-inch elastic bandage to secure the remainder of the splint in place. Carefully mold the splint around the malleoli. The plaster may overlap on the anterior aspect of the ankle; this overlap does not interfere with the splint’s ability to accommodate further swelling. Note that if a U-splint is combined with a posterior splint, apply the posterior splint first.
Walking Boots
Indications.: Use a walking boot (e.g., Cam Walker Boot) for the treatment of moderate to severe soft tissue injuries of the ankle, including second- and third-degree sprains (Fig. 50-23A).17 In addition, many orthopedic surgeons use it for isolated, nondisplaced lateral malleolar fractures.18 A walking boot provides a degree of immobilization similar to that of a U-splint but is easier to remove for bathing and dressing, and the Velcro straps allow adjustment for edema.
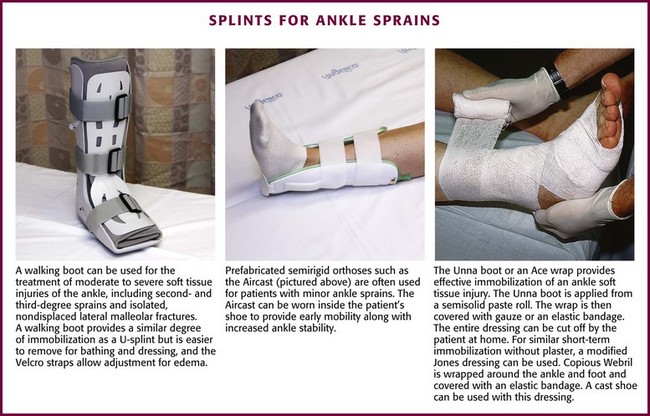
Figure 50-23 Splints for ankle sprains.
Refer patients in a walking boot for follow-up with an appropriate specialist. Advise them of the importance of partial or non–weight bearing as indicated by the type and degree of injury. When cleared by the follow-up physician, a walking boot allows easy transition to full weight bearing. Studies have shown that rapid mobilization after ankle injuries improves functional outcome and reduces disability time.7
Application.: Walking boots come in a variety of sizes from extra small to extra large, depending on the manufacturer. The boot should fit comfortably with the patient’s calcaneus snugly in the heel of the boot and the patient’s toes close to but not extending over the front edge of the boot. Once the appropriate size has been determined, place the patient’s bare foot and ankle into the boot, and adjust the Velcro straps for a secure, but comfortable fit.
Semirigid Orthosis
Indications.: In patients with lateral ankle sprains associated with a stable joint, a functional brace with early mobilization is frequently more comfortable and results in earlier return to normal function than does complete immobilization in a plaster splint or cast (see Fig. 50-23B).17–25 Consequently, functional bracing with early mobilization has become the treatment of choice in most EDs. However, it should be pointed out that there is no documented difference in long-term outcome between the two methods of treatment.
Application.: Most functional ankle braces resemble a U-splint with air bladders (Aircast, Inc., Summit, NJ) or foam padding (DeRoyal, Inc., Powell, TN) for cushioning the malleoli. The braces are secured about the ankle with Velcro straps. The device can be worn within the patient’s shoe over a sock and helps eliminate ankle instability.
Hard Shoe (Cast or Reese Shoe)
Indications.: Use a hard shoe to help reduce pain on ambulation in patients with fractures or soft tissue injuries of the foot. This device can also be used over a splint or cast to allow partial weight bearing. A hard shoe is commonly used for fractured toes that have been buddy-taped.
Application.: If a cast shoe is going to be used for a patient with a fractured toe, first buddy-tape the injured digit to the adjacent toe (Fig. 50-24). After this is done, the patient can slip the hard shoe on like a sandal. Fasten the shoe with ties or Velcro straps.
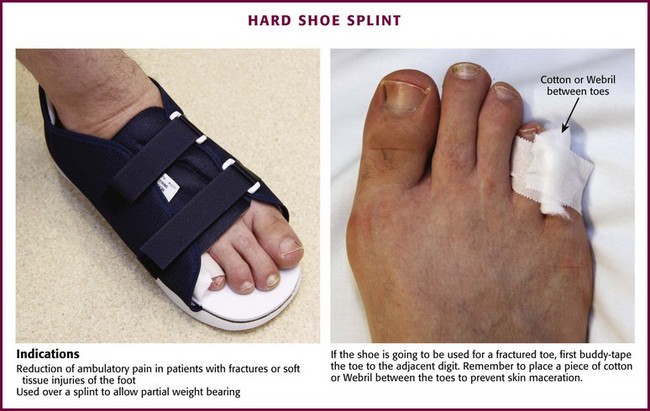
Figure 50-24 Hard shoe splint.
Ankle Wraps and Bandages
There are no data supporting the routine use of ankle wraps for simple sprains, but some pain relief may be afforded by a proper wrap. Some type of temporary immobilization is commonly used in the ED and usually requested and expected by patients. For minor ankle injuries, a simple elastic (Ace) bandage can be applied. Use a figure-of-eight configuration (see Fig. 50-23C). Apply the wrap to give only lateral support with minimal compression. It should not be tight enough to impair venous drainage, a common problem when patients apply their own elastic wraps (see Fig. 50-2).
An Unna boot placed over Webril is an alternative to a simple elastic bandage (see Fig. 50-23C). The Unna boot is constructed from a semisolid paste roll that hardens as it dries. Apply an Unna boot in a figure-of-eight configuration, similar to a simple elastic bandage. Once in place, wrap the ankle with roller gauze or an elastic bandage. The entire dressing can be cut off by the patient at home.
Soft Cast
Indications.: A soft cast is basically a modified Jones compression dressing for the ankle. Use it for minor ligamentous and soft tissue injuries of the foot and ankle that do not require prolonged or complete immobilization. A soft cast can help reduce the pain and swelling often associated with mild ankle sprains, and it gives support for early weight bearing.
Application.: Place the patient in a supine position with the foot and ankle extending off the end of the stretcher. Alternatively, ask an assistant to elevate the leg or place pillows under the knee and foreleg. Wrap the ankle and foot with five to seven layers of Webril starting at the metatarsal heads and continuing around the ankle in a figure-of-eight configuration. Extend the Webril 5 to 7 cm above the malleoli and overlap each turn by 25% to 50% of its width. After the Webril is in place, wrap an elastic bandage around the foot and ankle in a similar fashion. Additional layers of Webril and elastic bandages are seldom required. A cast shoe can be used with this dressing.
Complications of Splints
A compartment syndrome leading to ischemic injury and ultimately to a Volkmann ischemic contracture is the most worrisome complication of cylindrical casts. Although the risk for ischemia is drastically reduced with splinting, Webril or elastic bandages can cause significant constriction. To reduce the likelihood of constriction occurring, do not pull the elastic bandage excessively tight. If the patient has a high-risk injury, cut the Webril lengthwise before the plaster is applied. Stress the importance of elevation, no weight bearing, and application of cold packs, and carefully review the signs and symptoms of vascular compromise with every patient. All patients whose injuries have the potential for significant swelling or loss of vascular integrity should receive follow-up care in the first 24 to 48 hours. Never ignore complaints of increasing pain under a splint. Patients with splint-related discomfort must be reevaluated clinically and should not be treated with a telephone prescription for opioid analgesics (Fig. 50-25).
Heat Injury
Fiberglass splints produce minimal heat when drying, but plaster generates considerable heat as it hardens. Many clinicians are unaware of the potential for drying plaster to produce second-degree burns.26 Thermal injury can occur with both cylindrical casts and plaster splints. Some clinicians have reported a higher incidence of burns with the use of plaster splints, although the reasons for this are unclear.26,27 Box 50-4 lists factors that can increase the amount of heat produced during plaster recrystallization. Their effects are additive, and this fact should be taken into account when applying a splint. For example, if 15 sheets of plaster are needed for strength in a particular splint, one should not increase the heat production further by using extra-fast–drying plaster or reusing warm dip water. To avoid plaster burns, use only 8 to 12 sheets of plaster when possible, use fresh dip water with a temperature near 24°C, and never wrap the extremity in a sheet or pillow during the setting process. Peak temperatures usually occur between 5 and 15 minutes after plaster wetting.
Pressure Sores
Pressure sores are an uncommon complication of short-term splinting (Fig. 50-26).28 They can result from stockinette wrinkles, irregular wadding of Webril, incorrectly padded or unpadded bony prominences, irregular splint ends, plaster ridges, or indentations produced from using the fingers rather than the palms to smooth and mold the wet plaster. Attention to detail during padding and splinting reduces the incidence of pressure sores. However, whenever a patient complains of a persistent pain or burning sensation under any part of a splint, remove the splint and inspect the symptomatic area closely. The padding incorporated in premade plaster and fiberglass splints is generally all that is needed for safe short-term splinting. However, the life of a splint applied in the ED may be longer than intended by the clinician; therefore, it is prudent to err on the side of additional padding when placing splints on patients who may overuse the splint, such as those who will not use crutches, or for those who may not have ready access to follow-up.
Infection
Bacterial and fungal infections can occur under a splint.29,30 Infection is more common in the presence of an open wound but may occur with intact skin or in a skin lesion produced by prolonged splinting. The moist, warm, and dark environment created by the splint is an excellent nidus for infection. Toxic shock syndrome has been rarely reported from a staphylococcal skin infection that clandestinely developed under a splint or cast. Also, it has been shown that bacteria can multiply in slowly drying plaster. To avoid infection, clean and débride all wounds before splint application, and use clean, fresh tap water for plaster wetting. If necessary, apply a removable splint that allows periodic wound inspection or local wound care.
Dermatitis
Occasionally, a rash develops under a plaster cast or splint.31–35 Allergy to plaster is exceedingly rare, but there are several reports of contact dermatitis when formaldehyde and melamine resins are added to the plaster.33,34 The rash is usually pruritic with weeping papular or vesicular lesions. Because these resins are unnecessary for ED splints, their use should be avoided whenever possible. Dermatitis has also been reported with the use of fiberglass splinting material.36
Pruritus
Itching under a cast can be problematic. Patients, especially children, use various objects such as a pencil, coat hanger, or fork to get to the itch. This can cause skin maceration and possible infection, or a foreign body can be left under the cast (Fig. 50-27).
Joint Stiffness
Some degree of joint stiffness is an invariable consequence of immobilization (Fig. 50-28). It can range in severity from mild to incapacitating and can result in transient, prolonged, or in some cases, permanent loss of function. Stiffness appears to be worse with prolonged periods of immobilization, in elderly patients, and in patients with preexisting joint diseases such as rheumatoid arthritis or osteoarthritis. Thus, splints should be left on for only the time necessary for adequate healing. Table 50-3 lists several injuries that commonly require splinting, along with some suggestions for length of immobilization. Fractures, dislocations, or other conditions that require prolonged immobilization (>7 days) should have orthopedic follow-up. Tell patients that a splint is only a short-term device and that prolonged immobilization can be detrimental. For minor injuries, suggest that patients use their own judgment about when to remove the splint, but a definite end point should be set.
TABLE 50-3
Suggested Length of Immobilization for Conditions That Frequently Require Splinting
| LENGTH OF CONDITION | IMMOBILIZATION (DAYS) |
| Contusions | 1-3 |
| Abrasions | 1-3 |
| Soft tissue lacerations | 5-7 |
| Tendon lacerations | Variable* |
| Tendinitis | 5-7 |
| Puncture wounds and bites | 3-4 |
| Deep space infections and cellulitis | 3-5 |
| Mild sprains | 5-7 |
| Fractures and severe sprains | Variable† |
*Considerable controversy surrounds the length of immobilization for tendon lacerations, and duration is therefore best left to the consultant surgeon.
†Usually requires prolonged immobilization, which is best determined by an orthopedic surgeon.
Cast Pain
Cast-related pain is a common complaint that brings patients to the ED. Because of the potential for ischemia with circumferential casts, fully investigate all complaints, and rule out vascular compromise. If a patient states that a cast is too tight, it probably is (see Fig. 50-25). Do not prescribe narcotics for cast pain until a properly fitting (i.e., one that is not too tight) cast has been ensured.
Perform a detailed history and physical examination on all patients complaining of cast pain. The nature and onset of the pain are of particular importance. A dull, nonspecific pain that has worsened gradually since the time of injury may be the only clue to an early compartment syndrome (see Chapter 54). A sudden onset of throbbing pain associated with swelling and redness suggests a possible deep venous thrombosis. In both these cases, rapid intervention is the key to decreasing morbidity and mortality. During the physical examination, pay particular attention to areas of tenderness and the effect of active and passive movement on the severity of the pain.
To loosen a cast, use an oscillating cast saw to cut along the medial and lateral aspects of the cast (Fig. 50-29). This is called bivalving the cast, and it allows the halves to be spread and reapplied in a less constricting manner while still maintaining proper immobilization. To use an oscillating power saw, proceed in a series of downward cutting movements facilitated by wrist supination, and remove the blade between cuts to prevent it from getting hot enough to burn the skin. This is particularly important if synthetic material has been used in the cast. Also, do not allow the blade to slide along the skin, and never use the saw on unpadded plaster. In an apprehensive patient, demonstrate that the cast saw blade only vibrates (it does not turn) and that it does not cut the skin.
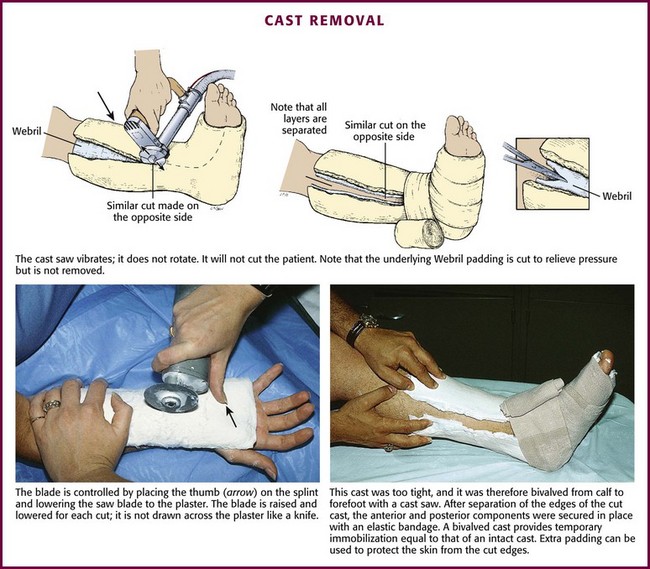
Figure 50-29 Cast removal.
After the medial and lateral sides of the cast are completely cut through, separate the two halves with a cast spreader, and cut the padding lengthwise with scissors. This may be sufficient to relieve early ischemia if the problem is simple postinjury swelling, but both the padding and the cast can be totally removed to inspect the injured area if necessary. If ischemia cannot be ruled out, measure compartment pressures (Chapter 54) and obtain an orthopedic consultation.
References are available at www.expertconsult.com
References
1. Howes, DS, Kaufman, JJ. Plaster splints: techniques and indications. Am Fam Physician. 1984;30:215.
2. Wu KK, ed. Techniques in Surgical Casting and Splinting. Philadelphia: Lea & Febiger, 1987.
3. Simon RR, Koenigsknecht SJ, eds. Emergency Orthopedics. The Extremities, 3rd ed, Norfolk, CT: Appleton & Lange, 1995.
4. Rockwood CA, Green DP, eds. Fractures in Adults, 5th ed, Philadelphia: Lippincott; Williams & Wilkins, 2001.
5. Brackenbury, PH. A comparative study of the management of ankle sprains. Br J Clin Pract. 1983;37:181.
6. Hedges, JR, Anwar, RA. Management of ankle sprains. Ann Emerg Med. 1980;9:298.
7. Kerkhoffs, GM. Immobilization for acute ankle sprain: a systemic review. Arch Orthop Trauma Surg. 2001;121:462.
8. Wehbe, MA. Plaster uses and misuses. Clin Orthop. 1982;167:242.
9. Luck, JV. Plaster of paris casts: an experimental and clinical analysis. JAMA. 1944;124:23.
10. Ortho-Glass Splinting Manual. Charlotte, NC: Parker Medical Associates, 1994.
11. Lavalette, R, Pope, MH, Dickstein, H. Setting temperatures of plaster casts. J Bone Joint Surg Am. 1982;64:907.
12. Gannaway, JK, Hunter, JR. Thermal effects of casting materials. Clin Orthop. 1983;181:191.
13. Clay, NR, Dias, JJ, Costigan, PS, et al. Need the thumb be immobilised in scaphoid fractures? A randomised prospective trial. J Bone Joint Surg Br. 1991;73:828.
14. Stanley, D, Norris, SH. Recovery following fractures of the clavicle treated conservatively. Injury. 1988;19:162.
15. Andersen, K, Jensen, PO, Lauritzen, J. Treatment of clavicular fractures: figure-of-8 bandage versus a simple sling. Acta Orthop Scand. 1987;58:71.
16. Halvorson, G, Iserson, KV. Comparison of four ankle splint designs. Ann Emerg Med. 1987;16:1249.
17. Pommering, TL, Kluchurosky, L, Hall, SL. Ankle and foot injuries in pediatric and adult atheletes. Prim Care. 2005;32:235.
18. Stuart, PR. Comparative study of functional bracing and plaster treatment of stable lateral malleolar fractures. Injury. 1989;20:323.
19. Brooks, S, Potter, B, Rainey, J. Treatment for partial tears of the lateral ligament of the ankle: a prospective trial. BMJ. 1981;282:606.
20. Bergfeld, JA, Cox, JS, Drez, D, et al. Symposium: management of acute ankle sprains. Contemp Orthop. 1986;13:83.
21. Gross, MT, Bradshaw, MK, Ventry, LC, et al. Comparison of support provided by ankle taping and semirigid orthosis. J Orthop Sports Phys Ther. 1987;9:33.
22. Friden, T, Zatterstrom, R, Lindstrand, A, et al. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17:118.
23. Moller-Larsen, F, Wethelund, J, Jurik, A, et al. Comparison of three different treatments for ruptured lateral ankle ligaments. Acta Orthop Scand. 1988;59:564.
24. Konradsen, L, Holmer, P, Sondergaard, L. Early mobilizing treatment for grade III ankle ligament injuries. Foot Ankle. 1991;12:69.
25. Eiff, M, Smith, A, Smith, G. Early mobilization versus immobilization in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22:83.
26. Kaplan, SS. Burns following application of plaster splint dressings. Report of two cases. J Bone Joint Surg Am. 1981;63:670.
27. Becker, DW, Jr. Danger of burns from fresh plaster splints surrounded by too much cotton. Plast Reconstr Surg. 1978;62:436.
28. Beidler, JG. Skin complications following cast applications. Report of a case. Arch Dermatol. 1968;98:159.
29. Houang, ET, Buckley, R, Williams, RJ, et al. Outbreak of plaster-associated Pseudomonas infection. Lancet. 1981;1:728.
30. Houang, ET, Buckley, R, Smith, M, et al. Survival of Pseudomonas aeruginosa in plaster of Paris. J Hosp Infect. 1981;2:231.
31. Conrad, AH, Ford, LT. Allergic contact dermatitis caused by Melmac orthopedic composition. JAMA. 1953;153:557.
32. Logan, WS, Perry, HO. Cast dermatitis due to formaldehyde sensitivity. Arch Dermatol. 1972;106:717.
33. Lovell, CR, Staniforth, P. Contact allergy to benzalkonium chloride in plaster of paris. Contact Dermatitis. 1981;7:343.
34. Logan, WS, Perry, HO. Contact dermatitis to resin-containing casts. Clin Orthop. 1973;90:150.
35. Pichler, BA, Snyder, M. Contact dermatitis caused by plaster casting material. J Am Podiatr Med Assoc. 1985;75:108.
36. Sertoli, A, Giorgini, S, Farli, M. Fiberglass dermatitis. Clin Dermatol. 1992;10:176.