Skeleton19
4.2 Joints21
4.3 Muscle23
Skeletal tissue exists for mechanical support. The structure and rigidity of bone reflect its weightbearing function and it is well supplied with blood. Bone formation (ossification) occurs in two ways: direct from membrane, and by means of a cartilaginous precursor. Ossification is not complete until late adolescence, thus allowing bone growth to take place. Joints can be classified as non-synovial (limited movement) and synovial (extensive movement). Another function of bone is the manufacture of blood cells (haemopoiesis). Skeletal muscle (histologically striated) is supplied by voluntary nerve impulses. Smooth muscle is supplied by involuntary nerve impulses. Cardiac muscle, although striated, has intrinsic contractility and is supplied by involuntary nerves.
You should:
• list the functions of cartilage and bone
• describe the blood supply of bone and how bone grows
• list the different types of joints and their relative mobility
• list the different characteristics of skeletal, smooth and cardiac muscle
• explain that skeletal muscles work in groups that usually share a common nerve supply.
4.1. Skeleton
Cartilage and bone provide mechanical support. Cartilage is more flexible than bone but confers insufficient rigidity to withstand gravity (large cartilaginous creatures are aquatic, where gravity matters less). Some cartilages remain more or less the same throughout life, while others undergo a gradual conversion to bone – ossification – which takes place before birth or during childhood and adolescence.
Bony skeleton (Fig. 4.1)
• Axial skeleton: skull, hyoid, vertebral column (including the sacrum), ribs, and sternum.
• Appendicular skeleton: pectoral and pelvic girdles, limb bones:
– pectoral girdle: clavicle, scapula
– upper limb: humerus, radius, ulna, carpal bones, metacarpals, phalanges
– pelvic girdle: hip bone (ilium, ischium, pubis)
– lower limb: femur, tibia, fibula, tarsal bones, metatarsals, phalanges.
 |
| Fig. 4.1 |
Sesamoid bones are bones that develop in tendons as they cross joints. The patella is an example, and there are others in the wrist and the feet.
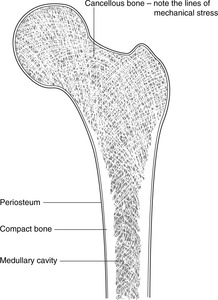
Section through bone (Fig. 4.2)
Important terms are:
• Cortical or compact bone: dense bone around the edges.
• Cancellous, trabecular or spongy bone in which the lines of mechanical stress are evident in the structure of the bone.
• Periosteum: the membranous covering. It has two layers: outer fibrous and inner cellular. The inner layer is vascular and contains stem cells which can when required differentiate into osteoblasts, for example in healing and repair. Damage to periosteum impairs bone healing.
• The medullary (marrow) cavity. This and the spaces in cancellous bone contain haemopoietic (blood-forming) cells; there is therefore a profuse arterial supply.
Parts of a long bone
• Head: one end, usually the proximal.
• Neck: the area immediately distal to the head.
• Condyles: rounded articular surfaces.
• Epicondyles: prominences adjacent to condyles.
• Epiphysis: the name given to the developing ends of a long bone (see later).
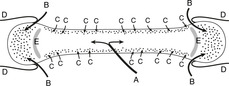
Arterial supply of a long bone (Fig. 4.3)
• A large nutrient artery enters through the nutrient foramen (Fig. 4.3A). Branches of this reach the ends of a mature long bone, but not of a developing long bone (see below).
• Capsular (retinacular) vessels enter the bone with the attachments of the joint capsule (Fig. 4.3B).
• Many small arteries penetrate the periosteum directly, particularly at the site of muscular attachments and near joints (Fig. 4.3C).
• Bones have a particularly rich blood supply because haemopoiesis (formation of blood components) takes place in the central marrow cavity.
Ossification and bone growth, the epiphyseal plate
The ends of bone – the epiphyses – are the last parts of a long bone to ossify, and until then they remain separated from the shaft of the bone by the epiphyseal plate of hyaline cartilage (Fig. 4.3E). Because these epiphyseal plates are the sites of growth in length, they are also known as growth plates. Blood vessels never cross epiphyseal plates and so the nutrient artery of the shaft contributes no supply to the ends of a developing long bone until after the epiphyseal plate has disappeared with final fusion of all the components of a bone. This matters: damage to the blood supply can result in death (necrosis) of the bony tissue and if this affects the growing end of a bone in children, normal development may be delayed or prevented. If it affects part of a bone that participates in a joint, movement will be affected.
Bone growth does not stop when ossification is complete: there is a continuous process of bony remodelling in response to altered stress.
Secretion of too much growth hormone before epiphyseal fusion results in gigantism, and after fusion, acromegaly (large extremities). Achondroplasia is a hereditary defect of endochondral ossification in which long bones of the limb fuse early giving short limbs, while the trunk and skull develop normally. Adolescent athletes who use growth hormone will find that it prolongs the life of the epiphyseal plate and delays the fusion of the ends of any long bones not yet united. This can have serious consequences.
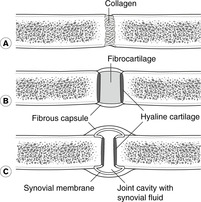
4.2. Joints (Fig. 4.4)
Bones confer rigidity; joints permit movement. They may be classified on the basis of structure as fibrous, cartilaginous or synovial. From a clinical point of view, a better classification is simply non-synovial and synovial, the former including both fibrous and cartilaginous.
 |
| Fig. 4.4 |
Non-synovial joints
Fibrous joints (Fig. 4.4A)
Two bones are bound together by fibrous tissue. Examples are the inferior tibiofibular joint, part of the ankle, a tooth fitting into the tooth socket (gomphosis), and joints (sutures) between bones of the skull vault. Fibrous joints permit little movement, except that fetal skull bones may move on each other before and during birth, but during early childhood movement becomes increasingly restricted.
Cartilaginous joints
These allow more movement. There are two types:
• Primary cartilaginous joints (not illustrated in Fig. 4.4). In these, bony tissue is separated by hyaline cartilage. The junction between the shaft and epiphysis of a long bone constitutes a primary cartilaginous joint. As the constituent parts of a long bone fuse during childhood and adolescence, primary cartilaginous joints gradually disappear, and in an adult there are only a few remaining, most notably the joint between the first rib and the sternum.
• Secondary cartilaginous joints or symphyses (Fig. 4.4B). In these, two articular surfaces are each covered by hyaline cartilage and between them is a fibrocartilaginous disc. They are found in the midline of the body and include the joints between neighbouring vertebral bodies, the joint between the two pubic bones (the pubic symphysis) and the joints between the parts of the sternum.
Age changes in cartilaginous joints. As age advances, cartilaginous joints may ossify, thus limiting movement. This occurs as a matter of course in primary cartilaginous joints (see above) and may occur in secondary cartilaginous joints. The last joint in the body to fuse in this way is that between the sphenoid and occipital bones of the skull in the mid-twenties. This is one reason why the shape of the face and head continues to change until that time.
Synovial joints (Fig. 4.4C)
In a synovial joint, articular surfaces are covered by articular cartilage (usually hyaline, sometimes fibrous) and between them is the synovial cavity limited externally by the joint capsule. Synovial membrane lines the inner aspect of the capsule and any other non-articular surface within the joint. It is important to note that synovial membrane does not cover the articular surfaces themselves. Movement is much freer at these joints, and in some cases extensive. Freedom of movement and stability are mutually incompatible: the more movement, the less stability. Joints at which a wide range of movement is permitted are associated with other means of conferring stability, such as muscles and ligaments.
Why synovial? Synovium is the name given to a specialised connective tissue that produces synovial fluid to lubricate the articular surfaces. Along with pericardium, pleura, and peritoneum it is often regarded as one of the serous membranes of the body – all involved in permitting one surface to move on another.
Types of synovial joints
A simple classification, depending upon the number of planes in which movement takes place, is:
• Plane: articular surfaces almost flat for gliding movements, e.g. some carpal joints
• Hinge: movement in one plane, e.g. elbow
• Pivot: movement around a pivot, e.g. atlanto-axial
• Saddle: saddle-shaped articular surfaces, allow movement in two planes, e.g. first carpometacarpal joint
• Ball and socket: relatively unrestricted movement, e.g. shoulder, hip.
Synovial membrane outside joints: bursas, synovial sheaths
Synovial membrane is found outside joints in places where friction resistance is necessary. There are many sites in the body where a muscle tendon or a bulky muscle passes over a bony prominence or beneath a fibrous band, often as a corner is turned. Anatomical arrangements to reduce friction at these sites include isolated synovial cavities between the opposing surfaces: bursas and synovial sheaths.
• Bursas are bags of synovial membrane and fluid found between tendons or muscles and skin or bone. They may be entirely separate from joints (even if near them), or they may be extensions of the synovial cavity of a joint. Examples of bursas are found in association with the shoulder and knee joints, but they occur elsewhere as well.
• Synovial sheaths are synovial cavities wrapped around tendons running in confined spaces, notably the wrist, hand and ankle. They will be described in more detail with the limbs.
Nerve supply of joints
Bones and joints are richly supplied with sensory nerve endings: bony and articular trauma and disease are painful. Sensory fibres from joints are found in all nerves supplying muscles that act upon the joint. In general, nerves that supply joints also supply the muscles that act on them, together with the skin over the bony attachments of those muscles: this is Hilton’s law.
Diseases of joints and synovium
• Articular surfaces may degenerate, as in osteoarthritis, which is, despite its name, a disease of hyaline cartilage. It may become severe enough to affect bone as well. This may limit movement and eventually such changes may result in the affected adjacent bones becoming fused.
• Synovium may become inflamed causing pain and limitation of movement. Rheumatoid arthritis is a disease in which inflamed and swollen synovium may become trapped between articular surfaces such that it is further damaged. This results in more inflammation and swelling, more synovial damage and more limitation of movement … and so on.
– Inflammation of a bursa: bursitis.
– Inflammation of a synovial sheath: synovitis.
– Inflammation of a synovial joint: arthritis.
4.3. Muscle
All cells are potentially capable of movement as a result of contractile proteins within them. Muscle tissue is made up of cells that are specialised for movement, and the more organised the tissue structure is, the quicker and more powerful the movement.
Skeletal muscle: voluntary
Skeletal muscle is supplied by voluntary nerve impulses. Histologically it is striated muscle – that is to say the contractile proteins are so well organised as to give rise to striations visible on microscopy. Skeletal muscle is attached to the skeleton and so causes movements of the trunk or limbs. It is also known as somatic muscle.
Visceral muscle: involuntary
Visceral muscle is supplied by involuntary nerve impulses. It is found in the wall of blood vessels and internal organs (viscera) derived from embryonic cells associated with the wall of the yolk sac or its derivatives.
• Smooth muscle is found in blood vessels and internal organs except the heart.
• Cardiac or heart muscle is striated.
Branchial arch muscle: voluntary
In the head and neck there is a third type of muscle associated with the cranial end of the gut tube (muscles of the mouth, pharynx and larynx). It is therefore visceral, but the muscles are supplied by voluntary nerves and are histologically striated. It is called branchial arch muscle because it is derived embryologically from the branchial (gill) arches.
Muscle attachments
A skeletal muscle is typically attached at both ends to bones. The muscle fibres themselves may be directly attached to an area of bone, or the muscle may form a tendon or aponeurosis (a flattened tendon) which is attached to a small area of the bone. When the muscle contracts, the two bones are approximated, causing movement at the joint between them. Muscles move joints: ‘biceps flexes the elbow’ is preferable to ‘biceps flexes the arm’. Some muscles cause movement at more than one joint because they are attached to bones separated by two or more joints. Biceps in the upper limb is such a muscle since it crosses two joints, the elbow and the shoulder. It follows that the action of biceps can be modified by activity of other muscles that stabilise one or other of the joints that biceps crosses.
Some voluntary muscles are attached at one end to the deeper layers of the skin; for example the muscles of facial expression which, when they contract, cause facial movements for expression of emotion, and communication.
Sites of muscle attachments to bone
Muscles are attached to bones either:
• directly, when the muscle fibres themselves are attached to a fairly extensive area of bone
• indirectly, when the muscle fibres converge into a tendon or an aponeurosis (flattened tendon, like a membrane) which attaches to a smaller area of bone.
Wherever a muscle or tendon is attached to a bone, the bony surface will be rough. Such an area is often sufficiently raised above the neighbouring surface to be called a process, a tuberosity, a tubercle, or a trochanter (different words for much the same thing).
It follows that a bony surface that is smooth is free of muscle attachments – indeed, such areas are often directly subcutaneous (e.g. the anteromedial surface of the tibia). You read earlier that arteries enter bones at the site of muscle attachments, and at such bony surfaces that lack muscle attachments the arterial supply is relatively poor. Because the healing process requires a generous blood supply, healing after injury may be impaired. Again, the subcutaneous surface of the tibia is a good example.
Origins, insertion, attachments
The relatively more fixed end of a muscle is known as the origin, and the relatively more mobile end as the insertion. However, there are many cases when one end of a muscle may be more fixed in a certain movement, and the other end more fixed in another movement, depending upon the posture of the body or the action being performed. For example, when you are sitting and you raise your thigh, the proximal end of the thigh muscles is more fixed and the distal end more mobile. But if you then put your feet on the ground and stand up, the distal end of the thigh muscles becomes relatively more fixed since you are raising your vertebral column upon a relatively stable lower limb. For these reasons and others, the term attachments is perfectly satisfactory. The memorising of origins and insertions is unnecessary except for physiotherapists and their colleagues.
Muscle groups
Muscles rarely act in isolation. They are found as part of a group of muscles usually supplied by the same nerve and within one fascial (connective tissue) compartment, and it is the group as a whole that acts. It is more useful clinically to talk of the extensor muscles of the thigh, or the flexor muscles of the arm than to worry about individual muscles within those groups. So not only need you not worry about remembering which end of a muscle is the origin and which the insertion, in many cases you need not worry about individual muscles – only muscle groups. The text will identify the more important individual muscles that you need to be concerned about.