37 Sacroiliac Joint Pain
Procedures for Diagnosis and Treatment
Over the last 2 decades, the sacroiliac joint (SIJ) has increasingly been recognized as an anatomic source of pain that figures in the differential diagnosis of a patient presenting with low back pain (LBP) and/or buttock pain with or without more distant referred pain.1–7 Because the SIJ is innervated, it can be a source of pain.2,8–13
Because SIJ pain refers into the buttock and iliac crest near the posterior-superior iliac spine, and also into the groin, abdomen, and leg including the foot,14,15 it can be confused with referred pain from other sources, particularly from the lumbar intervertebral disc, lumbar zygapophysial joint (ZJ), and the hip joint. Additionally, because of its propensity for referral into the leg, SIJ pain can be confused with radicular pain. Thus, it is essential that the clinician recognizes these potentially confounding features and takes adequate steps to differentiate between SIJ pain and other pain presentations.
In the early 1900s, the SIJ was thought to be the principal source of LBP,16 and an important cause of “sciatica.”17 Subsequently, and particularly after the discovery of the disc prolapse, it was considered that the lumbar spine—and in particular the lumbar intervertebral disc—was responsible for most back problems.17
Acknowledgment of the SIJ as a source of pain in the ensuing decades commenced in rheumatologic literature, but this largely related to seronegative arthropathies and case reports of various rare infections and tumors.18,19 Subsequently there have been substantial developments in the basic sciences relating to the SIJ, initially and primarily in the osteopathic, physiotherapy, and chiropractic literature,18,19 and later in biomechanical and radiologicliterature.20–26 The SIJ was overlooked as a possible pain generator outside of the inflammatory population perhaps because it was deep and inaccessible to specific accurate injection prior to the development of C-arm fluoroscopy, and because clinical examination tests had poor sensitivity and specificity. The advent of imaging-controlled diagnostic interventions has allowed for a more rational approach to diagnosis, and as a result, there is again an increasing awareness that the SIJ is an important cause of LBP and referred pain into the pelvis and leg. It is now estimated that the SIJ may be the cause of between 15% and 38% of all cases of LBP.4,27–30
The increased awareness of the potential for the SIJ to be a source of pain has not as yet translated into proven treatments. The literature concerning SIJ interventional treatment is sparse.1,31–35
Anatomy and Biomechanics
The SIJ is the articulation between the triangular sacrum and the two ilia. It is a true diarthrodial synovial joint, and is unlike any other joint in the body. Only the ventral third of the joint is a true synovial joint with a joint capsule and synovial cells;36 the remainder is composed of three ligaments,37 the ventral sacroiliac ligament, the interosseous sacroiliac ligament, and the posterior sacroiliac ligament.38 From fetal life onward, the iliac surface is fibrocartilage and the sacral surface is hyaline cartilage. Subsequent arthrosis of the joint tends to affect the fibrocartilaginous iliac side more than the sacral hyaline cartilage.39 The dorsal transition between the ligamentous and synovial components shows marked individual variability including osseous clefts, cartilage and subchondral defects, and vascular connective tissue in the bone marrow.36 Furthermore, aging is accompanied by extensive ridging in the interosseous region of the sacrum and ilium to the extent that it is present in 100% of those 55 years or older and also by ossification of the central interosseous region of the SI ligament in 60%, making it likely that by the sixth decade of life there is little or no movement in the SIJ.40 Other degenerative changes such as marginal osteophytes are not uncommon by the start of the fifth decade, at least unilaterally.41
The articular cartilage of the SIJ does not appear to degenerate in a similar manner to other synovial joints in which articular cartilage defects result in bony ankylosis. The SIJ articular cartilage is maintained even in the elderly; it seems that fibrous tissues contribute most to ankylosis so that with aging there is interposition of fibrocartilage-like tissues within the joint (complete fibrous ankylosis).42 Bony fusion seems to occur only in ankylosing spondylitis.43 Degenerative changes and intraarticular SIJ ankylosis are substantially more common in men than women.43–45
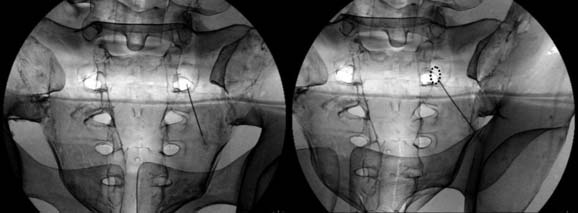
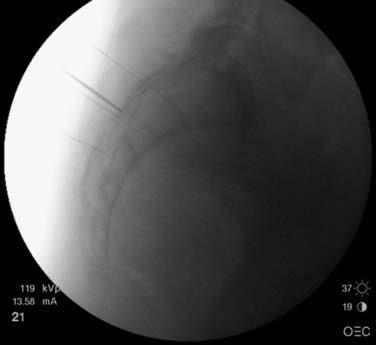
The sacrum contains four foraminal pairs on either side, S1 to S4. Each pair has a ventral and dorsal aperture. On x-ray, the ventral component of the foramen is the most obvious; the smaller dorsal foramen can be difficult to visualize. It is important to recognize this when performing imaging-guided procedures into a sacral foramen. The dorsal component of each foramen may be difficult to visualize on a static image particularly because of the superimposition of the larger ventral component and from bowel gas. However, with the use of CT scan or more preferably a C-arm image intensifier, the dorsal component can be identified. With the C-arm, this is achieved by varying the amount of obliquity and observing that the more superficial dorsal component moves to a greater extent relative to the deeper ventral component (Fig. 37-1).
The synovial part of the joint is more prominent caudally. At the level of the S1 foramen, the ventral 25% of the joint is synovial; at S2, the ventral 50% to 75% is synovial and at S3, 100% of the SIJ is synovial.46
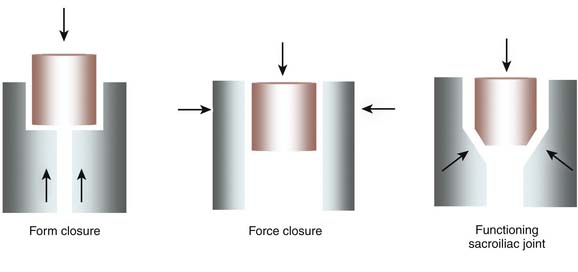
The pelvis is made up of three bones, with the sacrum positioned as the keystone in an arch from femur to femur (Fig,37-2). The stability of the sacrum within the pelvis is dependant on (1) the shape and orientation of the sacrum and its articulations with the ilia, (2) the integrity of the ligamentous structure around the joint, and (3) the extent of muscular compression across the joint. Variations in the shape and orientation of the sacrum and its articulations are rarely a problem except when these aberrations are quite extreme; for example, after pelvic fractures and in some congenital conditions. The ligamentous function of the SIJ is dependant on intact, stable ligaments and the orientation of the sacrum. The sacrum pivots in a sagittal plane around its true articular joint surface by between 6 and 11 degrees. Tilting of the superior sacrum in an anterior direction is called sacral nutation. This is its normal position, encouraged by the lumbar lordosis. Excess nutation can occur. Superiorly, such excess nutation is limited directly by the deep interosseous and long dorsal ligaments and indirectly by the iliolumbar ligament. Inferiorly, it is limited by the sacrococcygeal and sacrotuberous ligaments. If all of these ligaments are intact, nutation of the sacrum has the benefit of helping to pull the pelvic ring closed, thereby compressing the SIJs. This, the so-called “locked” position of the pelvis, has great biomechanical strength with force transfer occurring primarily through a well supported and mechanically advantaged joint surface and it ligaments. This passive locking mechanism, depending on the shape of the keystone and the integrity of the articular capsule and surrounding ligaments, is called form closure of the SIJ.
The ligaments and capsule of the SIJ cannot, however, provide adequate compression across the joint surface on their own. The primary compressors of the SIJs are muscular; their actions are termed force closure of the SIJ. Three main muscle groups have been identified: (1) muscles of the pelvic floor, (2) transverse abdominis, and (3) a posterior sling consisting of latissimus dorsi through the thoracolumbar fascia to the contralateral gluteals.20–22,47–56
Innervation
Sacroiliac joint innervation is important because the only method for making a diagnosis of SIJ origin pain is anesthetic block of the joint or its nerve supply, and one possible 53–56method of treatment is radiofrequency (RF) treatment directed at target nerves. The SIJ is definitely innervated and it can be a source of pain. The periarticular tissues of the SIJ contain mechanoreceptors and nociceptors.2 Nerve fibers varying from 0.2 micron to 2.5 microns in diameter end in five morphologically different terminals and these terminals are present in the SIJ capsule and adjacent ligaments.9 Substance P and calcitonin gene-related peptide (CGRP) immunoreactive nerve fibers have been found in the anterior SIJ capsule and interosseous ligament,13 the superficial layer of sacral and iliac cartilage, and the surrounding ligamentous structures.12 Nerves supplying the SIJ are distributed not only to the superficial and deep dorsal sacroiliac ligaments, but also to the sacrotuberous and sacrospinous ligaments; the dorsal rami continue their course laterally, sandwiched between superficial and deep portions of sacroiliac ligaments, and pierce the origin of the gluteus maximus muscle.57
It is considered that the synovial component of the SIJ has a different innervation to the posterior ligamentous component. The synovial joint is likely to be innervated mainly by ventral sources;8,9 its upper ventral portion is mainly innervated by the L5 ventral ramus and the lower ventral portion by the S2 ventral ramus or by branches from the sacral plexus.9 The synovial component has minimal innervation by the sacral dorsal rami.58
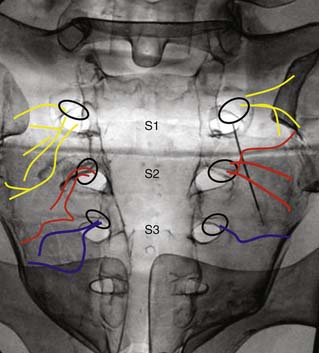
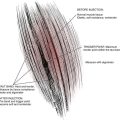
The dorsal sacroiliac ligaments are innervated by at least the L5 dorsal ramus and lateral branches of the S1-S3 dorsal rami. The L4 medial branch may be involved. The upper dorsal ligamentous structures are innervated by the L5 dorsal ramus; the lower dorsal ligaments by nerves arising from a plexus composed of lateral branches of the dorsal rami of the sacral nerves.9 These nerves range from 0.292 mm to 0.997 mm in diameter, and the nerves supplying both the synovial and ligamentous components of the SIJ complex have similar diameters.9 The lateral branches of the sacral dorsal rami emerge from the sacral foramina in a varied array, radiating cephalad, transverse, or caudad.58 When they emerge, they do not run in a constant plane,11,58,59 but run across the dorsal sacrum either through, superficial to, or deep to the dorsal sacroiliac ligament at a variable depth of up to 1 cm superficial to bone (Fig. 37-3).58,60
Pathophysiology
As noted previously, the SIJ is innervated and has the potential to be a source of pain. It can become painful as a result of both intrinsic and extrinsic factors. Intrinsic mechanisms include definitive biomedical processes such as sacroiliitis and tumors. These constitute red-flag conditions and are not covered in this chapter. The other intrinsic mechanism considered to be a risk factor in SIJ origin pain relates to aberration of biomechanical function. The technical terms used to describe these biomechanical features are form closure and force closure. Poor form closure of the SIJ is caused by inefficient bony structure/alignment, absent or stretched SIJ ligaments, or sacral counter nutation. Poor force closure is considered to arise through pain inhibition and poor firing of the compressive muscles (Fig. 37-4).61–67 It is likely that long-term lack of force closure across the SIJ can lead to increased strain on the ligamentous structures, which, over time may lengthen and cause further loss of pressure across the joint. Such a joint may then be resistant to muscular retraining.
Extrinsic mechanisms causing loss of form or force closure include trauma (macro or repetitive microtrauma), infection, and pregnancy.20,47,63,68–73
Pain in the region of the SIJ is not uncommon after posterior iliac graft harvesting.74 It occurs in 6% to 39% in patients who have had iliac grafting for spinal fusion.75,76 One possible cause is sacroiliac joint instability, caused by ligamentous disruption or violation of the synovial part of the SIJ during surgery. In patients who have had posterior iliac grafting and have persistent SIJ region pain with CT scan evidence of synovial disruption, SIJ degeneration is more prevalent on CT.77
SIJ pain is also not uncommon after spinal fusion. The prevalence of SIJ pain, diagnosed on the basis of 75% or more pain relief with local anesthetic block, in one group of patients with significant and chronic LBP postlumbar fusion surgery was found to be 35%,78 a figure that seems to be similar to that in other reports.79 Bone scan does not assist in the diagnosis of postfusion SIJ origin pain using local anesthetic as the diagnostic tool; however, clinical features that are somewhat predictive include pain that is different to the prefusion pain, particularly if it commences some time after the fusion has been performed.78 SIJ pain postfusion occurs as fusion increases the computed sacral angular motions and the average stress on the SIJ articular surface motion particularly in combined L4-5 and L5-S1 fusion.79 This can lead not only to an increased chance of pain, but also to premature SIJ degeneration; the prevalence of CT scan determined SIJ degeneration over a 5-year period postlumbar fusion was found to be 75% in one study that found a prevalence of only 38% in a matched control group.80 Consistent with the finding that L5-S1 fusion had the more significant biomechanical effect, the prevalence of SIJ degeneration was higher if the L5-S1 segment was included in the fusion.80
Sacroiliitis is characterized by chronic inflammation within the joint and the deep interosseous ligament, which forms the posterior capsule and is the largest syndesmosis in the body. Both hyperparathyroidism and repetitive shear stress injuries in athletes can mimic the presentation of sacroiliitis.81
In a study of long-term outcomes from SIJ radiofrequency neurotomy (RFN), SIJ pain was considered to be idiopathic in 30% of cases, and to derive from motor vehicle accidents in 9%, from a fall or slip in 24%, from overload or a work injury in 26%, and from other incidents in 11% of cases.82
Clinical Presentation and Diagnosis
The diagnosis of SIJ pain is predicated on diagnostic anesthetic injection because there are no other clinical or radiologic correlations that have been found to be reasonable surrogates. The most significant feature on clinical assessment of a patient considered to have SIJ origin pain is the site of pain; if the patient points to the posterior superior iliac spine (PSIS), then the pain is more likely to derive from the SIJ.28 Clinical examination has possible utility when examination findings are considered collectively. Radiologic findings are of no particular use other than in the exclusion of some red-flag conditions.
The International Association for the Study of Pain (IASP) has proposed a three-part criteria for the diagnosis of SIJ pain.83 In particular, diagnosis requires the following:
Site of Pain
In asymptomatic subjects, noxious stimulation of the SIJ evokes pain in the low back, buttock, and upper posterior thigh.4 In patients with SIJ pain established by fluoroscopically guided SIJ injection, 94% described buttock pain, 72% described lower lumbar pain, 14% described groin pain, 50% described associated lower-extremity pain, 28% described leg pain distal to the knee, and 14% reported foot pain.14 However, as noted, the most prominent site of pain presentation for SIJ pain is pain over the PSIS.28 SIJ pain rarely extends above L5.28 SIJ origin pain has a similar referral pattern to pain derived from the lumbar spine and from the hip joint,14,28 and thus, analysis of pain patterns is not in itself a reliable diagnostic factor.84
Type of Pain
SIJ pain can present with local PSIS pain and/or somatic referred pain. Local SIJ region pain can be deep and aching, but it can also be sharp and activated by movement. Somatic referred pain is generally described as diffuse, aching, and poorly localized. It is different from typical lumbar radicular pain, which is generally described as long, thin, sharp lancinating pain that can concentrate distally.85 Because SIJ-referred pain can extend into the leg, it can be confused with radicular pain, potentially leading to unnecessary spinal treatment.17,86 If the predominant pain is radicular, it is most likely to arise from the lumbar spine owing to disc prolapse or canal stenosis. However, it is not impossible for lumbosacral radicular pain to be caused by SIJ pathology. In one series, ventral capsule disruption was present in 70% of patients diagnosed with SIJ pain by intraarticular block.30 Joint injury, if associated with inflammation, can theoretically be associated with extrasacral perineural inflammation and pain.
It is also important to distinguish neuropathic pain from somatic referred pain. Neuropathic pain typically presents with descriptors such as burning, buzzing, and tingling, and has clinical features including allodynia. It can occur in association with somatic referred pain.85,86 Although uncommon, lumbosacral plexopathy, which is defined as neurologic deficit derived from the lumbosacral plexus, is more common in patients after sacral fractures than it is among the entire population of patients with pelvic and acetabular fractures.87 It stands to reason that SIJ trauma and pain can be associated with local neural damage, and hence, neuropathic pain. Fortin described five patterns of contrast medium extravasation after fluoroscopically guided SIJ injections by viewing postarthrography CT in 76 patients with LBP, of whom 61% displayed extravasation.3 It seems that extravasation does occur dorsally into the dorsal S1 foramen, superiorly at the sacral alar level to the L5 epiradicular sheath, and ventrally to the lumbosacral plexus, making it possible for local neural structures to be insulted by SIJ inflammation.
Clinical Examination
The validity of physical examination tests is reduced because they tend to stress adjacent soft tissue structures as well as the lumbar spine and hips.68
Singular examination tests such as palpation and movement tests are generally considered to be unhelpful in the diagnosis of SIJ pain.27,37,68,88,89 However, combined tests may be useful. Synovial SIJ pain can be predicted when three of five pain provocation tests are positive with a sensitivity and specificity of 91% and 78%, respectively, and a consequent likelihood ratio of 4.1.90–95 Specificity improves with the absence of centralization of pain. The tests used are:
It is unknown if these tests can predict ligamentous sources of SIJ pain; clinical examination has not been assessed using ligament injection as the criterion standard. These tests individually can be positive in up to 20% of the asymptomatic population.96
The SI joint is more likely to be the source of pain if the following occur:
Tests for SIJ instability have been proved reliable particularly in the postpartum population, but there is no data supporting their efficacy in the management of SIJ pain, except in the postpartum population.51,52,73,97–99
Multiple authors raise the concept of SIJ dysfunction, where the self-locking mechanism of the SIJ complex fails due to a loss of form and/or force closure.20–22,47–56,61–64,66,69–73,97–101 The tests used to assess SIJ dysfunction are reliable and valid.49–52 The presence of SIJ dysfunction is proposed by these authors as a putative cause of SIJ pain. However, although outcome studies on treating this SIJ dysfunction show significant improvements in disability, changes in pain are less impressive.61,64,100,102
Imaging
The diagnosis of SIJ origin pain is difficult because there are no valid or reliable correlations between imaging changes and SIJ pain. Imaging cannot be used as a criterion standard for diagnosis or as a basis on which to assess the validity of treatment. In one study, diagnostic CT-guided intrasynovial SIJ injections had a sensitivity of 57.5 %, a specificity of 69%, and a consequent poor likelihood ratio of 1.9,75 thus negating the use of CT in a presentation of putative SIJ origin pain except to rule out red-flag conditions. Bone scan has a very low sensitivity but a high specificity for SIJ pain diagnosed with diagnostic blocks, and is not worth performing.103 Similarly, plain radiography and MRI cannot reliably detect non–red-flag SIJ origin pain.28
Changes are often noted on imaging but they are not clinically significant. For example, the CT appearance of the SIJ is closely related to patient’s age, gender, BMI, and in women, parity.104 The widths of the SIJ space and of the subchondral sclerosis on the iliac and sacral sides narrow over time; they were measured to be 2.3±0.4mm, 2.5±1.6mm and 1.4±0.5 mm, respectively, in patients younger than 40 years of age and 1.9±0.2 mm, 3.6±2.1 mm and 2.3±1.1 mm, respectively, in patients older than 40 years of age.104 SIJ changes include increased joint space narrowing and loss of joint space uniformity. Subchondral sclerosis appears to be wider and less uniform in the elderly.104 Osteophytes are present even in younger patients and their prevalence increases with advancing age.104 CT has identified six anatomic variants termed accessory joints (19.1% of assessed SIJs), iliosacral complex (5.8%), bipartite iliac bony plate (4.1%), crescent-like iliac bony plate (3.7%), semicircular defects at the sacral or iliac side (3%), and ossification centers (0.6%).105
Diagnostic Injections
Properly conducted SIJ injection is considered the criterion standard diagnostic technique.27 Intricacies and subtleties in this diagnostic approach to SIJ pain need to be understood. Diagnostic injections can be performed using various forms of imaging guidance such as C-arm fluoroscopy, ultrasound, and CT. More recently, image fusion, in which a software technology matching real-time ultrasonography and a previously obtained CT, has been tested and found to be accurate, but it is slow, taking on average about 20 minutes.106 MR-guided sacroiliac and other spinal injections can also be performed in open high-field MRI using fast TSE sequence designs.107 However, although there was a reported accuracy of drug delivery of 100% for nerve root injections, the accuracy for ZJ and SIJ delivery was only 87%, and the average time taken was 29 minutes (range 19 to 67 minutes).107
Site of Injection
There are two components to the SIJ and it appears that SIJ pain can be established as the likely source of pain only if both components are assessed. The need to assess both components, however, should be predicated on the treatment that might ensue from such a diagnostic approach. As discussed earlier, the ligamentous component of the joint is innervated by at least the dorsal ramus of L5, and certainly by the lateral branches of the dorsal rami that emerge from the S1, S2, and S3 foramina. If the treatment is to be RFN of these nerves, then it stands to reason that the diagnostic injection should be directed at these nerves. As the synovial SIJ is innervated ventrally, nerve blocks cannot be used as a diagnostic test for synovial SIJ pain; lateral branch blocks do not anesthetize the synovial SIJ.58 The only method that can be used to diagnose synovial SIJ pain is intraarticular injection. This might be used as a test if steroid or other material is to be injected into the synovial component, or if a surgical procedure such as SIJ is considered relevant.
Because the sacral lateral branches run at a variable depth and have a variable course over the sacrum, multisite, multidepth, sacral lateral branch blocks are recommended; this method renders the interosseous and dorsal sacral ligaments insensate in 70% of subjects.58,60 Another option to lateral branch blocks is to inject into the ligamentous component of the SIJ itself using contrast to exclude extraneous injection.
Number of Injections
Are controlled blocks required? In high prevalence conditions, such as in the search for ZJ pain in a population of post-whiplash neck pain patients, it has been established that double blocks are required; one with a short-acting anesthetic and another with a longer acting anesthetic.108,109 As the prevalence of an index cohort decreases within a tested population, the chances of false-positive findings with single blocks rises substantially. In such circumstances, triple blocks may be necessary, with the addition of a placebo arm. The use of a control block is recommended by Hansen and colleagues because their review of two studies with 54110 and 120111 patients found a false-positive rate for the technique of between 20% and 22% for a single block.34 Conversely, Mitchell and coworkers assessed 1146 consecutive double-block technique combined intraarticular and ligamentous injections over a 2.5-year period and found that the first block predicted the control block result in 85% of cases for a positive block and in 87% for a negative block.112
Use of Contrast
Contrast is required in all instances because it confirms that the injectate is in the joint or ligament or adjacent to the nerve, and it excludes intravascular injection or extravasation into surrounding tissues. Ventral extravasation has been reported in as many as 61% of all SIJ injections;3 if so, false-positive blocks occur because of the proximity of sheaths of the adjacent nerve trunks or roots, including the lumbosacral trunk and the L5 and S1 nerve roots.89 Thus, when local anesthetic is injected into the SIJ, a possible short-term complication is leg weakness for the duration of the local anesthetic action. Any injection into the SIJ without contrast, even under CT, should be viewed with skepticism, at least in respect to its diagnostic utility.
Volume
In intraarticular SIJ injection, the accepted maximum volume is 2.5 mL,58 but less should be injected if there is increased pain or pressure. Ligamentous injection volume is about 2 mL. The multi-site, multidepth injections onto the lateral branches of the dorsal rami from S1 to S3 require 0.2 mL per infiltration.58
Treatment
Efficacy
Corticosteroid Injection
Sacroiliac corticosteroid injections have not been tested with randomized controlled trials (RCTs). Accordingly, a systematic review concluded that the evidence supporting therapeutic injection is limited.34 However, many case series studies report that intrasynovial SIJ corticosteroid injections provide good to excellent pain relief with a duration of up to 10 months.37
A retrospective practice audit of 155 patients who underwent diagnostic and therapeutic fluoroscopically guided contrast confirmed SIJ injections with local anesthetic and corticosteroid were considered positive if they produced 50% or greater pain relief during the local anesthetic block phase and if there was subsequent pain relief for 2 weeks or more. Of the 155 patients, 69 (45%) had previous lumbar surgery and 120 (77%) were positive responders over a mean duration follow-up period of 44 months (range 26 to 101 months).113 The positive responders received a mean of 2.7 injections per patient. Forty patients required one injection only, 29 required two, 22 required three, and 27 required four or more. The mean duration of response for those receiving more than one injection was 9.3 months per injection (range 1 to 58 months). There were no adverse events.
In practice, corticosteroid and other injections can be inserted into either or both the synovial or ligamentous component of the SIJ. Intrasynovial etanercept is now injected in the treatment of ankylosing spondylitis: a case series reported that it improved both clinical features and morphologic parameters significantly, and that it was safe and cost effective.114
Radiofrequency Neurotomy
Sacroiliac treatment using cooled RFN has been assessed positively with an RCT.115,116 In this trial, 28 patients were equally divided into treatment with cooled RFN and sham treatment groups. Patients in the treatment group received denervation of the L4 medial branch, the L5 dorsal ramus, and at the S1-3 lateral branches. The proportion of participants experiencing greater than 50% pain relief at 1, 3, and 6 months postoperatively in the treatment cohort was 79%, 64%, and 57%, respectively; in the placebo group, the proportion of participants experiencing greater than 50% pain relief at 1 and 3 months postoperatively was 14% and 0%, respectively. Subsequently, 11 patients crossed over to RFN treatment, and of these, at 1, 3, and 6 months the proportion of patients reporting improvement was 64%, 55%, and 36%, respectively. The treatment effect was seen to diminish by 12 months; at that time only 14% (two patients) of the treatment group had persistent pain relief. It was suggested that larger studies were needed to further assess the efficacy of SIJ RFN.
The same group reported on 77 patients who underwent lateral branch SIJ RFN treatment using a 50% reduction in pain at 6 months as a successful outcome. Of these, 40 (52%) obtained a positive outcome. The multivariate analysis found that predictors of an unsuccessful outcome were older than 65 years and experienced pain radiating below the knee. They also noted that cooled, rather than conventional RFN, was associated with a higher percentage of positive outcomes and that no single clinical variable reliably predicted treatment results.117
Previous case series had indicated that SIJ RFN may have a role to play in the treatment of SIJ pain. The first main paper describing SIJ RFN used a stereotactic technique. After displaying the anatomy of the lateral branches of the sacral dorsal rami, Yin and associates reported in a retrospective audit that 64% of 14 patients treated with SIJ RFN reported successful outcomes for at least 6 months, with 36% achieving total relief.31 Kapural and coworkers performed a retrospective chart review on their initial cases using the cooled RFN technique; short term efficacy was apparent as 18 out of 26 cases had good outcomes at 3 months.118 They also performed a safety audit on the first 100 cases. There were no significant complications other than short-term (less than 6 weeks) pain exacerbation in four cases, and in two cases an area of cutaneous numbness over the buttocks was experienced.118
Mitchell and colleagues performed a prospective consecutive case series on 82 cases using a traditional RFN method directed at the L4 medial branch, the L5 dorsal ramus, and the S1-3 lateral branches.11 The cases were divided equally into 5- to 7-month and 8- to 13-month follow-up. Greater than 50% pain relief was achieved in 22% of patients in the 5- to 7-month group and 42% of patients in the 8- to 13-month group. Patient satisfaction was 58% versus 63% in the respective groups. At 8 months, the average reduction in VAS was 33%, with the 42% of patients with greater than 50% relief reporting an average reduction of 74% in VAS.112
Outcomes from treating the SIJ complex with traditional RF needles are dependent to some degree on the cause of the original injury; patients able to identify the cause of their injury (whether it be from a motor vehicle accident, fall, overload/work injury, etc.) are more likely to report excellent pain relief following RFN than those unable to pinpoint the mode of injury.82
Although sacral RFN is a safe procedure, there has been a case report of a permanent L5 sensory radiculopathy following a bilateral L3 to L5 RFN.119 However, such a complication should only arise from inaccurate positioning of the needle.
Prolotherapy
Prolotherapy for LBP including SIJ region pain and tenderness appears to be no better than placebo. In a RCT, Yelland and colleagues tested patients with LBP that might have included putative SIJ pain with injection onto any local tender structure—either with a combination of 20% glucose and 0.2% lidocaine or with saline.120 The outcome was that prolotherapy was equally effective as placebo but that both seemed to be somewhat effective (in 46% of cases there was a 50% pain reduction and in 42% of cases there was a 50% reduction) in Roland-Morris disability index.
In a descriptive prospective trial case-series study, Cusi and associates examined functional outcome measures and improvements in load transfer on clinical examination but not pain after CT-guided injections of 50% glucose on three occasions 6 weeks apart.100 Functional improvement occurred in 76% of patients at 3- and 12-month follow-up and in 32% at 24-month follow-up.
Surgery
Surgery with SIJ arthrodesis (via a modified Smith-Petersen technique) for putative SIJ pain, diagnosed by pain relief with intraarticular joint injections under fluoroscopic guidance, has been studied and found in one series to be reasonably successful in terms of physical functioning, role physical, bodily pain, vitality, social functioning, role emotional, and neurogenic and pain indices.121 A case-series on 15 consecutive patients treated with percutaneous SIJ fusion using hollow modular anchorage screws filled with demineralized bone matrix after diagnosis with a single SIJ injection of local anesthetic and steroid under image intensifier control reported that at a mean follow-up of 17 months, there was a significant improvement in disability, physical function, and pain; of the 15 patients, 13 reported good-to-excellent improvement.122
However, a more sobering picture emerges from a retrospective study on 17 patients who underwent bilateral SIJ fusion with internal fixation and decortication of the SIJ after diagnosis via local anesthetic joint infiltration, temporary external fixation, or bone scan because at an average follow-up period of 39 months only three patients (18%) reported moderate or absent pain; the rest of the patients had either marked or severe pain.123
Another much less invasive technique, SIJ débridement, was retrospectively studied on 38 patients with SIJ pain diagnosed with SIJ injection; at a follow-up period of 2 years, 61% had 50% or more reduction in pain and 53% had 75% or more reduction in pain.33 Additionally, percutaneous, CT-guided stabilization from S1-2, has been reported to be a potentially acceptable treatment for recalcitrant SIJ pain.124
Methods
Sacroiliac Joint Injection
SIJ injection is perhaps the most difficult joint injection to perform because of the intricacies of SIJ morphology. It is generally easier to perform in the younger female in whom the joint space is likely to be wider. It can be difficult to perform in older people as the joint undergoes degeneration. It is not possible to inject into the joint when there it total ankylosis, but total bony ankylosis is seen only with ankylosing spondylitis.43 It can be difficult to get a synovial arthrogram in elderly men in particular because of the increasing age-related presence of complete fibrous SIJ ankylosis.42
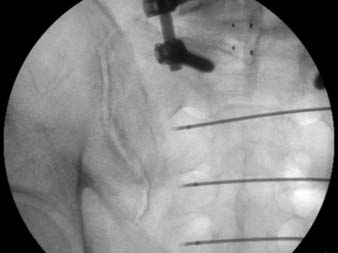
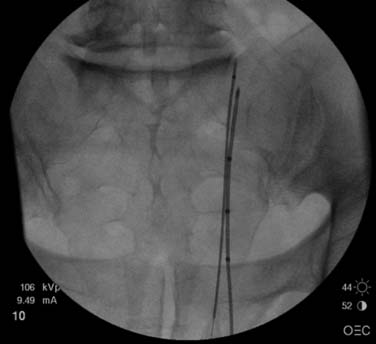
The patient lies prone on the x-ray table. Routine prepping and draping should occur and sterile technique is used throughout. The C-arm fluoroscope is centered over the inferior aspect of the appropriate SIJ. The object is to superimpose the dorsal and ventral joint lines at the inferior pole, so that a “clear” window is seen. It seems that no two joint lines are similar; thus, individual patient SIJ idiosyncrasies need to be recognized. One approach is to angle the C-arm between 10 and 20 degrees cephalic and, if the joint lines still do not overlap, to then vary the obliquity one way or the other by 5 and 10 degrees. If the joint lines still do not overlap, then repeat the same change of obliquity but with a caudad 10-to 20-degree tilt (Fig. 37-5).
When the joint lines overlap, then a “down beam” approach to the inferior aspect of the joint line is performed with a 22 gauge spinal needle. The needle can be bent a few degrees, using a no-touch technique, to allow the needle to be steered. Skin anesthesia is unnecessary. If the joint line is very sensitive on needle approximation, then 1 mL 2% lidocaine can be infiltrated at this point. However, for the purity of the block, it is preferable to not place local anesthetic outside the joint (Fig. 37-6).

Figure 37-6 Sacroiliac joint (SIJ) injection—needle approach.
The needle approaches the joint line “down beam” and is then slid superiorly into the joint.
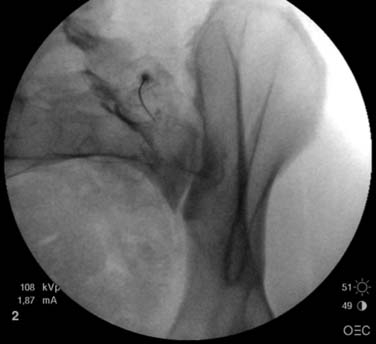
Resistance to the needle is felt as the joint capsule is entered, and often a “pop” is felt as the needle passes through the joint capsule; however, this is not a reliable sign of joint entry. When it is considered that the needle is intraarticular, the joint lines are separated radiologically by altering the obliquity back to a more PA tilt. The needle tip should still appear to be in one of the joint lines (Fig. 37-7). The C-arm is then adjusted obliquely the other way; again, the needle tip should appear to be in a joint line (Fig. 37-8).

Figure 37-8 Sacroiliac joint (SIJ) injection needle—oblique needle view (left).
The C-arm fluoroscopy is “obliqued” to the patient’s left. The needle tip is still in a joint line.
If this is not the case, contrast should NOT be injected. The needle is NOT in the joint and the approach view will be compromised if contrast is injected. If one of the oblique views does not show the needle in the joint, return to the approach view and insert the needle a further 2 mm or so. If doubt about the depth of the needle exists, use a lateral C-arm view for further assessment. Although the lateral view cannot confirm that the needle is intraarticular, it can ascertain whether or not the needle tip is a long way short of or past the joint.
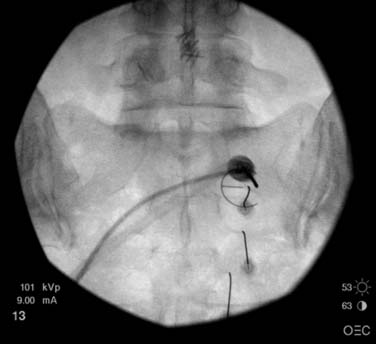
If both oblique views confirm the needle tip lies in one of the joint lines, then 0.2 mL of nonionic contrast is injected and then imaged. Contrast should flow into the joint with a minimum of resistance (Fig. 37-9). If resistance is encountered, then the needle is likely to be too ventral (too far into the joint). It can be carefully moved dorsally while maintaining pressure on the syringe; once the resistance lessens, contrast is then injected. If this dorsal movement is excessive, then the needle tip may become extraarticular; this component of needle tip positioning has to be extremely subtle. When the joint line is outlined adequately, the syringes are changed and formal joint injection is performed. It is essential to be assiduous in not moving the needle tip during the syringe exchange.
The deep interosseous ligament (DIL) can also be injected if there is a requirement to learn if this component is painful (by performing a diagnostic block) and/or to inject corticosteroid. The approach to the DIL is with the C-arm in a neutral cephalocaudad angle with contralateral oblique of 15 to 25 degrees. A “down beam” approach to touch the sacrum 1 cm medial to the DIL is used. The needle is then withdrawn 1 cm and “kicked” laterally into the DIL. The depth is level with the dorsal surface of the sacrum, up to a few mm superficial to the dorsal sacral boarder. Then 0.2 mL of nonionic contrast is injected to ensure the needle is not intravascular. The contrast should have a frothy or cloudlike appearance. If a striated pattern is seen, the needle is usually too ventral and is in the muscle ventral to the joint. If the contrast appears as a “blob” it is likely that the needle tip is too superficial. If in doubt, a lateral view may be helpful.
Radiofrequency Neurotomy
Traditional Method
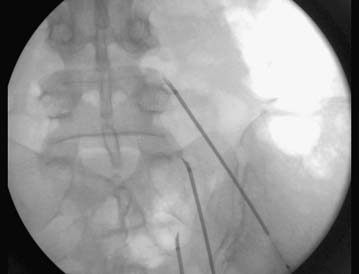
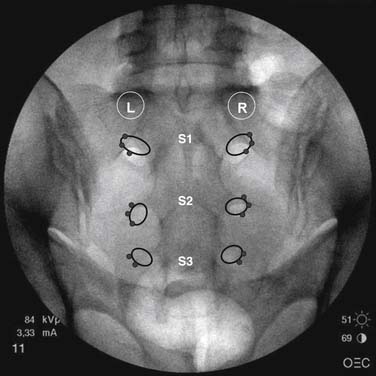
A series of lesions around the inferolateral corner to the superolateral corner of the S1-3 foramen should be performed. Each lesion should be less than 2 needle widths from the previous one. The area to be lesioned should cover all potential courses of the lateral branches (see Fig. 37-3). A second series of lesions should be performed 5 to 10 mm off bone to capture those nerves not lying on the sacral surface. The full course of the L5 dorsal branch needs to be covered. In addition to the lesion approaching the superior edge of the sacral ala, a pull back lesion should be performed. Additionally, a wide lesion, at least 5 mm lateral to the S1 superior articular process needs to be performed to cover the course of the L5 descending branch. An injection of cortisone at the conclusion of the procedure over the areas treated may help with postoperative pain control (Figs. 37-10 to 37-13).
Cooled Radiofrequency Neurotomy
This technique involves the use of a trochar to introduce a cooled radiofrequency probe onto the lateral branches of S1, S2, and S3. A traditional RFN treatment of L5 is then performed. On the right side, the S1 and S2 lesions are performed at the 1:30, 3:00, and 5:30 clock positions; the S3 lesions at 3:00 and 5:00 o’clock positions. On the left side the lesions performed are obviously mirror imaged; the S1 and S2 lesions are performed at 10:30, 9:00, and 6:30 clock positions and the S3 lesions at the 9 and 7 o’clock positions (Fig. 37-14). The lesions are performed off the bony surface of the dorsum of the sacrum by use of a depth indicator with the position being guided by a radio-opaque “epsilon” that is positioned on the skin surface over the sacral foramen. The lesions are performed at least 1 cm from the lateral edge of each sacral foramen (Figs. 37-15 and 37-16).
Simplicity Radiofrequency Neurotomy
There is currently no published outcome data on this technique, although the face validity of the technique is enticing. The technique involves placing the simplicity probe from a caudad direction under fluoroscopic control onto the dorsal surface of the sacrum lateral to the lateral edge of the sacral foramen. The probe has five different radiofrequency generators that sequentially perform RF lesions of approximately 5 mm radius along the length of the probe. The L5 branch needs to be treated separately with a traditional technique (Figs. 37-17 and 37-18).The technique is attractive with its ease of use and the size of the lesion developed. Outcome data are awaited.
Prolotherapy
As noted above, the study of Yelland and colleagues did not support prolotherapy for LBP, but the technique was not performed on patients with proven SIJ pain and the injections were not performed using imaging.120 Cusi and coworkers reported a case series based on injection of 50% glucose with local anesthetic into the DIL under fluoroscopic guidance.100 This technique needs further evaluation. It is a painful procedure and is best performed under sedation. Routine prepping and draping are first performed. The C-arm is lined up on the affected DIL in a neutral cephalocaudad but contralateral oblique position. The posterior ilium is then almost end on and there is a direct route down to the superior SIJ. A point 1 cm below and medial to the superolateral edge of the sacrum is selected and a 22 gauge 3.5-inch spinal needle is inserted “down the beam” to touch the superolateral edge of the sacrum (Fig. 37-19). A small amount of contrast is injected to ensure the needle is not intravascular; then, 1 mL of local anesthetic is injected followed by 1.5mLs of 50% (or mix the two in the one syringe) (Fig. 37-20). Using the same skin entry point, the needle is readjusted laterally so that the tip is first at the very lateral edge of the sacrum at the same height, and then it is moved more laterally to the medial edge of the iliac bone at the same height; the same injection is repeated at both sites.
The needle is then repositioned on the sacrum 1 cm below the original position 1 cm medial to the lateral edge of the sacrum and the three injections are repeated by moving the needle tip each time more laterally so that the third injection is again on the medial wall and the procedure is repeated at this level; 1 cm medial to the lateral edge, on the lateral edge, and on the medial wall of the iliac bone (Fig. 37-21). The needle is again repositioned 1 cm lower where it now lies on or close to the SIJ line, and second injection is performed (Fig. 37-22). Contrast should be used with each reposition to ensure the needle is not placed intravascularly or intrasynovially.
The patient receives routine monitoring in recovery and is discharged after a 2 or 3 hours. The patient will need adequate postprocedural analgesic. The procedure is repeated twice at 6-week intervals.
1. Fortin J.D., Aprill C.N., Ponthieux B., et al. Sacroiliac joint: pain referral maps upon applying a new injection/arthrography technique. Part II: Clinical evaluation. Spine. 1994;19:1483-1489.
2. Fortin J.D., Kissling R.O., O’Connor B.L., et al. Sacroiliac joint innervation and pain. Am J Orthop. 1999;28:687-690.
3. Fortin J.D., Washington W.J., Falco F.J. Three pathways between the sacroiliac joint and neural structures. Am J Neuroradiol. 1999;20:1429-1434.
4. Fortin J.D., Dwyer A.P., West S., Pier J. Sacroiliac joint: pain referral maps upon applying a new injection/arthrography technique. Part I: Asymptomatic volunteers. Spine. 1994;19:1475-1482.
5. Fortin J.D., Falco F.J. The Fortin finger test: an indicator of sacroiliac pain. Am J Orthop. 1997;26:477-480.
6. Forst S.L., Wheeler M.T., Fortin J.D., Vilensky J.A. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician. 2006;9:61-67.
7. Fortin J.D., Vilensky J.A., Merkel G.J. Can the sacroiliac joint cause sciatica? Pain Physician. 2003;6:269-271.
8. Solonen K.A. The sacroiliac joint in the light of anatomical, roentgenological and clinical studies. Acta Orthop Scand. 1957;27(suppl):1-127.
9. Ikeda R. Innervation of the sacroiliac joint. Macroscopical and histological studies. Nippon Ika Daigaku Zasshi. 1991;58:587-596.
10. Vilensky J.A., O’Connor B.L., Fortin J.D., et al. Histologic analysis of neural elements in the human sacroiliac joint. Spine. 2002;27:1202-1207.
11. McGrath M.C., Zhang M. Lateral branches of dorsal sacral nerve plexus and the long posterior sacroiliac ligament. Surg Radiol Anat. 2005;27:327-330.
12. Szadek K.M., Hoogland P.V., Zuurmond W.W., et al. Possible nociceptive structures in the sacroiliac joint cartilage: An immunohistochemical study. Clin Anat. 2010;23:192-198.
13. Szadek K.M., Hoogland P.V., Zuurmond W.W., et al. Nociceptive nerve fibers in the sacroiliac joint in humans. Reg Anesth Pain Med. 2008;33:36-43.
14. Slipman C.W., Jackson H.B., Lipetz J.S., et al. Sacroiliac joint pain referral zones. Arch Phys Med Rehabil. 2000;81:334-338.
15. Slipman C.W., Whyte W.S., Chow D.W., et al. Sacroiliac joint syndrome. Pain Physician. 2001;4:143-152.
16. Weksler N., Velan G.J., Semionov M., et al. the role of sacroiliac joint dysfunction in the genesis of low back pain: the obvious is not always right. Arch Orthop Trauma Surg. 2007;127:885-888.
17. Buijs E., Visser L., Groen G. Sciatica and the sacroiliac joint: a forgotten concept. Br J Anaesth. 2007;99:713-716.
18. Katz V., Schofferman J., Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech. 2003;16:96-99.
19. Reynolds H.M. Three-dimensional kinematics in the pelvic girdle. J Am Osteopath Assoc. 1980;80:277-280.
20. Vleeming A., Buyruk H.M., Stoeckart R., et al. An integrated therapy for peripartum pelvic instability: a study of the biomechanical effects of pelvic belts. Am J Obstet Gynecol. 1992;166:1243-1247.
21. Vleeming A., Stoeckart R., Volkers A.C., Snijders C.J. Relation between form and function in the sacroiliac joint. Part I: Clinical anatomical aspects. Spine. 1990;15:130-132.
22. Vleeming A., Pool-Goudzwaard A.L., Hammudoghlu D., et al. The function of the long dorsal sacroiliac ligament: its implication for understanding low back pain. Spine. 1996;21:556-562.
23. Pool-Goudzwaard A.L., Kleinrensink G.J., Snijders C.J., et al. The sacroiliac part of the iliolumbar ligament. J Anat. 2001;199:457-463.
24. Sturesson B., Selvik G., Uden A. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine. 1989;14:162-165.
25. Egund N., Olsson T.H., Schmid H., Selvik G., et al. Movements in the sacroiliac joints demonstrated with roentgen stereophotogrammetry. Acta Radiol Diagn. 1978;19:833-846.
26. Ozaki T., Rodl R., Gosheger G., et al. Sacral infiltration in pelvic sarcomas: joint infiltration analysis II. Clin Orthop Relat Res. 2003:152-158.
27. Rathmell J.P. The promise of an effective treatment for sacroiliac-related low back pain. Anesthesiology. 2008;109:167-168.
28. Dreyfuss P., Dreyer S.J., Cole A., et al. Sacroiliac joint pain. J Am Acad Orthop Surg. 2004;12:255-265.
29. Schwarzer A.C., Aprill C.N., Derby R., et al. The relative contributions of the disc and zygapophyseal joint in chronic low back pain. Spine. 1994;19:801-806.
30. Schwarzer A.C., Aprill C.N., Bogduk N. The sacroiliac joint in chronic low back pain. Spine. 1995;20:31-37.
31. Yin W., Willard F., Carreiro J., et al. Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine. 2003;28:2419-2425.
32. Stone J.A., Bartynski W.S. Treatment of facet and sacroiliac joint arthropathy: steroid injections and radiofrequency ablation. Tech Vasc Interv Radiol. 2009;12:22-32.
33. Haufe S.M., Mork A.R. Sacroiliac joint débridement: A novel technique for the treatment of sacroiliac joint pain. Photomed Laser Surg. 2005;23:596-598.
34. Hansen H.C., McKenzie-Brown A.M., Cohen S.P., et al. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007;10:165-184.
35. Braun J., Bollow M., Seyrekbasan F., et al. Computed tomography guided corticosteroid injection of the sacroiliac joint in patients with spondyloarthropathy with sacroiliitis: clinical outcome and followup by dynamic magnetic resonance imaging. J Rheumatol. 1996;23:659-664.
36. Puhakka K.B., Melsen F., Jurik A.G., et al. MR imaging of the normal sacroiliac joint with correlation to histology. Skeletal Radiol. 2004;33:15-28.
37. Cohen S.P. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101:1440-1453.
38. Steinke H., Hammer N., Slowik V., et al. Novel insights into the sacroiliac joint ligaments. Spine. 2010;35:257-263.
39. Bowen V., Cassidy J.D. Macroscopic and microscopic anatomy of the sacroiliac joint from embryonic life until the eighth decade. Spine. 1981;6:620-628.
40. Rosatelli A.L., Agur A.M., Chhaya S. Anatomy of the interosseous region of the sacroiliac joint. J Orthop Sports Phys Ther. 2006;36:200-208.
41. Stewart T.D. Pathologic changes in aging sacroiliac joints. A study of dissecting-room skeletons. Clin Orthop Relat Res. 1984:188-196.
42. Ikeno H., Matsumura H., Murakami G., et al. Which morphology of dry bone articular surfaces suggests so-called fibrous ankylosis in the elderly human sacroiliac joint? Anat Sci Int. 2006;81:39-46.
43. Resnick D., Niwayama G., Goergen T.G. Degenerative disease of the sacroiliac joint. Invest Radiol. 1975;10:608-621.
44. Brooke R. The Sacro-Iliac Joint. J Anat. 1924;58:299-305.
45. Sashin D. A critical analysis of the anatomy and the pathological changes of the sacroiliac joints. JBJS. 1930;12:891-910.
46. Taggart A.J., Desai S.M., Iveson J.M., Verow P.W. Computerized tomography of the sacro-iliac joints in the diagnosis of sacro-iliitis. Br J Rheumatol. 1984;23:258-266.
47. Vleeming A., de Vries H.J., Mens J.M., van Wingerden J.P. Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta Obstet Gynecol Scand. 2002;81:430-436.
48. Vleeming A., Volkers A.C., Snijders C.J., Stoeckart R. Relation between form and function in the sacroiliac joint. Part II: Biomechanical aspects. Spine. 1990;15:133-136.
49. Buyruk H.M., Snijders C.J., Vleeming A., et al. The measurements of sacroiliac joint stiffness with colour Doppler imaging: a study on healthy subjects. Eur J Radiol. 1995;21:117-121.
50. Mens J.M., Vleeming A., Snijders C.J., et al. The active straight leg raising test and mobility of the pelvic joints. Eur Spine J. 1999;8:468-473.
51. Mens J.M., Vleeming A., Snijders C.J., et al. Reliability and validity of the active straight leg raise test in posterior pelvic pain since pregnancy. Spine. 2001;26:1167-1171.
52. Mens J.M., Vleeming A., Snijders C.J., et al. Validity of the active straight leg raise test for measuring disease severity in patients with posterior pelvic pain after pregnancy. Spine. 2002;27:196-200.
53. Mooney V., Pozos R., Vleeming A., et al. Exercise treatment for sacroiliac pain. Orthopedics. 2001;24:29-32.
54. Sturesson B., Uden A., Vleeming A. A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test. Spine. 2000;25:364-368.
55. van Wingerden J.P., Vleeming A., Buyruk H.M., Raissadat K. Stabilization of the sacroiliac joint in vivo: verification of muscular contribution to force closure of the pelvis. Eur Spine J. 2004;13:199-205.
56. van Wingerden J.P., Vleeming A., Ronchetti I. Differences in standing and forward bending in women with chronic low back or pelvic girdle pain: indications for physical compensation strategies. Spine. 2008;33:E334-E341.
57. Grob K.R., Neuhuber W.L., Kissling R.O. Innervation of the sacroiliac joint of the human. Z Rheumatol. 1995;54:117-122.
58. Dreyfuss P., Henning T., Malladi N., et al. The ability of multi-site, multi-depth sacral lateral branch blocks to anesthetize the sacroiliac joint complex. Pain Med. 2009;10:679-688.
59. Willard FH, Carreiro JE, Manko W: The long posterior interosseous ligament and the sacrcoccygeal plexus. Third Interdisciplinary World Congress on Low Back and Pelvic Pain. Proceedings of the Third Interdisciplinary World Congress on Low Back and Pelvic Pain, 207–209.
60. Dreyfuss P., Snyder B.D., Park K., et al. The ability of single site, single depth sacral lateral branch blocks to anesthetize the sacroiliac joint complex. Pain Med. 2008;9:844-850.
61. Hides J.A., Jull G.A., Richardson C.A. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine. 2001;26:E243-E248.
62. Hides J.A., Richardson C.A., Jull G.A. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine. 1996;21:2763-2769.
63. Richardson C.A., Snijders C.J., Hides J.A., et al. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine. 2002;27:399-405.
64. Hodges P., Jull G. Does strengthening the abdominal muscles prevent low back pain? J Rheumatol. 2000;27:2286-2288.
65. Jull G.A., Richardson C.A. Motor control problems in patients with spinal pain: a new direction for therapeutic exercise. J Manipulative Physiol Ther. 2000;23:115-117.
66. Sapsford R.R., Hodges P.W., Richardson C.A., et al. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20:31-42.
67. Sterling M., Jull G., Wright A. The effect of musculoskeletal pain on motor activity and control. J Pain. 2001;2:135-145.
68. Cattley P., Winyard J., Trevaskis J., Eaton S. Validity and reliability of clinical tests for the sacroiliac joint. A review of literature. Australas Chiropr Osteopathy. 2002;10:73-80.
69. Damen L., Buyruk H.M., Guler-Uysal F., et al. The prognostic value of asymmetric laxity of the sacroiliac joints in pregnancy-related pelvic pain. Spine. 2002;27:2820-2824.
70. Damen L., Spoor C.W., Snijders C.J., et al. Does a pelvic belt influence sacroiliac joint laxity? Clin Biomech. 2002;17:495-498.
71. Damen L., Stijnen T., Roebroeck M.E., et al. Reliability of sacroiliac joint laxity measurement with Doppler imaging of vibrations. Ultrasound Med Biol. 2002;28:407-414.
72. Damen L., Buyruk H.M., Guler-Uysal F., et al. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet Gynecol Scand. 2001;80:1019-1024.
73. Mens J.M., Damen L., Snijders C.J., et al. The mechanical effect of a pelvic belt in patients with pregnancy-related pelvic pain. Clin Biomech. 2006;21:122-127.
74. Coventry M.B., Tapper E.M. Pelvic instability: a consequence of removing iliac bone for grafting. J Bone Joint Surg Am. 1972;54:83-101.
75. Elgafy H., Semaan H.B., Ebraheim N.A., Coombs R.J. Computed tomography findings in patients with sacroiliac pain. Clin Orthop Relat Res. 2001:112-118.
76. Summers B.N., Eisenstein S.M. Donor site pain from the ilium. A complication of lumbar spine fusion. J Bone Joint Surg Br. 1989;71:677-680.
77. Ebraheim N.A., Elgafy H., Semaan H.B. Computed tomographic findings in patients with persistent sacroiliac pain after posterior iliac graft harvesting. Spine. 2000;25:2047-2051.
78. Maigne J.Y., Planchon C.A. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J. 2005;14:654-658.
79. Ivanov A.A., Kiapour A., Ebraheim N.A., Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine. 2009;34:E162-E169.
80. Ha K.Y., Lee J.S., Kim K.W. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine. 2008;33:1192-1198.
81. Tuite M.J. Sacroiliac joint imaging. Semin Musculoskelet Radiol. 2008;12:72-82.
82. Mitchell B., McPhail T., Verrills P., et al. Chronic pelvic and sacroiliac joint pain: Diagnosis, radiofrequency neurotomy and neuromodulation. APS/NZPS Combined Conference. 2010.
83. Szadek K.M., van der W.P., van Tulder M.W., et al. Diagnostic validity of criteria for sacroiliac joint pain: a systematic review. J Pain. 2009;10:354-368.
84. Feinstein B., Langton J.N., Jameson R.M., Schiller F., et al. Experiments on pain referred from deep somatic tissues. J Bone Joint Surg Am. 1954;36-A:981-997.
85. Govind J. Lumbar radicular pain. Aust Fam Physician. 2004;33:409-412.
86. Irwin R.W., Harris M.B. Concomitant sacroiliac joint pain in patients with lumbar disc herniation: case series. J Surg Orthop Adv. 2004;13:224-227.
87. Kutsy R.L., Robinson L.R., Routt M.L.Jr. Lumbosacral plexopathy in pelvic trauma. Muscle Nerve. 2000;23:1757-1760.
88. Dreyfuss P., Michaelsen M., Pauza K., et al. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine. 1996;21:2594-2602.
89. Berthelot J.M., Labat J.J., Le Goff .B., et al. Provocative sacroiliac joint maneuvers and sacroiliac joint block are unreliable for diagnosing sacroiliac joint pain. Joint Bone Spine. 2006;73:17-23.
90. Laslett M., Williams M. The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine. 1994;19:1243-1249.
91. Laslett M. The value of the physical examination in diagnosis of painful sacroiliac joint pathologies. Spine. 1998;23:962-964.
92. Laslett M. Pain provocation tests for diagnosis of sacroiliac joint pain. Aust J Physiother. 2006;52:229.
93. Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16:142-152.
94. Laslett M., Aprill C.N., McDonald B., Young S.B., et al. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10:207-218.
95. Laslett M., Aprill C.N., McDonald B. Provocation sacroiliac joint tests have validity in the diagnosis of sacroiliac joint pain. Arch Phys Med Rehabil. 2006;87:874-875.
96. Dreyfuss P., Dryer S., Griffin J., et al. Positive sacroiliac screening tests in asymptomatic adults. Spine. 1994;19:1138-1143.
97. Hungerford B., Gilleard W., Hodges P. Evidence of altered lumbopelvic muscle recruitment in the presence of sacroiliac joint pain. Spine. 2003;28:1593-1600.
98. Hungerford B., Gilleard W., Lee D. Altered patterns of pelvic bone motion determined in subjects with posterior pelvic pain using skin markers. Clin Biomech. 2004;19:456-464.
99. Hungerford B.A., Gilleard W., Moran M., et al. Evaluation of the ability of physical therapists to palpate intrapelvic motion with the Stork test on the support side. PhysTher. 2007;87:879-887.
100. Cusi M., Saunders J., Hungerford B., et al. The use of prolotherapy in the sacroiliac joint. Br J Sports Med. 2010;44:100-104.
101. Buyruk H.M., Stam H.J., Snijders C.J., et al. The use of color Doppler imaging for the assessment of sacroiliac joint stiffness: a study on embalmed human pelvises. Eur J Radiol. 1995;21:112-116.
102. Weil Y.A., Hierholzer C., Sama D., et al. Management of persistent postpartum pelvic pain. Am J Orthop. 2008;37:621-626.
103. Prassopoulos P.K., Faflia C.P., Voloudaki A.E., Gourtsoyiannis N.C., et al. Sacroiliac joints: anatomical variants on CT. J Comput Assist Tomogr. 1999;23:323-327.
104. Slipman C.W., Sterenfeld E.B., Chou L.H., et al. The value of radionuclide imaging in the diagnosis of sacroiliac joint syndrome. Spine. 1996;21:2251-2254.
105. Faflia C.P., Prassopoulos P.K., Daskalogiannaki M.E., Gourtsoyiannis N.C., et al. Variation in the appearance of the normal sacroiliac joint on pelvic CT. Clin Radiol. 1998;53:742-746.
106. Klauser A.S., De Zordo .T., Feuchtner G.M., et al. Fusion of real-time US with CT images to guide sacroiliac joint injection in vitro and in vivo. Radiology. 2010;256(2):547-553.
107. Streitparth F., Walter T., Wonneberger U., et al. Image-guided spinal injection procedures in open high-field MRI with vertical field orientation: feasibility and technical features. Eur Radiol. 2010;20:395-403.
108. Lord S.M., Barnsley L., Bogduk N. The utility of comparative local anesthetic blocks versus placebo-controlled blocks for the diagnosis of cervical zygapophysial joint pain. Clin J Pain. 1995;11:208-213.
109. Schwarzer A.C., Aprill C.N., Derby R., et al. The false-positive rate of uncontrolled diagnostic blocks of the lumbar zygapophysial joints. Pain. 1994;58:195-200.
110. Maigne J.Y., Aivaliklis A., Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine. 1996;21:1889-1892.
111. Manchikanti L., Singh V., Pampati V., et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308-316.
112. Mitchell B., McPhail T., Verrills P., et al. Radiofrequency neurotomy for sacroiliac joint pain: A prospective study. J Science Med Sport. 2010;12(Supp 2):e6-e7.
113. Hawkins J., Schofferman J. Serial therapeutic sacroiliac joint injections: a practice audit. Pain Med. 2009;10:850-853.
114. Cui Y., Xiao Z., Shuxia W., et al. Computed tomography guided intra-articular injection of etanercept in the sacroiliac joint is an effective mode of treatment of ankylosing spondylitis. Scand J Rheumatol. 2010;39:229-322.
115. Cohen S.P., Hurley R.W., Buckenmaier iii C.C., et al. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109:279-288.
116. Cohen SP, Raja SN: A placebo-controlled study assessing lateral branch radiofrequency denervation for sacroiliac (SI) joint pain. 2008. Unpublished Work
117. Cohen S.P., Strassels S.A., Kurihara C., et al. Outcome predictors for sacroiliac joint (lateral branch) radiofrequency denervation. Reg Anesth Pain Med. 2009;34:206-214.
118. Kapural L., Stojanovic M., Bensitel T., et al. Cooled radiofrequency (RF) of L5 dorsal ramus for RF denervation of the sacroiliac joint: technical report. Pain Med. 2010;11:53-57.
119. Abbott Z., Smuck M., Haig A., Sagher O., et al. Irreversible spinal nerve injury from dorsal ramus radiofrequency neurotomy: a case report. Arch Phys Med Rehabil. 2007;88:1350-1352.
120. Yelland M.J., Glasziou P.P., Bogduk N., et al. Prolotherapy injections, saline injections, and exercises for chronic low-back pain: a randomized trial. Spine. 2004;29:9-16.
121. Buchowski J.M., Kebaish K.M., Sinkov V., et al. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J. 2005;5:520-529.
122. Khurana A., Guha A.R., Mohanty K., Ahuja S., et al. Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br. 2009;91:627-631.
123. Schutz U., Grob D. Poor outcome following bilateral sacroiliac joint fusion for degenerative sacroiliac joint syndrome. Acta Orthop Belg. 2006;72:296-308.
124. Ziran B.H., Heckman D., Smith W.R. CT-guided stabilization for chronic sacroiliac pain: a preliminary report. J Trauma. 2007;63:90-96.
125. Verrills P., Mitchell B., Vivian D., Sinclair C., et al. Peripheral nerve stimulation: A treatment in chronic low back pain and failed back surgery syndrome? Neuromodulation. 2009;12:68-75.
126. Tekin I., Mirzai H., Ok G., et al. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain. 2007;23:524-529.