Rosacea
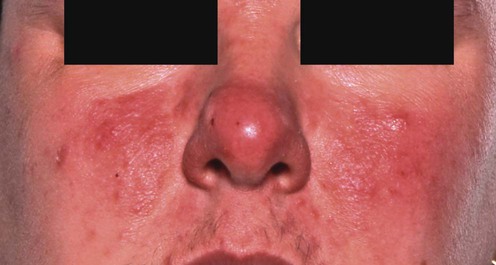
Inflammatory rosacea
First-line treatments
Second-line treatments
Third-line treatments
Erythematotelangiectatic rosacea
First-line therapies
Rosacea flushing
First-line therapies
Rosacea lymphedema (morbihan’s disease)
Ocular rosacea
First-line therapies



 Topical metronidazole
Topical metronidazole Topical azelaic acid
Topical azelaic acid Oral tetracyclines
Oral tetracyclines Oral erythromycin
Oral erythromycin Emollients
Emollients Topical erythromycin
Topical erythromycin Topical clindamycin
Topical clindamycin Oral metronidazole
Oral metronidazole Topical benzoyl peroxide
Topical benzoyl peroxide Ampicillin
Ampicillin Azithromycin
Azithromycin Systemic isotretinoin
Systemic isotretinoin Topical tretinoin
Topical tretinoin Topical adapalene
Topical adapalene Topical sulfur
Topical sulfur Topical corticosteroids
Topical corticosteroids Topical ketoconazole
Topical ketoconazole Systemic ketoconazole
Systemic ketoconazole Topical bifonazole
Topical bifonazole Photodynamic therapy
Photodynamic therapy Spironolactone
Spironolactone Demodex eradication
Demodex eradication Helicobacter pylori eradication
Helicobacter pylori eradication Sunscreens
Sunscreens Topical tacrolimus
Topical tacrolimus Topical pimecrolimus
Topical pimecrolimus Octreotide
Octreotide Inhibition of ovulation
Inhibition of ovulation Topical NADH
Topical NADH Topical 1-methylnicotinamide
Topical 1-methylnicotinamide Oral nicotinamide with zinc
Oral nicotinamide with zinc Zinc sulphate
Zinc sulphate Trichloroacetic acid peels
Trichloroacetic acid peels Brimonidine tartrate
Brimonidine tartrate Oxymetazoline
Oxymetazoline Cosmetic camouflage
Cosmetic camouflage Intense pulsed light
Intense pulsed light Vascular lasers
Vascular lasers Ondansetron
Ondansetron Clonidine
Clonidine Rilmenidine
Rilmenidine β-Blockers
β-Blockers Naloxone
Naloxone Cosmesis
Cosmesis Pulsed dye laser
Pulsed dye laser Intense pulsed light
Intense pulsed light Hypnosis
Hypnosis Granisetron
Granisetron Broad-spectrum antibiotics
Broad-spectrum antibiotics Facial massage
Facial massage Isotretinoin with ketotifen and H1 antagonist
Isotretinoin with ketotifen and H1 antagonist Prednisolone with metronidazole
Prednisolone with metronidazole CO2 laser blepharoplasty
CO2 laser blepharoplasty Surgical debulking of the eyelids
Surgical debulking of the eyelids Prednisolone and doxycycline
Prednisolone and doxycycline Tear substitutes, e.g., carbomers, liquid paraffin, hypromellose
Tear substitutes, e.g., carbomers, liquid paraffin, hypromellose Oral tetracyclines
Oral tetracyclines Topical cyclosporine
Topical cyclosporine Fusidic acid (topical)
Fusidic acid (topical) Helicobacter pylori eradication
Helicobacter pylori eradication Ondansetron
Ondansetron Systemic corticosteroids
Systemic corticosteroids Topical corticosteroids
Topical corticosteroids Isotretinoin
Isotretinoin Systemic antibiotics
Systemic antibiotics