Nasal passages and paranasal sinuses135
15.2 The larynx136
15.3 The lungs136
The respiratory system extends from the nasal orifices to the periphery of the lungs and the pleura, and includes the nasal passages, paranasal sinuses, larynx and lungs. The pathology of these structures will be discussed in this chapter. Respiratory diseases are so common that you will inevitably encounter them in whichever branch of medicine you decide to follow. Many bed-ridden patients develop some degree of bronchopneumonia. Pneumonia is also a frequent cause of hospital admission, and is often fatal in the elderly and infirm. Obstructive and restrictive (interstitial) lung diseases are common, causing significant morbidity among the general population. Last but not least, lung cancer is not only the most common malignancy in men, with increasing frequency in women, but it is also the most frequently fatal malignancy. Lung disease in general is a major cause of morbidity and mortality across the globe, and its importance in clinical practice cannot be overemphasised.
15.1. Nasal passages and paranasal sinuses
Structure and function
The nasal passages and sinuses lie in continuity and are lined by respiratory-type epithelium. The function of the nasal sinuses is to warm, humidify and clean inspired air.
Inflammatory disorders
Inflammatory diseases are the commonest disorders to affect the nasal passages and paranasal sinuses.
Rhinitis
Inflammation of the nasal passages has two main causes:
• The common cold (infective rhinitis). This is almost invariably initiated by a virus.
• Hay fever (allergic rhinitis). This is initiated by allergens, the inflammatory reaction being mediated via type I and type III hypersensitivity reactions (see Ch. 8).
Nasal polyps
These inflammatory swellings are common and result from recurrent inflammation of the nasal passages. They are often bilateral (in contrast with nasal tumours which are usually unilateral).
Sinusitis
Inflammation of the sinuses is frequently a complication of acute rhinitis. Swelling of the nasal mucosa obstructs the drainage orifices of the sinuses. This leads to stasis of the secretions within the sinuses, with consequent infection and inflammation.
Tumours
Tumours of the nasal passages and sinuses are uncommon.
Benign
The most frequent benign tumours are:
• squamous papilloma
• inverted papilloma (transitional cell papilloma)
• haemangioma
• angiofibroma.
Malignant
Malignant tumours of the nasal passages and paranasal sinuses include:
• squamous cell carcinoma
• transitional cell carcinoma
• adenocarcinoma
• plasmacytoma
• olfactory neuroblastoma.
15.2. The larynx
Structure and function
The larynx connects the trachea to the pharynx. It is a complex organ with numerous connective tissue elements. The lining epithelium varies from non-keratinising stratified squamous to respiratory-type epithelium. The function of the larynx is to allow air into the trachea and to produce sound for speaking. The epiglottis prevents food from entering the trachea.
Inflammatory disorders
Laryngitis
Inflammation of the larynx can be the result of infection, overuse of the voice, mechanical irritation or exposure to tobacco, other chemical agents, or allergens. Infective laryngitis can be caused by a number of viruses and bacteria. The laryngeal inflammation is usually mild, but if it is severe, such as in diphtheria, the resultant oedema and exudate can cause laryngeal obstruction, particularly in children.
Epiglottitis
The most commonly implicated organism in epiglottitis is the bacteria Haemophilus influenzae. Infection results in marked oedema and enlargement of the epiglottis, which can cause life-threatening airway obstruction in children.
Tumours
Benign
The commonest benign tumours are:
• laryngeal polyps (‘singers’ nodes’). These are most often found in smokers or people who overuse their larynx
• squamous papilloma.
Malignant
The most frequent malignant tumour of the larynx is squamous cell carcinoma, which typically affects males over 40. This tumour is associated with cigarette smoking, and there may be an increased risk in those exposed to asbestos. Arising most often on the vocal cords, the carcinoma invades locally and can later cause widespread distant metastases.
15.3. The lungs
You should:
• understand the structure and function of the lungs
• know the major groups of lung disorders
• know the various types of infective, obstructive, restrictive, vascular and neoplastic lung conditions
• understand the aetiology and pathogenesis of important respiratory diseases.
Structure and function of the lungs
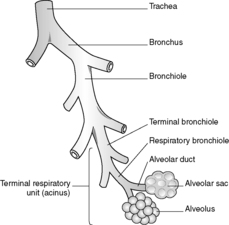
The function of the lungs is to exchange gases between the inspired air and the blood. Inspired air passes from the trachea into the main left and right bronchi. Each bronchus then branches dichotomously giving rise to progressively smaller airways, hence the term ‘respiratory tree’ (Figure 36). Progressive branching of the bronchi forms bronchioles. Bronchioles branch until they form terminal bronchioles. The part of the lung distal to each terminal bronchiole is called the acinus, or terminal respiratory unit. Branching of the terminal bronchioles gives rise to respiratory bronchioles, which in turn branch into alveolar ducts. Each alveolar duct branches and empties into blind-ended alveolar sacs, where gas exchange occurs. A group of 3–5 acini is referred to as a lobule.
The trachea, bronchi and bronchioles are lined by respiratory-type epithelium. The alveoli are lined by type I and type II pneumocytes, beneath which lies a thin connective tissue membrane. This membrane separates the alveoli from the pulmonary capillaries but allows rapid and efficient diffusion of gases.
Inflammatory disorders
Bronchitis
Acute bronchitis can be caused by infection or exposure to irritant chemical agents such as tobacco smoke, sulphur dioxide and chlorine. Infective inflammation of the bronchi is usually accompanied by inflammation of the trachea and larynx (acute laryngotracheobronchitis), which is clinically more severe in children (‘croup’). Acute infective bronchitis is most commonly initiated by viruses such as respiratory syncytial virus (RSV), although bacteria can also be a cause. Episodes of acute bronchitis are often seen in people with chronic bronchitis, causing an exacerbation of the established disease.
Bronchiolitis
There are three main types of bronchiolitis:
• Primary bronchiolitis: This is most commonly seen in infants, in whom it can cause symptoms of acute respiratory distress. The inflammation is usually caused by viruses, especially RSV. Resolution is usual, but a minority of patients develop bronchopneumonia.
• Follicular bronchiolitis: This is seen in patients with rheumatoid arthritis. Lymphoid aggregates with germinal centres compress the airways.
• Bronchiolitis obliterans: This can occur from a number of diseases and disease states, and is characterised by the obliteration of bronchiolar lumina by masses of organising inflammatory exudate.
Bacterial pneumonia
Pneumonia is defined as an inflammatory condition of the lung characterised by consolidation (solidification) of the pulmonary tissue. In infective pneumonia, the causative organism infects the lung parenchyma, causing the formation of an inflammatory exudate within the alveolar spaces with consequent consolidation.
Pathogenesis
The respiratory system uses a number of defence mechanisms to clear or destroy any inhaled microorganisms.
These include:
• nasal secretions
• the mucociliary apparatus
• alveolar clearance by macrophages
• coughing and sneezing.
Pneumonia can result whenever these defence mechanisms are impaired (see Table 21).
| Defect in defence mechanism | Causes |
|---|---|
| Loss or suppression of the cough reflex | Coma, sedation, neuromuscular disorders, drugs |
| Impairment of ciliary function | Immotile cilia syndrome (Kartagener syndrome) |
| Injury to the mucociliary apparatus | Cigarette smoking |
| Accumulation of secretions | Cystic fibrosis, bronchiectasis |
| Interference with alveolar macrophage function | Cigarette smoking, hypoxia |
| Flooding of the alveoli | Pulmonary congestion and oedema |
| Reduction in immune response | Immunosuppression |
Classification
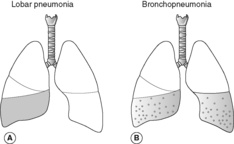
Classically, pneumonia is classified according to the main anatomical pattern of consolidation into bronchopneumonia and lobar pneumonia (Figure 37).
Bronchopneumonia Bronchopneumonia is characterised by patchy consolidation of the lung. Those individuals most at risk are elderly people, infants, and people with debilitating illnesses. Typical aetiological organisms include streptococci, staphylococci, pneumococci, H. influenzae, Pseudomonas aeruginosa and coliform bacteria. The consolidation is multilobular and frequently bilateral and basal. Histologically, a neutrophil-rich exudate fills the bronchi, bronchioles and adjacent alveolar spaces.
Lobar pneumonia Lobar pneumonia is characterised by consolidation of a large portion of a lobe or an entire lobe, and it typically affects otherwise healthy adults aged between 20 and 50years. The most common pathogenic organism is Streptococcus pneumoniae. Less common causal organisms are Klebsiella pneumoniae, staphylococci, streptococci and H. influenzae.
Atypical pneumonia
The term ‘atypical’ in the context of pneumonia is used when the inflammatory changes in the lungs are confined to the alveolar septa and interstitium, without a significant alveolar exudate. Characteristically, patients have few localising symptoms even with severe atypical pneumonia. As such, atypical pneumonia should be suspected when the chest X-ray findings are much worse than the symptoms.
Immunocompromised patients are particularly at risk.
Aetiology
In immunocompetent individuals, the causes of atypical pneumonia are:
• Viruses, e.g. influenza, RSV, adenovirus
• Bacteria, e.g. Legionella pneumophila (Legionnaire disease)
• Mycoplasma
• Coxiella burnetii (Q fever).
In immunocompromised individuals the causes of atypical pneumonia are:
• Viruses, e.g. CMV, measles, varicella
• Bacteria, e.g. Pneumocystis carinii, Chlamydia
• Fungi, e.g. Candida, Aspergillus.
Aspiration pneumonia
When food or liquid is aspirated into the lung, there is irritation of the pulmonary tissue by the acidic gastric contents and introduction of organisms from the oropharynx. Inflammation and consolidation of the affected part of the lung may ensue. At-risk clinical situations include sedation, coma, anaesthesia and acute alcoholism.
Lung abscess
A lung abscess is a local suppurative process within the lungs (often walled off), accompanied by necrosis of the lung tissue.
Aetiology and pathogenesis
Under the right conditions, almost any pathogen can cause a lung abscess. An abscess may form as a result of:
• Aspiration or bacterial pneumonia
• Entrapment of septic emboli in the lungs (e.g. embolisation of vegetations in infective endocarditis)
• Infection of a pulmonary infarct
• Airway obstruction. An abscess may form beyond the obstruction, which may be a tumour or a foreign body
• Miscellaneous situations, such as following penetrating trauma to the lung or the spread of infection from neighbouring organs.
Complications
With antibiotic therapy, many resolve and heal completely leaving a fibrous scar. A persistent abscess may require surgical treatment. Possible complications of a lung abscess include an empyema (pus in the pleural space), pyopneumothorax, haemorrhage and spread of infection to distant sites to cause, for example, brain abscesses or meningitis.
Tuberculosis
The term ‘tuberculosis’ refers to the disease caused by Mycobacterium tuberculosis (found within infected respiratory secretions and air droplets) and less commonly Mycobacterium bovis (found in the milk of diseased cows). Tuberculosis is the single most important infectious cause of death in the world. Up until the mid-1980s, Western countries had seen a decline in the number of clinical cases because of:
• improved hygiene and social conditions
• the introduction of effective antibiotics against the bacilli
• the introduction of immunisation with bacille Calmette–Guérin (BCG).
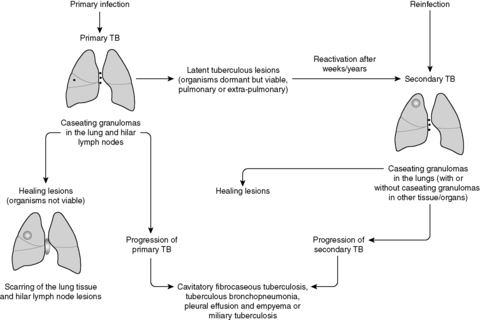
At present the incidence of tuberculosis is rising in the USA, Europe and Africa, most probably due to the increasing incidence of human immunodeficiency virus (HIV) infection. Furthermore, antibiotic-resistant strains are now being isolated. The lung is the commonest site for infection. Tuberculosis is classically divided into two phases, primary and post-primary (secondary) tuberculosis (Figure 38).
 |
| Figure 38 |
Primary tuberculosis
Inhaled M. tuberculosis passes into the lungs and initiates a non-specific inflammatory response. Alveolar macrophages phagocytose the organism and transport it to the hilar lymph nodes. These naive macrophages are unable to kill the organism, and so more macrophages are recruited. Meanwhile, the bacilli multiply, lyse the host cell and then infect more macrophages. At this point, the organisms can potentially disseminate via the bloodstream to other parts of the lung and more distant sites. In immunocompetent hosts, the mycobacteria activate the T cells, which can cause lysis of infected macrophages and stimulate macrophages to mature into epithelioid cells, which are effective killers of M. tuberculosis. Some epithelioid cells fuse to become multinucleated giant cells. Consequently, a granuloma forms consisting of epithelioid cells, giant cells and a central area of caseous necrosis corresponding to lysed infected macrophages (see Ch. 4). The bacilli are unable to survive in such acidic and oxygen-poor conditions, and so infection is controlled. A calcified scar forms in both the affected lung parenchyma (Ghon focus) and the hilar lymph nodes, which together are called the primary Ghon complex. Importantly, bacilli may still survive in these scarred foci for many years. Primary tuberculosis is asymptomatic in most cases. Rarely, particularly with infants, children or immunocompromised adults, the primary lesion may progress, resulting in cavitation, tuberculous bronchopneumonia, pleural effusion and empyema, or miliary tuberculosis (tuberculosis spreading around the body).
Miliary tuberculosis
If the tuberculous bacteraemia becomes heavy during primary or post-primary tuberculosis, miliary tuberculosis may result. Miliary tuberculosis is characterised by numerous granulomas in many organs, and may be fatal if left untreated.
Obstructive airways disease
This group of disorders is characterised by an increase in resistance to airflow, owing to partial or complete obstruction at any level of the respiratory tree. The major obstructive disorders are chronic bronchitis, emphysema, asthma and bronchiectasis. The symptom common to all these disorders is ‘dyspnoea’ (difficulty breathing), but each have their own clinical and anatomical characteristics.
Chronic bronchitis and emphysema almost always coexist, and the term chronic obstructive pulmonary disease (COPD) is often used to refer to them.
Chronic bronchitis
Aetiology
Undoubtedly, the single most important cause is cigarette smoking.
Pathogenesis
Irritants, such as tobacco smoke, cause two main abnormalities, which lead to airway obstruction.
• Increase in size (hypertrophy) of submucosal glands and a marked increase in the number (hyperplasia) of goblet cells. There is consequent hypersecretion of mucus, mainly in the large airways, which results in mucous plugging and overproduction of sputum.
• A respiratory bronchiolitis affecting the smaller airways of less than 2mm in diameter.
Infection does not seem to play a role in the initiation of chronic bronchitis, but is an important cause of exacerbations.
Emphysema
Emphysema is characterised by abnormal permanent dilatation of the air spaces distal to the terminal bronchioles, accompanied by destruction of their walls without obvious fibrosis. The clinical symptoms of emphysema do not appear until at least a third of the lung parenchyma is destroyed. Typically, patients overventilate to remain well oxygenated, and are then referred to as ‘pink puffers’.
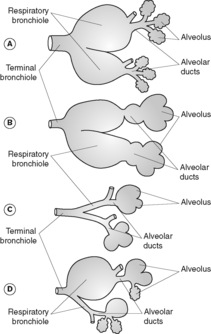
Classification
Emphysema is classified into four main types according to the anatomical distribution of the lesions and based on the appearance of the lungs with the naked eye or hand lens (Figure 39).
Centrilobular (centriacinar) emphysema In this type there is involvement of the central or proximal parts of the acinus with sparing of the distal alveoli. The lesions are closely associated with cigarette smoking and are more common in the upper lobes.
Panlobular (panacinar) emphysema In this type all airways distal to the terminal bronchioles (i.e. the entire acinus) are involved. The lower lobes are more commonly affected, particularly the bases. Panacinar emphysema is associated with α1-antitrypsin deficiency.
Paraseptal emphysema In this type the distal (peripheral) part of the acinus is involved, with sparing of the proximal part. It is usually more severe in the upper lobes. The affected airways can become very dilated, forming cyst-like structures which are termed ‘bullae’ if they reach over 10mm in diameter. These bullae may rupture, resulting in a spontaneous pneumothorax.
Irregular emphysema In this type the acinus is irregularly involved. Irregular emphysema is almost invariably associated with scarring.
Pathogenesis
Current evidence indicates that emphysema is due to an imbalance between protease and antiprotease activity in the lung. Support for this theory is based on the association between α1-antitrypsin deficiency and the development of emphysema. α1-Antitrypsin inhibits the actions of proteases, particularly elastase, which is secreted by neutrophils. α1-Antitrypsin deficiency is a genetic disorder showing an autosomal recessive pattern of inheritance. Homozygous patients have reduced levels of the enzyme and have a tendency to develop emphysema because they are unable to inhibit elastase secreted by inflammatory cells. Destruction of the airway wall ensues. The process is further compounded by smoking, mainly because smokers have more inflammatory cells in their lungs.
Irregular emphysema is thought to be due to air trapping because of fibrotic scarring. The scars are the result of a previous inflammatory process.
Pathology
In the advanced stages of the disease, the lungs may appear voluminous and bullae may be seen. Microscopically, there are abnormal fenestrations in the walls of the alveoli with complete destruction of the septal walls.
Asthma
Asthma is divided into two basic types:
• extrinsic asthma
• intrinsic asthma
Extrinsic asthma
This type of asthma is induced by exposure to an extrinsic allergen, and is mediated by a type I hypersensitivity reaction.
Atopic allergic asthma This is the most common type of asthma. It usually begins in childhood and patients may also have other atopic disorders such as hay fever or eczema. There is often a family history of asthma, hay fever or eczema. The asthma is triggered by environmental allergens such as dust, pollen, food and animal dander. Inhalation of such allergens triggers a type I, IgE-mediated hypersensitivity reaction characterised by an immediate response and a late phase reaction caused by the local release of inflammatory mediators from a variety of cell types (Figure 40). The precise pathogenesis of asthma involves interactions between many cell types and mediators, and these interactions are not fully understood. A number of chemical mediators are implicated in the asthma response. Histamine, prostaglandin D2, leukotrienes, platelet-activating factor, tumour necrosis factor (TNF), chemokines and various interleukins are among those substances thought to be important.
The following morphological changes are seen in the lungs in cases of severe asthma:
• mucous plugging of bronchi. These plugs may contain whorls of shed epithelium (Curschmann’s spirals)
• oedema and inflammation of the bronchial walls. Histologically, there is prominence of eosinophils. Eosinophil membrane protein can be seen as crystals called Charcot–Leyden crystals
• over-inflation of the lungs distal to the obstruction
• mucous gland hypertrophy
• bronchial wall smooth muscle hypertrophy
• thickening of the bronchial basement membrane.
Occupational asthma This form of asthma is triggered by agents inhaled at work, e.g. fumes, dusts, gases and other chemicals. The airway reaction is thought to be mediated by type I and type III hypersensitivity.
Allergic bronchopulmonary aspergillosis This type of asthma is induced by the inhalation of spores of the fungus Aspergillus fumigatus. The inhaled spores induce type I and type III hypersensitivity reactions.
Intrinsic asthma
Intrinsic asthma can be induced by pulmonary infection (usually viral), ingestion of aspirin, cold, exercise and stress. The mechanism leading to the bronchoconstriction seems to be non-immunological. The pathogenesis remains uncertain.
Bronchiectasis
Bronchiectasis is characterised by permanent dilatation of bronchi and bronchioles. Patients suffer from cough with the production of copious amounts of foul-smelling sputum.
Pathogenesis
Both obstruction and infection are usually necessary for development of bronchiectasis. Obstruction of the bronchial lumen results in secondary inflammation and fibrosis. The damaged bronchial walls weaken and eventually become irreversibly dilated. The obstruction can be due to a foreign body, tumour, inspissated mucus or external compression. Persistent infection results in inflammation and leads to extensive weakening and destruction of the airway walls. Either infection or obstruction may be the initiating factors in the development of bronchiectasis. Persistent infection may lead to obstruction of airways, and obstruction may lead to secondary infection.
It therefore follows that bronchiectasis may be associated with congenital or hereditary disorders such as cystic fibrosis, Kartagener syndrome or immunodeficiency states.
Complications
Complications such as empyema formation, brain abscess and amyloidosis are now rare.
Interstitial (restrictive) lung diseases
The interstitium of the lung consists of the basement membrane of the endothelial and epithelial cells, collagen fibres, elastic tissue, fibroblasts and occasional inflammatory cells. In interstitial (restrictive) lung diseases, there is diffuse infiltration of the interstitium, leading to increased amounts of tissue in the lung and causing reduced lung compliance and lung volume, and reduced oxygen diffusing capacity. The functional changes are restrictive rather than obstructive, and affected patients develop symptoms of progressive breathlessness and cough.
Many conditions belong to this group of disorders. Although each begins as a distinct entity, they all ultimately cause scarring and destruction of the lung, referred to as ‘honeycomb lung’.
Pathogenesis
Regardless of the type of interstitial lung disease, the earliest change seen in the lungs is the influx of inflammatory cells into the alveoli and alveolar walls. This distorts the normal structure of the alveoli and results in the release of chemical mediators, which injure parenchymal cells and promote fibrosis. Ultimately, with remodelling, the alveoli are replaced by cystic spaces separated by fibrous connective tissue (honeycomb lung).
Classification
| Classification according to aetiology | Classification according to speed of onset of damage | ||
|---|---|---|---|
| Known aetiology | Unknown aetiology | Acute interstitial diseases | Chronic interstitial diseases |
| Environmental agents | Idiopathic pulmonary fibrosis | ARDS | Idiopathic pulmonary fibrosis |
| Radiation | Drugs and toxins | Pneumoconiosis | |
| Hypersensitivity pneumonitis | Sarcoid | Acute radiation pneumonitis | Sarcoid |
| Following adult respiratory distress syndrome (ARDS) | Goodpasture’s syndrome Idiopathic pulmonary haemosiderosis | Diffuse pulmonary haemorrhage syndromes | Collagen vascular diseases |
| Drugs and toxins | Collagen vascular diseases | ||
Pneumoconiosis
This term is used to refer to a group of lung diseases resulting from the inhalation of dusts, fumes and vapours.
Coalworker pneumoconiosis
Coalworker pneumoconiosis (CWP) is caused by inhalation of coal dust. Because coal dust particles are less than 2–3μm in size, they travel all the way to the alveoli. The coal dust is ingested by alveolar macrophages, which then aggregate around the airways and lymphatics. During their attempts to degrade the particles, macrophages release inflammatory chemical mediators, which cause parenchymal injury and induce fibrosis. The effect of coal dust on the lungs progresses through three stages. Progression through the stages, with continued exposure to coal dust, varies significantly from person to person.
1. Anthracosis refers to the presence of coal-dust pigment within the lung and is asymptomatic.
2. Simple CWP refers to focal accumulations of dust-laden macrophages within the lung. This stage can be further subdivided into macular and nodular CWP. Coal macules are lesions measuring 1–2mm in diameter, while coal nodules are larger and contain collagen fibres. The effect of simple CWP on lung function is minimal.
Silicosis
Silicates are inorganic minerals found in stone and sand. Silica particles are particularly fibrogenic and, after inhalation, enter the terminal respiratory units, where they stimulate the release of chemical mediators from macrophages. They also have toxic effects on macrophages and epithelial cells, denaturing their cell membranes. Grossly, affected lungs contain multiple fibrous nodules, which may coalesce to form large scars. Fibrotic lesions may also occur in the hilar lymph nodes and their characteristic appearance on radiography is referred to as ‘eggshell calcification’. With progression of the disease there is severe impairment of lung function.
Asbestosis
Asbestos is a family of silicates that form fibres. There are two distinct geometric forms of asbestos:
• serpentine: curly flexible fibres; includes the chrysotile form
• amphibole: straight stiff fibres; includes the crocidolite and amosite forms.
Amphiboles are more pathogenic than serpentines. The long, thin fibres have a small enough diameter (0.25–0.5μm) to reach all the way to the alveoli and become impacted there. Alveolar macrophages attempt to ingest and degrade the fibres but, in so doing, release chemical mediators that cause tissue injury and fibrosis resulting in asbestosis. The fibrosis tends to be diffuse rather than nodular. During the attempts at engulfment and digestion, asbestos fibres become coated by mucopolysaccharides and haemosiderin, producing a beaded appearance under microscopy (asbestos bodies). As well as asbestosis, exposure to asbestos can cause other pathological changes in the lungs:
• pleural plaques – the commonest manifestation of asbestos exposure (they are asymptomatic)
• pleural effusion
• diffuse pleural fibrosis
• bronchogenic carcinoma
• mesothelioma
• other extrapulmonary neoplasms, e.g. laryngeal, gastrointestinal.
Berylliosis
Berylliosis results from prolonged exposure to beryllium. Workers in the nuclear and aerospace industries are at risk, but new cases of chronic berylliosis are now rare. Beryllium induces the formation of pulmonary and systemic granulomatous lesions. The pulmonary granulomas eventually become fibrotic.
Caplan’s syndrome
This refers to the coexistence of rheumatoid nodules with pneumoconiosis.
Idiopathic pulmonary fibrosis
In this condition there is diffuse pulmonary fibrosis of unknown aetiology. The disorder typically affects individuals between 45 and 65. With progression of the disease, respiratory failure with or without cor pulmonale ensues. Although some patients benefit from treatment with corticosteroids, median survival is less than 5years.
Hypersensitivity pneumonitis (extrinsic allergic alveolitis)
This is caused by intense prolonged exposure to antigens which evoke type III and type IV hypersensitivity responses. Conditions such as farmer’s lung, pigeon breeder’s lung, and humidifier lung are included in this type of interstitial lung disease.
Drugs and toxins
After they are absorbed into the body, some drugs (e.g. bleomycin, nitrofurantoin, gold, penicillamine and amiodarone) and some other toxic substances (e.g. paraquat) can cause fibrosis within the lungs.
Sarcoidosis
This condition is characterised by non-caseating granulomas within many tissues and organs. There is lung and lymph node involvement in the vast majority of cases. The chest X-ray of affected individuals typically shows bilateral hilar lymphadenopathy.
Pulmonary involvement in collagen vascular disorders
• Systemic sclerosis (scleroderma)
• Systemic lupus erythematosus (SLE)
• Rheumatoid arthritis, pulmonary involvement occurs in one of four forms:
• chronic pleuritis
• diffuse interstitial fibrosis
• intrapulmonary rheumatoid nodules
• rheumatoid nodules with pneumoconiosis (Caplan’s syndrome).
Diffuse pulmonary haemorrhage syndromes
Goodpasture’s syndrome
In this condition, circulating anti-glomerular basement membrane (anti-GBM) antibodies cross-react with pulmonary alveolar basement membrane, resulting in intrapulmonary haemorrhage.
Idiopathic pulmonary haemosiderosis
Typically affects children and is manifest by recurrent episodes of intra-alveolar haemorrhage.
Vasculitides causing intra-pulmonary haemorrhage
Involvement of the lung by vasculitides such as hypersensitivity angiitis, Wegener’s granulomatosis and SLE can cause intrapulmonary haemorrhage.
Adult respiratory distress syndrome
Adult respiratory distress syndrome (ARDS) is characterised by rapid onset of respiratory distress, initiated by the delivery of a massive insult to the alveolar capillary walls. Endothelial damage allows leakage of proteins and fibrin into the alveoli with the formation of hyaline membranes, which act as barriers to gas exchange. The insult can occur in a number of clinical settings, but infection and physical injuries such as burns and head injuries are the most common causes. The condition is fatal within a few days in 50% of cases despite intensive therapy. For the majority of survivors, there is permanent lung damage with fibrosis. Resolution of the inflammation and complete recovery is unusual.
Bronchiolitis obliterans organising pneumonia
The major pathological finding in bronchiolitis obliterans organising pneumonia (BOOP) is polypoid plugs of loose fibrous tissue (Masson bodies) filling the bronchioles. Aetiologies include infections, inhaled toxins, drugs, collagen vascular diseases and bronchial obstruction.
Miscellaneous
Other less common causes of interstitial lung disease include conditions such as Langerhans’ cell histiocytosis X, pulmonary eosinophilia and pulmonary alveolar proteinosis.
Vascular diseases of the lungs
Pulmonary oedema and congestion
Pulmonary oedema signifies increased fluid in the lung interstitium, causing breathlessness and cough productive of frothy, pink sputum. There are several causes of pulmonary oedema.
• Common cause:
• increased venous hydrostatic pressure.
• Uncommon causes:
• injury to the alveolar capillary bed, e.g. acute respiratory distress syndrome (ARDS)
• blockage of lymphatic drainage
• lowered plasma oncotic pressure.
The commonest cause of pulmonary oedema is increased venous hydrostatic pressure, most often resulting from left ventricular failure. When the increasing hydrostatic pressure exceeds the oncotic pressure within the pulmonary capillaries, fluid is forced out of the vessels and into the lung interstitium, with resultant pulmonary oedema. Oedematous lungs are heavy, congested and wet. Histologically, the alveolar capillaries are engorged, and frothy, pink precipitate can be seen within the alveoli. Alveolar microhaemorrhages may be seen with associated haemosiderin-laden macrophages (‘heart failure cells’).
Pulmonary embolism
An embolus is a detached intravascular solid, liquid or gaseous mass, which is carried by the blood to a site distant from its point of origin. Pulmonary embolism refers to the occlusion of some part of the pulmonary arterial tree by an embolus.
Pulmonary thrombo-embolism
This is by far the commonest type of embolus. In most cases, the thrombotic mass originates in the deep veins of the legs above the level of the knee. After detachment, the embolic mass travels via the bloodstream to the right side of the heart and into the main pulmonary artery. Thereafter, the calibre of the blood vessels decreases progressively and the embolus eventually becomes lodged. The consequences of this depend on the volume of lung tissue subsequently deprived of blood. Emboli that occlude the main pulmonary artery or impact across the bifurcation (saddle embolus, see Ch. 14, Figure 35) or occlude the right or left pulmonary artery, often cause sudden death. Death is usually due to acute right heart failure.
Because of the dual blood supply to most parts of the lungs, pulmonary embolism causes infarction only when the circulation is already inadequate, e.g. patients with cardiac or respiratory disease. Infarcts are typically wedge shaped. Most emboli eventually resolve by fibrinolysis. However, since patients who have had one pulmonary embolus are at high risk of having more, therapy with fibrinolytic agents is usually initiated. Prevention of deep vein thrombosis is of major clinical importance.
Fat embolism
Fat emboli result from fracture of bones containing fatty marrow (usually the long bones, e.g. femur), or by massive injury to subcutaneous fat. The globules of fat enter torn veins and become emboli.
Gas embolism
Air emboli can occur after chest trauma. Nitrogen can come out of solution in divers during decompression (‘decompression sickness’).
Amniotic fluid embolism
This type of embolus can occur during delivery or abortion. During labour, amniotic fluid may enter torn uterine veins. Flakes of keratin and epithelial cells shed from the fetal skin embolise to the lungs, where they become lodged. If the patient survives the initial crisis, thrombogenic substances contained within the amniotic fluid trigger disseminated intravascular coagulation.
Tumour embolism
Clusters of tumour cells may enter the venous circulation and, if large enough, occlude the pulmonary veins.
Pulmonary hypertension
Pulmonary hypertension is defined as the point when the mean pulmonary blood pressure reaches a quarter of the systemic level. Patients present with dyspnoea and fatigue, or anginal-type chest pain. Over time, symptoms worsen and right ventricular hypertrophy develops with ensuing cor pulmonale.
Pulmonary hypertension can be primary, but it is most often secondary to other cardiopulmonary conditions such as:
• pulmonary embolism
• obstructive lung diseases
• interstitial lung diseases
• left ventricular failure
• mitral stenosis.
Pathology
Changes seen within the arteries include the deposition of atheroma, an increase in the thickness of the muscular media (medial hypertrophy) and intimal fibrosis. Changes relating to the underlying cause are also seen.
Lung tumours
Bronchogenic carcinoma
Bronchogenic carcinoma is the commonest malignancy in the UK, and has the worst prognosis. It accounts for around a third of all cancer deaths in men, and the incidence is rising in women. Typically, patients are aged between 40 and 70years.
Aetiology
Cigarette smoking There is overwhelming evidence implicating cigarette smoking as a major risk factor for the development of lung cancer.
Occupational hazards There is a high correlation between asbestos exposure and the risk of lung cancer, especially adenocarcinoma. The risk is heightened dramatically if the individual also smokes. All types of radiation may be carcinogenic. There is also an increased risk of lung cancer among people who work with nickel, chromates, coal, mustard gas, arsenic, beryllium and iron.
Scarring Some lung cancers, especially adenocarcinomas, appear to arise in areas of previous scarring, e.g. old tuberculous foci. It has been proposed that scarring induces dysplasia of pneumocytes, predisposing to lung cancer in that area.
Classification
Bronchogenic carcinoma is classified according to the appearance under light microscopy:
• squamous cell carcinoma (25–40%)
• adenocarcinoma (25–40%)
• small cell carcinoma (20–25%)
• large cell carcinoma (10–15%).
Occasionally, lung carcinomas are simply classified as either small cell carcinoma or non-small cell carcinoma. The relevance of this type of classification is that small cell carcinomas are more responsive to chemotherapy than any of the other types of lung cancer.
Squamous cell carcinoma This type of lung cancer is closely associated with smoking. The tumour commonly arises in the central bronchi and spreads locally, usually at a rapid rate. Metastases usually occur later than with the other types of lung cancer. The tumours are thought to arise from areas of squamous metaplasia through grades of dysplasia.
Adenocarcinoma This type of cancer is usually peripheral and is sometimes associated with scarring. It is the most common type of lung cancer in women and non-smokers. Adenocarcinomas grow more slowly than the squamous cell carcinomas.
Large cell carcinoma These are usually central, highly aggressive tumours. Histologically, the cells are highly pleomorphic with numerous bizarre mitoses. Large cell carcinoma may represent squamous cell carcinomas and adenocarcinomas that are so poorly differentiated that they can no longer be recognised.
Gross pathology
The tumour starts as an irregular thickening, which grows either exophytically (outwards into the lumen), to produce an intraluminal mass, or endophytically (into the bronchial wall), causing erosion of the bronchial wall. Spread is by local extension to neighbouring tissues, spread to lymph nodes and distant metastases.
Clinical features
The clinical features of lung cancer are the result of local spread within the lung, direct spread to neighbouring structures, distant spread or paraneoplastic syndromes.
Effects of local intrapulmonary spread:
• cough – due to irritation of the airways
• haemoptysis – due to erosion of small blood vessels
• wheezing, stridor, atelectasis, pneumonia, bronchiectasis, lung abscess – due to airway obstruction.
Effects of direct spread to neighbouring structures:
• pain – with involvement of nerves, or the pleura (pleuritis)
• shortness of breath – extension to the pleura causes pleural effusions
• hoarse voice – with involvement of the recurrent laryngeal nerve
• paralysis of the diaphragm – with involvement of the phrenic nerve
• symptoms caused by a tumour in the lung apex (Pancoast’s tumour):
• Horner’s syndrome (sunken eye, small pupil, eyelid drooping and loss of sweating on the same side of the lesion) due to involvement of the sympathetic ganglia
• pain and weakness in the shoulder and arm due to involvement of the branchial plexus
• vena caval syndrome – characterised by facial congestion, oedema of the face, neck and upper arms, and distension of the veins in the neck and over the chest.
Effects of distant spread: depend on the sites of the secondary deposits.
Paraneoplastic syndromes These are signs or symptoms in cancer patients that are not explicable in terms of local or metastatic spread of the tumour. General paraneoplastic syndromes include weight loss, fever and loss of appetite.
Paraneoplastic syndromes may be associated with the secretion of hormones (endocrinopathies). All types of bronchogenic carcinoma can secrete hormones, including antidiuretic hormone (ADH), adrenocorticotrophic hormone (ACTH), parathormone, parathyroid hormone-related peptide, some cytokines, calcitonin, gonadotrophin and serotonin, and the syndromes associated with secretion of these hormones may become clinically apparent (e.g. development of Cushing’s syndrome with the secretion of ACTH).
Other paraneoplastic syndromes that can occur are:
• Lambert–Eaton myasthenic syndrome
• peripheral neuropathy
• hypertrophic pulmonary osteoarthropathy.
Treatment and prognosis
The stage of the tumour at presentation is of prognostic significance (the tumour node metastasis (TNM) staging system is usually adopted), but the prognosis is generally poor. The only hope of cure is total resection of the tumour, which is only possible with peripheral tumours without metastases. Some patients with small cell carcinoma benefit from radiotherapy and chemotherapy, which can induce remission (occasionally sustained).
Neuroendocrine tumours
Three types of malignant neuroendocrine tumours are found in the lung:
• small cell carcinoma (discussed above)
• bronchial carcinoid
• large-cell neuroendocrine carcinoma.
Bronchial carcinoids are considered to be tumours of low-grade malignancy and resemble carcinoid tumours found elsewhere, e.g. intestine. They are capable of producing the classic carcinoid syndrome. Growth of these tumours is slow and they may be amenable to resection. Consequently, the survival figures for bronchial carcinoids are much better than those for bronchogenic carcinoma.
Large-cell neuroendocrine tumours are more aggressive than bronchial carcinoids.
Miscellaneous primary lung tumours
Included in this category of lung tumour are:
• benign and malignant tumours of salivary gland-type
• benign and malignant mesenchymal tumours
• benign and malignant lymphoreticular tumours
• lung hamartomas
• adenomas.
15.4. The pleura
Structure of the pleura
The pleura are composed of two opposing layers of connective tissue lined by mesothelial cells. The visceral pleura covers the lungs and the parietal pleura lines the internal thoracic wall and covers the thoracic surface of the diaphragm, the heart and the mediastinum. The potential space between these two layers is called the pleural cavity or pleural space.
Pleural effusion
This term denotes an increased accumulation of fluid between the two layers of the pleura, causing shortness of breath. Pleural effusions can occur in the following settings:
• increased hydrostatic pressure, e.g. congestive cardiac failure
• increased capillary permeability, e.g. pneumonia, bronchogenic carcinoma, mesothelioma
• decreased intrapleural negative pressure, e.g. atelectasis
• decreased lymphatic drainage, e.g. mediastinal carcinomatosis
• decreased oncotic pressure (hypoalbuminaemia), e.g. nephrotic syndrome, liver cirrhosis.
Pleural effusions can be either inflammatory, when they are associated with a pleuritis, or non-inflammatory (see Table 23). To try to establish the cause of the effusion, a diagnostic aspiration of the pleural fluid is useful. If the fluid is a transudate (protein <20g/L), then heart failure or hypoalbuminaemia is the cause; if the fluid is an exudate (protein >30g/L), then all other causes should be considered.
| Type of pleural effusion | Common associations | |
|---|---|---|
| Inflammatory | Serofibrinous effusion | Inflammation of the adjacent lung, e.g. pneumonia, lung abscess, tuberculosis, collagen vascular diseases |
| Suppurative effusion (empyema, pyothorax) | Suppuration in the adjacent lung | |
| Haemorrhagic effusion | Neoplastic infiltration, pulmonary infarction | |
| Non-inflammatory | Serous effusion (hydrothorax) | Cardiac failure, renal failure, liver failure |
| Haemothorax | Trauma to chest wall, ruptured aortic aneurysm | |
| Chylothorax (lymph in the pleural space) | Obstruction of the lymphatics by tumour |
Pneumothorax
Pneumothorax refers to air/gas in the pleural cavity. When severe, a pneumothorax can cause symptoms of respiratory distress and may be fatal. Resorption of the air in the pleural space occurs slowly, and if deemed necessary, interventional procedures may be used to remove the air from the pleural cavity, e.g. chest drain.
Spontaneous pneumothorax
This type of pneumothorax occurs in people with pre-existing disease that causes rupture of an alveolus. It is most often seen in association with emphysema, asthma and tuberculosis.
Traumatic pneumothorax
This can occur following penetrating injuries to the chest.
Therapeutic pneumothorax
Intentional deflation of the lung was a method once used to enhance healing of tuberculous lesions.
Spontaneous idiopathic pneumothorax
This condition occurs in young healthy people, and seems to be due to rupture of small peripheral usually apical subpleural blebs. Recurrent attacks are common.
Tumours
Tumours of the pleura may be benign or malignant.
Benign
The solitary fibrous tumour of the pleura is a tumour that is often attached to the pleura by a peduncle. These benign tumours can become enormous.
Malignant
Malignant tumours of the pleura may be primary or secondary. Secondary (metastatic) tumours (e.g. from lung carcinomas or breast carcinomas) are much more common than primary tumours of the pleura.
Malignant mesothelioma
This term refers to a malignant tumour of mesothelial cells, and when applied to the pleura, means a primary malignant tumour of the pleura.
Aetiology Malignant mesothelioma is associated with exposure to asbestos, particularly crocidolite (‘blue’ asbestos) and amosite (‘brown’ asbestos). It should be noted, however, that for any individual asbestos worker, the risk of developing malignant mesothelioma is much lower than the risk of developing lung carcinoma.
Pathology The tumour begins as pleural nodules that enlarge and extend over the surface of the lung, gradually encasing it. Infiltration of the chest wall and intercostal muscles by the tumour causes severe pain. Histologically, mesotheliomas may be composed of epithelial cells (epithelioid type) or spindle cells (sarcomatoid type) or a mixture of both.
Self-assessment: questions
One best answer questions
2. A 79-year-old retired shipyard worker complains of marked progressive weight loss over the last 4months and increasing breathlessness. On chest imaging he is found to have a large unilateral pleural effusion and diffuse pleural thickening encasing the lung. The most likely diagnosis is:
a. bronchial carcinoma
b. asbestosis
c. silicosis
d. mesothelioma
e. empyema
True-false questions
1. The following statements are correct:
a. epiglottitis is usually caused by the bacterium Haemophilus influenzae
b. squamous cell carcinoma of the larynx is strongly associated with cigarette smoking
c. epithelial dysplasia precedes squamous cell carcinoma of the larynx
d. laryngeal cancer often presents with persistent hoarseness of voice
e. laryngeal cancer may present with haemoptysis
2. The following statements are correct:
a. smokers are at an increased risk of developing pneumonia
b. bronchopneumonia is characterised by consolidation of a large portion of a lobe or of an entire lobe
c. Pneumocystis carinii is the organism frequently implicated in the development of bronchopneumonia
d. lobar pneumonia is most frequently caused by the bacterium Streptococcus pneumoniae
e. pneumonia can be treated with antibiotics and is now never fatal
3. The following statements regarding tuberculosis are correct:
a. since the 1980s, Western countries have seen a decline in the incidence of tuberculosis
b. primary pulmonary tuberculosis is always symptomatic
c. histologically, tuberculosis is characterised by the presence of caseating granulomas
d. tuberculosis may affect the gastrointestinal tract
e. miliary tuberculosis represents lymphohaematogenous dissemination of the infection
4. The following statements regarding obstructive airways disease are correct:
a. in the pathogenesis of chronic bronchitis, smoking induces hypersecretion of mucus in airways
b. in emphysema there is abnormal permanent dilatation of the bronchi
c. emphysema may be associated with α1-antitrypsin deficiency
d. asthma is characterised by irreversible bronchoconstriction
e. obstruction and infection are important influences in the pathogenesis of bronchiectasis
5. Interstitial lung disease:
a. is associated with reduced vital capacity of the lung
b. is associated with reduced peak expiratory flow rate (PEFR)
c. may be caused by inhalation of mineral dusts
d. may lead to cardiac failure
e. in its advanced form results in a macroscopic appearance referred to as ‘honeycomb lung’
6. The following statements are correct:
a. the most common cause of pulmonary oedema is left ventricular failure
b. an embolus may be a solid, liquid or gas
c. pulmonary thrombo-embolism may cause pleuritic chest pain
d. pulmonary thrombo-emboli most commonly originate from the arteries of the lower limbs
e. pulmonary hypertension is almost always idiopathic
7. The following statements regarding lung cancer are correct:
a. smoking is associated with an increased risk of developing small cell carcinoma of the lung
c. bronchogenic carcinoma may cause development of a hoarse voice
d. there is an association between bronchogenic carcinoma and Cushing’s syndrome
e. lung cancer may be associated with a pleural effusion
8. The following statements are correct:
a. a tension pneumothorax is a medical emergency that requires immediate management
b. pneumonia is the likely cause of a pleural effusion that has a protein content of <20g/L
c. involvement of the pleural cavity by tumour induces a haemorrhagic pleural effusion
d. mesothelioma is a benign tumour of the pleura
e. asbestos exposure is a risk factor for the development of mesothelioma
9. The following statements are true:
a. pleural effusions are always bilateral
b. idiopathic pulmonary fibrosis is one of the diseases associated with finger clubbing
c. cystic fibrosis is a recessively inherited disorder
d. exposure to asbestos is called ‘asbestosis’
e. there may be a significant time lag between exposure to asbestos and development of an asbestos-related disease
10. The following statements are true:
a. malignant tumours can cause pulmonary embolism
b. status asthmaticus is a medical emergency
c. patients with chronic bronchitis have an increased risk of developing pneumonia
d. small cell carcinomas of the lung are the only lung tumours that can secrete hormones
e. Goodpasture’s syndrome is an example of a type II hypersensitivity reaction
Case history questions
Case history 1
A 58-year-old man was admitted to hospital for repair of an inguinal hernia under a general anaesthetic. He smoked 10 cigarettes a day for 40years (20 pack years). On the third postoperative day, he became pyrexial and developed a cough productive for green sputum. A blood count showed a raised white cell count with increased neutrophil polymorphs. A chest X-ray showed patchy opacities.
1. From these symptoms, signs and investigations, what is the most likely diagnosis?
2. What predisposing factors are present in this case?
3. Describe the pathological changes in the lungs.
Case history 2
A 72-year-old woman presents to her general practitioner with a persistent cough, haemoptysis, shortness of breath, weight loss and a hoarse voice. She is an ex-smoker. On clinical examination, she has finger clubbing, wasting of the small muscles of the left hand and left-sided Horner’s syndrome.
1. What is the most likely diagnosis?
2. What is the pathological basis for these signs and symptoms?
3. What further investigations should be performed?
Short note questions
Write brief notes on the following:
1. The classification and pathogenesis of emphysema.
2. Respiratory tract pathology caused by asbestos exposure.
3. The differential diagnosis of a pleural effusion.
Viva questions
1. What diseases of the respiratory tract are related to smoking?
2. What defence mechanisms are employed by the respiratory tract to reduce the risk of infection by microorganisms?
Self-assessment: answers
One best answer
2. d. The clinical symptoms and signs suggest a malignant disease process; the pleural thickening encasing the lung is characteristic of malignant mesothelioma (it is not usually seen with bronchial carcinoma). Occupational history of asbestos exposure is aetiologically important in mesothelioma; workers in a wide range of construction industries may have been exposed to carcinogenic asbestos fibres. Pneumoconioses (including silicosis and asbestosis) cause fibrosis within the lung, as opposed to pleural thickening.
True-false answers
1.
a. True.
b. True.
c. True.
d. True.
e. True.
2.
a. True. Cigarette smoke interferes with alveolar macrophage function and causes injury to the mucociliary apparatus.
b. False.
c. False.
d. True.
e. False. Despite antibiotic treatment pneumonia may still be fatal, especially in the debilitated.
3.
a. False. Since the 1980s, Western countries have seen a rise in the incidence of tuberculosis.
b. False. Primary tuberculosis is frequently asymptomatic.
c. True.
d. True. Either during lymphohaematogenous dissemination or during primary infection due to ingestion of Mycobacterium bovis (unpasteurised milk).
e. True.
4.
a. True.
b. False. There is permanent dilatation of the airways distal to the terminal bronchioles.
c. True.
d. False. The bronchoconstriction is characteristically reversible.
e. True.
5.
a. True.
b. False. The PEFR is usually normal.
c. True.
d. True. Interstitial lung disease can lead to cor pulmonale.
e. True.
6.
a. True.
b. True.
c. True.
d. False. They most frequently originate from the veins of the lower limbs.
e. False. Most cases of pulmonary hypertension are secondary to other pathology.
7.
a. True.
b. False. Small cell carcinomas are particularly sensitive to chemotherapy.
c. True. If a lung tumour spreads into the mediastinum, there may be involvement of the recurrent laryngeal nerve as it passes close to the aortic arch.
d. True. Some bronchogenic tumours secrete hormones. Secretion of ACTH may induce Cushing’s syndrome.
e. True.
8.
a. True.
b. False. A protein content of <20g/L indicates that the effusion is a transudate. Pneumonia would cause an exudative effusion.
c. True.
d. False. Although the name of this tumour suggests that it is benign, mesotheliomas are in fact malignant.
e. True.
9.
a. False.
b. True.
c. True.
d. False. Asbestosis refers to interstitial fibrosis due to asbestos.
e. True.
10.
a. True.
b. True.
c. True.
d. False.
e. True.
Case history answers
Case history 1
2. Comment: You need to know the defence mechanisms that are in operation in the respiratory tract to prevent infection, and ways in which they may be impaired predisposing individuals to pneumonia. There are several predisposing factors in this case. First, general anaesthesia would cause suppression of the cough reflex. Second, coughing increases intra-abdominal pressure and so any pain associated with the abdominal surgical wound would be increased when the patient coughs. Hence he may try to avoid coughing. Third, the patient is a smoker, and cigarette smoke interferes with alveolar macrophage function and injures the mucociliary apparatus.
3. In bronchopneumonia there is often widespread but patchy consolidation. The primary infection is centred on the bronchi, with spread to involve the adjacent bronchioles and alveolar spaces. In this case, the changes may be seen mostly in the dependent parts of the lung, where the retained secretions would accumulate. Macroscopically, the lungs would show firm red/grey airless areas and pus may be present in the airways. Microscopically, there is acute inflammation in the airways.
Case history 2
1. This combination of symptoms in an elderly person who is an ex-smoker is highly suggestive of a malignant process. The findings on clinical examination support a diagnosis of a lung cancer. The Horner’s syndrome, together with the muscle wasting seen in the hands, is particularly suggestive of an apical (Pancoast’s) tumour.
2. The cough may be due to distal infection, airway irritation, or airway obstruction by a tumour or lymph node mass. Haemoptysis results from ulceration of the tumour and consequent bleeding into the airway. Shortness of breath may be due to pleural effusions or obstruction of a main airway by tumour. The hoarse voice is caused by recurrent laryngeal nerve palsy secondary to mediastinal spread. Wasting of the small muscles of the hand is due to infiltration of the branchial plexus. Horner’s syndrome results when there is involvement of the cervical sympathetic plexus.
3. A tissue diagnosis should be sought so that an appropriate management plan can be formulated. Small cell carcinomas may be more sensitive to chemotherapy and radiotherapy than non-small cell carcinomas. Several methods may be used. Cells in sputum, bronchoscopy-obtained bronchial brushings and washings, or pleural fluid can be examined under the microscope for any cytological features of malignancy. In the vast majority of cases small cell and non-small cell carcinomas can be distinguished. For central tumours, tissue may be obtained during bronchoscopy (bronchial biopsy). Biopsy of peripheral tumours may be done percutaneously (needle biopsy). After tissue diagnosis, further investigations are directed towards tumour staging, e.g. CT scan.
Short note answers
1. Comment: Start your answer with the definition of emphysema. Then go on to explain how emphysema is classified into four main types according to the anatomical distribution of the lesions, and the appearance of the lungs with the naked eye or hand lens. The four main types are centrilobular, panlobular, paraseptal and irregular, and you should be able to describe each of them. The pathogenesis of emphysema is not fully understood, but evidence suggests that emphysema is due to an imbalance between protease and anti-protease activity in the lung. Hence its association with smoking (which causes increased recruitment of neutrophil polymorphs to the lung where they release elastase) and α1-antitrypsin deficiency.
2. Exposure to asbestos is linked to the development of a number of disorders of the respiratory tract, namely pleural plaques (asymptomatic), pleural effusions, asbestosis, bronchogenic carcinoma, mesothelioma and laryngeal carcinoma. These conditions usually develop in the setting of occupational exposure to asbestos, where the fibres can be inhaled.
3. Pleural effusion denotes the presence of fluid within the pleural space. There are several causes of a pleural effusion, but they can be divided into ‘inflammatory’ and ‘non-inflammatory’. Comment: you should know the various causes of each. Pleural effusions can be detected either during physical examination of the chest or on imaging (e.g. chest X-ray), and to determine the cause of an effusion you must extract as much information as possible from these, as well as taking a thorough history. A diagnostic tap can also be performed. The appearance of the fluid may provide clues. Note if the fluid is clear, cloudy or bloodstained, or composed entirely of blood, pus or lymph. If the protein content is measured, you can determine whether the fluid is a transudate or an exudate – inflammatory effusions are exudates and therefore have a higher protein content. If neoplastic infiltration is suspected, the fluid can be examined under the microscope for the presence of malignant cells.
Viva answers
2. The respiratory tract employs several defence mechanisms to clear or destroy inhaled microorganisms. These include: nasal mucus (in which particles are trapped); coughing and sneezing; the mucociliary apparatus (which traps particles in the lung and moves them within the mucous layer towards the nasopharynx where they are swallowed or expectorated); and alveolar clearance (particles that reach the alveoli are phagocytosed by alveolar macrophages). Pneumonia results whenever these defence mechanisms are impaired.