Respiratory Care in Alternative Settings
After reading this chapter you will be able to:
 Describe alternative care settings in which respiratory care is often performed.
Describe alternative care settings in which respiratory care is often performed.
 Discuss more recent developments and trends in respiratory care at alternative sites.
Discuss more recent developments and trends in respiratory care at alternative sites.
 Identify who regulates alternative care settings.
Identify who regulates alternative care settings.
 List the standards that apply to the delivery of respiratory care in alternative settings.
List the standards that apply to the delivery of respiratory care in alternative settings.
 Describe how to help formulate an effective discharge plan.
Describe how to help formulate an effective discharge plan.
 List factors to evaluate when assessing alternative care sites and support services.
List factors to evaluate when assessing alternative care sites and support services.
 Discuss how to justify, provide, evaluate, and modify oxygen (O2) therapy in alternative care settings.
Discuss how to justify, provide, evaluate, and modify oxygen (O2) therapy in alternative care settings.
 Explain how to select, assemble, monitor, and maintain O2 therapy equipment in alternative settings.
Explain how to select, assemble, monitor, and maintain O2 therapy equipment in alternative settings.
 Identify the special challenges that exist in providing ventilatory support outside an acute care hospital.
Identify the special challenges that exist in providing ventilatory support outside an acute care hospital.
 Describe how to instruct patients or caregivers and confirm their ability to provide care in alternative settings.
Describe how to instruct patients or caregivers and confirm their ability to provide care in alternative settings.
 Identify which patients benefit the most from ventilatory support outside acute care hospitals.
Identify which patients benefit the most from ventilatory support outside acute care hospitals.
 Explain how to select, assemble, monitor, and maintain portable ventilatory support and continuous positive airway pressure equipment, including applicable interfaces or appliances.
Explain how to select, assemble, monitor, and maintain portable ventilatory support and continuous positive airway pressure equipment, including applicable interfaces or appliances.
 Describe proper documentation regarding patient evaluation and progress in alternative settings.
Describe proper documentation regarding patient evaluation and progress in alternative settings.
 State how to ensure safety and infection control in alternative patient care settings.
State how to ensure safety and infection control in alternative patient care settings.
With the introduction of Medicare in 1965, the cost savings and patient welfare benefits associated with home care and other nonacute care settings were recognized. This legislation established a reimbursement structure for health care services in alternative settings, including services provided at home. Since its adoption, Medicare is credited with substantial increases in the number of patients cared for at home. From 1967-1985, the number of home care agencies certified to participate in Medicare tripled to almost 6000. This figure peaked to slightly more 10,000 in 1997, the year in which the Balanced Budget Act (BBA) was introduced. The BBA of 1997, which is discussed in more detail in the following section, and other subsequent legislation had a monumental impact on health care reimbursement by reducing payments to durable medical equipment (DME) companies, home health agencies, and other alternative sites. Despite this reduction in reimbursement, however, approximately 10 million Americans continued to receive health care at home in 2007 at an estimated cost of approximately $50 million.1
Alternative health care settings offer the advantage of lower costs and enhanced patient comfort compared with acute care facilities. In 2007, the average daily acute care hospital charges were more than $4000 versus less than $1000 for SNFs.1 However, improper or premature discharging of patients to alternative care settings and poor care plan implementation can erase these benefits and result in short-term readmission. This problem is particularly relevant to respiratory care because it has been found that the short-term readmission rate for patients with chronic obstructive pulmonary disease (COPD) is almost 20%.2,3 Proper patient screening and evaluation and appropriate discharge planning, including a multidisciplinary care plan, proper care plan implementation, and patient follow-up, can minimize the risk of readmission.4
This chapter provides relevant definitions, discusses more recent policy developments, discusses aspects of optimal discharge and patient care planning, and reviews various therapeutic respiratory modalities in alternative care sites. A major alternative site is the sleep laboratory where respiratory therapists (RTs) conduct polysomnography, or sleep studies; this facet of respiratory care is covered in Chapter 30, which focuses exclusively on the pathophysiology, diagnosis, and treatment of disorders of sleep.
More Recent Developments and Trends
One of the most notable changes is the introduction of Medicare’s prospective payment system (PPS). Until the introduction of the PPS in the 1990s, Medicare mainly reimbursed providers such as home care agencies for “reasonable” charges up to a maximum monthly or one-time amount. However, under the PPS, reimbursement for many types of respiratory equipment in alternative sites is based on a predetermined monthly payment, adjusted for factors such as the health condition and geography. Additionally, certain types of respiratory equipment are categorized as capped-rental items. Capped-rental items are items eligible for reimbursement under the PPS for only a predetermined number of months, after which the equipment is deemed owned by the patient and rental payments cease. Other legislation that has substantially affected Medicare reimbursement includes the BBA of 1997 and the Deficit Reduction Act of 2005. Among other things, the BBA reduced reimbursement for home O2 by 25% in 1998 and another 5% in 1999. The Deficit Reduction Act modified the PPS further by again reducing monthly payment for selected respiratory equipment and adding to the list of capped-rental items. Under this legislation, modalities such as home O2 and bilevel positive airway pressure (bilevel PAP) with timed respiratory rate backup are capped at 36 months (O2) and 13 months (bilevel PAP). The net effect of these and subsequent reimbursement reductions has been much lower reimbursement for respiratory care equipment in alternative sites. This unfavorable trend continues to present challenges to agencies and facilities attempting to provide quality care to patients in such settings.5
At the time of the writing of this chapter, other policy and legislative changes have been enacted but not yet fully implemented. Most notable of these is the Patient Protection and Affordable Care Act of 2010. There are many facets to this bill ranging from the expansion of health care coverage to many uninsured Americans, prohibiting the exclusion of preexisting conditions, and increasing the scope of coverage for certain types of preventive care. However, the provisions of this bill are still being closely examined, and modifications are likely. The exact impact of this bill and any related legislation on the U.S. health care system and the field of respiratory care remains to be seen.6
Another area that has been under review for some time is reimbursement for reasonable time spent by RTs in administering care and patient education in alternative care settings such as the home. Reimbursement under federal Medicare and state Medicaid programs applies only to respiratory equipment, such as home O2 and mechanical ventilators, and RT time is not covered. Although a few states have piloted programs to reimburse for certain therapies and education done by RTs in alternative settings, widespread acceptance has not occurred. Although Medicare provides limited payment for nursing and physical therapy at home, it generally does not reimburse for RTs in such a setting. The American Association for Respiratory Care (AARC), through its Government Affairs initiatives, continues to promote legislation and sponsor efforts to expand the recognition of RTs. As a result of the delicate balance among factors such as increasing health care costs, limited resources, and patient care, it appears that the PPS and other related policies will continue to be reviewed and modified by government agencies such as the Centers for Medicare and Medicaid Services (CMS).7
Other changes affecting RTs in alternative sites have resulted from research study outcomes. In 1999, a report from Muse and Associates to the AARC found that Medicare beneficiaries treated by RTs had better outcomes and lower cost in such facilities.8 More recently, other research projects have shown cost and quality benefits when RTs are involved in the management of patients receiving home O2 therapy and in outpatient asthma education programs.9 It is hoped that the Muse Report and the growing body of evidence stemming from other initiatives will help public agencies and private health care payers recognize the value of RTs in alternative care settings and shape policies accordingly.
Relevant Terms and Goals
Long-Term Subacute Care Hospitals
Advances in technology, research, and clinical specialization have permitted more acutely ill patients to be treated outside of large-scale, acute care hospitals. Over the past decade, LTACHs have become more prevalent. These facilities provide highly focused care to patients with complex medical conditions, including patients who have been ventilator-dependent and difficult to wean. Generally, LTACHs employ a highly experienced clinical staff, including RTs, to provide integrated interdisciplinary care using the latest equipment and specialized treatment protocols. During the 20- to 30-day typical length of stay at an LTACH, patients commonly experience significant improvement, including successful weaning from mechanical ventilation and increased tolerance for activities of daily living.10
Subacute Care
According to the National Association of Subacute/Post Acute Care, subacute care is a comprehensive level of inpatient care for stable patients who (1) have experienced an acute event resulting from injury, illness, or exacerbation of a disease process; (2) have a determined course of treatment; and (3) require diagnostic or invasive procedures but not those requiring acute care.10 Typically, the severity of the patient’s condition requires active physician direction with frequent on-site visits, professional nursing care, significant ancillary services, and an outcomes-focused interdisciplinary approach employing a professional team.
The goal of acute care is to apply intensive resources to stabilize patients after severe episodic illness, whereas subacute care aims to restore the whole patient back to the highest practical level of function—ideally self-care. This holistic approach requires goal-oriented interdisciplinary team care, with frequent assessment of progress and a time-limited plan of care.11
Home Care
The AARC defines respiratory home care as specific forms of respiratory care provided in the patient’s place of residence by personnel trained in respiratory care working under medical supervision.12 The primary goal of home care is to provide quality health care services to patients in their home setting, minimizing their dependence on institutional care. In regard to respiratory home care, several specific objectives are evident. Respiratory home care can contribute to the following:
• Supporting and maintaining life
• Improving patients’ physical, emotional, and social well-being
• Promoting patient and family self-sufficiency
Although not all aspects of respiratory home care have proven effective, various studies have shown that carefully selected treatment regimens can be of significant benefit to patients. These benefits include increased longevity, improved quality of life, increased functional performance, and a reduction in the individual and societal costs associated with hospitalization.13,14
Standards
Regulations
Most reimbursement for care in alternative settings is through either the federal Medicare program or federal or state Medicaid programs. As the largest purchaser of health services, the federal government (in connection with state and local governments) plays a major role in setting standards and regulating this industry. The federal agency responsible for the overall administration of Medicare and Medicaid is the Centers for Medicare and Medicaid Services (CMS). Created in 1997, CMS oversees the framework for providing health coverage to elderly adults, disabled adults, and many disadvantaged young children in the United States.5,6
As part of this structure, CMS created the Medicare Provider Certification Program. This program ensures that institutional providers that serve Medicare beneficiaries, including hospitals, SNFs, LTACHs, home health agencies, and assisted living facilities, meet minimum health and safety requirements. These requirements are called conditions of participation. Current conditions of participation emphasize quality indicators, outcome measures, and cost efficiency designed to improve the quality and effectiveness of care provided to beneficiaries.5,6 Institutions undergo certification surveys to determine their compliance with the applicable conditions of participation. These surveys are conducted by either state survey agencies or private accrediting organizations, such as The Joint Commission (TJC), which is discussed in more detail in the following section.15,16
Private Sector Accreditation
The primary organization responsible for standard setting and voluntary accreditation of care providers in alternative settings is TJC. To assist hospitals and health care organizations with the accreditation process and overall performance improvement, TJC develops and publishes standards and National Patient Safety Goals for long-term and subacute care, home care, and assisted living facilities. The standards cover general functional categories relating to quality patient care and the process and structure of the organization. These categories include patient rights, ethics, and assessment and organizational leadership and management of information. The patient safety goals target for improvement common problem areas for health care organizations, such as proper patient identification, medication safety, and infection control.15,16
In regard to home care, TJC applies different protocols to assess different types of home care agencies. The home equipment management protocol pertains only to companies that rent or sell home medical equipment. In most cases, this type of provider is involved only with basic O2 and aerosol therapy setups and does not provide in-depth visits for patient assessment or evaluation. Agencies involved with clinical respiratory services perform periodic home visits with patient assessment. Agencies applying for accreditation at this level are involved with more sophisticated forms of home care that require routine follow-up visits, such as management of artificial airways and ventilator-dependent patients. The standards for this type of home care accreditation are more extensive and rigorous.15,16
Traditional Acute Care Versus Alternative Setting Care
For the RT, working in the alternative care setting is distinctly different from working in an acute care hospital. Key differences involve resource availability, supervision and work schedules, documentation and assessment, and provider-patient interaction (Table 51-1).17 Although some practitioners do not like the alternative work settings, many find the greater independence, professional team orientation, creativity, and higher level of patient and family interaction quite rewarding. In addition, most RTs working in the alternative care environment argue that only in these settings is their full scope of training really used.
TABLE 51-1
| Area | Traditional Setting (Acute Care Hospital) | Alternative Settings (Long-Term Acute Care, Subacute, Home Care) |
| Diagnostic resources | In-house laboratory, x-ray, ABG analysis, PFT | Must rely on outside vendors to provide diagnostic tests |
| Equipment support | Extensive; supported by piped-in O2 and suctioning | Limited availability; must use portable O2 and suctioning systems |
| Travel requirements | None; remain in one facility | Must travel between facilities or residences |
| Level of supervision | Direct supervision | Respiratory care provider works independently with minimal supervision |
| Patient assessment | Moderate—primarily provided by attending physician or residents | Heavy—core responsibility related to care planning |
| Documentation requirements | Moderate—limited to medical recordkeeping | Heavy—includes initial justification, ongoing follow-up, and often detailed financial recordkeeping |
| Work schedule | Specific hours | Varied work schedule, often including “on-call” off hours coverage |
| Time constraints | More than one shift to deliver therapy | Must complete all therapy during shift or visit |
| Patient-family interaction | Limited treatment time available; little family interaction | One-on-one therapy; intensive family interaction |
| Provider interaction | Primarily attending physicians and patient’s nurses | Continuous interaction with all members of professional team |
Discharge Planning
Effective discharge planning provides the foundation for quality care in the alternative care setting. A properly designed and implemented discharge plan guides the multidisciplinary team in successfully transferring a respiratory care patient from the health care facility to an alternative site of care.18 Effective implementation of the discharge plan also ensures the safety and efficacy of the patient’s continuing care.
To guide practitioners in providing quality care, the AARC has published Clinical Practice Guideline: Discharge Planning for the Respiratory Care Patient.19 Excerpts from this guideline appear in Clinical Practice Guideline 51-1.
Multidisciplinary Team
Although a physician normally initiates an order to discharge a patient to an alternative site, many other health care professionals are involved in the discharge process. Table 51-2 identifies these key professionals and their major responsibilities.18 As with pulmonary rehabilitation (see Chapter 50), a team approach produces the best patient results. Communication and mutual respect for the talents and abilities of each team member are two key elements in making patient care in the alternative care setting work. Any breakdown in the system may delay or adversely affect patient discharge and the patient’s physical health and mental well-being.
TABLE 51-2
Members of Patient Care Team in Alternative Settings
| Discipline | Responsibilities |
| Utilization review | Advises or recommends consideration of patient discharge. Documents patient’s in-hospital care |
| Discharge planning (social service or community or public health) | Brings all the needed elements together and ensures that a patient can be discharged to alternative care sites. Makes contacts with outside agencies that may assist with patient care |
| Physician | Writes order for patient discharge. Evaluates patient’s condition and prescribes needed care. Establishes therapeutic objectives |
| Respiratory care | Evaluates patient and recommends appropriate respiratory care. Provides care and follow-up |
| Nursing | Writes and implements nursing care plan for patient. Assesses patient’s status and provides necessary follow-up |
| Dietary and nutrition | Assesses patient’s nutritional needs and writes dietary plan for patient. Makes arrangements for meals as necessary |
| Physical and occupational therapy | Provides necessary physical therapy and recommends any additional modalities or procedures |
| Psychiatry or psychology | Assesses patient’s emotional status and provides any needed counseling or support |
| DME supplier or home care company | Provides needed equipment and supplies and handles any emergency situations involving delivery or equipment operation |
Site and Support Service Evaluation
The primary factors determining the appropriate site for discharge are the goals and needs of the patient. These goals and needs should be met in an optimal and cost-effective manner using the resources available at the proposed site. In terms of institutional personnel, the staff of the selected facility must have all the competencies required to meet the patient’s respiratory needs, be able to provide other needed health care services (e.g., physical therapy), and provide adequate 24-hour coverage.17,19
For discharge to the home, it is essential that the ability of caregivers to learn and perform the required care be evaluated before transfer. Caregivers must clearly demonstrate and have documented the competencies required to care for the specific patient and, in combination, provide 24-hour coverage.17,19
• Service 24 hours, 7 days a week
• Third-party insurance processing
When selecting a DME supplier from the available choices, the patient and family members and other members of the discharge planning team should consider the company’s accreditation status, cost and scope of services, dependability, location, personnel, past track record, and availability. To help ensure a basic level of quality, one should select a DME supplier that is accredited. In addition, the service should be problem-free and provided by reliable, experienced, professional, and courteous staff. Charges should be reasonable and competitive, and clinical respiratory services should be provided by credentialed RTs.17
Finally, the selected site must meet basic safety standards and be suitable for managing the patient’s specific condition. It should be free of fire, health, and safety hazards; provide adequate heating, cooling, and ventilation; provide adequate electrical service; and provide for patient access and mobility with adequate patient space (room to house medical and adaptive equipment) and storage facilities. The selected site must be capable of operating, maintaining, and supporting all equipment needed by the patient; including both respiratory and ancillary equipment and supplies as needed, such as the ventilator, suction, O2, intravenous therapy, nutritional therapy, and adaptive equipment.17,19 Box 51-1 lists key factors one should assess in planning the discharge of a respiratory care patient to the home environment.
Oxygen Therapy in Alternative Settings
O2 therapy is the most common mode of respiratory care in alternative care settings. This high use is based on the fact that O2 therapy improves both survival and quality of life in selected patient groups, especially patients with advanced COPD.20,21 In particular, studies have shown improved nocturnal O2 saturation, reduced pulmonary artery pressure, and lower pulmonary vascular resistance with appropriate outpatient O2 therapy.22,23
To guide practitioners in providing quality care, the AARC has published a Practice Guideline on Oxygen Therapy in the Home or Extended Care Facility.24 Excerpts from the AARC guideline, including the indications, contraindications, precautions and possible complications, method, assessment of need, assessment of outcome, and monitoring, appear in Clinical Practice Guideline 51-2.
Oxygen Therapy Prescription
As indicated in Clinical Practice Guideline 51-2, O2 prescriptions must be based on documented hypoxemia, as determined by either arterial blood gas analysis or oximetry. Prescriptions for O2 therapy no longer can be based simply on patient diagnosis or signs and symptoms. In addition, as-needed O2 therapy is no longer acceptable in the alternative care setting.
When the need for O2 therapy is established, the physician writes a prescription. A prescription for O2 therapy in the alternative care setting must include the following elements:25
• Flow rate in L/min or concentration or both
• Frequency of use in hours per day and minutes per hour (if applicable)
• Diagnosis (severe primary lung disease, secondary conditions related to lung disease and hypoxia, related conditions or symptoms that may improve with O2)
• Laboratory evidence (arterial blood gas analysis or oximetry under the appropriate testing conditions); home care companies cannot provide this testing
• Additional medical documentation (no acceptable alternatives to home O2 therapy)
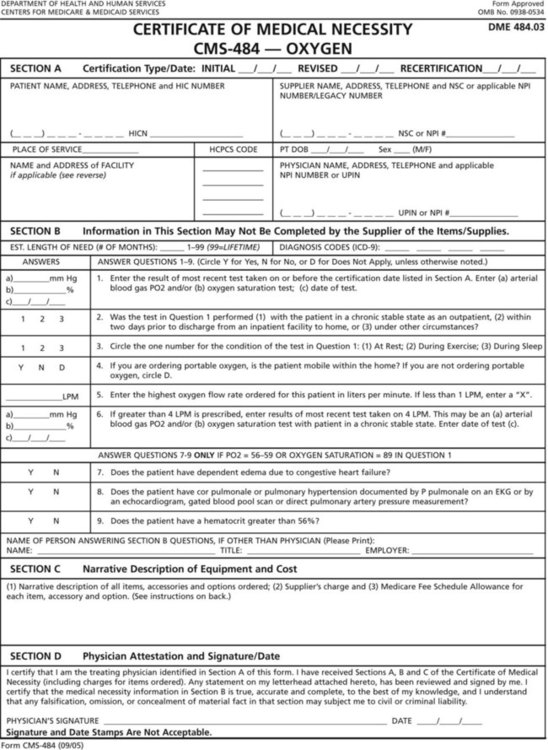
For home use, the ordering physician must authorize O2 therapy using the CMS Certification of Medical Necessity form for O2 (Figure 51-1). After the need for long-term therapy is documented, repeat arterial blood gas analysis or SpO2 measurements are not needed. However, blood O2 levels may still be measured when the need arises to assess changes in the patient’s condition.26
Supply Methods
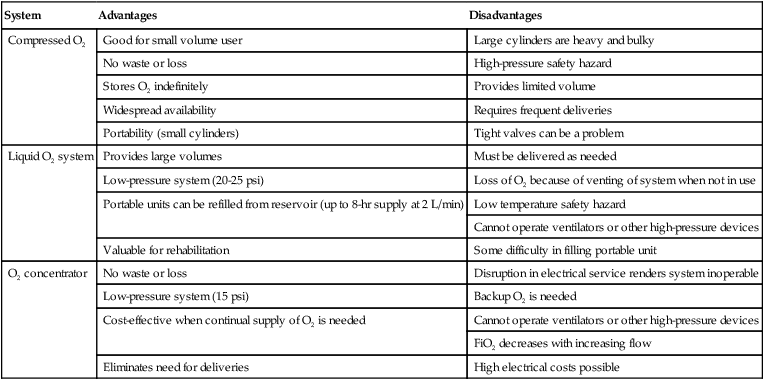
Most alternative care sites do not have bulk O2 storage or delivery systems. In these settings, O2 normally is supplied from one of the following three sources:27 (1) compressed O2 cylinders, (2) liquid O2 systems, or (3) O2 concentrators. Table 51-3 summarizes the major advantages and disadvantages of each system.
TABLE 51-3
Advantages and Disadvantages of Major Alternative Oxygen Supply Systems
| System | Advantages | Disadvantages |
| Compressed O2 | Good for small volume user | Large cylinders are heavy and bulky |
| No waste or loss | High-pressure safety hazard | |
| Stores O2 indefinitely | Provides limited volume | |
| Widespread availability | Requires frequent deliveries | |
| Portability (small cylinders) | Tight valves can be a problem | |
| Liquid O2 system | Provides large volumes | Must be delivered as needed |
| Low-pressure system (20-25 psi) | Loss of O2 because of venting of system when not in use | |
| Portable units can be refilled from reservoir (up to 8-hr supply at 2 L/min) | Low temperature safety hazard | |
| Cannot operate ventilators or other high-pressure devices | ||
| Valuable for rehabilitation | Some difficulty in filling portable unit | |
| O2 concentrator | No waste or loss | Disruption in electrical service renders system inoperable |
| Low-pressure system (15 psi) | Backup O2 is needed | |
| Cost-effective when continual supply of O2 is needed | Cannot operate ventilators or other high-pressure devices | |
| FiO2 decreases with increasing flow | ||
| Eliminates need for deliveries | High electrical costs possible |
Compressed Oxygen Cylinders
The primary use of compressed O2 cylinders in alternative settings is either for ambulation (small cylinders) or as a backup to liquid or concentrator supply systems (H/K cylinders). Safety measures for cylinder O2 are the same as those discussed in Chapters 37 and 38. For home use, the RT should thoroughly review these safety measures with both the patient and family members. After instruction, the RT should always confirm and document abilities of caregivers to use the delivery system safely.
In addition to the cylinder gas, a pressure-reducing valve with flowmeter is needed to deliver O2 at the prescribed flow. Standard clinical flowmeters deliver flows up to 15 L/min; flows used in alternative settings are typically in the 0.25 to 5 L/min range. For this reason, the RT should select a calibrated low-flow flowmeter whenever possible. Alternatively, a preset flow restrictor can be used (see Chapter 37).
As in the hospital, there is usually no need to humidify nasal O2 at flows of 4 L/min or less.24 If humidification is needed, a simple unheated bubble humidifier can be used. Because the mineral content of tap water may be high (hard water), water used in these humidifiers should be distilled. Otherwise, the porous diffusing element may become occluded. Although complete blockage is unlikely, occlusion of the diffusing element can impair humidification and alter flow.
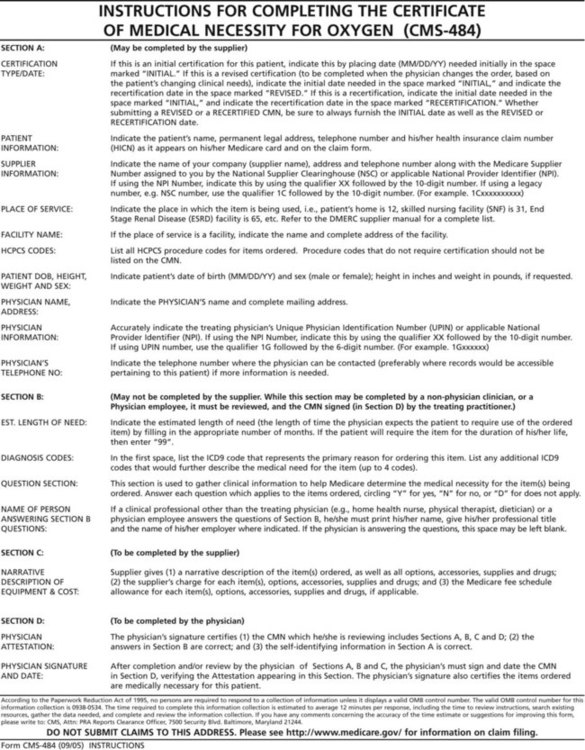
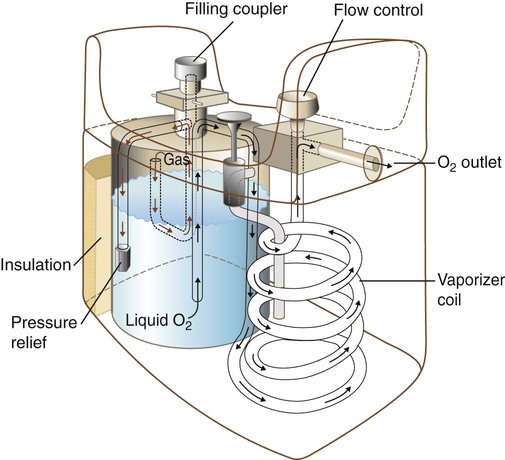
Liquid Oxygen Systems
Because 1 cubic ft of liquid O2 equals 860 cubic ft of gas, liquid O2 systems can store large quantities of O2 in small spaces; this is ideal for the high-volume user. As shown in Figure 51-2, a typical personal liquid O2 system is a miniature version of a hospital stand tank. Similar to its larger counterpart, this system consists of a reservoir unit similar in design to a thermos bottle. The inner container of liquid O2 is suspended in an outer container, with a vacuum in between. The liquid O2 is kept at approximately −300° F. Because of constant vaporization, gaseous O2 always exists above the liquid. When the cylinder is not in use, this vaporization maintains pressures between 20 psi and 25 psi. When pressures increase above this level, gas vents out the pressure relief valve.
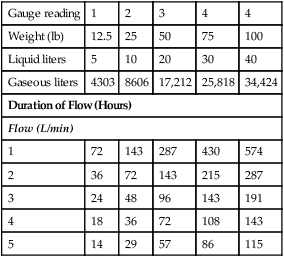
To help avoid these computations, many manufacturers provide simple conversion charts. Table 51-4 is an example of a conversion chart for a typical 100-lb personal liquid O2 system.
TABLE 51-4
Conversion Chart for Computing Duration of Flow for 100-lb (40-L) Liquid Oxygen Reservoir
| Gauge reading | 1 | 2 | 3 | 4 | 4 |
| Weight (lb) | 12.5 | 25 | 50 | 75 | 100 |
| Liquid liters | 5 | 10 | 20 | 30 | 40 |
| Gaseous liters | 4303 | 8606 | 17,212 | 25,818 | 34,424 |
| Duration of Flow (Hours) | |||||
| Flow (L/min) | |||||
| 1 | 72 | 143 | 287 | 430 | 574 |
| 2 | 36 | 72 | 143 | 215 | 287 |
| 3 | 24 | 48 | 96 | 143 | 191 |
| 4 | 18 | 36 | 72 | 108 | 143 |
| 5 | 14 | 29 | 57 | 86 | 115 |
Many personal liquid O2 systems also come with smaller portable units (Figure 51-3). This system is ideal for an ambulatory patient who is capable of physical activity. Typical portable units weigh 5 to 14 lb and can be refilled directly from the stationary reservoir. Most portable units come with a carrying case or small cart and can provide 5 to 8 hours of O2 at a flow of 2 L/min. Either an adjustable flow restrictor or a Bourdon-type gauge is used to meter flow, with a weight gauge used to indicate O2 contents. The functional use time of portable liquid O2 units can be extended with O2-conserving devices, including the demand-flow systems discussed later in this chapter.
Because of the extremely low temperature of liquid O2, patients and caregivers must be extremely careful when refilling these portable systems. Box 51-2 lists the steps needed to fill a portable liquid O2 unit from a reservoir.27 The procedure takes approximately 1 to 2 minutes, depending on the size of the portable tank. Wearing gloves can help prevent liquid O2 skin burns.
Oxygen Concentrators
An O2 concentrator is an electrically powered device that physically separates the O2 in room air from nitrogen. The most common type of concentrator uses a molecular sieve to extract O2.27 Concentrators using membrane technology also exist, but they are not in common use.
The molecular sieve concentrator uses a pump to compress and deliver filtered room air to one of two sets of sieves (Figure 51-4). These sieves contain sodium-aluminum silicate pellets that absorb nitrogen, carbon dioxide (CO2), and water vapor. To remove these unwanted gases from the pellets, an automatic pressure swing cycle switches back and forth between the sieve sets. One set is pressurized to produce O2, and the other is depressurized to purge nitrogen, CO2, and water vapor.
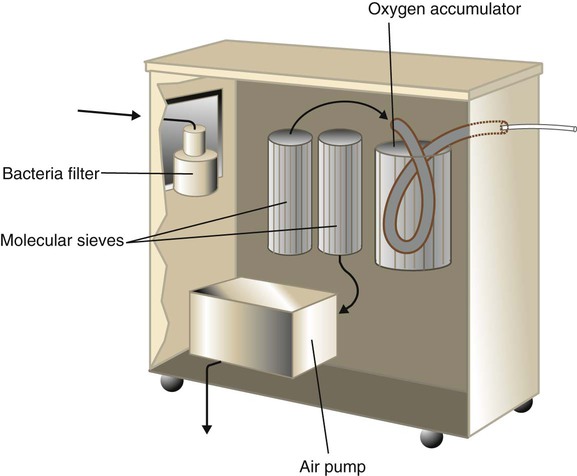
Gas leaving the sieves is stored in a small accumulator. At flows of 1 to 2 L/min, the typical molecular sieve concentrator provides between 92% and 95% O2. At 5 L/min or greater, O2 concentrations are between 85% and 93%.27 The output of many concentrator models has been limited to 5 L/min. However, more recently, models capable of delivering 10 L/min, such as the Respironics Millennium M10 (Phillips-Respironics, Murrysville, PA) have been introduced. In addition, technologic advances have accounted for other enhancements to O2 production and delivery devices in alternative care settings. One such device is the Inogen One G2 System (Inogen Inc., Goleta, CA), which is a portable battery-powered concentrator with demand-flow conserving capabilities. The Inogen unit affords patients receiving low-flow O2 increased mobility and has been approved for use in most commercial aircraft.
Problem Solving and Troubleshooting
Technical problems with O2 supply systems in alternative settings are similar to problems encountered in the acute care hospital (see Chapter 37). In addition to these technical problems, situations can arise when patients or caregivers fail to follow instructions properly or respond as needed to simple incidents. To avoid communication problems, verbal instructions should always be reinforced by providing simple written instructions for subsequent reference. In addition, the clinician should always confirm and document the ability of caregivers to use the delivery system safely, including how to troubleshoot simple problems. The ability of caregivers and patients to give an adequate return demonstration on proper equipment usage should also be recorded.24
To avoid problems before they occur, the patient or caregiver should be instructed to check all O2 delivery equipment at least once a day.18 The proper function of all equipment, including liter flow and connections, should also be confirmed. In addition, the remaining liquid or compressed gas content of the supply system should be checked. Last, concentrator air inlet filters must be cleaned weekly. In the home setting, providing the patient or caregiver with a simple checklist form can help ensure that these important tasks are performed regularly.
Possible physical hazards to patients and caregivers include unsecured cylinders, ungrounded equipment, mishandling of liquid (resulting in burns), and fire.24 Careful preliminary instruction, followed by ongoing assessment of the environment, can help minimize these problems. Bacterial contamination of nebulizer or humidification systems is another potential problem.24 Infection control procedures designed to minimize this problem are discussed in detail on p. 1336.
Inaccurate O2 flows or concentrations can also occur. Accurate flow output of O2 systems should be confirmed by the supplier (using calibrated laboratory meters) before equipment is placed in alternative settings.28 In the home, O2 concentrator fractional inspired oxygen (FiO2) levels should be checked and confirmed as part of a routine monthly maintenance visit.29 Routine maintenance of these devices should include cleaning and replacing filters, checking the alarm system, and confirming FiO2 levels using either the unit’s O2 sensor or a separate calibrated O2 analyzer. If the concentration is less than the manufacturer’s specification at the given flow, the pellet canisters are probably exhausted and should be replaced.
Delivery Methods
The performance characteristics, advantages, and disadvantages of transtracheal O2 catheters and reservoir cannulas are described in detail in Chapter 38. We focus here on the application of the transtracheal O2 catheter and the technical aspects of demand-flow systems.
Transtracheal Oxygen Therapy
Transtracheal oxygen therapy (TTOT) is O2 delivered via a catheter with a small orifice that is inserted through the skin and neck tissue into the trachea. Although uncommon, this delivery method offers advantages of improved cosmetic appearance and lower flows to achieve the same therapeutic effect. However, not all patients requiring long-term O2 therapy are good candidates for TTOT. TTOT is indicated only for patients who meet one or more of the following criteria: (1) cannot be adequately oxygenated with standard approaches, (2) do not comply well when using other devices, (3) exhibit complications from nasal cannula use, (4) prefer TTOT for cosmetic reasons, and (5) have need for increased mobility.30 TTOT may also be a treatment alternative for some patients with sleep apnea when nasal continuous positive airway pressure (CPAP) is not tolerated or when combined O2 and nasal CPAP are required.
As with most modalities in alternative care settings, the success of TTOT depends mainly on effective patient education and ongoing self-care with professional follow-up. Key patient responsibilities include routine catheter cleaning and recognizing and troubleshooting common problems. Box 51-3 describes key self-care guidelines for patients with transtracheal O2 catheters.
Demand-Flow Oxygen Systems
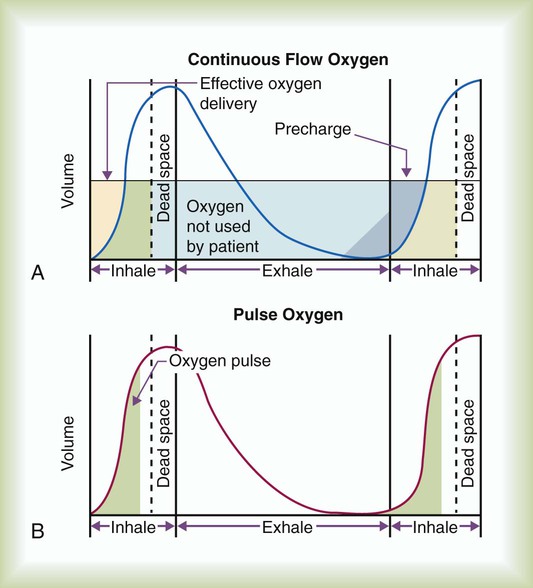
A demand-flow O2 delivery device, also known as a pulsed-dose O2-conserving device, uses a flow sensor and valve to synchronize gas delivery with the beginning of inspiration.31 As indicated in Figure 51-5, A, with continuous O2 flow, most of the effective O2 delivery occurs during the first half of inspiration. All the O2 delivered during the latter half of inspiration and throughout most of expiration is wasted. Figure 51-5, B, shows the effect of a synchronized pulse of O2 delivered at the beginning of inspiration. Ideally, this O2 pulse should occur during the first quarter of inspiration. Under these conditions, a pulsed O2 system can produce SaO2 levels equal to levels seen with continuous flow, while using 60% less O2.32
In theory, demand-flow O2 systems provide the greatest savings in O2 use for a given level of arterial saturation. In addition, there is generally no need for humidification. Demand-flow systems also have been successfully adapted for use with transtracheal catheters, resulting in even more efficient O2 delivery. Current Medicare reimbursement guidelines provide no significant additional payments to cover the additional cost of demand delivery systems. Also, some patients receiving demand-flow O2 desaturate during exercise.31,33
Problem Solving and Troubleshooting
Most problems with long-term O2 delivery systems are related to people. Patients and caregivers often fail to follow instructions or comply with the prescribed therapeutic or maintenance regimen.24 Generally, caregivers should be allowed to operate and maintain O2 delivery devices only after they have been instructed by credentialed RTs and have demonstrated the appropriate level of skill. In no case should the patient or caregiver be allowed or instructed to alter flow settings. Instead, when in doubt, they should be taught to switch to the backup supply at the same liter flow.
The most common complications of TTOT are listed in Box 51-4. Although these problems occur infrequently, the clinician must be on constant guard for their occurrence. In particular, the RT should immediately report any evidence of tract tenderness, fever, excessive cough, increased dyspnea, or subcutaneous emphysema to the patient’s physician.
Because transtracheal catheters are normally used with humidifiers, the clinician also must be prepared to troubleshoot this equipment. Guidelines for dealing with leaks and obstructions in O2 delivery systems using humidifiers are provided in Chapter 35. Given the small bore of transtracheal catheters, the clinician should generally use a humidifier with a high-pressure (2 psi) relief valve; otherwise, the pop-off constantly sounds. As previously discussed, distilled water is satisfactory for airway humidification in alternative settings.
Similarly, there can be problems with the use of demand-flow or pulsed-dose O2-conserving systems. Although improvements to these devices have significantly increased their use, these units tend to add to the weight of portable setups, and they can easily be damaged. These and other potential problems with demand-flow O2 delivery systems are listed in Box 51-5.33
Ventilatory Support in Alternative Settings
Providing successful ventilatory support outside the acute care hospital requires careful patient selection and good discharge planning.34 Key factors include an interdisciplinary team approach, effective caregiver and family education, thorough assessment and preparation of the environment, and careful selection of needed equipment and supplies. Properly planned ventilatory support delivered in alternative settings can provide major benefits for both the patient and family, with substantial savings in health care costs.35
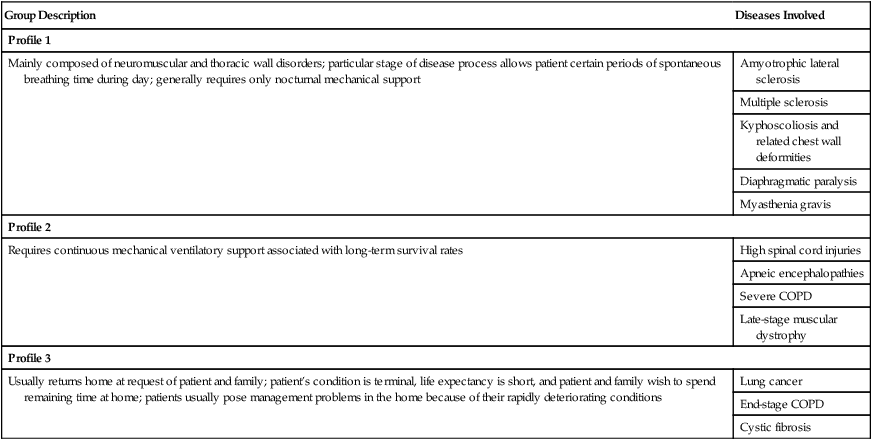
Patient Selection
Most patients needing ventilatory support outside the acute care hospital fall into one of the following three broad categories:36
1. Patients unable to maintain adequate ventilation over prolonged periods (in particular, noninvasive nocturnal or intermittent use)
2. Patients requiring continuous mechanical ventilation for long-term survival
3. Patients who are terminally ill with short life expectancies
Table 51-5 provides more detailed profiles of these patient groups. In addition to adults, a growing number of ventilator-assisted children are being managed in alternative settings. The same basic principles of discharge planning and patient care for adult patients should be followed for ventilator-assisted children.37
TABLE 51-5
Profiles of Patient Groups Requiring Ventilatory Support in Alternative Settings
| Group Description | Diseases Involved |
| Profile 1 | |
| Mainly composed of neuromuscular and thoracic wall disorders; particular stage of disease process allows patient certain periods of spontaneous breathing time during day; generally requires only nocturnal mechanical support | Amyotrophic lateral sclerosis |
| Multiple sclerosis | |
| Kyphoscoliosis and related chest wall deformities | |
| Diaphragmatic paralysis | |
| Myasthenia gravis | |
| Profile 2 | |
| Requires continuous mechanical ventilatory support associated with long-term survival rates | High spinal cord injuries |
| Apneic encephalopathies | |
| Severe COPD | |
| Late-stage muscular dystrophy | |
| Profile 3 | |
| Usually returns home at request of patient and family; patient’s condition is terminal, life expectancy is short, and patient and family wish to spend remaining time at home; patients usually pose management problems in the home because of their rapidly deteriorating conditions | Lung cancer |
| End-stage COPD | |
| Cystic fibrosis | |
Regardless of diagnosis, patients being considered for ventilatory support in alternative settings must be medically and psychologically stable. In regard to assessing patient stability, Box 51-6 outlines the criteria developed by the American College of Chest Physicians (ACCP).38
Settings and Approaches
The most common setting for ventilatory support outside the acute care hospital is the home. Additional sites include LTACHs and long-term care facilities, including specialized long-term units designed specifically for ventilator patients.38,39
Based on individual evaluation of patient need, one of the following two major support approaches may be considered: (1) invasive or (2) noninvasive support. In alternative settings, invasive ventilatory support always involves application of positive pressure ventilation by tracheotomy. Noninvasive approaches include positive pressure and negative pressure ventilation via an intact upper airway or abdominal displacement methods.40,41
Standards and Guidelines
Standards and guidelines for ventilatory support outside the acute care hospital continue to evolve. In the late 1980s, both the ACCP and the AARC developed and published recommendations for the care of ventilator-assisted individuals in the home and alternative care sites.38,42 More recently, the AARC developed a clinical practice guideline on long-term invasive mechanical ventilation in the home.43 Excerpts from these guidelines appear in Clinical Practice Guideline 51-3.
Special Challenges in Providing Home Ventilatory Support
Prerequisites
For home ventilatory support to be successful, several prerequisites must be met, including the following:44
• Willingness of family to accept responsibility
• Adequacy of family and professional support
In regard to the home setting, the same factors listed in Box 51-1 should be evaluated for patients being considered for home ventilatory support.
Planning
1. Family is consulted regarding feasibility.
2. Physician writes appropriate orders.
3. Discharge planner coordinates efforts of team members and discharge plan is formulated.
4. Physician and other team members discuss plan with family and caregivers.
5. Education and training are initiated and completed.
6. Patient and family are prepared for discharge.
7. Home layout is assessed with necessary changes made.
8. Equipment and supplies are readied.
9. Discharge planner meets with team and makes final preparations.
10. Patient is discharged (with trial period, if necessary).
11. Local power company is notified regarding the presence of life-support equipment; appropriate backup power (battery or compressed gas source) is made available.
12. Ongoing and follow-up care is provided by visiting nurse, RT, and other health care professionals (as necessary).
Caregiver Education
To prepare patients, family members, and other caregivers properly for home discharge, a comprehensive educational program must be undertaken and completed. Essential skills that must be taught include the following:34
• Airway management, including tracheostomy and stoma care, cuff care, suctioning, cough-assist, changing artificial airways or ties
• Chest physical therapy techniques, including percussion, vibration, and coughing
• Medication administration, including oral and aerosol
• Patient movement and ambulation
All caregivers should successfully complete this educational process. The specific time frame varies depending on caregiver ability and availability for training sessions. Training generally requires a minimum of 1 to 2 weeks, over which time several education sessions can take place and cover instruction, demonstration, caregiver practice, and evaluation. Caregivers should be strongly encouraged to complete a course in basic life support, such as offered by the American Heart Association, before the patient is discharged. Ideally, the patient should have a trial period on the actual home ventilator before discharge. In the early stages after discharge, patient follow-up by an RT likely should occur every day. As patient and caregivers become more familiar with the equipment and procedures, follow-up visits generally decrease to about once per month.45,46
Invasive versus Noninvasive Ventilatory Support
Until more recently, invasive positive pressure ventilation by tracheostomy was the default standard for long-term mechanical ventilation, especially for patients requiring 24-hour support. However, long-term tracheostomy is associated with many serious complications, including secretion retention, infection, aspiration, and ventilator-associated pneumonia. In addition, a permanent tracheostomy poses significant communication problems between caregivers and patients. Because many long-term care facilities treat a tracheostomy as an open wound, patient placement at certain sites is prohibited.47 Last, invasive ventilation by tracheostomy poses significant limits on the patient’s quality of life. For these reasons, noninvasive support is becoming increasingly popular. Noninvasive ventilatory support involves any method designed to augment alveolar ventilation without an endotracheal airway. Noninvasive ventilation (NIV) is usually the first choice. Any individual requiring mechanical ventilation can be supported with NIV if the following conditions are met:47
• The patient is mentally competent, cooperative, and not using heavy sedation or narcotics.
• Supplemental O2 therapy is generally minimal (FiO2 ≤ 40%).
• SaO2 can be maintained at greater than 90% by aggressive airway clearance techniques.
• Bulbar muscle function is adequate for swallowing without potentially dangerous aspiration.
• No history exists of substance abuse or uncontrollable seizures.
• Unassisted or manually assisted peak expiratory flows during coughing exceed about 3 L/sec.
• No conditions are present that interfere with NIV interfaces (e.g., facial trauma, inadequate bite for mouthpiece, presence of orogastric or nasogastric tube, or facial hair that can hamper an airtight seal).
Patients who can benefit from NIV generally fall into one of two categories.48 Patients in the first category have conditions in which cessation of ventilation could lead to imminent death. This category includes both acutely ill patients (patients with asthma, acute exacerbation of COPD, or pulmonary edema) and patients requiring long-term, 24-hour support (some patients with quadriplegia or patients with certain neuromuscular disorders). Patients in the second category have conditions in which NIV may offer clinical benefit, but cessation is not life-threatening. These patients generally require only intermittent or nocturnal support. Patients in this category include patients with chronic neuromuscular and chest wall diseases, such as muscular dystrophy and kyphoscoliosis. The application of long-term NIV for patients with obstructive disorders such as end-stage COPD or cystic fibrosis is less well documented, although some favorable results have been reported.48 Relative contraindications to NIV include severe upper airway dysfunction, copious secretions that cannot be cleared by spontaneous or assisted cough, and O2 concentration requirements exceeding 40%.48
Previously popular in alternative settings, negative pressure ventilation is now considered a second-line strategy for noninvasive ventilatory support. Compared with NIV, negative pressure ventilation is harder to apply, more cumbersome, and less well tolerated (because of poor breath synchronization). Negative pressure ventilation tends to limit patient mobility and can worsen upper airway obstruction in susceptible patients. Nonetheless, negative pressure ventilation may be appropriate in patients who are unable to use NIV or who have failed NIV trials.41 Negative pressure ventilation may also be considered for patients who require frequent airway access for suctioning or patients with severe nasal congestion.47
Equipment
Box 51-7 lists the essential equipment and supplies needed for ventilator-dependent patients in alternative settings.34,37
Selecting Appropriate Ventilator
The choice of ventilator for a patient in an alternative care setting should be based on the patient’s clinical need and the available support resources. In some cases, patient needs may dictate that more than one ventilator be provided.43 A second backup ventilator should be provided for patients who cannot maintain spontaneous ventilation for more than 4 consecutive hours, for patients living in an area where a replacement ventilator cannot be secured within about 2 hours, and for patients whose care plan requires mechanical ventilation during mobility.48
If invasive ventilation by tracheostomy is the selected approach, the best choice is a positive pressure ventilator. The invasive route also requires a humidification system, preferably a servo-controlled heated humidifier with alarms. Patients with a tracheostomy without retained secretions may use a heat and moisture exchanger during transport or to enhance their mobility.43 For patients with an intact upper airway, a device capable of NIV is the first choice, unless contraindicated (Box 51-8 lists the absolute contraindications against using NIV).49 In patients with an intact upper airway for whom NIV is contraindicated or unsuccessful, a negative pressure ventilator may be considered.
Positive Pressure Ventilators
Table 51-6 lists the essential, recommended, and optional features of positive pressure ventilators used in alternative care settings. An essential feature is basic to safe and effective operation in most patient care settings. A recommended feature helps provide optimal patient management. An optional feature is possibly useful in limited situations but not needed for most patients.42,50
TABLE 51-6
| Feature | Necessity |
| Positive pressure tidal breaths | Essential |
| Mandatory rate | Essential |
| Flow or inspiratory-to-expiratory or inspiratory time | Recommended* |
| Expiratory pressure (PEEP) | Optional |
| FiO2 to 1 | Optional |
| Patient spontaneous breath (e.g., CPAP, intermittent mandatory ventilation) | Optional |
| Breath-triggering mechanism (flow or pressure sensors to initiate ventilator breath) | Recommended* |
| Flow-timing interaction (e.g., pressure support) | Optional |
| Feedback control (e.g., mandatory minute ventilation) | Optional |
*Essential if the patient has intact ventilatory drive and respiratory muscles or if the possibility of partial or complete ventilator independence is anticipated.
As shown in Figure 51-6, there are many new positive pressure ventilators designed for use in alternative settings. These ventilators can be used on adults or pediatric patients weighing at least 5 kg. Some are approximately the size and weight of a laptop computer and have many of the capabilities of much larger mechanical ventilators used in alternative sites and in acute care. These new ventilators offer ventilator-dependent patients the advantages of greater mobility and space conservation. Many of these models also offer pressure support to augment spontaneous breaths and can provide positive end expiratory pressure (PEEP) without having to add an adapter to the ventilator circuit.51–53

Many new positive pressure ventilators designed for alternative care settings (Figure 51-7; see Figure 51-6) have an internal battery, which can provide 6 hours of use should AC line power fail. For longer periods of use away from AC line power, many of these devices can run for 10 to 12 hours using a 12-V deep-cell (marine) battery.

Additionally, time-triggered or patient-triggered, pressure-limited, flow-cycled devices (pressure support with timed backup) have been successfully applied in alternative settings.41,54,55 Many units are currently available (Figure 51-8) that are specifically designed to provide this type of support, usually noninvasively by nasal or oronasal (full-face) masks.41,56,57
Any existing positive pressure ventilator essentially can be used to provide NIV.48,58 Many patients, especially patients with COPD, prefer pressure-limited over volume-cycled ventilation. However, patients with neuromuscular or neurologic disorders often favor the consistent high inflations provided by volume ventilation, which enhance coughing and phonation. In addition, the alarm capabilities and internal battery backup provided with current portable volume ventilators make them the best choice for patients who cannot sustain any spontaneous breathing.56
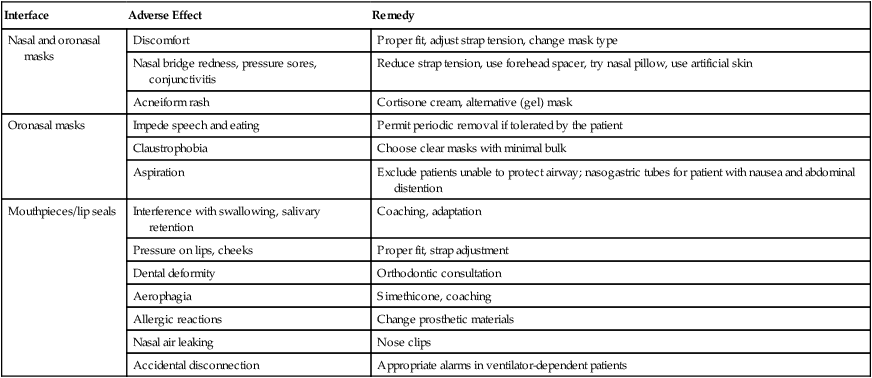
The biggest challenge with NIV is not selecting the right ventilator but getting a good, comfortable, minimal leak interface. Interfaces commonly found in alternative care settings include oronasal (full-face) masks; nasal masks; nasal “pillows”; and simple, flanged, or custom mouthpieces. For long-term use, some patients prefer alternating between devices. A patient may prefer a simple mouthpiece for easy accessibility during the day, with a nasal mask providing support at night.48 Table 51-7 summarizes common problems associated with NIV interfaces and how to correct them.41,59
TABLE 51-7
Adverse Effects of Noninvasive Ventilation Interfaces and Possible Corrective Actions
| Interface | Adverse Effect | Remedy |
| Nasal and oronasal masks | Discomfort | Proper fit, adjust strap tension, change mask type |
| Nasal bridge redness, pressure sores, conjunctivitis | Reduce strap tension, use forehead spacer, try nasal pillow, use artificial skin | |
| Acneiform rash | Cortisone cream, alternative (gel) mask | |
| Oronasal masks | Impede speech and eating | Permit periodic removal if tolerated by the patient |
| Claustrophobia | Choose clear masks with minimal bulk | |
| Aspiration | Exclude patients unable to protect airway; nasogastric tubes for patient with nausea and abdominal distention | |
| Mouthpieces/lip seals | Interference with swallowing, salivary retention | Coaching, adaptation |
| Pressure on lips, cheeks | Proper fit, strap adjustment | |
| Dental deformity | Orthodontic consultation | |
| Aerophagia | Simethicone, coaching | |
| Allergic reactions | Change prosthetic materials | |
| Nasal air leaking | Nose clips | |
| Accidental disconnection | Appropriate alarms in ventilator-dependent patients |
All positive-pressure ventilators used in alternative settings must have an alarm to indicate loss of power (pneumatic or electrical). Portable volume-cycled ventilators should also incorporate a high-pressure alarm or cycle override. For patients with conditions in which cessation of ventilation would cause death, a patient-disconnect alarm (low-pressure or low-exhaled volume) must be provided.43,48 In some settings, a remote alarm or secondary disconnect alarm, or both, may be needed. A secondary alarm may be based on chest wall impedance and cardiac activity, exhaled volume, end-tidal CO2, or pulse oximetry with alarm capabilities.43 For patients in alternative settings who require only intermittent NIV, a loss of power alarm is generally sufficient.48
Negative Pressure Ventilators
With the increased popularity of noninvasive and invasive positive pressure ventilation, negative pressure ventilators are rarely used for ventilatory support in alternative settings.41,60 The original negative pressure ventilator was the iron lung, used for patients needing ventilator assistance after poliomyelitis. For practical reasons, the cumbersome iron lung was essentially replaced by the chest cuirass and wrap or “pneumosuit.”
The chest cuirass (a rigid shell) and wrap-type systems (nylon fabric surrounding a semicylindrical tentlike support) are simply enclosures that allow application of negative pressure to the thorax. These devices require a separate electrically powered negative pressure generator. An example of a negative pressure generator used to power cuirass or wrap-type systems is the Philips-Respironics NEV-100 (Phillips-Respironics, Murrysville, PA).60
Evaluation and Follow-Up
Patient parameters to be monitored during positive pressure ventilation are essentially the same parameters that are assessed in the acute care setting, with an emphasis on simplicity.61 The caregiver should assess the patient’s vital signs, lung sounds, and sputum production on a daily basis; arterial blood gas analysis (by the RT) may be conducted monthly or only when changes in the care plan appear to be needed. Likewise, compliance and resistance measures are performed only when other evidence indicates the need.
Other Modes of Respiratory Care in Alternative Sites
Bland Aerosol Therapy
The delivery of bland aerosols has been common in alternative sites for many years. According to the AARC’s Clinical Practice Guideline, bland aerosol therapy includes the delivery of sterile water or various concentrations of saline solution in aerosol form.62 The aerosol can be produced by either an ultrasonic or jet (large volume) nebulizer. If using a jet nebulizer, a 50-psi air compressor is also required. Supplemental O2 is provided by either a concentrator or liquid supply system.
Depending on the patient’s condition and therapeutic objectives, bland aerosol therapy may be either continuous or intermittent. Historically, this approach was used for patients with tracheostomies because of their bypassed upper airway. Current knowledge suggests that bland aerosol therapy alone has little effect on the properties of mucus or its clearance.62 However, it may be useful as an adjunct to airway clearance procedures in patients who regularly produce large amounts of sputum.63
Aerosol Drug Administration
Most pulmonary drugs are available in either metered dose inhaler or dry powder inhaler form. Alternatively, the caregiver can use a small volume nebulizer powered by a low output diaphragm compressor.64 Guidelines on selecting the best delivery method for aerosolized drugs are discussed in Chapter 36. Regarding reimbursement for home use of small volume nebulizer or compressor systems, Medicare limits reimbursement by (1) requiring a certificate of medical necessity and (2) capping rental costs. Consequently, the reimbursable expenses related to aerosol drug administration in the home is quite limited.5
Airway Care and Clearance Methods
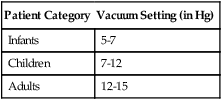
In most alternative care settings, tracheobronchial clearance is often accomplished by suctioning using a portable electrically powered suction pump with collection bottle and connection tubing. In accordance with the AARC Clinical Practice Guideline for suctioning of the patient at home, some patients may be taught to suction themselves. Proper suctioning procedures should also be taught to caregivers. Education and training on proper suctioning methods may begin before patient discharge from the acute care setting, with reinforcement and follow-up as needed.65 Because many of these systems measure pressure in inches of mercury (in Hg), care must be taken to teach proper adjustment according to patient age. Daily maintenance and cleaning are required. In an alternative care setting, a single suction catheter commonly may be used for 24 hours and then discarded. This measure helps control supply costs. To prevent bacterial growth, catheters are placed in a disinfecting solution such as hydrogen peroxide or 2.5% acetic acid between suctioning attempts.
Numerous methods are available for patients in an alternative care setting with an intact upper airway who need help with secretion clearance. These methods include both patient-independent and caregiver-dependent techniques.66 Patients can be taught to apply independently coughing, forced exhalation, active cycle of breathing, and autogenic drainage methods. Caregiver assistance is required with traditional postural drainage, percussion and vibration, and directed or assisted cough. Additional assistance can be provided by mechanical devices such as positive expiratory pressure mask, flutter valve, intrapulmonary percussive ventilator, and high-frequency chest compression vest, which are routinely used for patients with cystic fibrosis.
Another airway clearance method involves the use of cough-assist devices such as the Emerson mechanical inexsufflator, or “coughlator.” These devices have been on the market since the 1950s but have gained more widespread acceptance only more recently. The inexsufflator uses alternating positive and negative pressure as a form of lung expansion and airway clearance therapy. These devices can be especially effective with patients receiving NIV. The application of secretion clearance devices or techniques by nonprofessional caregivers should involve good preliminary instruction and ongoing follow-up by the RT working in any alternative site.66 See Chapter 33 for more in-depth discussion of the inexsufflator.
Nasal Continuous Positive Airway Pressure Therapy
Nasal CPAP therapy has become an accepted form of home care used to treat sleep apnea-hypopnea syndrome. For Medicare reimbursement of home nasal CPAP equipment, the diagnosis of sleep apnea must be confirmed by polysomnography, also known as a sleep study. With proper application and patient compliance, CPAP therapy can dramatically lessen or resolve the many problems associated with sleep apnea-hypopnea syndrome (morning headaches, daytime hypersomnolence, cognitive impairment). The patient’s quality of life can be enhanced, and the incidence of more severe complications, such as systemic and pulmonary hypertension and cor pulmonale, may be reduced.67
Equipment
A typical nasal CPAP apparatus consists of a flow generator capable of establishing varying levels of PEEP or CPAP, a circuit, and a patient interface (e.g., nasal mask, nasal pillows). One of the most common interfaces in alternative settings is the nasal mask (Figure 51-9). Most systems provide manually adjustable pressures in the range of 2.5 to 20 cm H2O. Many units now have a ramp feature that gradually increases the pressure to the prescribed level over a time interval. This feature helps some patients fall asleep and may increase therapy compliance.

A variation of nasal CPAP therapy is bilevel PAP. CPAP uses a single pressure level, whereas bilevel PAP uses two levels: (1) inspiratory positive airway pressure (IPAP) and (2) expiratory positive airway pressure (EPAP). In some patients, independent adjustment of IPAP and EPAP achieves the same results as conventional nasal CPAP therapy but at lower levels of expiratory pressure. In other patients, the difference in IPAP and EPAP aids the patient’s inspiratory effort, improving ventilation. In this respect, bilevel PAP may be used as a form of NIV for patients with ventilatory insufficiency. Bilevel PAP may also reduce the adverse effects associated with nasal CPAP therapy and improve patient tolerance.68
Determining Proper Continuous Positive Airway Pressure Level
CPAP units were developed more recently that automatically adjust the pressures to maintain airway patency, despite physiologic changes such as those affecting airway muscle tone or weight gain or loss. These self-titrating or auto-CPAP devices generally result in use of the lowest effective pressures and better patient compliance, while reducing the need for a sleep study and titration. As a result of such benefits, these devices are gaining widespread acceptance.69
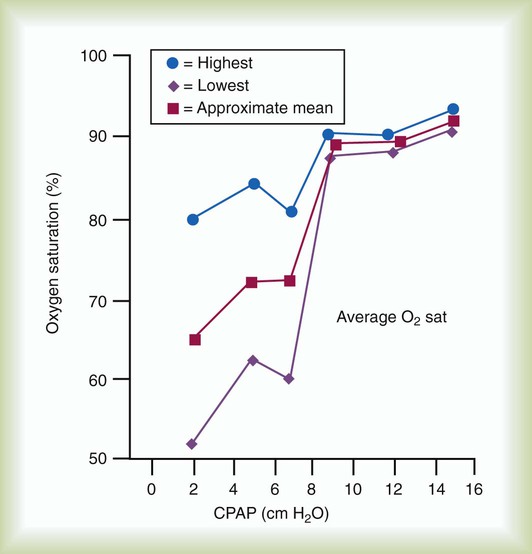
Alternatively, CPAP may be titrated against pulse oximetry data (Figure 51-10). In this case, the goal is to use the lowest CPAP that prevents arterial desaturation (SpO2 <90%).
Problem Solving and Troubleshooting
Conjunctivitis probably is the result of mask leakage around the bridge of the nose, which is easily corrected by ensuring a good seal in this area. Epistaxis and nasal discomfort are associated with drying of the nasal mucosa—a particular problem in cold, dry winter climates. Methods used to overcome excessive drying include in-line humidifiers, room vaporizers, chin straps (to decrease loss of upper airway moisture), and saline nasal sprays.70 Because none of these methods have proved satisfactory for all patients, selection should be based on individual patient acceptance and observed improvement in comfort. However, almost all patients receiving nocturnal CPAP therapy benefit from the addition of an in-line humidifier.
The most common problem with the CPAP apparatus is an inability to reach or maintain the set pressure. This problem is usually due to either inadequate flow or, more commonly, system leaks. Common causes of leaks include inappropriate patient interface (mask vs. nasal pillows) or pressure loss through an open mouth. As part of their initial training, patients and caregivers should be taught how to recognize and correct these common problems. Box 51-10 outlines the procedures patients or caregivers can use to troubleshoot inadequate flows and system leaks.71
Follow-up with patients soon after they begin CPAP therapy is important to resolve complications promptly. If left unresolved, these issues often discourage the patient and result in decreased compliance and a return of original symptoms.71
Apnea Monitoring
Apnea monitors alert clinicians and caregivers of certain life-threatening events, most notably recurrent apnea, bradycardia, and hypoxemia. At-risk infants are frequently set up on apnea monitors while they are in the hospital. After extensive family instruction in both equipment use and resuscitation, some of these infants may be discharged to the home with this equipment.72
Most apnea monitors detect both respirations and heart rate and activate audio and visual alarms when preset high or low limits are reached. Follow-up visits by the RT or a nurse are usually frequent at first but occur less often as the family becomes skilled with the equipment and monitoring routine. Some models record each alarm event and can be useful in monitoring the patient’s progress. The “memory” of such monitors generally requires periodic downloading during a follow-up visit or via a cable or telephone modem. Apnea monitors are usually discontinued after an infant has a negative pneumocardiogram (sleep study) or when recorded memory reveals no events during a prescribed time frame. Generally, apnea monitors are needed for 2 to 4 months for many of these patients.72
Patient Assessment and Documentation
Institutional Long-Term Care
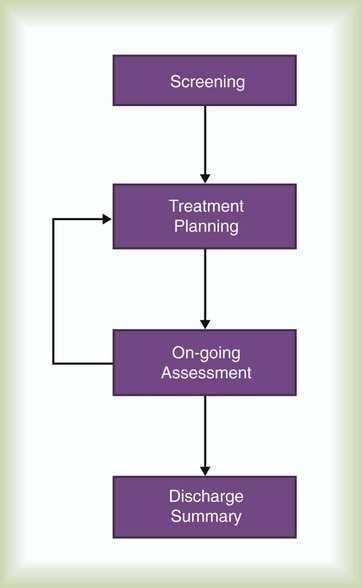
In institutions providing long-term care, the assessment and documentation process involves four key components: screening, treatment planning, ongoing assessment, and discharge (Figure 51-11).
Screening
On admission to a long-term care facility, all patients with a respiratory-related admitting diagnosis should be screened by an RT.17 This screening is often accomplished solely by chart review, without direct contact with the newly admitted patient or resident. During screening, the RT reviews the pertinent respiratory diagnosis, onset and severity of symptoms (including the impressions of the resident’s nurse), current radiograph results, pulmonary function tests, arterial blood gas values, and other nonrespiratory treatment orders (e.g., physical therapy).
If the review indicates the need for a more in-depth assessment, the RT can recommend a more complete evaluation. On receipt of the appropriate orders, the RT interviews the patient and conducts a physical assessment, including inspection, palpation, auscultation, and percussion. Key clinical findings include description of breath sounds; rate, depth, and pattern of respirations; heart rate; signs of dyspnea; cough; sputum production; level of consciousness; and ability of the resident to understand and follow commands. Also noteworthy are the resident’s prior respiratory status, use of supplemental O2, skin turgor, and medications. Where indicated, a pulse oximetry test is performed during the evaluation.17,18
Treatment Planning and Ongoing Assessment
Based on the information obtained during the initial screening process, the RT designs a specific treatment plan. A typical treatment plan includes patient demographics, assessment information, short-term and long-term goals reflective of overall rehabilitation potential, and measures to be used to achieve such goals. A treatment plan for a resident of a long-term care facility with moderate to severe COPD would likely reflect the treatment goal of correcting hypoxemia through the use of low-flow O2 and patient monitoring.17,18
After therapy has been initiated, the RT uses several other tools to monitor a patient’s progress. In addition to regular treatment documentation, the RT should document a regular summary on each patient. This summary provides a synopsis of residents’ progress toward goal attainment, including changes in respiratory status, results of any additional tests, explanation of any patient education, and recommendations for additional therapy. These summaries become part of the resident’s permanent record, with a copy going to the attending physician. Additionally, treatment plans and progress summaries are often required documentation for third-party reimbursement.17,18
Home Care
A home care plan must specify not only the types of care provided but also a strategy for patient follow-up. The individual making the follow-up visits could be the attending physician but more commonly is the visiting nurse, a physical therapist, or an RT. For patients receiving respiratory care at home, follow-up by a home care team member should occur regularly, particularly for patients on “hi-tech” equipment such as ventilators and apnea monitors.12 Some patients may require more frequent follow-up, especially patients recently discharged or patients requiring ventilatory support. Factors relevant to the frequency of home visits include the following:
• Patient’s condition and therapeutic needs (objectives)
• Level of family or caregiver support available
• Type and complexity of home care equipment
When a visit is made by the RT, numerous functions must be performed, including the following:
• Patient assessment (objective and subjective data), including pretreatment and posttreatment clinical assessment
• Patient’s compliance with prescribed respiratory home care
• Equipment assessment (operation, cleanliness, and need for related supplies)
A standard written report, consistent with the care plan, should be completed by the visiting RT. Copies are often sent to the patient’s physician, the home care referral source, and any other member of the team requiring this information. The report should become part of the patient’s medical record and should be referred to when following the patient’s course and overall progress.12,16
Equipment Disinfection and Maintenance
With more and more patients receiving respiratory care outside the hospital, the danger of infection caused by direct contact with caregivers and visitors or indirect contact with contaminated articles and equipment has grown. To help minimize home-related infection, guidelines for disinfecting home respiratory care equipment have been established. Accepted infection control techniques are based on clinical evidence, such as the evidence outlined in several of the AARC Clinical Practice Guidelines that pertain to respiratory care provided in alternative settings.24,43,62,65,73
Collectively, these guidelines focus on sources of infection, basic principles of infection control, patients at high risk, disinfection methods, equipment processing, and care of solutions and medications. Procedures focus significantly on surveillance, prevention, and control of infection.15,16
In regard to using water for humidification or nebulization, it is recommended that distilled water be used as a first choice. However, boiled water, cooled in a refrigerator and discarded after 24 hours, is also generally acceptable. It is recommended that manufacturers’ guidelines for the proper handling of specific medications be strictly followed. Detailed instructions for patients and caregivers on how to clean and disinfect selected respiratory care equipment are generally available from most manufacturers. Policy and procedure manuals should describe equipment cleaning and infection control measures and require that home care patients and caregivers receive verbal and written instructions on this topic.73,74
Palliative Care
The definition of palliative care by the World Health Organization involves the control of pain and other symptoms such as dyspnea of terminally ill patients and maximizing the psychologic, social, and spiritual well-being of family members and patients nearing the end of life.75 Many terminally ill patients have respiratory dysfunction directly or indirectly resulting from their terminal illness. Some of these patients choose to experience the remainder of their life at home. Hospice is a philosophy of care that helps support the efforts of such patients by providing clinician coverage and equipment to these patients at home.75