Pulmonary Function Tests
Guidelines for Interpretation and Sample Problems
This appendix provides an outline of a simplified approach to interpreting pulmonary function tests and gives several examples of test results presented as unknown problems. Because details of the interpretation of these tests may vary among laboratories, the approach here focuses on the general concepts rather than the specific details, providing a step-by-step approach to analyzing pulmonary function tests. The concepts underlying this step-by-step approach are covered in the relevant section on pulmonary function tests in Chapter 3.
Analysis of Pulmonary Function Tests
1. Examination of lung volumes:
a. A decrease in total lung capacity (TLC) generally indicates the presence of a restrictive pattern. However, TLC measured by helium dilution may also be artificially depressed when there are poorly communicating or noncommunicating regions within the lung (e.g., in bullous lung disease).
b. Are lung volumes symmetrically reduced (i.e., are TLC, residual volume [RV], functional residual capacity [FRC], and vital capacity [VC] all decreased to approximately the same extent)? If so, this suggests interstitial lung disease as the cause of the restrictive pattern. A low diffusing capacity also supports the diagnosis of interstitial lung disease as the cause of the restrictive pattern.
c. A relatively preserved RV and a normal diffusing capacity suggest another cause of restrictive disease, such as neuromuscular or chest wall disease. Poor effort from the patient may also create this type of pattern.
2. Examination of the mechanics—that is, flow rates measured from the forced expiratory spirogram:
a. A decrease in the ratio of forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC) indicates obstruction. In some cases of airflow obstruction, both FEV1 and FVC are reduced by approximately the same extent, and FEV1/FVC may be preserved. Clues to the presence of obstructive disease in this setting are a low forced expiratory flow from 25% to 75% of vital capacity (FEF25%-75%), a normal to high TLC with a high ratio of RV to TLC, and the configuration of the flow-volume curve.
b. Interpretation of FEF25%-75% (also called maximal midexpiratory flow [MMF]):
(1) FEF25%-75% is subject to more variability than most other measurements obtained during a forced expiration, so guidelines for normal values are less well established.
(2) When lung volumes are low, FEF25%-75% can also be decreased without necessarily indicating coexisting airflow obstruction. Therefore, in the presence of decreased lung volumes, a low FEF25%-75% indicates obstruction primarily if the decrease in FEF25%-75% is out of proportion to the decrease in lung volumes.
(3) Taking into account the aforementioned qualifications, FEF25%-75% may be a relatively sensitive measurement for airway obstruction. An isolated abnormality in FEF25%-75% has sometimes been considered a marker for early or very mild airflow obstruction, theoretically reflecting “small airway disease.”
3. Interpretation of diffusing capacity of the lung for carbon monoxide (DLCO):
a. Make sure the value has been corrected for the patient’s hemoglobin level. If not, the value will be falsely low if the patient is anemic.
b. A decrease in the diffusing capacity reflects disease affecting the alveolar-capillary membrane (decreased surface area for gas exchange and/or abnormal thickness of the membrane) or a decrease in pulmonary capillary blood volume.
c. An increase in the diffusing capacity can reflect increased pulmonary capillary blood volume or erythrocytes within alveolar spaces (pulmonary hemorrhage).
4. Interpretation of the flow-volume curve:
a. An obstructive pattern is reflected by decreased flow relative to lung volume, generally accompanied by a “scooped out” or “coved” appearance to the descending part of the expiratory curve (see Fig. 3-19).
b. A restrictive pattern is characterized by decreased volumes (i.e., narrowing of the curve along the volume or X-axis) and relatively preserved flow rates. The flow rates often appear increased relative to the small lung volumes, producing a tall, narrow curve.
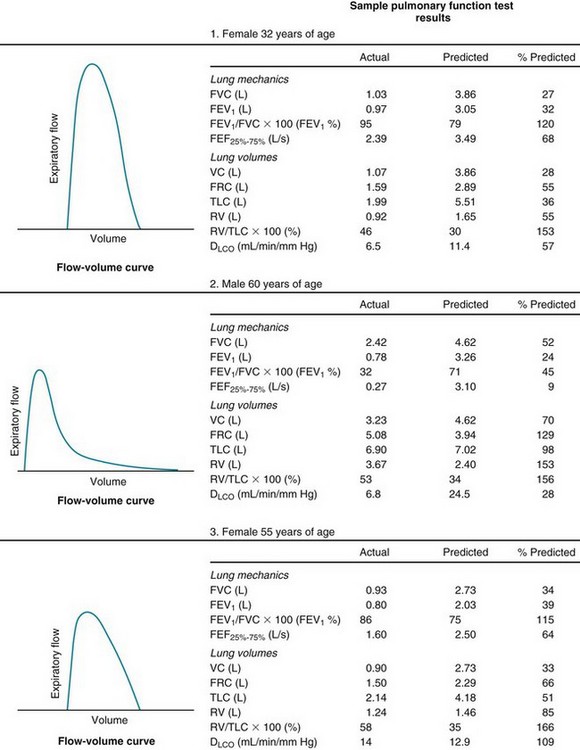
Answers
1. All measurements of lung volume (TLC, VC, FRC, RV) are significantly decreased, indicative of restrictive disease. FEV1 and FVC are decreased because of low lung volumes, but FEV1/FVC is preserved. This finding, along with the fact that FEF25%-75% is not decreased out of proportion to the decrease in lung volumes, indicates there is no obstruction. Diffusing capacity is decreased, suggesting that the restrictive disease is secondary to an abnormality of the pulmonary parenchyma rather than a result of chest wall or neuromuscular disease. The flow-volume curve is tall and narrow, consistent with a restrictive pattern. Diagnosis: Interstitial lung disease secondary to pulmonary sarcoidosis.
2. FEV1 and FVC are both decreased. Because FEV1 is decreased more than FVC, FEV1/FVC is decreased. FEF25%-75% is also decreased. These values are indicative of obstructive lung disease. TLC is normal, and RV and FRC are increased. RV/TLC ratio is also increased. Therefore, there is no restriction, but the high RV/TLC ratio indicates there is “air trapping,” as is often expected with airflow obstruction. The diffusing capacity is decreased, reflecting loss of alveolar-capillary bed. The flow-volume curve shows an obstructive pattern characterized by a striking decrease in flow rates, well seen throughout most of the expiratory curve after the initial peak flow rate. This combination of significant airflow obstruction with normal or increased volumes and a low diffusing capacity suggests emphysema.
3. TLC and FRC are reduced, indicating restrictive disease. RV is relatively preserved. FEV1 and FVC both are decreased, but FEV1/FVC ratio is preserved. There is no evidence for coexisting obstructive disease. Diffusing capacity is normal, suggesting the alveolar-capillary bed is preserved. The flow-volume curve is relatively tall and narrow, without any evidence of obstructive disease. Diagnosis: Restrictive pattern secondary to chest wall disease (kyphoscoliosis).