14 Patients with pelvic girdle pain: An osteopathic perspective
Introduction
1. The human being is a dynamic unit of function.
2. The body possesses self-regulatory mechanisms that are self-healing in nature.
3. Structure and function are interrelated at all levels.
4. Rational treatment is based on these principles.
(Ward & Sprafka 1981, Lesho 1999, Educational Council on Osteopathic Principles 2009)
Though anatomy and physiology are commonly taught in parts and systems, the first tenet recognizes that the person is a dynamic unified whole, not the mere compilation of anatomical parts or physiological systems. The pelvic girdle is anatomically linked to the entire spine and upper and lower extremities; it is an integral component to standing and sitting postures and motions (Beal 1982, Ronchetti et al. 2008). Therefore, in search of the cause of PGP and dysfunction, the clinician should examine the entire musculoskeletal system while the patient is walking, standing and sitting, as well as in the passive postures of lying supine and prone. The pelvic girdle is also intimately associated with the pelvic viscera that it protects (Beal 1985, Tettambel 2005). Additionally, the person’s environment, social life, diet and nutrition, drugs used or abused, sleep patterns, emotions, beliefs and other behavioural factors play a role in the generation and recovery from PGP (O’Sullivan & Beales 2007, Vøllestad & Stuge 2009).
The second tenet stresses that the body is capable of self-regulation, self-healing and health maintenance. This capability is inherent, but at times may require assistance in the form of manual therapy, surgery, exercise, nutritional advice, pharmacology or counselling (Tettambel 2007, Fall et al. 2010).
The third tenet states that structure and function are inter-related. Bodies have architectural (anatomical) form and engineering (physiological) processes that intimately influence each other. In the pelvic girdle, if there is sacroiliac dysfunction or lumbosacral torsion, a patient may have mechanical or structural back pain that might contribute to bowel dysfunction or urinary problems (Beal 1985, Browning 1990, Tettambel 2005). Conversely, if a woman has a difficult pregnancy or childbirth, she may develop pelvic pain as a result of a caesarean section or vaginally delivering a very large baby with or without instrumentation. Over time, the pain may become chronic, affecting her posture and gait (Ronchetti et al. 2008); and she may not anticipate another pregnancy with a positive attitude. Thus, the fourth osteopathic key tenet is pertinent: rational treatment is based upon the three previous principles. In this instance, to restore normal functionality, rational treatment may consist of postpartum spinal and extremity manual therapy; exercise to maintain stability and encourage flexibility of her musculoskeletal system; and perhaps family planning counselling to allow her to care for herself and her family.
Each of the above principles is important to the understanding of somatic dysfunction. Somatic dysfunction can be defined as ‘impaired or altered function of related components of the somatic (body framework) system: skeletal, arthrodial and myofascial structures and their related vascular, lymphatic and neural elements’ (Educational Council on Osteopathic Principles 2009). When a patient presents with PGP, the clinician should consider whether there is a somatic component to the chief complaint, injury or illness:
• Where in the soma might the problem exist?
• Although the presenting painful condition may involve the pelvic girdle, could other bones, muscles, ligaments, nerves, vasculature, pelvic organs, fascia and/or related structures be primary features? (See Chapter 9.)
There may also be other relationships between the pelvic container and its contents, potentially affected by posture, gait and pulmonary ventilation (see Chapter 11). Somatic dysfunction could also be the result of a neurophysiological phenomenon, i.e. peripheral or central sensitization (Howell & Willard 2005) (see Chapter 3 for physiological mechanisms). Reflex loops of visceral and somatic excitation and facilitation may also be involved, introducing autonomic and referred pain to the equation (Janig 2008).
If there is a disturbance of the normal function of somatic structures, how might the problem best be addressed? Somatic dysfunction possesses characteristics identifiable by means of palpation to appreciate static or motion asymmetry of the body, as well as changes – structural and physiological – in other body tissues or systems. Osteopathic clinicians who perform osteopathic manipulative treatment (OMT) commonly use a combination of tests that evaluate the patient for signs of sensitive or tender points, tissue texture abnormalities in the soft tissues surrounding the spinal and pelvic joints, asymmetry of anatomical landmarks and alterations in quality or quantity of range of joint motion (Dinnar et al. 1982, Beal 1982, Fryer et al. 2009). A useful mnemonic, ‘STAR’, may be helpful to establish a palpatory structural diagnosis that may be amenable to manipulative treatment (Educational Council on Osteopathic Principles 2009) (see Box 14.1).
Box 14.1 STAR mnemonic used to establish a palpatory structural diagnosis amenable to manipulative treatment
• ‘S’ represents sensitivity. Sensitivity may occur as the result of tissue contact or pressure that would not be sufficient to cause discomfort in ‘normal’ tissues. This may be reported as tender or painful by the patient when being palpated. To establish a diagnosis of somatic dysfunction, sensitivity may or may not be present. Sensitivity may be subjective and not always a reliable indicator of dysfunction. However, a patient may not be aware of any pain until a structure is palpated. Usually, a patient with a complaint of pain may be anxious about the performance of a palpatory exam and report increased tenderness on palpation of a structure because the structure was palpated (Fryer et al. 2004a).
• ‘T’ represents tissue texture abnormality that is palpable evidence of physiological dysfunction. Palpable changes found in skin, subcutaneous tissue, fascia and muscles reflect disturbances in local tissues, related organs or specific spinal segments. Tissue changes can be acute or chronic somatic dysfunctions. In acute dysfunction, one can palpate warmth, moisture, as well as bogginess and increased tension of tissues. Oedema may be present. Conversely, in chronic dysfunction, the tissues may feel cool, thin, dry and ropey (O’Connell 2003, Fryer et al. 2005).
• ‘A’ represents structural asymmetry, which may be observed or palpated. Anatomical landmarks, such as iliac crests or trochanter heights, can be visualized to compare bilateral location. These landmarks can also be palpated to assess position bilaterally as well (Beal 1982).
• ‘R’ represents range of motion. This motion may be either active or passive with quantitative and qualitative features. To evaluate joints of the pelvic girdle by palpation, one must note how much the joint moves and how well it moves. What restrictions to normal motion are present? Where are the anatomical, restrictive and pathological barriers in both active and passive motion testing? How do these barriers affect local joint motion as well as the rest of the pelvis (Beal 1982)? Ultimately how does this dysfunction affect the body as a unit of function (Tettambel 2005)?
When the pelvic girdle is restricted, gait and posture change (van Wingerden et al. 2008). Persistent PGP can negatively affect the patient’s attitude about ability to function, sometimes to a state of depression and altered sensorium due to chronicity of the problem (Gutke et al. 2007). Pelvic girdle motion may also be restricted by pelvic organ pathology (Beal 1985). A bimanual pelvic exam may detect a mass, pelvic inflammatory disease, adhesions from infection or surgery, or possibly signs of endometriosis (Tettambel 2005). In addition to restriction of motion, pain may be elicited (Boyle 2008). However, in a patient with PGP due to somatic dysfunction, the primary objective should be to treat the dysfunction underlying the pain (Damen et al. 2001).
Used alone, digital pain provocation for sensitivity of the soft or osseous tissues is the most reliable of the four types of palpatory tests in the neck and back regions (Seffinger et al. 2004, Stochkendahl et al. 2006). Lumbar percussion for pain provocation is very specific, so it can be used as a screening test; if it reproduces the patient’s reported pain, then there is indeed a truly painful condition at that location (Kristiansson & Svardsudd 1996). It must be understood that reliability of pain provocation tests does not indicate that more than one examiner can reliably feel or interpret the sensitivity of the palpated tissues; rather that a patient can reliably state repetitively that a palpated site is sensitive when palpated by different practitioners (Seffinger et al. 2004, Haneline & Young 2009). Soft tissue tests assessing for tissue texture abnormalities, altered compliance or presence of muscle tension are in general not reliable when used as the sole source of palpatory information (Seffinger et al 2004, Stochkendahl 2006, Haneline & Young 2009). Although regional range of motion tests are more reliable than segmental range of motion tests, motion tests for SIJ or lumbar mobility are not in general reliable (Hestbaek & Leboeuf-Yde 2000, van der Wurff et al. 2000a, 2000b, Seffinger et al. 2004, Stochkendahl 2006, Robinson et al. 2007). However, using a cluster of pain provocation tests combined with motion tests improves reliability (Arab et al. 2009). Likewise, combinations of pain provocation tests have demonstrated validity (Van der Wurff et al. 2006, Hancock et al. 2007, Szadek et al. 2009). Pelvic distraction, thigh thrust, compression and sacral thrust tests in combination are accurate in detecting the SIJ as a source of pain (Laslett et al. 2003, 2005). When all tests do not provoke pain, the SIJ can be ruled out as a source of the pain. One study demonstrated that the maximum interexaminer reliability occurs when only the result of the most reliable test is used to determine the side of SIJ dysfunction, sacral base position and innominate bone position (Tong et al. 2006).
The European guidelines for physical diagnosis of PGP (Vleeming et al. 2008) recommend using the following tests as they have demonstrated reliability:
• Posterior pelvic pain provocation test (P4);
• Patrick’s Faber (hip flexion, abduction, external rotation);
• Palpation for sensitivity of the long dorsal SIJ ligament;
• Palpation for sensitivity of the pubic symphysis;
• Motion tests of femoral compression, lumbar movement and supine iliac gapping (Kristiansson & Svardsudd 1996, DonTigny 2005a, 2005b);
• Digital pressure to assess the sacrospinous ligament and posterior superior iliac spine (Kristiansson & Svardsudd 1996);
Using a combination of reliable lumbar and pelvic motion and sensitivity assessment tests in pregnant patients with non-specific lumbopelvic pain, two examiners were able to reach substantial agreement in differentiating patients as having either lumbar pain or PGP (Gutke et al. 2009). This is useful since up to 25% of patients presenting to a spine specialist pain clinic with low back pain are likely to actually have PGP (sacroiliac and/or hip as pain generator) (Sembrano & Polly 2009). If primary care clinicians were better at screening patients with low back pain, unnecessary referrals to specialists would result, limiting unnecessary expenditures of precious personal and healthcare industry financial resources.
Evaluation of the pubic symphysis and tubercles for levelness and tenderness is used to determine imbalance of forces attached there, including the rectus abdominis muscles and sheath, thigh adductor muscles (adductor magnus, longus and brevis, the gracilis and the pectineus), inguinal ligament and pelvic floor muscles (levator ani and coccygeus) (Greenman 2003).
The information outlined above forms a foundation for understanding an osteopathic approach to assessing and treating patients with PGP (Jordan 2006). Beyond palpatory evaluation for evidence of somatic dysfunction (i.e. assessing for STAR), additional information may help to determine treatment plans. Patient gender, age, professional and social activities, attitude, as well as other factors help determine the approach to evaluation and a care plan.
• Dancers, for example, commonly complain of lumbopelvic and various musculoskeletal pain at various times in their career depending on the demands placed upon them by the choreographer, the environment, their skill, age, coping ability and experience (Demann 1997, Hincapié et al. 2008).
• Athletes of sports that entail increased mechanical load on the lumbosacral spine and pelvis are at higher risk for PGP and low back pain (Bahr et al. 2004).
• The elite athlete has special considerations as well (Bo & Backe-Hansen 2007).
• The type of employment may affect the cause and nature of PGP. For example, the main biomechanical risk factors identified for the development of low back work-related musculoskeletal disorder were heavy physical work, awkward static and dynamic working postures, and lifting; the psychosocial risk factors identified were negative affectivity, low level of job control, high psychological demands and high work dissatisfaction; individual risk factors identified were younger age and high body mass index (da Costa & Vieira 2009).
• Motor vehicle collision survivors might have injuries from steering wheel blows to the pelvis, compression of door panels into the hip, lapbelt-incurred lumbopelvic torsions, or femoropelvic compression from floorboard and pedal ground forces at time of impact; or when bracing in preparation of the impending event.
• Older adults may have developed posture or gait disorders due to trauma (falls, accidents), or disease (neurological, vascular, cataracts) that can affect pelvic girdle mechanics.
• Young females who participate in sports may have ligamentous laxity, making them more susceptible to injury (Bo & Backe-Hansen 2007). Pelvic ligamentous laxity is helpful in childbearing years, but not desirable in menopause (Gabbe 2007).
• Pregnancy and birth trauma may result in chronic PGP (Latthe 2006, van der Hulst 2006).
• Sexual trauma may also result in pelvic pain and dysfunction.
• Postmenopausal women are at risk for pelvic organ prolapse, bladder or bowel incontinence, osteoporosis and degenerative arthritis (Prather 2007). Hormonal factors also influence pelvic structures, function and pain (O’Sullivan & Beales 2007, Eberhard-Gran & Eskild 2008).
• Women who work outside the home may develop pain due to ‘wardrobe malfunctions’ of restrictive clothing or uncomfortable shoes (Chen et al. 2005), as well as postural challenges that accompany manual labour or repetitive actions.
• Obesity as a result of pregnancy, endocrine problems, or poor nutritional habits contributes to pelvic girdle dysfunction (Mottola 2009).
An osteopathic approach to the patient with PGP would start with collection of historical information and the performing of a comprehensive physical examination, including a palpatory structural examination. A patient-centred treatment approach would investigate what would be required to promote health in the presence of challenging situations. In osteopathic literature there are five conceptual treatment models to promote health and modify disease (pathological) processes (Educational Council on Osteopathic Principles 1987, 2009, Hruby 1991, 1992). As the body is an integrated whole, posture, neural responses, respiration/circulation, metabolic processes and behaviour are tightly woven together; dysfunction of any of these coordinated body functions will therefore compromise the entire organism. Each of these models is discussed in this chapter, with intended therapeutic benefits, within the four key principles outlined above.
Biomechanical model
The biomechanical model requires knowledge of posture and motion as they relate to PGP and dysfunction (see Box 14.2). The patient should be observed in active posture as well as in the resting supine position. Palpatory examination using the combination of elements of STAR should be employed. It is necessary to consider how motions of the pelvic container affect both motion and function of the pelvic contents. Also requiring consideration is how pelvic dysfunction relates, from cause-and-effect perspectives, to the spine, abdomen, rib cage, lower and upper extremities. The spinal curves, lateral as well as anterior-posterior, require assessment, with consideration of their effect on muscle length and tension. Posture is assessed when standing or sitting from anterior, posterior and lateral views. Notes on postural influences are to be found in Chapter 11. Orthopaedic tests help determine structural and functional involvement of particular lumbopelvic components (Liebenson 2004, 2007). When evaluating the patient, painful structures usually denote muscle spasm or hypertonicity, but may also indicate peripheral and/or central sensitization (Howell & Willard 2005) or the result of decreased muscle activity (Fryer et al. 2004b). The antagonists to hypertonic muscles may be inhibited. Short- and long-term (up to 2 years) outcomes improve with an individualized exercise programme addressing muscle imbalance to relieve such weakness or inhibition (Stuge et al. 2004a, 2004b). Presence of rectus abdominis muscle diastasis, especially in post partum women, should be assessed and treated due to the effect it can have on the integrity of the abdomino-pelvic ‘canister’ and its functions in providing postural stability, controlled bladder function and efficient breathing mechanics (Lee et al. 2008).
Box 14.2 Biomechanical aetiological features
• Congenital deformities such as small hemipelvis, club foot, facet asymmetry in the lumbosacral spine, partial or complete sacralization of the fifth lumbar, spondylolisthesis, spina bifida occulta, or butterfly (or bat) wing process can alter lumbopelvic biomechanics (Bailey & Beckwith 1937). Most of these conditions are discovered by X-ray, when there is an unsuccessful course of conservative care, which may have included manipulation. They may or may not be related to PGP and may or may not require surgical correction. Spine surgical consultation is indicated if symptoms do not improve or worsen with conservative measures.
• Anatomical short leg can cause sacral base unlevelling and pelvic asymmetry related to lumbopelvic pain (Juhl et al. 2004). Posture and gait can be affected with resultant musculoskeletal imbalance, scoliotic spinal curves and pain (Juhl et al. 2005). Heel lift therapy should be considered in patients with PGP and low back pain associated with unlevel sacral base due to anatomical short leg (Lipton et al. 2009).
• Injury to the coccyx due to trauma or childbirth can affect sacral motion via its ligamentous attachments (Meleger & Krivickas 2007). Ligamentous strains of the coccyx can also affect motion of the ilia and ischia, as well as cause pain in the pelvis, perineum and lower extremities. Coccygeal muscle pain can persist despite normalization of sacral dynamics due to the strong ligamentous spans retaining positional strain patterns; the authors have noted that some patients with persistent coccydynia complain of coccygeal pain with bowel movements, micturition, coitus, and upon sitting, standing or moving, likely because two-thirds of the levator ani sling muscles involve the coccyx.
• Lumbopelvic somatic dysfunction can compromise pelvic diaphragm (levator ani and coccygeus muscles) balance and functions, resulting in pelvic floor pain and bladder dysfunction (Pool-Goudzwaard et al. 2005, Arab et al. 2010). Bowel function may also be compromised (Ng 2007).
• Pelvic obliquity can arise from imbalances of the iliopsoas muscles and quadratus lumborum muscles. These form the deepest of the lumbopelvic core muscle layers.
• Difficult childbirth may induce pubic shears or avulsions. In addition to painful gait, dyspareunia with sexual dysfunction and bladder voiding dysfunction can result.
• In the Mitchell model of the ‘walking cycle’, the transverse axis for gait is through the pubic symphysis. Shears and compression strains would not only affect gait, but posture and pelvic bowl tilt as well (Greenman 2003). Movement at the pubic symphysis may be small, but intense pain on standing (on one leg) or walking may be reported by the patient when dysfunction exists (Greenman 2003).
Mitchell (1958) was an osteopathic pioneer in the development of a biomechanical model to explain the role of the pelvis in posture and gait. Mitchell also collaborated in the development of muscle energy technique (MET), a modality employed to treat somatic dysfunction (Goodridge 1981). This approach and his techniques have been adopted widely across professions and cultures. When joints such as SIJ are altered from their ideal positioning, or if inflammation or joint fluid pressures are elevated, inhibited motion occurs, often with resultant pain (Howell & Willard 2005). Muscle energy techniques (MET) may be used to balance muscle tone (i.e. stretch hypertonic muscles and strengthen hypotonic muscles), relieve asymmetrical forces upon spinal and peripheral joints, and enable restoration of normal joint motion (Wilson et al. 2003, Selkow et al. 2009). Benefits of MET manipulation alone, and combined with exercise, are beginning to be assessed by randomized clinical trials (Wilson et al. 2003, Selkow et al. 2009). Further studies are needed, especially in the contexts of the patient’s age and other activities of daily living.
Gait (or other means of locomotion) should be assessed for its cadence, symmetry, rate and reported ease through repeated visual or kinematic observation. Specific patterns of muscle activity have been fitted into the six determinants of the gait cycle (Kerrigan et al. 2000, 2001, Esquinazi & Mukul 2008). In patients with PGP, muscle activity patterns are not only altered during gait (Wu et al. 2008), but also during the active straight leg raising (ASLR) test as compared with pain-free subjects (O’Sullivan et al. 2002, Beales et al. 2009a, 2009b). Researchers found increased minute ventilation, decreased diaphragmatic excursion (O’Sullivan et al. 2002), increased intra-abdominal pressure (Beales et al. 2009a, 2009b) and increased pelvic floor descent (O’Sullivan et al. 2002, Beales et al. 2009a, 2009b) during the ASLR test in PGP patients, indicating considerable widespread effects on the neuromuscular control of respiration and pelvic floor function. Interestingly, enhancement of pelvis stability via manual compression through the ilia reversed these differences (O’Sullivan et al. 2002, Beales et al. 2009a, 2009b). Hu et al. (2010) therefore reasoned that since manual pelvic compression restores normal abdominal and pelvic motor control in patients with PGP during the ASLR test, a pelvic compression belt worn while walking might provide similar stabilizing effects. Nulligravid women walked on a treadmill at increasing speeds while wearing or not wearing a belt. Simultaneously, there was fine-wire electromyography (fwEMG) of the psoas, iliacus and transversus abdominis muscles and surface EMG (sEMG) of other hip and trunk muscles. Wearing a pelvic belt while walking reduced core abdominal muscle activity and induced contralateral activation of biceps femoris and gluteus maximus, thus promoting anterior tilting of the pelvis and enhancing force closure effects. Thus, poor force closure of the SIJs may be a key component of the altered gait, respiration and pelvic floor mechanics observed in some patients with PGP. Pregnancy adds another mechanical challenge to the patient with form and force closure problems. Wu et al. (2004) compared gaits of healthy women who were pregnant or nulligravid and found them to be very similar except for increased antiphase pelvis–thorax coordination among pregnant subjects walking quickly; the difference is greater among women with PGP while pregnant (Wu et al. 2008).
Pelvic mechanics are also altered in men who have PGP. Hungerford et al. (2004) did kinematic assessment of pelvic bone motion in men with posterior pelvic pain (PPP) compared to men without PPP. Posterior rotation of the weight-bearing innominate was observed in controls, while anterior rotation during weight-bearing occurred in symptomatic men.
Sacral motion can occur around a variety of axes: anteroposterior, vertical, horizontal or oblique (Beal 1982). It is most likely, however, that there is no stationary sacral axis and that the axis shifts with the introduction of movement (Beal 1982). Sacral and lumbar spine motions are often impaired in patients with PGP (Beal 1982, van Wingerden et al. 2008). Sacroiliac motion can be restricted at the superior or inferior aspects of the SIJ; compression can also occur (Beal 1982, Vleeming et al. 1990a, 1990b). There are no muscle attachments directly connecting the sacrum to the pelvic girdle. The sacrum is suspended between the ilia by ligaments. Its motion is influenced by joint surface (form closure) and myofascial and ligamentous function (force closure) (Vleeming 1990a). Ligamentous strains or laxity during pregnancy can disrupt joint mechanics, cause low back and pelvic girdle pain (Damen et al. 2001), and contribute to muscle imbalances in the pelvis, lower extremities and trunk of the body. In gynaecology patients, evaluation of sacral motion and dysfunction, along with pelvic girdle motion, should be assessed. On clinical gynaecological examination, strains of the broad ligament and uterine malpositioning may be inter-related with altered bone and joint mechanics (Barney 2008, Boyle 2008). The abdominal, lumbar, pelvic and lower extremity myofascial tension affects SIJ stiffness and stability (Van Wingerden et al. 2004). Patients with PGP with or without low back pain have altered standing posture and forward-bending motions (Van Wingerden et al. 2008). Therefore, it is important to assess and treat not only contiguous bony and ligamentous structures but the back, pelvic and extremity muscles and fascia as well, in helping the patient resolve not only the PGP, but to restore and maximize gait, posture and motion.
Hip range of motion impacts lumbopelvic integrity (Liebenson 2004, 2007) and should be checked in all directions to assess its six muscle groups. Janda (1977, 1986) found that prone hip extension reveals hamstring strain substitution for gluteus maximus activation. Nadler et al. (2002) associated impaired hip extension with propensity for low back pain in women. Vleeming and colleagues (2007) have written extensively about the biomechanical integration of rectus femoris muscle and sacrotuberous ligament as a key component of form closure and force closure affecting the long dorsal sacroiliac ligament and other pelvic girdle structures. Janda (1977, 1986) and Nadler et al. (2002) also found that weak hip abductors contribute to lumbopelvic instability and motor control substitution. Hip pain is also increased with lumbar hyperflexibility more frequently than stiffness (Biering-Sorensen 1984). Hip external rotation is likely to show lumbopelvic dysfunction than internal rotation (Liebenson 2007).
There is marked similarity between osteopathic and physical therapy assessments of dysfunction present in patients with PGP as evidenced by correlating the reports from Greenman (1996) with the integrated pelvic girdle model of Vleeming et al. (2007) and Lee (2004) (see Table 14.1).
Table 14.1 Osteopathic and physical therapy assessments of dysfunction
| Somatic dysfunctions (SD) in persistent low back pain (Greenman 1996) | Integrated model of pelvic girdle: form closure, force closure, motor control, emotional awareness (Lee 2004, Vleeming et al. 2007) |
|---|---|
| Non-physiological pelvic SD (pubic shears) | Core, abdomen, pelvic floor and hip adductor muscles imbalance at pubic tubercles and rami |
| Non-physiological pelvic SD (sacroiliac shears) | Improper load distribution of sacroiliac joint (SIJ) |
| Sacral nutation failure (including non-neutral and backward sacral torsion SD) | Flexion (nutation): sacrotuberous ligament-biceps femoris Extension (counternutation): long dorsal sacroiliac ligament |
| Pelvic tilt/‘Short-leg syndrome’/unlevel sacral base | Impaired pelvic–trunk coordination |
| Muscle imbalance (including psoas syndrome) | Global muscle and core muscle faulty recruitment |
| Lumbar single level (Type II) lumbar SD | L5 associated with SIJ dysfunction |
Osteopathic manipulative treatment options (see Box 14.3)
Osteopathic manipulative treatment (OMT) has been shown to be efficacious in treating chronic low back and pelvic pain (Licciardone et al. 2005), low back pain during pregnancy (Licciardone et al. 2010), pelvic pain from chronic prostatitis (Marx et al. 2009), and is advocated for women with chronic pelvic pain (Tettambel 2007) and patients with PGP (Greenman 2003). When diagnosing and treating somatic dysfunction with OMT, choosing the type of manipulative procedure appropriate for the patient requires training and experience.
Box 14.3 Osteopathic terminology (ECOP 2009)
• Somatic dysfunction. Impaired or altered function of related components of the somatic (body framework) system: skeletal, arthrodial and myofascial structures, and their related vascular, lymphatic and neural elements. Somatic dysfunction is treatable using osteopathic manipulative treatment.
• Osteopathic manipulative treatment. The therapeutic application of manually guided forces by an osteopathic physician (US) or practitioner to improve physiological function and/or support homeostasis, which have been altered by somatic dysfunction. OMT employs a variety of techniques, including:
In addition, knowing when and how much OMT to provide is important.
• Diagnosis of recent, acute strains or sprains from trauma requires early biomechanical intervention, but in small and frequent doses.
• Chronic conditions respond to larger doses of manipulation given at longer intervals (Kimberly 1976, Ferreira et al. 2003, Greenman 2003, Bronfort et al. 2006). Taking into consideration the age of the patient is another factor in determining the dose of OMT.
• Younger (adolescent) patients may tolerate more vigorous muscular and ligamentous treatment procedures; however, theoretically, due to the immaturity and primarily cartilaginous structure of the young child’s pelvis, imprecise aggressive treatment of these joints could disrupt cartilaginous portions of pelvic bones, induce membranous strains, and possibly result in fractures or deranged joint structures.
• Other adjustments to how much OMT to provide need to be made for the ill patient who often has limited energy reserves, weakness and pain.
• Soft tissue, articulatory procedures, such as joint springing, and thrust, or high-velocity/low-amplitude (HVLA), OMT, when performed gently and precisely are effective and well-tolerated in most patients; thrust (HVLA) for SIJ dysfunction and PGP has been used successfully during pregnancy (Daly et al. 1991). Counterstrain, myofascial release, balanced ligamentous tension, and cranial balanced membranous tension treatments are all helpful for patients of any age; they may be most often utilized in infants and young children (Hayes & Bezilla 2006) as well as elderly patients with advanced arthritis or other degenerative disease processes (Hruby 2008). Similar to chiropractic articulatory adjustments, osteopathic manipulations involving thrust are the techniques most likely to have contraindications (bony metastases, bony infections, osteoporosis, etc.), while soft tissue and non-thrust techniques are relatively safe when prudently performed by skilled practitioners (Kuchera et al. 2003).
Respiratory–circulatory model
Somatic dysfunction involves neurogenic inflammatory processes, decreased lymph and blood flow, and palpable congestion of the soft tissues (Pickar 2002, Howell & Willard 2005). A goal of manipulation is to relieve congestion (see Chapter 11).
• Osteopathic manual procedures to the thorax, thoracic inlet and diaphragm have been shown to improve cardiopulmonary function (O-Yurvati et al. 2005).
• Spontaneous breathing improves movement of lymph from the abdominal to the thoracic cavity (Lattuada & Hedenstierna 2006).
• External manual rhythmical abdominal pumping increasing lymph flow and flux in the thoracic duct (Hodge et al. 2007, Downey et al. 2008).
The respiratory–circulatory model views somatic dysfunction in relation to the influence on the ease of respiration and lymph and venous drainage, more than the view of neural entrapment or biomechanically altered function. Skeletal muscles and the thoracic and pelvic diaphragms are pumps of the low-pressure venous and lymphatic systems. Diaphragms and the body core maintain pressure differentials to facilitate flow of the low-pressure circulatory system. Inhalation and exhalation movements are coupled with this fluid flow mechanism (Knott et al. 2005, Lattuada 2006). Based on clinical experience, it is theorized that in order to maximize the potential of these physiological processes (and thoracic diaphragm function in particular) the pelvis, vertebral column and thorax must be functionally flexible and balanced, to maintain appropriate muscle tone. One therapeutic goal of osteopathic manipulation is enhancing pumping action of the musculoskeletal system to aid the return of venous and lymphatic flow to the heart and the reduction of the ‘work’ of breathing, by increasing the efficiency of each breath.
The balance and maintenance of negative pressures of the thorax and the pelvis depend on efficient and related functions of both the respiratory and pelvic diaphragms. Pelvic congestion, lower extremity oedema, pelvic inflammation and infection are relieved not only when mechanical obstructions are cleared, but also when the blood can deliver nutrition to tissues and, along with the lymph system, remove toxic products of metabolism. Exercise influences the pelvic diaphragm from below to stimulate pumping actions to move fluids (Hodges et al. 1997, Hodges & Richardson 1997) and therefore is an important component of the patient care plan.
Another, and primary, area to be treated in order to move body fluids to reduce inflammation and oedema is the thoracic inlet (Zink 1973, Hodges et al. 2003). By first relieving back pressure caused by fascial restrictions in the left and right supraclavicular fossae and around the left and right first ribs, referred to as ‘opening’ the thoracic inlet (the area of terminal lymphatic drainage), then relieving myofascial restrictions in the abdominal and pelvic diaphragms, it is theorized that fluid congestion in the pelvis is better able to drain. After addressing other restrictions – skeletal, arthrodial, ligamentous, fascial – a lymphatic pump would extend the benefit of continued fluid motion, augmented by respiration and posture (Nicholas & Oleski 2002, Knott et al. 2005).
Neurological model
The neurological model of osteopathic treatment strives to address autonomic imbalance, relieve peripheral and central sensitization and alleviate pain. Viscerosomatic reflexes, when successfully treated, reduce residual effects in somatic structures that have resulted from a visceral problem; or the viscus may be influenced as a result of stimulation of somatovisceral reflexes (Patterson & Howell 1992, Jänig 2008). Sympathetic nerve supply to pelvic organs is primarily from the thoracolumbar spine. Somatic dysfunction of this area could refer pain to the pelvis (Beal 1985, Patterson & Howell 1992). However, the parasympathetic supply to the pelvis is primarily through the pelvic nerves (S2–4). Somatic dysfunction of the sacrum theoretically could affect bladder (Weiss 2001, Arab et al. 2010) and bowel (Ng 2007) function, as well as influence dysmenorrhoea (Holtzman et al. 2008) and dyspareunia (Gentilcore-Saulnier et al. 2010) through somatovisceral reflexes (Patterson & Howell 1992, Jänig 2008). One purpose of treating the sacrum from the neurological perspective would be to rule out mechanical causes of the PGP. This is particularly useful when the pain is not relieved by OMT, forcing the astute clinician to consider organ dysfunction as a possible generator of pelvic pain through viscerosomatic reflexes (Patterson & Howell 1992) or through central sensitization (Winkelstein 2004, Howell & Willard 2005).
Additional manual approaches to PGP include deep inhibition of myofascial trigger points located on muscles and fascias on the pelvic floor, which are attached to bones of the pelvic girdle (Anderson et al. 2009) (see Chapters 14 and 15). Some of these trigger points may refer pain to other muscles in the pelvis. Relief of these myofascial trigger points through physical therapeutics may also decrease pain sensations related to bladder function, as in the case of patients with interstitial cystitis (Weiss 2001). The points may be located externally on the pelvis, or internally in the vagina. In addition to relieving PGP and chronic pelvic pain, urogenital function may also improve from specific myofascial manual therapy (FitzGerald et al. 2009).
Counterstrain tenderpoints, on the other hand, do not refer pain to other structures. These tenderpoints were empirically identified in the clinical practice of Lawrence Jones, in the 1950s. Dr. Jones found that certain points that were sensitive to digital provocation were relieved (by at least 70%) during sustained passive positioning (from up to 90–120 seconds) of the body in postures. Subsequent evaluation commonly notes reduced sensitivity and enhanced mobility and functionality of soft tissues and associated joints (Dardzinski et al. 2000, Lewis & Flynn 2001, Speicher et al. 2004). There are also many hypotheses regarding the mechanisms that might explain how strain–counterstrain works. Most researchers consider that modified nociception, as well as the Golgi tendon organ, and alpha Ia afferent and gamma efferents are involved (Bailey & Dick 1992). The exact mechanism of action of the relationship between somatic tender, or trigger, points and somatic and visceral pain and function continues to be investigated (Patterson & Howell 1992, Meltzer & Standley 2007).
Metabolic energy model
The metabolic energy approach to treating pelvic pain addresses hormonal and biochemical factors that influence pelvic girdle pain. In patients with musculoskeletal complaints who only temporarily respond to manipulative treatment, in spite of correctly addressing somatic dysfunctions, it might be useful to consider, for example, investigating thyroid dysfunction, calcium levels, vitamin D levels, abnormal cortisol levels or diabetes (Goldman et al. 2008). Frequently these patients complain of muscle weakness or general fatigue. On palpatory evaluation, changes in tissue texture may lead one to consider laboratory evaluation of a metabolic problem influencing a structural problem (i.e. osteoporosis). In females, oestrogen and relaxin hormones may alter ligament function during and after the childbearing years. In such individuals, in addition to treating hormonal imbalances, nutritional counselling to obtain optimal weight for her age, a practitioner would also advise the patient about types of exercises for weight maintenance, structural stability and flexibility. The patient would also benefit from evaluation of her posture and gait to reduce musculoskeletal strains and injuries.
Consider also a patient with compromised cardiopulmonary function who has PGP and dysfunction that increases the effort of sitting and ambulating, thus taxing the energy economy of the entire musculoskeletal system while exerting excessive energy demand on the heart and lungs. The management plan needs to be modified for patients with cardiopulmonary intolerance to exercises and manual treatments that depend on patient force, such as muscle energy techniques. The practitioner should control the amount of counterforce provided by the patient depending on patient comfort and tolerance without compromising efficacy. Patient respiratory and ocular motion assists (synkinesis) can be utilized to facilitate energy conservation as needed in select patients (Lewit et al. 1997).
Behavioural model
The behavioural model of osteopathic care strives to identify mind–body issues affecting pelvic girdle pain. Thoughts and emotions related to pain are explored to discover a possible somatic component to the problem. Chronic pain is a factor in treating depression. Sleep becomes disrupted, causing increased fatigue and pain (Goldman et al. 2008, Tibbits 2008). Discussion about medical treatment including pain relief medication, hormone replacement therapy, antidepressants and anti-anxiety agents should also include concern about self- or over-medication. Recommendations for care might include counselling, supportive care and an exercise programme to keep active to tolerance (Tettambel 2007). Osteopathic treatment may relieve fascial strains to aid relaxation or reduce anxiety; it may not fully alleviate PGP. Behavioural changes of the patient may help the individual accept the complexity of the symptoms and possibly a long course of treatment.
The cause of low back pain in general is of unknown aetiology in 85% of patients (Deyo & Weinstein 2001) and is feared by 40% of sufferers to be a sign of a serious problem (Waddell 1998); thus, reassurance is one of the most important aspects of the management plan. Vleeming et al. (2007) address this directly in terms of psychosocial and emotional aspects of body–mind medicine. In lumbopelvic girdle pain, imbalance and dysfunction alter gait, posture, functional capacities and other essential tasks that can shift a person’s outlook as well as presentation of ability to others.
A key component of the osteopathic examination of the patient with pelvic girdle pain is to make an accurate diagnosis and propose a rational management plan. Establishing a trusting doctor–patient relationship and assuring dedication to helping the patient alleviate pain is critical to successful management of the problem. Indeed, the patient’s belief in the possibility of improvement (i.e. hope) has been demonstrated to be a predictor of clinical significance in women having PGP postpartum (Vøllestad & Stuge 2009).
Case study 14.1: Male
• Neurological examination is negative for eliciting any deficiencies in motor strength, sensation or coordination.
• In the standing postural assessment, his thoracic kyphosis is flattened and his head is held anterior to the lateral postural line of gravity. He has a right convex scoliosis at the thoracolumbar junction from T10–L2 with apex at T12.
• His gait appears normal and gross range of motion of the upper and lower extremities is full.
• Seated and supine active and passive straight leg raising tests are negative for shooting posterior leg pain at 70° bilaterally.
• There are no signs of a short leg.
• The right hamstring muscle group is more hypertonic than the left.
• His pelvic anatomic landmarks, including iliac crest levels, anterior posterior diameter between posterior superior iliac spines and anterior iliac spines are asymmetrical; his right hemipelvis is noticeably smaller than the left side.
• Motion restriction is present at the lumbosacral and SIJs and pubic symphysis. He has a lumbosacral torsion and an iliosacral shear.
• Muscle imbalances are present in the psoas, multifidi, erector spinae, quadratus lumborum, piriformis and gluteus medius muscles.
• On the seated examination, his L5 is found to be flexed, rotated left, sidebent left; the sacrum is rotated right on a left oblique axis; L4 is also rotated left; L3 is flexed, rotated right, sidebent right; T10–L2 is neutral, rotated right, sidebent left.
• The left piriformis and psoas muscles are tense and tender, and have decreased range of motion. The right inferior surface of the posterior superior iliac spine, right side of the L5 spinous process and the left iliolumbar ligament are tender to palpation.
• Backward bending in the prone position causes the sacrum to rotate more to the right and the lumbosacral posterior-anterior spring test is positive (resistant).
• The right thoracic diaphragm and right pelvic diaphragm excursions are restricted during exhalation.
• The left thoracic spine between T4 and T8 is neutral, rotated left, sidebent right. T2 is extended, rotated right, sidebent right. The right first rib is elevated, with hypertonic and tender middle scalene muscles. The cervical spine is restricted at C3–6 possibly due to the scalene muscle spasm. The atlantoaxial joint is rotated left and the occipitoatlas joint is extended, rotated right, sidebent left. The right posterior quadrant of the cranium has decreased compliance compared to the contralateral side.
• Myofascial release to the thoracolumbar fascia (see Figure 14.1);
• Muscle energy techniques for the lumbosacral somatic dysfunction (see Figure 14.2 and video link 1)![]() ;
;
• HVLA for the pelvic shear (see Figure 14.3 and video link #2)![]() ;
;
• Functional technique for the lumbar spine dysfunction (see Figure 14.4 and video link #3)![]() ;
;
• Strain–counterstrain for the piriformis tender points (see Figure 14.5 and video link #4)![]() ;
;
• Muscle energy treatment to stretch the hypertonic psoas muscles (see Figure 14.6);
• Muscle energy for the pubic dysfunction (see Figure 14.7);
• Muscle energy for lumbar spine somatic dysfunction with the patient in the seated position was performed at times during his treatments, as depicted in Figure 14.8 and video link #5![]() ;
;
• HVLA for the lumbar spine somatic dysfunctions with the patient sidelying was used often as depicted in Figure 14.9 and video link #7a![]() ;
;
• Soft tissue massage for the thoracic and lumbar paraspinal muscle hypertonicity (see video link #6)![]() ;
;
• HVLA for the cervical spine somatic dysfunction;
• Muscle energy for the costal cage dysfunctions;
• Balanced membranous tension for the cranium somatic dysfunctions.

Figure 14.8 • Muscle energy for lumbar spine somatic dysfunction with the patient in the seated position
From the neurological perspective, most commonly, PGP involving the SIJ is accompanied by pain radiating no further down the leg than the knee (Szadek et al. 2009). However, this patient had non-painful paraesthesias to the foot. This suggested that there was a neurological root being compromised at S1 or the sciatic nerve itself was irritated as it passes by, or through, the piriformis muscle (Boyajian-O’Neill et al. 2008). To decrease lumbosacral pain and peripheral sensitization, tenderness was reduced with strain–counterstrain techniques for the sacral and lumbar regions, including the piriformis muscle tender point. The urinary urgency sensation resolved a couple of days after the somatic dysfunctions resolved (somatovisceral reflex), possibly due to a decrease in afferent stimuli from the joint and soft tissue nociceptors in the spine and pelvis (Howell & Willard 2005).
For improvement in respiration–circulation, myofascial release was provided for the lumbodorsal fascia, the thoracic inlet, and thoracic and pelvic diaphragm somatic dysfunctions. Muscle energy was used to release the scalene spasm. Improved costal cage and diaphragm motion was restored to maximize respiratory function (see also Chapter 12).
Metabolic treatment with testosterone supplementation helped restore muscle wasting (Bassil et al. 2009), but since he had an asymmetry of muscle mass due to his scoliotic lumbosacral spine mechanics, he had an increase in his asymmetric paraspinal thoracolumbar muscle mass with increasing doses of testosterone, which made him uncomfortable and in more pain. OMT did not help decrease the hypertonicity or hypertrophy of the thoracolumbar muscle mass, but decreased doses of testosterone did. Subsequently, OMT was effective in relieving pain and improving muscle balance and lumbopelvic stability in posture and motion. Urinary urgency symptoms diminished as well.
Home exercise programme
A detailed history should ascertain whether remote injuries, procedures or events might inform the current presentation in ways that impact function or expectation. Setting attainable short- and long-term goals and reviewing them periodically helps track and quantify clinical and personal success. Age, gender, chronicity and expectations are factors to consider when setting goals. Specific therapeutic measures may target distinct clinical presentations such as piriformis syndrome, trochanteric bursitis, iliopectineal bursitis, osteitis pubis, groin or thigh strains, and other pelvic girdle conditions (DePalma 2001).
Individualized exercise programme prescriptions can help people improve mobility, stretching and strengthening of the lumbopelvic region. When designing a programme, it is necessary to consider the structural components and their attachments while testing to determine functional compromise, imbalance or pain provocation guide exercise selection. It is helpful to consider the sequencing of exercises by introducing relaxed breathing first to promote functional releasing of regional tension (Vleeming et al. 2007). Stretching sequentially can facilitate mobilization; Sahrmann (2001) advocates addressing the hip flexors and anterior capsule, then piriformis, and then hamstrings, first in passive and then progressively independent active activation. Following Janda’s guidelines (1977, 1986), Isaacs and Bookhout (2002) and Greenman (2003) propose that muscle groups that are commonly tight release well when agonist–antagonist groups are treated by alternate contract–release intervals, as in muscle energy technique (see Chapter 11 and elsewhere in this chapter).
The effect of exercise on women with postpartum PGP has been evaluated in two randomized controlled trials (Mens et al. 2000, Stuge et al. 2004a, 2004b). In 2006 Stuge and colleagues compared the studies to determine variant findings (Stuge et al. 2006). Overall, the studies demonstrated that the group of women that performed specific stabilizing exercises reported lower pain and disability ratings and higher quality of life for the duration of the study and for 1–2 years postpartum.
Stuge and colleagues (Stuge et al. 2004a, 2004b) chose Lee and Vleeming’s integrated model (1998) of self-expansion, where components of form closure and force closure are augmented by motor control and an appreciation of emotions and awareness related to pelvic girdle stability. The pelvic girdle’s structural elements comprise what Lee calls a Circle of Integrity. In the Stuge group’s protocol, greater emphasis was placed on deep core local muscles and the larger torque-producing global muscle systems in order to stabilize the spine as well as the pelvic girdle (Figure 14.10). Coordinated motor activation was emphasized and individualized during training to promote improved motor control of the deeper core muscles independent of superficial muscles (see Box 14.4). Asymmetric SIJ motion called for muscle energy mobilization by the individuals or by their therapist. Three sets of ten repetitions were performed by participants three times a week, and intensity was scaled to avoid lumbopelvic trembling or uncomfortable pain sensations during or after training. Preloading of superficial muscles before global muscle recruitment was encouraged to promote stability instead of rigidity.
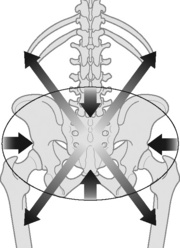
Figure 14.10 • An illustration of muscles with implication for lumbopelvic stability and control. Short arrows indicate deep local muscles (the transverse abdominals, the multifidus, diaphragm and the pelvic floor muscles). Long arrows indicate the posterior oblique muscle sling with latissimus dorsi, gluteus maximus and the intervening thoracolumbar fascia (Stuge et al. 2006)
Box 14.4 The abdominal rectus sheath
The abdominal rectus sheath, also known as the ‘six-pack’ of buff bodybuilders, is the anterior superficial layer overlying the true core abdominal muscles: transversus abdominis internal and external obliques. These layers form a three-ply wrap of muscles from the lumbar spine and thoracolumbar fascia behind, to the pubic rami, thoracic costal outlet and linea alba in front, supported from below by the coordinated activity of the pelvic floor. The multifidus muscles at the base of the lumbosacral spine comprise 90% of the caudal sacral paraspinal musculature (Mitchell 2001).
Exercise regimens and therapeutic options
The pelvic girdle is a parabolic bowl capable of integrated load distribution through form closure, force closure and motor control. Hence, rehabilitation of the patient with PGP integrates functional and structural elements by manipulation, manual treatments and individualized exercise programmes. Progressive exercise programmes for dynamic lumbopelvic stabilization have been recommended by Lee (2004), Liebenson (2003, 2004, 2007, 2008, 2010), Creager (2001), Akuthota et al. (2008), Cusi (2010a) and many others. Cusi simplifies the regimen: After diagnosing the type, location, and extent of ‘load transfer failure’, a specific, targeted and progressive treatment programme consisting of exercise and other therapeutics is started. The exercise regimen he proposes has three steps:
1. Isolation. Engage the involved structures to restore deep core strength and reduce faulty global recruitment (Lee’s ‘downtraining’) so that the person learns ‘neutral’ lumbopelvic positioning (slight lumbar lordosis, or 12 o’clock for the pelvic clock).
2. Combination. Improve endurance and coordination by progressive challenges such as adding limb movements while maintaining the core and breathing.
3. Function. Progress to functional activities of daily living, work and recreation. If structural integrity is not consistently maintained despite consistent effort and appropriate programme practice, direct stabilization of disrupted tissues may be attained by use of prolotherapy before resorting to surgery (Dagenais et al. 2007, Cusi et al. 2010b).
Exercise equipment such as balls, resistance bands and foam rolls may provide additional learning opportunities (Creager 1994, 1998, 2001, Leibenson 2010). Liebenson (2008) recommends stabilizing the entire lumbopelvic region by training in ‘abdominal brace’ methods of all-around co-activation. Pelvic belts might help certain individuals improve stability while regaining internal strength and stamina (or until postpartum) (Nillson-Wickmar et al. 2005).
Exercises for the pelvic girdle, lumbar spine and hips are best addressed as a unity comprising components (Lee 2004). After establishing which structures are involved (form control), determine faulty function (force control) and disproportional global and local muscle recruitment (motor control). Breath and relaxation training add the fourth element (emotions and awareness) to the integrated model (Lee 2004, Vleeming et al. 2007).
Certain principles are common to treatment programmes:
The first step of the exercise regimen is learning neutral spine mechanics, a process of tilting the pelvis anteriorly and cephalad in a symmetrical and controlled manner. The desired small amount of lumbar lordosis is maintained while the person breathes; this position corresponds to 12 o’clock of a pelvic clock (a figurative clock on the person’s belly facing forward) (Sahrmann 2001, Isaacs & Bookhout 2002, Greenman 2003). This is accomplished by co-contracting the transversus abdominis and multifidus muscles simultaneously; learning to do this is facilitated by in-session training and take-home exercises (Creager 2001, Lee 2004, Vleeming et al. 2007). Following Janda’s lead, Liebenson (2007) advances the classic TrA-MF focus to performing circumferential contraction of the entire abdominal wall as an ‘abdominal brace’ that provides stability while a person is responding to postural perturbations. Kinesthetic awareness can be facilitated if the individual self-monitors smooth and even movement at the anterior superior iliac spines while moving from 12 to 6 o’clock, 3 (left) to 9 (right) o’clock, and then through clockwise and counterclockwise rotations while keeping the pelvis on the exercise surface instead of bridging (Isaacs & Bookhout 2002).
Once neutral spine and clock movements are coordinated with breathing, this kinesthetic awareness is applied to dynamic lumbopelvic core stabilization movements involving the limbs while the person is supine, prone, on all fours (quad position) or standing. Liebenson (2008) cites McGill (1995, 1998) who found that safe loading of the lumbopelvic region is accomplished with quad single leg raise, opposite arm/leg raise, side bridge on knees or on ankles, and curl-up positions. Good form is essential and should be the emphasis from the start rather than the number of repetitions. McGill (2007) recommends doing cat-cow in quad position 8–10 times to warm up, then doing three sets of a ‘reverse pyramid’ (15, 12, and then eight repetitions) of any manoeuvre. Liebenson (2007, 2008) outlines ‘stability training variables’ to promote satisfactory motor control and movement pattern re-education:
• Intensity: submaximal, less than 50% of single repetition maximum.
• Sets and repetitions: start with one set of approximately six repeats, then progress to 15 repeats, then McGill’s reverse pyramid.
• Hold times: emphasize endurance by holding for 1–2 breaths (6–10 s).
• Form: movements should be performed slowly with appropriate form for motor control training and injury prevention.
• Frequency: daily or twice a day.
• Duration: improvement noted after consistent performance for at least 3 months.
• Goals: structural stability and functional improvement should reach individualized needs for performance capacities and activities of daily living.
Liebenson provides examples of several exercises to add: side-lying bridges, bird-dog quad elevation of opposite arm and leg, and dying bug supine activation of the limbs bent and extended (Liebenson 2008). Supine bridges can be performed with or without a ball between the knees or resistance band around them (Creager 1994, Liebenson 2007); pubic symphysis self-mobilization can be done from this position if the person exhales while contracting knees together into the ball or apart into the band. Creager (1994, 1998, 2001) and Lee (2004) provide many other progressive exercise routines using equipment such as balls and resistance bands. Liebenson (2010) implements foam roll exercises. A person is encouraged to progress to integrating dynamic core stabilization principles and practices into functional and occupational activities that can be performed as an independent home programme.
Elden et al. (2008a, 2008b) has found that both acupuncture and stabilizing exercises are safe treatments for pregnant women having PGP without increased fetal risk; with repeated clinical assessment, nearly all of the women in the study were found to be pain-free 12 weeks after giving birth. Schlinger (2006) finds that Feldenkrais, Alexander Technique and yoga body-awareness approaches are useful adjuncts to medical care.
Independent home exercise programmes must be done consistently at least 3 days per week, with additional activities or sports participation as tolerated. Granath et al. (2006) found that healthy pregnant women who participated in water aerobics once a week reported less back pain or absenteeism than those women doing land-based exercises once a week. DiFrancisco-Donoghue et al. (2007) conducted strength training in older adults (65–79 years old) and found that once or twice weekly produced similar levels of health and functional benefit. The adage ‘you rest, you rust’ has been confirmed by an animal model showing that exercise reduces joint stiffness after blunt trauma (Weaver & Haut 2005).
Akuthota V., Ferreiro A., Moore T., et al. Core stability exercise principles. Curr. Sports Med. Rep.. 2008;7(1):39-44.
Anderson R.U., Sawyer T., Wise D., Morey A., et al. Painful myofascial trigger points and pain sites in men with chronic prostatitis/chronic pelvic pain syndrome. J. Urol.. 2009;182(6):2753-2758.
Arab A.M., Abdollahi I., Joghataei M.T., et al. Inter and intra examiner reliability of single and composites of selected motion palpation and pain provocation tests for sacroiliac joint. Man. Ther.. 2009;14(2):213-221.
Arab A.M., Behbahani R.B., Lorestani L., et al. Assessment of pelvic floor muscle function in women with and without low back pain using transabdominal ultrasound. Man. Ther.. 2010:1-5. Jan 18[Epub ahead of print]
Bahr R., Andersen S.O., Løken S., et al. Low back pain among endurance athletes with and without specific back loading: a cross-sectional survey of cross-country skiers, rowers, orienteerers, and nonathletic controls. Spine. 2004;29(4):449-454.
Bailey H.W., Beckwith C.G. Short leg and spinal anomalies: their incidence and effects on spinal mechanics. In: Peterson B., editor. 1983. Postural balance and Imbalance. Indianapolis: American Academy of Osteopathy; 1937:63-70.
Bailey M., Dick L. Nociceptive considerations in treating with counterstrain. J. Am. Osteopath. Assoc.. 1992;92(3):334-341.
Barney S.P. Pelvic masses. Med. Clin. North Am.. 2008;92(5):1143-1161.
Bassil N., Alkaade S., Morley J.E. The benefits and risks of testosterone replacement therapy: a review. Ther. Clin. Risk Manage.. 2009;5(3):427-448.
Beales D.J., O’Sullivan P.B., Briffa N.K. Motor control patterns during an active straight leg raise in pain-free subjects. Spine. 2009;34(1):E1-E8. Spine
Beales D.J., O’sullivan P.B., Briffa N.K. Motor control patterns during an active straight leg raise in chronic pelvic girdle pain subjects. Spine. 2009;34(9):861-870. Spine
Beal M.C. The sacroiliac problem: Review of anatomy, mechanics, and diagnosis. J. Am. Osteopath. Assoc.. 1982;81:667-679.
Beal M.C. Viscerosomatic reflexes: A review. J. Am. Osteopath. Assoc.. 1985;85:786-801.
Biering-Sorensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine. 1984;9:106-119.
Bo K., Backe-Hansen K. Do elite athletes experience low back, pelvic girdle and pelvic floor complaints during and after pregnancy? Scand. J. Med. Sci. Sports. 2007;17(5):480-487.
Boyajian-O’Neill L., McClain R., Coleman M., et al. Diagnosis and management of piriformis syndrome: an osteopathic approach. J. Am. Osteopath. Assoc.. 2008;108:657-664.
Boyle K.J. Benign gynecologic conditions. Surg. Clin. North Am.. 2008;88(2):245-264.
Bronfort G., Haas M., Evans R.L., et al. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: A systematic review and best evidence synthesis. Spine J.. 2006;4:335-356.
Browning J.E. Mechanically induced pelvic pain and organic dysfunction in a patient without low back pain. J. Manipulative Physiol. Ther.. 1990;13(7):406-411.
Chen C.H., Huang M.H., Chen T.W., et al. Relationship between ankle position and pelvic floor muscle activity in female stress urinary incontinence. Urology. 2005;66(2):288-292.
Creager C.C. Therapeutic Exercises Using the Swiss Ball. Berthoud, Colorado: Executive Physical Therapy, Inc; 1994.
Creager C.C. Therapeutic Exercises Using Resistive Bands. Berthoud, Colorado: Executive Physical Therapy, Inc; 1998.
Creager C.C. Bounce Back Into Shape After Baby: The Ultimate Guide to aFun-Filled, Time and Energy Efficient Workout – With Your Baby. Berthoud, CO: Executive Physical Therapy, Inc; 2001.
Cusi M.F. Paradigm for assessment and treatment of SIJ mechanical dysfunction. J. Bodyw. Mov. Ther.. 2010;14(2):152-161.
Cusi M., Saunders J., Hungerford B., et al. The use of prolotherapy in the sacroiliac joint. Br. J. Sports Med.. 2010;44(2):100-104.
da Costa B.R., Vieira E.R. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am. J. Ind. Med.. 2009;14:1-39.
Dagenais S., Mayer J., Wooley J., et al. Safety and toxicity of prolotherapy for back pain. In: Vleeming A., Mooney V., Cusi M., editors. Sixth Interdisciplinary World Congress on Low Back & Pelvic Pain. Diagnosis and Treatment; the Balance Between Research and the Clinic. Barcelona, Spain: ECO, 2007.
Daly J.M., Frame P.S., Rapoza P.A. Sacroiliac subluxation: a common, treatable cause of low-back pain in pregnancy. Fam. Pract. Res. J.. 1991;11(2):149-159.
Damen L., Buyruk H., Güler-Uysal F., et al. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet. Gynecol. Scand.. 2001;80(11):1019-1024.
Dardzinski J.A., Ostrov B.E., Hamann L.S. Myofascial pain unresponsive to standard treatment: Successful use of a strain and counterstrain technique with physical therapy. J. Clin. Rheumatol.. 2000;6(4):169-174.
DeMann L.E.Jr. Sacroiliac dysfunction in dancers with low back pain. Man. Ther.. 1997;2(1):2-10.
DePalma B. Rehabilitation of the groin, hip, and thigh. In: Prentice W.E., editor. Techniques in Musculoskeletal Rehabilitation. New York: McGraw-Hill; 2001:509-525.
Deyo R.A., Weinstein J.N. Low back pain. N. Engl. J. Med.. 2001;344(5):363-370.
DiFrancisco-Donoghue J., Werner W., Douris P.C. Comparison of once-weekly and twice-weekly strength training in older adults. Br. J. Sports Med.. 2007;41(1):19-22.
Dinnar U., Beal M.C., Goodridge J.P., et al. Description of fifty diagnostic tests used with osteopathic manipulation. J. Am. Osteopath. Assoc.. 1982;81:314-321.
DonTigny R.L. Critical analysis of the functional dynamics of the sacroiliac joints as they pertain to normal gait. J. Orthopedic Med.. 2005;27:3-10.
DonTigny R.L. Pathology of the sacroiliac joint and its effect on normal gait. J. Orthopedic Med.. 2005;27:61-69.
Downey H.F., Durgam P., Williams A.G.Jr., et al. Lymph flow in the thoracic duct of conscious dogs during lymphatic pump treatment, exercise, and expansion of extracellular fluid volume. Lymphat. Res. Biol.. 2008;6(1):3-13.
Eberhard-Gran M., Eskild A. Diabetes mellitus and pelvic girdle syndrome in pregnancy. Is there an association? Acta Obstet. Gynecol. Scand.. 2008;87(10):1015-1019.
Educational Council on Osteopathic Principles (ECOP). Core Curriculum Outline. Washington, DC: American Association of Colleges of Osteopathic Medicine; 1987.
Educational Council on Osteopathic Principles (ECOP). Glossary of Osteopathic Terminology. Washington, DC: American Association of Colleges of Osteopathic Medicine; 2009.
Elden H., Ostgaard H.C., Fagevik-Olsen M., et al. Treatments of pelvic girdle pain in pregnant women: adverse effects of standard treatment, acupuncture and stabilizing exercises on the pregnancy, mother, delivery and the fetus/neonate. BMC Complement. Altern. Med.. 2008;8:34. Jun 26
Elden H., Hagberg H., Olsen M.F., et al. Regression of pelvic girdle pain after delivery: follow-up of a randomized single blind controlled trial with different treatment modalities. Acta Obstet. Gynecol. Scand.. 2008;87(2):201-208.
Esquinazi A., Mukul T. Gait analysis: technology and clinical applications. In: Braddom R.L., editor. Physical medicine and rehabilitation. third ed. Philadelphia: Saunders; 2008:93-110.
Fall M., Baranowski A.P., Elneil S., et al. Guidelines on Chronic Pelvic Pain. European Association of Urology. Eur. Urol.. 2010;57:35-48.
Ferreira M.L., Ferreira P.H., Latimer J., et al. Efficacy of spinal manipulative therapy for low back pain of less than three months’ duration. J. Manipulative Physiol. Ther.. 2003;26:593-601.
FitzGerald M.P., Anderson R.U., Potts J. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J. Urol.. 2009;182(2):570-580.
Fryer G., Morris T., Gibbons P. Relation between thoracic paraspinal tissues and pressure sensitivity measured by digital algometer. Journal of Osteopathic Medicine. 2004;7(2):64-69.
Fryer G., Morris T., Gibbons P. Paraspinal muscles and intervertebral dysfunction: Part two. J. Manipulative Physiol. Ther.. 2004;27(5):348-357.
Fryer G., Morris T., Gibbons P. The relationship between palpation of thoracic tissues and deep paraspinal muscle thickness. Int. J. Osteopathic Med.. 2005;8(1):22-28.
Fryer G., Morse C.M., Johnson J.C. Spinal and sacroiliac assessment and treatment techniques used by osteopathic physicians in the United States. Osteopathic Med. Primary Care. 2009;3:4.
Gabbe S.G., editor, Skeletal and Postural Changes. fifth ed. Williams’ Obstetrics: Normal and Problem Pregnancies. Philadelphia: Elsevier; 2007. (Chapter 3)
Gentilcore-Saulnier E., McLean L., Goldfinger C. Pelvic floor muscle assessment outcomes in women with and without provoked vestibulodynia and the impact of a physical therapy program. J. Sex. Med.. 2010. Jan 6 [Epub ahead of print]
Goldman L., Ausiello D., editors, Cecil’s Textbook of Internal Medicine. twenty-third ed. Philadelphia: Elsevier; 2008:1663. 1700–1708, 1761–1767, 1897–1906, 2078–2083
Goodridge J.P. Muscle energy technique: definition, explanation, methods of procedure. J. Am. Osteopath. Assoc.. 1981;81(4):249-253.
Granath A.B., Hellgren M.S., Gunnarsson R.K. Water aerobics reduces sick leave due to low back pain during pregnancy. J. Obstet. Gynecol. Neonatal Nurs.. 2006;35(4):465-471.
Greenman P.E. Syndromes of the lumbar spine, pelvis, and sacrum. Phys. Med. Rehabil. Clin. North Am.. 1996;7:773-785.
Greenman P.E. Principles of Manual Medicine, third ed. Philadelphia: Lippincott, Williams & Wilkins; 2003.
Gutke A., Josefsson A., Oberg B. Pelvic girdle pain and lumbar pain in relation to postpartum depressive symptoms. Spine. 2007;32(13):1430-1436.
Gutke A., Kjellby-Wendt G., Oberg B. The inter-rater reliability of a standardized classification system for pregnancy-related lumbopelvic pain. Man. Ther.. 2009. Jul 24 [Epub ahead of print]
Hancock M.J., Maher C.G., Latimer J., et al. Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur. Spine J.. 2007;16:1539-1550.
Haneline M.T., Young M. A review of intraexaminer and interexaminer reliability of static spinal palpation: a literature synthesis. J. Manipulative Physiol. Ther.. 2009;32(5):379-386.
Hayes N.M., Bezilla T.A. Incidence of iatrogenesis associated with osteopathic manipulative treatment of pediatric patients. J. Am. Osteopath. Assoc.. 2006;106(10):605-608.
Hestbaek L., Leboeuf-Yde C. Are chiropractic tests for the lumbo-pelvic spine reliable and valid? A systematic critical literature review. J. Manipulative Physiol. Ther.. 2000;23:258-275.
Hincapié C.A., Morton E.J., Cassidy J.D. Musculoskeletal injuries and pain in dancers: A systematic review. Arch. Phys. Med. Rehabil.. 2008;89(9):1819-1829.
Hodge L.M., King H.H., Williams A.G.Jr., et al. Abdominal lymphatic pump treatment increases leukocyte count and flux in thoracic duct lymph. Lymphat. Res. Biol.. 2007;5(2):127-133.
Hodges P.W., Mosely G.L. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J. Electromyogr. Kinesiol.. 2003;13:361.
Hodges P.W., Richardson C.A. Contraction of the abdominal muscles associated with movement of the lower limb. Phys. Ther.. 1997;77:132.
Hodges P.W., Gandevia S., Richardson C.A. Contractions of specific abdominal muscles in postural tasks are affected by respiratory maneuvers. J. Appl. Physiol.. 1997;83(3):753.
Holtzman D.A., Petrocco-Napuli K.L., Burke J.R. Prospective case series on the effects of lumbosacral manipulation on dysmenorrhea. J. Manipulative Physiol. Ther.. 2008;31(3):237-246.
Howell J.N., Willard F. Nociception: New understandings and their possible relation to somatic dysfunction and its treatment. Ohio Res. and Clin. Rev.. 2005;15:12-15.
Hruby R.J. Pathophysiologic models: aids to the selection of manipulative techniques. Am. Acad. Osteopathy J.. 1991;1(3):8-10.
Hruby R.J. Pathophysiologic models and the selection of osteopathic manipulative techniques. J. Osteopath. Med.. 1992;6(4):25-30.
Hruby R.J. Osteopathic medicine and the geriatric patient. Am. Acad. Osteopathy J.. 2008;18(3):16-20.
Hu H., Meijer O.G., van Dieën J.H., et al. Muscle activity during the active straight leg raise (ASLR), and the effects of a pelvic belt on the ASLR and on treadmill walking. J. Biomech.. 2010;43(3):532-539.
Hungerford B., Gilleard W., Lee D. Altered patterns of pelvic bone motion determined in subjects with posterior pelvic pain using skin markers. Clin. Biomech.. 2004;19(5):456-464.
Isaacs E.R., Bookhout M.R. Bourdillon’s Spinal Manipulation. sixth ed. Boston: Butterworth/Heinemann; 2002:283-314.
Janda V. Muscles, central nervous motor regulation and back problems. In: Korr I.M., editor. The Neurobiologic Mechanisms in Manipulative Therapy. New York: Plenum Press; 1977:27-41.
Janda V. Muscle weakness and inhibition (pseudoparesis) in back pain syndromes. In: Grieve G.P., editor. Modern Manual Therapy of the Vertebral Column. Edinburgh: Churchill Livingstone; 1986:197-201.
Jänig W. Pain in the sympathetic nervous system: pathophysiological mechanisms. In Mathias C.J., Bannister R., editors: Autonomic Failure, fifth ed., New York: Oxford University Press, 2008.
Jordan T.R. Conceptual and treatment models in osteopathy II: Sacroiliac mechanics revisited. Am. Acad. Osteopathy J.. 2006;16(2):11-17.
Juhl J.H., Ippolito Cremin T.M., Russell G. Prevalence of frontal plane pelvic postural asymmetry – part 1. J. Am. Osteopath. Assoc. 2004;104;(10):411-421.J. Am. Osteopath. Assoc.. 2005;105(1):5. Erratum in:
Kerrigan D., Della Croce U., Carciello M., et al. A revised view of the determinants of gait: significance of heel rise. Arch. Phys. Med. Rehabil.. 2000;81:1077-1080.
Kerrigan D., Riley P., Lelas J., et al. Quantification of pelvic rotation as a determinant of gait. Arch. Phys. Med. Rehabil.. 2001;82:217-220.
Kimberly P. Formulating a prescription for osteopathic manipulative treatment. J. Am. Osteopath. Assoc.. 1976;75:486-499.
Knott E.M., Tune J.D., Stoll S.T., et al. Increased lymphatic flow in the thoracic duct during manipulative intervention. J. Am. Osteopath. Assoc.. 2005;105(10):447-456.
Kristiansson P., Svardsudd K. Discriminatory power of tests applied in back pain during pregnancy. Spine. 1996;21(20):2337-2343. discussion 2343–2344
Kuchera M.L., DiGiovanna E.L., Greenman P.E. Efficacy and complications. In: Ward R.C., et al, editors. Foundations for Osteopathic Medicine. second ed. Philadelphia: Lippincott, Williams & Wilkins; 2003:1143-1152.
Laslett M., Young S.B., Aprill C.N., et al. Diagnosing painful sacroiliac joints: a validity study of a McKenzie evaluation and sacroiliac joint provocation tests. Aust. J. Physiother.. 2003;49:89-97.
Laslett M., Aprill C.N., McDonald B., et al. Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man. Ther.. 2005;10:207-218.
Latthe P. Factors predisposing women to chronic pelvic pain: systematic review. Br. Med. J.. 2006;332(7544):749-755.
Lattuada M., Hedenstierna G. Abdominal lymph flow in an endotoxin sepsis model: influence of spontaneous breathing and mechanical ventilation. Crit. Care Med.. 2006;34(11):2792-2798.
Lee D.G. The Pelvic Girdle, third ed. Edinburgh: Elsevier Science; 2004.
Lee D.G., Vleeming A. Impaired load transfer through the pelvic girdle – a new model of altered neutral zone function. Proceedings from the 3rd Interdisciplinary World Congress on Low Back and Pelvic Pain. Vienna, Austria. 1998.
Lee D.G., Lee L.J., McLaughlin L. Stability, continence and breathing: The role of fascia following pregnancy and delivery. J. Bodyw. Mov. Ther.. 2008;12:333-348.
Lesho E.P. An overview of osteopathic medicine. Arch. Fam. Med.. 1999(6):477-484.
Lewis T., Flynn C. Use of strain-counterstrain in treatment of patients with low back pain. J. Manual Manip. Ther.. 2001;9(2):92-98.
Lewit K., Berger M., Holzmüller G. Breathing movements: The synkinesis of respiration with looking up and down. J. Musculoskeletal Pain. 1997;5(4):57-69.
Licciardone J.C., Brimhall A.K., King L.N. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet. Disord.. 2005;6:43. Aug 4
Licciardone J.C., Buchanan S., Hensel K.L., et al. Osteopathic manipulative treatment of back pain and related symptoms during pregnancy: a randomized controlled trial. Am. J. Obstet. Gynecol.. 2010;202(1):43.e1-43.e8.
Liebenson C. Functional training. Part 2: integrating functional training into clinical practice. J. Bodyw. Mov. Ther.. 2003;7(1):20-21.
Liebenson C. Spinal stabilization an update. Part 2: functional assessment. J. Bodyw. Mov. Ther.. 2004;8(2):199-213.
Liebenson C. Hip dysfunction and back pain. J. Bodyw. Mov. Ther.. 2007;11:111-115.
Liebenson C. A modern approach to abdominal training. Part III: Putting it together. J. Bodyw. Mov. Ther.. 2008;12:31-36.
Liebenson C. Self-management: patient section. Postural exercises on the foam roll. J. Bodyw. Mov. Ther.. 2010;14(2):203-205.
Lipton J.A., Flowers-Johnson J., Bunnell M.T., et al. The use of heel lifts and custom orthotics in reducing self-reported chronic musculoskeletal pain scores. Am. Acad. Osteopathy J.. 2009(1):15-17. 19–20
Marx S., Cimniak U., Beckert R., et al. Chronic prostatitis/chronic pelvic pain syndrome. Influence of osteopathic treatment – a randomized controlled study [Article in German]. Urologe A. 2009;48(11):1339-1345.
McGill S.M. The mechanics of torso flexion: sit-ups and standing dynamic flexion manouvres [sic]. Clin. Biomech.. 1995;10:184-192.
McGill S.M. Low back exercises: prescription for the healthy back and when recovering from injury. Resources Manual for Guidelines for Exercise Testing and Prescription. third ed. Indianapolis, IN: American College of Sports Medicine; 1998. Williams & Wilkins, Baltimore
McGill S.M. Low Back Disorders: Evidence Based Prevention and Rehabilitation, second ed. Champaign, IL: Human Kinetics Publishers; 2007.
Meleger A.L., Krivickas L.S. Neck and back pain: musculoskeletal disorders. Neurological Clinics. 2007;25(2):419-438.
Meltzer K.R., Standley P.R. Modeled repetitive motion strain and indirect osteopathic manipulative techniques in regulation of human fibroblast proliferation and interleukin secretion. J. Am. Osteopath. Assoc.. 2007;107(12):527-536.
Mens J.M.A., Snijders C.J., Stam H.J. Diagonal trunk muscle exercises in peripartum pelvic pain: a randomized clinical trial. Phys. Ther.. 2000;80(12):1164-1173.
Mitchell F.Jr. The muscle energy manual – evaluation and treatment of the pelvis and sacrum. East Lansing, Michigan: MET Press; 2001.
Mitchell F.L.Sr. Structural pelvic function. Carmel, CA: Yearbook of the American Academy of Osteopathy, American Academy of Osteopathy; 1958:71-90. (now Indianapolis)
Mottola M.F. Exercise prescription for overweight and obese women: pregnancy and post-partum. Obstet. Clin. North Am.. 2009;36(2):301-316.
Nadler S.F., Malanga G.A., Bartoli L.A., et al. Hip muscle imbalance and low back pain in athletes: influence of core strengthening. Med. Sci. Sports Exerc.. 2002;34(1):9-16.
Ng C.L. Levator ani syndrome – a case study and literature review. Aust. Fam. Physician. 2007;36(6):449-452.
Nicholas A., Oleski S. Osteopathic manipulative treatment for postoperative pain. J. Am. Osteopath. Assoc.. 2002;102(S3):S5-S8.
Nillson-Wikmar L., Holm K., Oijerstedt R., et al. Effect of three different physical therapy treatments on pain and activity in pregnant women with pelvic girdle pain: a randomized clinical trial with 3, 6, and 12 months follow-up postpartum. Spine. 2005;30(8):850-856.
O’Connell J. Bioelectric responsiveness of fascia: A model for understanding the effects of manipulation. Tech. Orthopaedics. 2003;18(1):67-73.
O’Sullivan P.B., Beales D.J. Diagnosis and classification of pelvic girdle pain disorders—Part 1: A mechanism based approach within a biopsychosocial framework. Man. Ther.. 2007;12(2):86-97.
O’Sullivan P.B., Beales D.J., Beetham J.A., et al. Altered motor control strategies in subjects with sacroiliac joint pain during the active straight-leg-raise test. Spine. 2002;27(1):E1-E8.
O-Yurvati A.H., Carnes M.S., Clearfield M.B., et al. Hemodynamic effects of osteopathic manipulative treatment immediately after coronary artery bypass graft surgery. J. Am. Osteopath. Assoc.. 2005;105(10):475-481.
Patterson M.M., Howell J.N., editors. The Central Connection: Somatovisceral/ Viscerosomatic Interaction. Indianapolis: American Academy of Osteopathy, 1992.
Pickar J.G. Neurophysiological effects of spinal manipulation. Spine J.. 2002;2:357-371.
Pool-Goudzwaard A.L., ten Hove M.C.P.H.S., Vierhout M.E. Relations between pregnancy-related low back pain, pelvic floor activity and pelvic floor dysfunction. Int. Urogynecol. J.. 2005;16:468-474.
Prather H. Recognizing and treating pelvic pain and pelvic floor dysfunction. Phys. Med. Rehabil. Clin. North Am.. 2007;18(3):477-496.
Robinson H.S., Brox J.I., Robinson R., et al. The reliability of selected motion and pain provocation tests for the sacroiliac joint. Man. Ther.. 2007;2(1):72-79.
Ronchetti I., Vleeming A., van Wingerden J.P. Physical characteristics of women with severe pelvic girdle pain after pregnancy: A descriptive cohort study. Spine. 2008;33(5):E145-E151.
Sahrmann S. Diagnosis and Treatment of Movement Impaired Syndromes. St. Louis: Mosby; 2001.
Schlinger M. Feldenkrais Method, Alexander Technique, and yoga–body awareness therapy in the performing arts. Phys. Med. Rehabil. Clin. N. Am.. 2006;17(4):865-875.
Seffinger M.A., Najm W.I., Mishra S.I., et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004;29:E413-E425.
Selkow N.M., Grindstaff T.L., Cross K.M., et al. Short-term effect of muscle energy technique on pain in individuals with non-specific lumbopelvic pain: a pilot study. J. Man. Manip. Ther.. 2009;17(1):E14-E18.
Sembrano J.N., Polly D.W.Jr. How often is low back pain not coming from the back? Spine. 2009;34(1):E27-E32.
Speicher T., et al. Effect of strain counterstrain on pain and strength in hip musculature. J. Man. Manip. Ther.. 2004;12(4):215-223.
Stochkendahl M.J., Christensen H.W., Hartvigsen J., et al. Manual examination of the spine: a systematic critical literature review of reproducibility. J. Manipulative Physiol. Ther.. 2006;29(6):475-485.
Stuge B., Laerum E., Kirkesola G., et al. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy. A randomized controlled trial. Spine. 2004;29(4):351-359.
Stuge B., Veierød M.B., Laerum E., et al. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy. A two-year follow-up of a randomized clinical trial. Spine. 2004;29(10):E197-E203.
Stuge B., Holm I., Vøllestad N. To treat or not treat postpartum pelvic girdle pain with stabilising exercises? Man. Ther.. 2006;11:337-343.
Szadek K., van der Wurff P., van Tulder M., et al. Diagnostic validity of criteria for sacroiliac joint pain: a systematic review. J. Pain. 2009;10(4):354-368.
Tettambel M.A. An osteopathic approach to treating women with chronic pelvic pain. J. Am. Osteopath. Assoc.. 2005;105(9 Suppl. 4):S20-S22.
Tettambel M.A. Using integrative therapies to treat women with chronic pelvic pain. J. Am. Osteopath. Assoc.. 2007;107(10 Suppl. 6):ES 17-20.
Tibbits G.M. Sleep disorders: causes, effects, solutions. Prim. Care. 2008;35(4):817-837.
Tong H.C., Heyman O.G., Lado D.A., et al. Interexaminer reliability of three methods of combining test results to determine side of sacral restriction, sacral base position, and innominate bone position. J. Am. Osteopath. Assoc.. 2006;106:464-468.
Van der Hulst L.A. Bad experience, good birthing: Dutch low-risk pregnant women with a history of sexual abuse. J. Psychosom. Obstet. Gynaecol.. 2006;27(1):59-66.
Van der Wurff P., Hagmeijer R.H.M., Meyne W. Clinical tests of the sacroiliac joint. A systematic methodological review. Part 1: Reliability. Man. Ther.. 2000;5(1):30-36.
Van der Wurff P., Hagmeijer R.H.M., Meyne W. Clinical tests of the sacroiliac joint. A systematic methodological review. Part 2: Validity. Man. Ther.. 2000;5:89-96.
Van der Wurff P., Buijs E.J., Groen G.J. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch. Phys. Med. Rehabil.. 2006;87:10-14.
Van Wingerden J.P., Vleeming A., Buyruk H.M., et al. Stabilization of the SIJ in vivo: verification of muscular contribution to force closure of the pelvis. Eur. Spine J.. 2004;13(3):199-205.
Van Wingerden J.P., Vleeming A., Ronchetti I. Differences in standing and forward bending in women with chronic low back or pelvic girdle pain: indications for physical compensation strategies. Spine. 2008;33(11):E334-E341.
Vleeming A., Stoeckart R., Volkers A.C.W., et al. Relation between form and function in the sacroiliac joint. 1: Clinical anatomical aspects. Spine. 1990;15:130-132.
Vleeming A., Volkers A.C.W., Snijders C.J., et al. Relation between form and function in the sacroiliac joint. 2. Biomechanical aspects. Spine. 1990;15(2):133-136.
Vleeming A., Mooney V., Stoeckart R. Movement, stability and lumbopelvic pain: Integration of research and therapy, second ed. Edinburgh: Churchill Livingstone; 2007.
Vleeming A., Albert H.B., Ösgaard H.C., et al. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur. Spine J.. 2008;17(6):794-819.
Vøllestad N.K., Stuge B. Prognostic factors for recovery from postpartum pelvic girdle pain. Eur. Spine J.. 2009;18(5):718-726.
Waddell G. The Back Pain Revolution. New York: Churchill Livingstone; 1998.
Ward R., Sprafka S. Glossary of osteopathic terminology. J. Am. Osteopath. Assoc.. 1981;80(8):552-567.
Weaver B.T., Haut R.C. Enforced exercise after blunt trauma significantly affects biomechanical and histological changes in rabbit retro-patellar cartilage. J. Biomech.. 2005;38(5):1177-1183.
Weiss J.M. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J. Urol.. 2001;166(6):2226-2231.
Wilson E., Payton O., Donegan-Shoaf L., et al. Muscle energy technique in patients with acute low back pain: A pilot clinical trial. J. Orthop. Sports Phys. Ther.. 2003;33:502-512.
Winkelstein B.A. Mechanisms of central sensitization, neuroimmunology & injury biomechanics in persistent pain: implications for musculoskeletal disorders. J. Electromyogr. Kinesiol.. 2004;14(1):87-93.
Wu W.H., Meijer O.G., Bruijn S.M., et al. Gait in pregnancy-related pelvic girdle pain: amplitudes, timing, and coordination of horizontal trunk rotations. Eur. Spine J.. 2008;17(9):1160-1169. Epub 2008 Jul 26
Wu W., Meijer O.G., Lamoth C.J., et al. Gait coordination in pregnancy: transverse pelvic and thoracic rotations and their relative phase. Clin. Biomech. (Bristol, Avon). 2004;19(5):480-488.
Zink G.G. Applications of the osteopathic holistic approach to homeostasis. In: American Academy of Osteopathy Yearbook. Indianapolis: American Academy of Osteopathy; 1973:37.














