Pacemakers
Generic codes of pacemaker
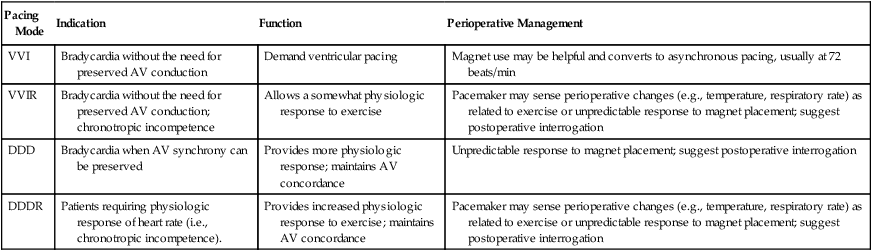
Developed originally by the International Conference on Heart Disease and subsequently modified by the NASPE/BPEG (North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group) alliance, the NASPE/BPEG code consists of five letters of the alphabet that describe the five programmable functions of the pacing system (Box 151-1). The first letter of the code indicates the chamber being paced; the second, the chamber being sensed; and the third, the response to sensing (I and T indicate inhibited or triggered responses, respectively). An R in the fourth position indicates that the pacemaker incorporates a sensor to modulate the rate independently of intrinsic cardiac activity, such as with activity or respiration. A P in the fifth position, for example, indicates that the pacemaker “paces” to treat a tachyarrhythmia. However, letters in the fourth and fifth positions are uncommonly used. Table 151-1 summarizes commonly used configurations.
Table 151-1
Common Permanent Pacemaker Modes
| Pacing Mode | Indication | Function | Perioperative Management |
| VVI | Bradycardia without the need for preserved AV conduction | Demand ventricular pacing | Magnet use may be helpful and converts to asynchronous pacing, usually at 72 beats/min |
| VVIR | Bradycardia without the need for preserved AV conduction; chronotropic incompetence | Allows a somewhat physiologic response to exercise | Pacemaker may sense perioperative changes (e.g., temperature, respiratory rate) as related to exercise or unpredictable response to magnet placement; suggest postoperative interrogation |
| DDD | Bradycardia when AV synchrony can be preserved | Provides more physiologic response; maintains AV concordance | Unpredictable response to magnet placement; suggest postoperative interrogation |
| DDDR | Patients requiring physiologic response of heart rate (i.e., chronotropic incompetence). | Provides increased physiologic response to exercise; maintains AV concordance | Pacemaker may sense perioperative changes (e.g., temperature, respiratory rate) as related to exercise or unpredictable response to magnet placement; suggest postoperative interrogation |
Electromagnetic interference
• Bipolar cautery should be used as much as possible because it causes less EMI.
• If unipolar cautery is to be used during the operation, the grounding plate should be placed close to the operative site and as far away as possible from the site of pacemaker, usually on the patient’s thigh.
• Electrocautery should not be used within 15 cm of a pacemaker.
• The use of electrocautery should be limited to 1-sec bursts in every 10 sec to prevent asystole.
• During the use of cautery, the magnet should not be placed on the pulse generator because it may cause pacemaker malfunction.
• Drugs, such as isoproterenol and atropine, should be available.
• If defibrillation is required in a patient with a pacemaker, paddles should be positioned as far away as possible from the pacemaker generator. If possible, the paddles should be placed anterior to posterior.
• Careful monitoring of pulse (by pulse oximetry or direct arterial pressure measurement) is necessary during electrocautery because electrocardiograph monitoring can also be affected by interference.
• The lead from nerve stimulators should not overlay the generator.
• The device should always be rechecked after the operation if electrocautery was used during the procedure.
Summary
Patients with implanted pacemakers can be managed safely for surgery and other nonsurgical procedures, but to do so requires a thorough understanding of the indication for and the programming of the pacemaker. Anesthetic management should be planned preoperatively according to patient’s medical status, and for those patients who are pacemaker dependent, intraoperative monitoring of a pulse is recommended. Precautions should be taken to minimize EMI while using electrocautery. The magnet should not be placed over the pacemaker in the operating room while electrocautery is in use. Rate-responsive pacemakers should have the rate-responsive mode disabled before the operation begins. Provision of temporary pacing should be available in the operating room to deal with pacemaker malfunction (Table 151-2).
Table 151-2
Pacemaker Malfunctions: Mechanisms and Potential Causes
| Malfunction | Description/Manifestation | Potential Causes |
| Failure to output | No pacing artifact is present despite an indication to pace. | Battery failure Lead fracture Fractured lead insulation Oversensing (inhibiting pacer output) Poor lead connection at the takeoff from the pacer “Cross-talk” (i.e., a phenomenon occurring when atrial output is sensed by a ventricular lead in a dual-chamber pacer) |
| Failure to capture | Pacing artifact is not followed by an atrial or a ventricular complex. | Lead fracture Lead dislodgement Fracture lead insulation Elevated pacing threshold Myocardial infarction at the lead tip Drugs (e.g., flecainide) Metabolic abnormalities (e.g., hyperkalemia, acidosis, alkalosis) Cardiac perforation Poor lead connection at the takeoff from the generator Improper amplitude or pulse width settings |
| Oversensing* | A pacer senses noncardiac electrical activity and is inhibited, resulting in a heart rate lower than the present rate. | Muscle activity—particularly of the diaphragm or pectoralis muscles Electromagnetic interference Fractured lead insulation |
| Undersensing† | A pacer misses intrinsic depolarization and paces despite intrinsic activity, resulting in the pacemaker’s operating in an asynchronous mode. | Poor lead positioning Lead dislodgement Magnet application Low battery Myocardial infarction |
| Pacemaker-mediated tachycardia* | A PVC occurs in a patient with a dual-chamber pacemaker. | If a PVC is transmitted in a retrograde manner through the AV node, it may in turn depolarize the atria. The depolarization is detected by the atrial sensor, which then stimulates the ventricular leads to fire, thereby creating an endless loop. Although the maximum rate is limited by the programmed upper limit of the pacemaker, ischemia may develop in susceptible patients. |
| Runaway pacemaker | A malfunction of the pacemaker generator resulting in life-threatening rapid tachycardia (up to 200 beats/min). | Battery failure External damage to the generator |
| Pacemaker syndrome | Patient feels worse after pacemaker placement and presents with progressively worsening CHF. | Loss of AV synchrony, whereby the pathway is reversed and now has a ventricular origin |
| Twiddler syndrome‡ | Chest radiograph reveals twisting, coiling, fracture, dislodgement, or migration of the leads. | Patient persistently disturbs or manipulates the generator, resulting in malfunction. |
| Cardiac monitor pseudomalfunction§ | Cardiac monitor reports incorrect heart rate. | No malfunction is present; the monitor inappropriately interprets pacing artifacts. |
| Pacemaker pseudomalfunction¶ | Pacing system appears to malfunction. | No malfunction is present; the “malfunction” is a normal programmed pacer function, primarily due to new algorithms that preserve intrinsic conduction and more physiologic pacing. |
AV, Atrioventricular; CHF, congestive heart failure; PVC, premature ventricular contraction.
*This condition is diagnosable and treatable with magnet application.
†Management is similar to that for other types of failures.
‡Requires surgical correction and patient counseling and education.
§Clinicians faced with this issue should first palpate the patient’s pulse and correlate this finding with the results of a pulse oximeter plethysmogram to verify the findings on the cardiac monitor. New monitors have settings to adapt for patients with pacemakers and provide more accurate heart rates.
¶Correction may involve changing the programming or changing the device.





