18 Osteopathic Manipulative Medicine
A Functional Approach to Pain
“Nature applies to you the switch of pain when her mandates are disregarded, and when you feel the smarting of her switch, do not pour drugs into your stomachs, but let a skillful engineer adjust your human machine, so that every part works with Nature’s requirements.”1
History of Osteopathy
Truly an American practice of medicine, osteopathy began on June 22, 1874 in Kansas when Andrew Taylor Still, MD “flung to the breeze the banner of osteopathy”1 and “like an explorer trimmed [his] sail…”.1 A.T. Still was born in 1828 in Jonesboro, Virginia, but he grew up in Missouri as the son of a Methodist minister. Many stories surround the early years of Dr. Still, but little historical evidence is documented. As a Methodist minister, his father was a “circuit rider,” a preacher who would travel out to the edges of the frontier, settle his family, and provide religious service to the pioneers of that day. Although he would also do some missionary work to the indigenous people, conversion was rarely successful. Young Andrew was known to have spoken with the Native Americans around his father’s settlement and was said to have learned about the practice of herbal medicine from them. He was also known to have taken some skeletal remains from the burial grounds and with them began his study of anatomy. As he grew older and the debate around slave states and free states grew, he was a noted abolitionist and later joined the Kansas militia as sides were taken in the early days of the Civil War.
Following his tour of duty in the Kansas militia, he returned home and began the study of medicine as it was practiced in the late 1800s. Practices such as bleeding, administration of purgatives and cathartics, including arsenic and mercury, were common and considered standard of care at that time. This “heroic medicine” was mainly directed at suppressing symptoms and was practiced prior to the advent of the microbial orientation of disease or the understanding of much of the pathophysiology that we take for granted today. He became an accomplished physician by apprenticeship as was the custom and was awarded the title of Medical Doctor. An important event occurred in 1864 when a meningitis outbreak took the lives of three of Still’s children. This devastated Andrew and he “blamed the gross ignorance of the medical profession for the deaths of his children.”2 This tragedy created an alarming sense of helplessness in Andrew and from then on he was determined to find better methods of healing.2
After a prolonged episode of depression and fasting, along with meditation and prayer, he came to the realization that the human form was a perfect reflection of the divinity that created it with the further realization that all of the natural elements of healing were present in the human body, and needed a physician only to release them. He reasoned that any being so created would have contained within it all of the substances it needs to heal itself and that the mechanical structure of the body must have a significant impact on its function. As Still’s most prominent quote said “To find health should be the object of the doctor. Anyone can find disease.”3 It was also the object of the physician to understand every aspect of human anatomy because it is only through understanding of anatomy that an accurate assessment of the healthy functioning of the body could be ascertained. This new science, Dr. Still called “osteopathy”, because it was the study of the relationship that the osseous structure and its interrelationships had on health. He advocated abandoning all use of drugs in favor of dietary, spiritual, and mechanical functional treatment.
Because of this growing success, A.T. Still began to attract the attention of other physicians who wanted to learn this skill that seemed to be healing those who were previously found to be beyond repair. In 1892, he started the American School of Osteopathy in Kirksville, Missouri, and began teaching the first class of 17 students, of which notably three were women. The major system of study was anatomic dissection and the study of manual therapies designed to improve the overall functioning of the human body, allowing it to move toward its natural state of health. One of these first 17 students was Arthur Hildreth, a friend of the Still family, who went on to great success and eventually wrote a book about his great teacher. In the book he says of Dr. Still: “I wish it were in my power to describe in a simple, practical way some of his most outstanding technics. Not only the methods he used but also his own individual way of explaining what he did,” also, “Dr. Still’s technique was marvelous, often beyond our comprehension. He seemed to do everything so easily we wondered how he could accomplish so much.”4 This same Dr. Hildreth was the pioneer who led the charge in many states to gain practice rights for this new method of healing called ”osteopathy”.
Principles of Osteopathic Medicine
Diagnostic Principles
Because osteopathic manipulative treatment is aimed at restoration of function, the diagnosis of dysfunction within the somatic system is a crucial starting point. As Dr. Still’s writing was ripe with concepts and barren with practice, the clarification and development of these topics is ongoing within the osteopathic profession.
The primary structural diagnosis in osteopathic manipulative medicine is “somatic dysfunction.” This is defined by the AOA glossary of terms as “impaired or altered function of related components of the somatic (body framework) system: skeletal, arthrodial, and myofascial structures and their related vascular, lymphatic, and neural elements.”5 This broad definition is important for two reasons: (1) it creates a definitive concept around a palpatory experience and (2) it extends the scope of dysfunction to a zone greater than that of the neuromusculoskeletal system, that of the visceral and cellular functioning of the human organism.
Diagnostic Process
In addition to conventional medical diagnostic procedures, palpatory examination leading to segmental diagnosis of somatic dysfunction is essential to the practice of osteopathic manipulative medicine. Typically, the process of coming to a diagnosis usually involves some measure of palpatory screen, scan, and finally, segmental definition. Screening is the process of palpation and movement designed to answer the question, “Is there a problem?” Scanning answers the question, “Where is the problem?” and segmental definition answers the question, “What is the problem?”6
The scanning examination is one that narrows the finding of somatic dysfunction to a segment, rib, or joint. This is accomplished by a more focused palpation over the region assessing changes in tissue texture that are more specific to the region involved. For instance in the thoracic spine, palpation along the zone of the transverse processes, segment by segment, will help to identify the segment that is dysfunctional, usually by noting a firmness of the surrounding tissue as compared to the segmental transverse process above and below it. This finding is then confirmed through motion testing by initiating passive side-bending or rotation in the thoracic spine and then observing the tissue response to that motion and comparing that response to motion in the segments above and below it. For example, after screening the thoracic spine and finding it to be dysfunctional, a scan is performed and the 5th thoracic segment displays increased tissue tension at the region of the transverse process when compared to the transverse processes above and below it. With the patient’s arms crossed (to eliminate unconscious external stabilization), the trunk is side-bent to the left and an assessment of ease or bind at the 5th thoracic segment is identified as compared to the segments above and below. If restriction to motion is identified with left side-bending, there will be ease to right side-bending of the thoracic spine. Typically, a restriction to motion is more easily appreciated on palpation, but conventionally, the segment is always described in its direction of ease; therefore, the 5th thoracic segment with restriction to side-bending to the left is described as “side-bent right.” The choice of side-bending as a test is completely arbitrary here and passive rotation could just as easily have been demonstrated. The findings of segmental tissue texture change and motion asymmetry determine a positive scan and the next step, segmental definition, must be accomplished if any treatment is to be considered (Fig. 18-1).
Segmental definition is the process of finely tuning one’s scan and focusing palpation and motion testing to account for all possible motion characteristics that occur at the particular segment or joint. To continue our example of the 5th thoracic vertebrae, we identified that motion ease is palpated in lateral side-bending to the right.3 Additionally, we must further check rotation right and left, flexion and extension, anterior or posterior translation, cephalad or caudad translation, or ease in response to the respiratory cycle of inhalation or exhalation. Again, this testing is done passively with the operator moving the patient in all of the aforementioned planes of motion with a palpating hand checking for tissue response to that movement. This provides the most accurate and detailed type of definition for a vertebral segment. Segmental definition of joints of the extremities is a natural extension of the scan for that region. Because motion restriction is detected asymmetrically in the extremities, that motion is more definitively described according to the major motions, but also the minor or secondary motions, such as glide and translation. While these secondary motions are significant in the vertebral column, these subtler motions in the extremities often hold the key to defining dysfunction and, hence, treating it.
Treatment
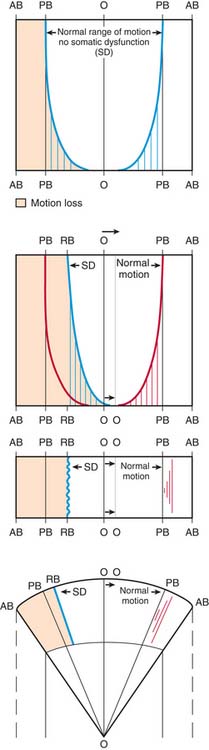
Inherent in these descriptions is the barrier concept. This much debated concept is a direct result of palpatory experience in segmental definition (Fig. 18-2). One model of the barrier concept states that there exists within any segment or joint, a neutral zone in which all of the forces that normally impinge on that segment or joint are equal and balanced. There is a zone around that neutral area that represents the entirety of the normal range of motion that segment or joint possesses. Any motion that segment or joint performs is met with increasing resistance as it approaches its endpoint of motion or barrier. Some definitions of the barrier include distinctions of motion that describe the barrier to passive motion versus the barrier to active motion, or the barrier that exists between the endpoint of passive motion and the barrier that occurs at the limitation of bony resistance of the skeleton. Another important part of the barrier concept is that of a pathologic neutral. When a joint or segment is functioning fully, its neutral position of rest is balanced within its endpoints of motion. When one of the functional endpoints of motion or barriers have been changed through dysfunction, then a new balance point is established that is still neutral in relation to its total potential of function. That change in the neutral is palpable in structural diagnosis as somatic dysfunction. The restriction to motion in one or more planes of motion creates palpatory findings that are commensurate with the definitions of dysfunction.
Muscle Energy Treatment: Lumbar
Muscle energy treatment was developed by Fred Mitchell, Sr., DO, as a way to approach problems directly without high-velocity, low-amplitude thrusting.7 This is a direct technique in which the operator moves the dysfunctional segment toward its restrictive barrier and then stabilizes it while the patient applies an isometric contraction away from the barrier. This contraction is held for 3 to 5 seconds and the patient is instructed to discontinue the contraction. At that point, the operator readjusts the position of the segment to accommodate for the muscle relaxation and lengthening that has occurred, and moves the segment into a new barrier. This sequence is repeated until maximum improvement in the segmental findings is achieved. The advantage of this technique is that the force that is applied is generated by the patient and monitored by the physician. Dr. Fred Mitchell, Jr, DO, who wrote extensively about his father’s technique, explained that the anatomy in a patient’s own (body) was more precisely and intimately known to the patient’s muscles than they could be to any examiner. For this reason he said, his father chose to use the energy of the patient’s muscles instead of his own for the corrective forces.7 This alleviates the danger or unnecessarily overzealous application of an externally applied force. Difficulties with this procedure usually surround the localization of force by the practitioner, lack of stabilization against the isometric contraction on the part of the physician, and too great a force applied by the patient. The force applied need only be great enough to engage the tissues at the level of the localized, treated segment. Too great a force can become too diffuse and difficult to localize around the segment, it may also be too strong to oppose by the physician. The treated segment must be stabilized in its position against the barrier and if that stabilization is compromised because the physician is trembling against the force of the patient, it will be impossible to maintain a stable position at the barrier. Muscle energy technique, when properly applied, should not look like a wrestling match.
The lumbar spine is identified as the lower five vertebrae resting on the sacrum. These are large vertebrae with no rib attachments. Primary motions at these segments include flexion, extension, side-bending, and rotation. The intervertebral discs support the vertebrae, providing both a cushion for shock absorption and a stable, yet flexible interface between the segments, allowing for movement. The remainder of the vertebrae include a pedicle and spinous process creating the spinal canal; transverse processes bilaterally and articular processes above and below the transverse process that create functional joints with the spinal segments superior and inferior to it. These processes form the zygapophyseal or facet joints, true synovial joints in the lumbar spine. Between the pedicles of each of the vertebral segments course the peripheral spinal nerve roots.8
Pain in the lumbar spine is common and multifactorial.9 It is beyond the scope of this chapter to discuss all of the possible causes of back pain; more importantly, there is much speculation about the true etiologies of any of these types of pain. Common pathologies occurring in the lumbar spine that can easily affect the function of the region include: osteoarthritis, herniated nucleus pulposus, inflammatory arthropathy, spondylolisthesis, spondylosis, and ligamentous strain. Although each of these problems has its unique presentation, they each have the capacity to express themselves as a functional limitation of that region, exhibiting signs of somatic dysfunction. Disruption of the normal integrity of the musculoligamentous structures of the axial spine in any location can result in muscular hypertonicity. Because this hypertonicity is usually asymmetrical and is generally restrictive in motion of the spine, diagnosis of tissue texture differences and resultant motion asymmetry is quickly identified. Important in the diagnosis of somatic dysfunction at any location is the appreciation of the anatomic and subsequent physiologic influences any dysfunction can have at local, adjacent regions or distal regions, whether by myofascial continuity or neural irritability.
Important influences that extend from lumbar dysfunction include regional influences. Lumbar dysfunction with its requisite biomechanical changes can affect segments locally adjacent. Because of the physiologic differences between the regions of the axial spine, dysfunction in the lumbar region can influence the appearance of dysfunction in the thoracic spine and sacropelvis and vice versa. As a result of normal physiologic relationships within the viscera and their relationship to the lumbar region anatomically, functions of those viscera can be affected, especially the viscera of the lower pelvis including the large intestine, sigmoid colon, rectum, and pelvic organs. Although this is partly due to the direct effect that a change in normal biomechanics can have on involuntary motions such as those associated with respiration, some of the effect is due to a reflex influence of the somatic system on the autonomic nervous system in the levels of the spine that are affected. In this case, T12 to L2 are most closely associated with the sympathetic cell bodies that provide autonomic influence to the colon below splenic flexure and other pelvic organs. In this way, osteopathic manipulative medicine extends beyond the realm of musculoskeletal pain management and becomes part of a complete system of medicine in which its application begins to influence the visceral function and ultimately the metabolic health of the organism.10 At this point the encompassing definition of “somatic dysfunction” becomes actualized in its application of treatment.
The physician grasps the opposite shoulder by placing his arm across the anterior cervical thoracic junction of the patient and holds the patient snugly. He moves the patient’s trunk passively until the position of restriction is palpated at the previously identified segmental level, which in this case means rotating her trunk to the left and side-bending to the left with lumbar extension until the force of these motions is palpated at L4. The accuracy of the localization of these forces is crucial to the effective application of these techniques (Fig. 18-3). Too little motion and the forces will be localized superior to the segmental region, too much motion and the forces will be directed at a level inferior to the dysfunctional segment. When localization is achieved, the patient is asked to attempt to side-bend and rotate away from the position that she has been put into by the physician. In this case, the patient is directed to, “gently turn to the right.” Generally, only one direction of motion is necessary to activate the force sufficiently to achieve an effect at the dysfunctional segment. Because of normal spinal mechanics, motion in one of the cardinal directions of the spine will affect motion in all the other planes where motion is engaged, so by asking the patient only to rotate, side-bending and flexion are normally engaged. The force of the isometric contraction must be palpated at the level of the dysfunctional segment. The localized isometric contraction is held for 3 to 5 seconds and then the patient is asked to stop turning, or to relax. A moment is given to appreciate the relaxation in the tissues and then the segment is moved into its next restrictive barrier, in this case, slightly further rotated left, side-bent left, and extended. This sequence is repeated as many times as it is needed to effect maximal change, but generally this occurs within five repetitions. At that point, the patient is slowly and gently returned to physiologic neutral, and the dysfunctional segment is checked again for improvement in tissue texture and motion.
Muscle energy treatment is easy to apply to all regions of the body although the lumbar region is demonstrated here. Wherever one can identify a structural diagnosis in which one or more planes of motion are restricted, the patient can always be moved into the edge of that restriction and with a series of isometric contractions, change the presence of that barrier. This includes all of the axial skeleton and appendicular skeleton. The physiology of muscle energy treatment is suspected to be an activation of intramuscular proprioceptive fibers called Golgi tendon organs.11 These sensory units are found at the musculotendinous junctions and, when activated, will reflexively cause the motor units to temporarily shut down and relax the muscle tissue. They are thought to have a protective function against overstretching the muscle. By placing the muscle in a position of restriction and then having the patient isometrically contract, these fibers are thought to be activated and then reflexively allow for muscle relaxation. After the next point of restriction or barrier is achieved, the process is repeated until the dysfunction is resolved. Muscle energy treatment is very effective in conditions where an obvious muscular hypertonicity is palpated. It may be too vigorous treatment in an acute injury, although there are no contraindications for its use in that situation. In general, muscle energy treatment is well tolerated by patients and extremely effective in its treatment of somatic dysfunction.
Strain Counterstrain Treatment: Cervical Region
Strain counterstrain treatment, or spontaneous release by positioning, was developed by Lawrence Jones, DO, and first described in the literature in 1964. The initial discovery of this technique is derived from a patient encounter wherein Dr. Jones was having difficulty treating his patient’s low back pain. After treating him several times unsuccessfully, he asked his patient if there was any position that could be comfortable for him. As the patient assumed that position on the treatment table, Dr. Jones began to prop his extremities and support his spine. After achieving that position of comfort, Dr. Jones left the room and went about treating other patients. When he returned to the treatment room, his patient was asleep. He quietly woke him to find that he was pain free. After slowly removing his supports and helping him sit up from the treatment table, the patient exclaimed that he felt better than he had been in months. Shocked at the dramatic improvement, Dr. Jones began to experiment with this type of “spontaneous release by positioning.” His discovery led him to find that dysfunction generally exhibited itself through tender points, discrete areas of tenderness to palpation. As he found these points, he also began to develop treatment positions for them. His initial explorations were on the posterior surface of the body, but later he discovered the importance of treating points on the anterior body that related to those on the posterior surface.12
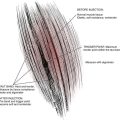
The principle of this style of treatment involves understanding the pattern of trauma, its dysfunctional stabilization, and its eventual resolution. The original trauma is described in the context of a segmental strain. This described scenario creates an overstretch of an agonist muscle and a reflexive contraction of the antagonist muscle. Immediately after the moment of strain, there is a recoil where the agonist muscle attempts to return to its original level of stretch. The speed at which this occurs, however, results in the reflexively contracted antagonist being unable to relax, resulting in a secondary persistent counterstrain of the antagonist muscle. The treatment for this problem involves shortening the antagonist to a point in which spontaneous relaxation occurs followed by a slow return to neutral, eliminating the dysfunction.13
The physiology of this treatment is thought to revolve around the activity of the muscle spindle fiber. This intrafusal proprioceptive fiber responds to relative length of muscle. In contrast to the stretch receptors of the Golgi tendon organ, these muscle spindles seem to respond to increasing length by increasing tone as opposed to decrease. Muscle spindles are thought to be related to a reflexive protective mechanism and increasing the resistance to the muscle becoming overstretched. This is modulated by the gamma motoneuron, one of the types of neural fibers responsible for maintenance of muscle tone. By shortening these fibers during strain counterstrain treatment, this is thought to reduce the afferent stimulus to the spinal cord and subsequent down-regulation of the gamma efferent back to the muscle itself.14 Howell and colleagues demonstrated that osteopathic treatment with strain-counterstrain in Achilles tendinitis resulted in a reduction in stretch reflex amplitude but without changing H-reflex amplitude, suggesting a reset of the intrafusal mechanism without changing the spinal reflex.15
The principles of treatment are straightforward in their description, but again, the correct execution of this treatment is one that requires practice and patience on the part of the physician. The first step in treatment of dysfunction using strain counterstrain treatment is the identification of the “tender point.” This is usually a discrete, nonradiating area found within the belly of the muscle or at the muscular attachment at a body prominence. Multiple tender points may be found in a regionally related group of muscles and, in that case, the most tender point should be taken and treated first. These tender points are differentiated from myofascial trigger points in that there is not the characteristic radiation of pain that is typical of a trigger point.16 In order to quantify the amount of tenderness at the beginning of treatment, the patient is instructed that whatever tenderness is being elicited with palpation should be considered a 10/10 in intensity to begin.
Approaching the tender point is a step-wise process. Contact is maintained on the tender point with the palpating finger tip, preferably not the thumb to eliminate the practitioner’s appreciation of his own pulse. Additionally, the finger tips are more sensitive than the thumb to palpation. As the patient’s body position is adjusted to approximate the desired location, the patient is asked, “is this less tender?” If the answer is, “yes,” then a quantification of the improvement is obtained. If improvement is 70% or better, then that position is held for 90 seconds. If, however, the improvement is present but less than 70%, the position is fine-tuned to get closer to the point at which the counterstrained muscle fibers are shortened and afferent barrage from the muscle spindle subsides.
The cervical spine region is unique because it articulates with the cranium superiorly and the thoracic cage inferiorly. Rotation, side-bending, flexion, and extension are all movements of the spine that are integral to the function of the cervical region and important to the organism. As the final common biomechanical pathway from the appendicular and axial skeleton toward the cranium, the cervical spine fulfills an important function for the organism, primarily by directing its sense organs—vision, hearing, smell, and taste—toward the external environment. Its remarkable freedom of movement provides a suspensory function during gait and a stabilizer to the cranium during rapid changes in directional movement. It serves to keep the gaze level and uses remarkable proprioceptive influences to sustain that during normal motion of the body. Closely associated with the cervical spine are the vertebral arteries and carotid arteries, which are crucial in creating the cerebral circulation. Venous drainage of the head through the jugular veins is through the region of the cervical spine. The two halves of the autonomic nervous system are in close proximity in the cervical spine with the cell bodies of the vagus nerve emerging from the jugular foramen of the cranium, providing parasympathetic function extending inferiorly from the brainstem to the level of C2 and the sympathetic cervical ganglia providing afferent stimulation to the head, neck, and cardiac regions. The viscera of the esophagus and trachea have their origins in the cervical spine. The importance of considering the anterior and posterior musculature in stabilization of a particular region is easiest to appreciate in the cervical spine. Posteriorly, the erector spinae group of muscles along with the upper splenius capitis and cervicis muscles interface at the cranial base with the rectus capitis muscles along with the obliquus capitis muscles. Anteriorly, the sternocleidomastoid provides a significant support against rapid extension of the head on the cervical spine, and longus colli and capitis provide support and aid in flexion of the neck. The uppermost two cervical vertebrae are the atlas and axis, both of which are considered atypical cervical vertebrae. The axis, C1, articulates with the cranial base and C2. It lacks a vertebral body or transverse processes. The articulation with the occiput is primarily designed to allow for flexion and extension of the head on the cervical spine, whereas the articulation between C1 and C2 allows for the primary rotation of the head to the right and left. This is because the atlas and axis behave as one segment providing two distinct motion functions. The contact between C1 and C2, the dens and its surrounding ligaments and cartilage is actually a modification of a vertebral body and intervertebral disk. The remaining cervical vertebrae from C3 to C7 are the typical vertebrae with a round vertebral body and intervertebral disc. Unique to these vertebrae are their nearly horizontal articular facets in the superior segments that become progressively more oblique in their presentation as they move inferiorly, but still oriented in an anterior to posterior plane. Additionally, the transverse processes of the cervical vertebrae from C2 to C7 have foramen that allow the passage of the vertebral arteries bilaterally and vertically. These converge over the atlas and enter the foramen magnum where they produce the posterior arch of the circle of Willis at the brainstem.8
Treatment positions for tender points in the cervical spine fall into three broad categories. Specific exceptions to these generalizations occur but are beyond the focus of this chapter and necessitate further study. Typically, the two types of tender points are posterior and anterior. The posterior points fall directly over the spinous processes of the cervical spine and generally require passive extension as a position of comfort. An alternative location for the posterior points is just on the lateral and inferior edge of the spinous process (Fig. 18-4). Treatment of these points requires extension, side-bending, and rotation away from the side of the tender point for resolution. The anterior tender points are found along the anterior surface of the transverse processes of the cervical spine and require side-bending toward and rotation away from the side of the tender point combined with flexion of the cervical spine to obtain resolution of the tender point (Fig. 18-5).14
High Velocity Low Amplitude: Thoracic Spine
HVLA was the dominant form of osteopathic manipulation taught in the United States for the first half of the 20th century until the advent of muscle energy treatment. Interestingly, although this was so widely taught in the early days of osteopathy, this treatment was probably not what Dr. Still practiced. Through limited descriptions of his treatments in his writings and one short film clip that shows him treating a shoulder, along with writings of some of his students, Still probably did not treat with HVLA, but more likely treated from the myofascial and articulatory perspective, some of which will be described later in this chapter. Dr. Ray English wrote of Dr. Still’s technique “I have seen [Dr. Still] adjust lesions but I have never heard him adjust a lesion.”17 It is reported that D.D. Palmer, the founder of chiropractic in 1895, visited Dr. Still in 1893, was treated by him, and had numerous meetings with him. After the “discovery” of chiropractic, “the Palmer method” was demonstrated by Dr. C.E. Achorn at the American Osteopathic Association convention in 1900. Although this was described as “a very crude and very poor imitation of the kind of manipulative therapy Dr. Still practiced,4” it is thought that Palmer’s influence may have been reabsorbed into the osteopathic profession and elaborated as osteopathic HVLA treatment. The ease of the description of this treatment seems to belie its pervasiveness as the dominant style of treatment taught in the osteopathic colleges until newer methods were developed—eventually leading to the elaboration of Still Technique5 (a more developed description of some of the articulatory techniques thought to represent Still’s original style) in the 1990s. Because of its universality of application and simplicity of execution, HVLA continues to be the most popular style of manipulation in osteopathic practice.18
The skill of execution of HVLA technique lies in the localization of the barrier and the quality of the thrust. In HVLA, the barrier is palpated by movement of regional treatment zones, typically in opposite directions in an effort to “lock out” the barrier. In the axial spine, the zygapophyseal joints are those that are most commonly treated with HVLA. Generally, the anatomy of those joints and their direction of articulation define the motion that is undertaken by the physician to engage the barrier and later, the application of thrust. The name, “high velocity low amplitude”, is an apt descriptor for the type of force applied. Classically, a short 1⁄8-inch thrust is quickly applied to the barrier and then the region is rechecked. This can be a difficult concept for a beginning student to grasp. This thrust quickly moves the articulations apart and often results in an audible pop or crack. No definitive explanation for the therapeutic benefit of this procedure has been agreed on, although neural mechanisms along with alteration in cross-link connective tissue adhesions has been proposed.5
This technique is particularly indicated for dysfunctions of a chronic nature in otherwise healthy adolescents or adults. Of all manipulative medicine techniques, those of the high velocity style are fraught with the highest morbidity. Of the regions that can be treated with high velocity manipulation, the cervical spine carries with it the highest morbidity and potential mortality. The American Osteopathic Association published a position paper in 2004 after reviewing the reported adverse events associated with cervical HVLA treatment as well as its benefits and concluded that osteopathic manipulative treatment of the cervical spine with HVLA treatment is effective for neck pain and is relatively safe, especially in comparison to other common treatments.19 Because of these risks, relative contraindications to use of HVLA procedures include rheumatoid arthritis, Down’s syndrome, bony carcinoma, osteoporosis, and osteomyelitis. The benefit of the application of this technique, in skilled hands, generally outweighs the risk in most situations and provides rapid relief of dysfunction and allows for great patient satisfaction.
Thoracic Spine
The thoracic spine consists of twelve thoracic vertebrae and creates a biomechanical transition between the cervical spine and the lumbar spine. This transition is reflected in the anatomic and functional differences as the thoracic spine changes along its length (See Fig. 18-1). The spinous processes of the first three thoracic vertebrae closely resemble those of the cervical vertebrae, generally pointing directly posterior; however, these spinous processes tend to point slightly inferior. The next three thoracic vertebral spinous processes point slightly more inferior and end in the horizontal plane of the intervertebral discs of T3-6. This trend continues in the next three thoracic vertebrae until the spinous processes end at the vertebral body of the segment inferior to the one above. T10-12 represent a functional transition toward a more lumbar appearance and reverses the anatomic trend of the first nine vertebrae as the spinous process ends at the horizontal plane of the segment of its origin.11 Similarly, the thoracic spine has a unique anatomy of its articular facets, transitioning from a superior-inferior orientation with an oblique orientation posterior and inferior, similar to the cervical segments in the upper thoracic region, to a more medial-lateral orientation in the lower thoracic region, similar to the lumbar segments. The orientation of these facets has a direct affect on the angle of thrust when performing osteopathic manipulative therapy (OMT) on the thoracic spine.
Closely associated with the thoracic spine are the nerve roots that emerge from the neural foramina created by each pair of thoracic vertebrae. Immediately adjacent to these neural elements are the thoracic chain ganglia, representing the thoracic segment of the sympathetic nervous system. Importantly, the cell bodies for the preganglionic fibers occur at the segments T1-L2. Addressing dysfunction within these segments provides a useful approach to the potential impact of imbalance within the autonomic segments and visceral disease. I.M. Korr, PhD, an early neurophysiologist within the osteopathic profession, proposed the model that irritation and facilitation within the autonomic nervous system was the first predisposing factor to illness that could be expressed in the body.5 This facilitation and subsequent elevation in sympathetic nervous system tone with its tendency toward vasoconstriction created an environment that would be limited in its capacity to support health by a restriction in vascular flow. This is one of the primary aspects of an osteopathic physiology of pathogenesis. This is known as the somatovisceral reflex.
Diagnosis of thoracic dysfunction is made using the screen, scan, and segmental definition methods previously described. Alternatively, the thoracic spine may be defined in the following manner. After screening determines that a dysfunction is present in the thoracic region, palpatory scanning in the seated position identifies tissue texture changes characteristic of dysfunction (i.e., segmental tissue change associated with a rotation of the transverse process to the right or left). This feels like a prominence in the paravertebral tissue that is firmer than simple muscle tension—an asymmetrical prominent bony landmark in the tissue of that particular segment. The level of dysfunction is identified by counting spinous processes, keeping in mind the variations in the thoracic levels relative to the spinous processes characteristic of this region of the spine. When these changes are localized, thumbs are placed on the region of the transverse processes and the patient is asked to bend forward. As the patient bends forward, the palpating hands identify any changes in position or motion at the rotated transverse processes. If the asymmetry improves in the flexed position, the position of ease is identified as “flexed.” If the asymmetry does not improve, the patient is asked to sit up straight and arch his or her back slightly with the neck slightly extended, causing thoracic extension. If improvement in the asymmetry of the transverse processes is identified, the position of ease is identified as “extended.” If no change is palpated in either position, flexed or extended, then the position of ease is identified as “neutral.” Because of the principles of spinal mechanics known as Fryette’s Laws,20 a dysfunction that is either flexed or extended also exhibits rotation and side-bending to the same side and a dysfunction that is neutral exhibits side-bending and rotation to opposite sides. In this example, if T5 was found to exhibit rotation to the right and found to be in ease with flexion, it would be identified as “flexed, rotated right, and side-bent right.” If it was found to be in ease with extension, it would be identified as “extended, rotated right, and side-bent right.” If no change was palpated with flexion or extension, it would be identified as “neutral, side-bent left, rotated right.”
Thoracic HVLA Treatment 1: Flexed Dysfunction
As a direct technique, HVLA demands segmental definition diagnosis of somatic dysfunction so an appropriate position into the restrictive barrier can be introduced before thrusting. In this technique, the patient is placed in the prone position and the diagnosed segment is identified. The physician stands to the side of the patient that exhibits thoracic rotation dysfunction and places his hands on the thoracic region with hypothenar eminences on opposite sides of the diagnosed segment (Fig. 18-6). The hands are placed in opposite directions so that the fingers are pointing cephalad on the side of the thoracic side-bending and caudad on the side opposite the side of thoracic side-bending. For example, in the diagnosis of “T5 flexed, rotated, and side-bent right,” the physician stands on the right side of the prone patient and places the hypothenar eminences on the region of the transverse processes with the fingers on the left side of the spine pointing cephalad and those on the right side pointing caudad. This provides a position for creating tissue tension that encourages leftward side-bending. The tissue tension and motion restriction is tested in that position, moving the tissue into the barrier by slightly increasing the side-bending to the left through opposite motions of the cephalad and caudad hands. The patient is instructed to take a deep breath and exhale. Contact with the tissue is maintained through inspiration and followed through exhalation as the barrier is more significantly engaged through slightly greater increases in pressure. At the end of exhalation, the barrier is completely engaged and a slight ⅛-inch thrust toward the table and with both cephalad and caudad pointing hands quickly moving in opposite directions, in a twisting manner.
Thoracic Treatment 2: Extended Dysfunction
Treatment of this type of dysfunction is performed with the patient in the supine position. A diagnosis is made of the dysfunctional thoracic segment. For this example, the diagnosis is T5 extended, rotated, and side-bent right. The physician stands on the side of the supine patient that is opposite that of the rotation. In this example, the physician would stand on the left side of the supine patient. The patient is asked to cross both arms across the chest snugly and grasp the shoulders. This provides the elbows as a point of contact for the physician’s sternum, draws the scapulae laterally for better contact with the thoracic spine, and tightens the fascia of the thoracic cage, allowing for a more specific direction of force into the segmental barrier. The cervical-occipital junction is supported with the right hand of the physician, whereas the left hand reaches around and behind the patient to make contact with the dysfunctional thoracic segment. An open-handed fist is used to localize the dysfunctional segment by making contact with the thenar eminence on the rotated transverse process (Fig. 18-7). The patient’s torso is brought anterior into flexion and then relaxed over the open-fist fulcrum balance force between the physician’s sternum, the fulcrum, and the supporting hand on the occipital-cervical junction. When forces are balanced and the barrier is engaged, the patient is asked to inhale and exhale. On the exhaling breath, the physician follows the thoracic cage as it collapses in anterior-posterior diameter and at the end of exhalation, applies a short 1⁄8-inch thrust through the sternum, patient’s elbows, and through the dysfunctional articulation. The direction of this thrust has a slightly cephalad orientation as the motion is intended to create a relative flexion of the thoracic segments that are restricted in extension (Fig. 18-8).
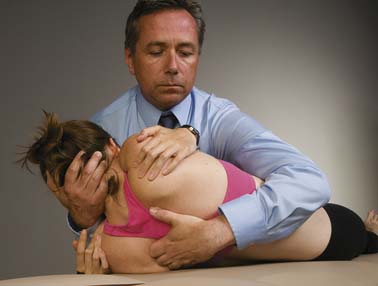
Figure 18-7 Correct placement of thenar eminence on posterior transverse process in preparation for supine HVLA.
Two significant points of refinement in the successful approach to HVLA in clinical practice are accuracy of engagement of the functional barrier and appropriate application of force. The application of force is sometimes described as that amount of force necessary to squash a grape under one finger without sullying your finger with the juice. This is an excellent image of the accuracy, the speed, the type of force, and the slight recoil that occurs in a thrust technique. There is no wind-up and no follow-through. This is a specific and directed application of rapid compression intended only to move the intended segment past the barrier and no more. This force may be accompanied by a sound of pop or click but this is not necessary for the treatment to be effective. Effectiveness of treatment is measured by reevaluation of the diagnosed segment after the treatment is performed.
Myofascial Release: The Extremities
The origin of myofascial release technique in osteopathy dates to the time of A. T. Still. In Principles of Osteopathy he writes: “we think we prove conception, growth, and cause of all diseases to be in the fascia.”3 Given the importance that he attaches to the fascia, it is likely that within his style of technique, treatment of the fascia was given significant consideration. Considering the ubiquity of fascia within the body it is easy to overemphasize or casually ignore its presence. Treatment of the fascia can be superficial or deep and may be applied from a perspective of direct or indirect technique or a combination of the two.
Myofascial technique often makes use of motion stacking when addressing dysfunctioning from the position of the extremities. Motion stacking occurs when one part of the extremity is moved into a chosen position according to one’s intention and then begins to move another portion of the extremity into another position with the intention of holding the first position. For example, in addressing the upper extremity from a distal to proximal approach using direct fascial technique, first the hand and wrist is moved into a position that engages resistance in as many fascial planes as possible. Next, while maintaining that position with the wrist, the forearm is secondarily engaged in resistance in as many fascial planes as possible. This process is continued proximally along the upper extremity until the motions are stacked into the axilla or proximally. At that point, the phenomena of hysteresis or creep occurs and the fascia will release spontaneously while held in tension. Attention to the different regions of an extremity can be engaged separately also, by first treating the wrist, returning to neutral, treating the forearm, returning to neutral, and so on.
The Extremities
The upper and lower extremities in the human body occur as appendicular extensions of the thoracic cage and of the abdominal cavity, embryologically.21 The human extremities provide us with locomotion to find sustenance and with methods of connecting with the world from our hearts and touching the solid forms around us. Anatomically, they consist of one long bone that articulates with the axial skeleton through a highly mobile “ball and socket” type of joint, a double-bone that articulates with the first via a hinge joint, with the upper extremity example of this being able to fully supinate and pronate, and finally a distal multiply articular appendage designed for locomotion or object manipulation and kinesthetic awareness ending in five distal phalanges. For the purposes of the elaboration of myofascial technique, each of these extremities can be addressed individually in treatment of the extremity itself, or it can be viewed as a long lever that, when activated, can be used to affect the integrity of the fascial network at regions significantly distal to the point of motion input.
The connective tissue fascial network of the extremities begins in the superficial layer as loose connective tissue, or areolar connective tissue, occurring subdermally and often including a panicular layer of adipose tissue. Internal and contiguous to that layer is the intermediate layer of connective tissue that represents the fascia surrounding the muscle layers. This layer of fascia invests into the muscle tissue itself dividing the muscle into individual fascicles and then providing intercellular support. This intermediate layer continues centrally until it becomes a deep fascial layer that integrates into the ligamentous and periosteal tissue of the upper extremity. This fascia begins proximally as the investing fascia of the axial skeleton, nervous system, and mediastinum, extending radially through the viscera out to the visceral pleura, parietal pleura, thoracic cage, and the superficial muscles of the anterior and posterior thorax and distally to the proximal anterior and posterior shoulder region. Inferiorly, this fascia begins axially, investing in the retroperitoneal structures and viscera, the abdominal viscera, mesenteries, visceral peritoneum, parietal peritoneum, extending out through the superficial musculature of the anterior and posterior abdomen, extending into the pelvis and distal to the myofascial network of the girdle of the hip.22 This litany of structures is only a rudimentary description of the totality of the presence of the fascia within the human organism and could be elaborated in much greater detail.
Myofascial Release
Upper Extremity
In this example, treatment of the upper extremity begins with the patient in the lateral recumbent position with the extremity to be treated, off the table. Treatment begins proximally by engaging the fascial tissue surrounding the scapula. The physician’s hand surrounds the posterior portion of the scapula and passively moves it cephalad, caudad, medial, and lateral. When a barrier is reached, the tissue is permitted to release spontaneously or with respiratory assistance as in the palpatory exercise example. Next, the deep fascia of the extremity is addressed by abducting the arm while the fascia of the anterior axilla and then the posterior axilla is stabilized. The fascia of the elbow is next addressed by stabilizing the elbow while slowing supination and then pronating the forearm to the endpoints of motion in each direction. The fascia of the wrist is addressed through slow articular stretching of the radiocarpal joint; the metacarpals are individually articulated with attention to the connective tissue; and the fascia of the phalanges is mobilized as well. Finally, the entire upper extremity is brought into abduction and external rotation, engaging the pectoralis fascia along with the myofascial network of the upper extremity. Next internal rotation and adduction of the upper extremity is performed, engaging the myofascial tissue of the upper extremity along with the posterior trapezius, latissimus dorsi, and other axial fascial connections, superficial and deep (Fig. 18-9).
The Lower Extremity
This treatment efficiently addresses dysfunction at multiple levels of the lower extremity and engages the fascia of the anterior and posterior pelvis. Internal rotation of the lower extremity with the knee in flexion and the ankle stabilized creates a relative inversion of the talocalcaneal joint, internal rotation of the tibia, posterior lateral glide of the tibia at the femur, posterior glide of the proximal fibula, internal rotation of the femur at the acetabulum, and associated fascial engagement of the posterior pelvis including the gluteal and piriformis regions. Internal rotation of the lower extremity largely creates the opposite motions and tensional engagement of the anterior pelvis and internal rotators of the hip including the anterior fibers of the gluteus medius and minimus, the adductor longus and brevis, the pectineus, the medial hamstrings (semitendinosus and semimembranosus) and the tensor fascia latae (Fig. 18-10). Myofascial technique can be applied to any area of the body effectively with focused palpation and knowledge of the musculoskeletal anatomy. Although both treatment techniques described here are direct techniques, application of indirect myofascial technique methods is also appropriate by combining palpation and regional motion to find the greatest ease or path of least resistance as the dysfunctional region is moved away from the barrier and an allowance of spontaneous resolution through intrinsic movement toward health and functional homeostasis occurs.
Osteopathy in the Cranial Field
Treatment of the cranium fundamentally applies the principles of osteopathic manipulative treatment for the rest of the body, but involves a greater sensitivity to palpatory cues and appreciation of the subtle motion in the region of the head. Central to the practice of osteopathy in the cranial field is the understanding of the mechanics of the cranium and how that motion is reflected in the rest of the body. A respect for the potentially negative impact of treatment of the cranial region is also necessary and extensive treatment should not be undertaken by the beginner, but should only be attempted after sufficient introductory training by an instructor-led course. To that end, this chapter will cover only principles of cranial technique with an example of treatment that is effective and safe to apply by relatively inexperienced hands.
The origin of cranial osteopathy as an extension of other types of osteopathic manipulative treatment is credited to William G. Sutherland, DO, a student of Dr. Still. The moment of its origination was when young Dr. Sutherland, walked past a model of a disarticulated skull in 1899 at the American School of Osteopathy, and “like a blinding flash of light came the thought—beveled like the gills of a fish and indicating articular mobility for a respiratory mechanism.”23
This began his study and development of cranial osteopathy. He later wrote that he was merely following Dr. Still’s advice to dig on as Dr. Still earlier wrote, “the cerebrospinal fluid is the highest known element that is contained in the human body, and unless the brain furnishes the fluid in abundance a disabled condition of the body will remain,” and mandated that, “this great river of life must be tapped and the withering field irrigated at once, or the harvest of health be forever lost.”3 Dr. Sutherland devised mechanisms to create dysfunction in his own cranium, studied the effects it would have, and then developed treatments to resolve them. He wrote The Cranial Bowl in 1939 and taught the cranial concept to interested physicians from 1940 to 1953.24
The cranial concept was a development of the mechanical principles of the cranial motion combined with the motion of the cerebrospinal fluid and the relationship of both to respiration. The combination of all three of these aspects he combined as the primary respiratory mechanism. Dr. Sutherland elucidated five fundamental principles of the cranial concept: (1) the fluctuation of the cerebrospinal fluid, (2) the function of the reciprocal tension membrane, (3) the motility of the neural tube, (4) the articular mobility of the cranial bones, and (5) the involuntary mobility of the sacrum between the ilia. Fundamentally, this concept states that primary respiration, the fundamental metabolic cellular process of existence, is driven first intrinsically through the related components of the central nervous system including the cerebrospinal fluid. Although each aspect of the components of the primary respiratory mechanism have been studied in anatomic and physiologic detail,25 this overriding concept of the function of the primary respiratory mechanism remains elusive and falls somewhere between the domains of physiology and phenomenologic epistemology.
While detailed explanations about the palpatory diagnostic findings are well beyond the purposes of this chapter, a cursory illustration of some of the aspects of this concept will be attempted here. The bones of the cranium develop embryologically as either membranous bone or cartilaginous bone depending on their location. In general, the bones of the base of the cranium, the basiocciput and the sphenoid and petrous temporal arise out of cartilage, whereas the temporal squamous, occipital squamous, parietal, early frontal bones arise out of membrane. These slowly approximate each other as development continues after birth until they interdigitate during late ossification and become sutures. These sutures are not fused, but are largely patent with dissectible connective tissue fibers, lymphatics, and occasional nerve fibers present. The patency of the sutures allows for motion and this has been recorded and documented. The motion that occurs at these sutures is reflective of a deeper motion that drives them, and the development of the articulations is a result of that motion. With fine palpation, it is possible to appreciate a subtle cyclical expansion and contraction of the cranium with a rate of 6 to 12 oscillations per minute and with a variable amplitude.26 This motion is first appreciated as a flexion and extension that occurs at the cranial base in the synchondrosis of the sphenoid and base of the occiput. Motion is distributed to the paired cranial bones of the temporal and parietal that articulate the cranial base, and flexion and extension then becomes internal and external rotation. This combination of motions—flexion, extension, internal and external rotation—translates into a palpatory experience of a rhythmic expansion and contraction of the cranium. This motion is intrinsic and primary, but is also associated with respiration and extends its influence to all the tissues of the body as inspiration is linked with external rotation of all the paired bones of the body and exhalation is linked with internal rotation of all the paired bones of the body.
Palpation Exercise
If one is to appreciate the palpatory experience of osteopathic treatment within the cranial field, the following exercise is presented. Treatment of the cranium is usually applied with the patient in the supine position. The physician sits at the head of the table on a chair that is at a height such that the elbows can rest comfortably without disturbing the erect seated posture of the practitioner. One of Dr. Sutherland’s students, Rollin E. Becker, DO wrote about establishing a treating fulcrum in a region other than the hands to allow for the greatest palpatory sensitivity.27 This fulcrum is usually the forearm or elbow and this portion of the upper extremity makes firm contact with the treatment table to allow for less distracting proprioceptive input in the hands and fingers. The hands are lightly placed on the vault of the cranium, thumbs touching and off the cranium to prevent over compression (Fig. 18-11). The index finger rests in the region of the greater wing of the sphenoid posterior to the lateral canthus of the eye. The middle finger rests just superior to the auricle. The fourth digit rests just inferior to the auricle and the fifth digit is posterior and inferior to the mastoid process in the region of the squamous portion of the occiput. When this position is achieved, the physician must take account of the amount of pressure that he is imposing on his patient. The amount of pressure must be enough to make light contact, but no more, because undue pressure can negatively affect the quality of the intrinsic motion present within the cranial vault. The physician checks his posture and relaxes as much as possible, again to reduce the amount of extraneous proprioceptive input, allowing for the greatest sensitivity to subtle motion. Next, the physician focuses on the space occupied between his palpating hands rather than what is happening at the surface under his fingers. Focusing on that space allows for the appreciation of the rhythmic alteration of the shape of the volume under his palpating hands. Commonly, he might first appreciate the rhythmic oscillations of respiration as it is transmitted up to the cranium or the cardiac pulse as it resonates into the cranium, but the cranial rhythm is a movement that is independent from that. With continued practice and refocus it is possible to palpate the cranial rhythm with its 6 to 12 cycles per minute periodicity and variable amplitude. This is the starting point for appreciation of the normal functional movement of the cranium, all cranial diagnosis, and subsequent intervention or treatment.
Treatment: Release of the Cranial Base and Atlas
One of the significant portions of cranial anatomy is reflected in the articulation between the base of the occiput and the atlas. This area is rich with neural, vascular, and fascial structures. The base of the occiput near the atlas is the location of the jugular venous foramen in the articulation between the occiput and the temporal bone. This foramen provides venous drainage from the cranial vault along with the exit of cranial nerves IX, X, and XI. In addition, the cell bodies of the vagal nucleus descend in the upper spinal cord to the level of C2. At the cranial base, the dura still has some freedom of motion before it becomes attached at C2. A small fascial connection between the suboccipital muscles called the nuchal ligament is found in this region also.28 This is the final common pathway for all forces rising from the lower extremities, trunk, and upper extremities as the transition is made from the relatively mobile spine to the relatively immobile cranium. For this reason, release of this region is considered vital to maintaining homeostasis in the organism. Although this is a common location to begin to treat headaches, it is also useful in treatment of visceral problems because of its potential influence on the vagus nerve. If this area is addressed with skill, deep relaxation of the patient is quickly achieved. This parasympathetic “relaxation response” is considered to be a healthy and healing alternative to the hypersympathetic overdrive that we tend to exist in as a culture. The origin of this technique dates to the early days of A.T. Still, when he rested his head on a loop of plough rope, fell asleep and awoke to find his headache had been relieved.1
This treatment is performed with the patient in the supine position with the physician at the head of the table as previously described. The fingers of the treating hand make contact with the tissue just under occiput in the tissue of the region of the atlas because the atlas has no definitive landmark as a spinous process. The tips of the fingers are gently extended anteriorly into the muscles of the suboccipital tissue, allowing a normal relaxation as the pressure is increased. Importantly, only enough pressure necessary to engage the tissue is needed here (Fig. 18-12). Too much pressure can cause undue discomfort for the patient and becomes fatiguing to the hands of a new practitioner. Too little pressure and the technique is simply ineffective. Once the initial release of positioning is obtained, the practitioner can appreciate an asymmetry of tension within the tissue. Increasing the pressure on the side that is less tight, attempting to balance the tension between the two sides allows for a release of the tissue on the more restricted side. This is an indirect approach as we are moving into the ease of the tissue and allowing for a spontaneous correction. This anteriorly directed contact in the suboccipital region continues until no further release of the tissue is appreciated by the practitioner, usually within a few minutes.
Conclusion
The reader is encouraged to contact the following organizations to obtain further information about their curricula designed to more completely introduce the concepts, principles, and techniques described in this chapter:
1. Still AT: Autobiography of A.T. Still. Kirksville, Mo, 1908.
2. Trowbridge C. Andrew Taylor Still, 1828-1917. Kirksville, Mo: The Thomas Jefferson University Press; 1991.
3. Still A.T. Philosophy of Osteopathy. 1899.
4. Hildreth A.G. The Lengthening Shadow of Dr. Andrew Taylor Still. Kirksville, Mo: Simpson; 1942.
5. Ward R.C., editor. Foundations for Osteopathic Medicine. 2nd ed. Philadelphia: Lippincot Williams & Wilkins, 2003.
6. Johnston WL, Friedman HD, Eland DC: Functional Methods, 2nd ed. Indianapolis, In: American Academy of Osteopathy, 2005.
7. Mitchell F.L.J. The Muscle Energy Manual. East Lansing, Mich: MET Press; 1995.
8. Gray’s Anatomy, 40th ed. UK: Elsevier; 2008.
9. Bhangle S.D., Sapru S., Panush R.S. Back pain made simple: An approach based on principles and evidence. Cleve Clin J Med. 2009;76:393-399.
10. Beal M.C. Viscerosomatic reflexes: A review. J Am Osteopath Assoc. 1985;85:786-801.
11. Kuchera W.A., Kuchera M.L. Osteopathic Principles in Practice, 2nd ed. Columbus, Ohio: Greyden Press; 1994.
12. Jones L.H. Spontaneous release by positioning. The DO. 1964:109-116.
13. Jones L.H. Strain and Counterstrain. Newark, Ohio: American Academy of Osteopathy; 1981.
14. Rennie P.R., Glover J.C., Carvalho C., Key L. Counterstrain and Exercise: An Integrated Approach, 2nd ed. Williamston, Michigan: RennieMatrix; 2004.
15. Howell J.N., Cabell K.S., Chila A.G., Eland D.C. Stretch reflex and Hoffmann reflex responses to osteopathic manipulative treatment in subjects with Achilles tendinitis. J Am Osteopath Assoc. 2006;106:537-545.
16. Simons D.G., Travell J.G. Myofascial Pain and Dysfunction: The Trigger Point Manual, 2nd ed. Baltimore: Lippincott Williams and Wilkins; 1999.
17. English R. The Theory of Technique JAOA. 1920.
18. Johnson S.M., Kurtz M.E. Osteopathic manipulative treatment techniques preferred by contemporary osteopathic physicians. J Am Osteopath Assoc. 2003;103:219-224.
19. American osteopathic association position paper on osteopathic manipulative treatment of the cervical spine. AAO Newsletter. 2004:15-17.
20. Kimberly P.E. Outline of Osteopathic Manipulative Procedures: The Kimberly Manual. Millenium. Marceline, Miss: Walsworth Publishing. 2000.
21. Blechschmidt E. The Otogenetic Basis of Human Anatomy; A Biodynamic Approach to Development from Conception to Birth. Berkeley, Cal: North Atlantic Books; 2004.
22. Becker R.F. The meaning of fascia and fascial continuity. Osteopathic Ann. 1975:186-196.
23. Magoun H.I. Ostoepathy in the Cranial Field. Meridian, Idaho: Sutherland Cranial Teaching Foundation; 1976.
24. Sutherland W.G. Teachings in the Science of Osteopathy. Portland, Ore: Rudra Press; 1990.
25. Bibliography of Research Related to Osteopathy in the Cranial Field. Indianapolis, In: Cranial Academy Publishers; 1999.
26. Liem T., McPartland J.M., Skinner E. Cranial Osteopathy: Principles and Practice, 2nd ed. China: Elsevier; 2004.
27. Becker R.E. Life in Motion. Portland, Ore: Stillness Press; 1997.
28. Dean N.A., Mitchell B.S. Anatomic relation between the nuchal ligament (ligamentum nuchae) and the spinal dura mater in the craniocervical region. Clin Anat. 2002;15:182-185.