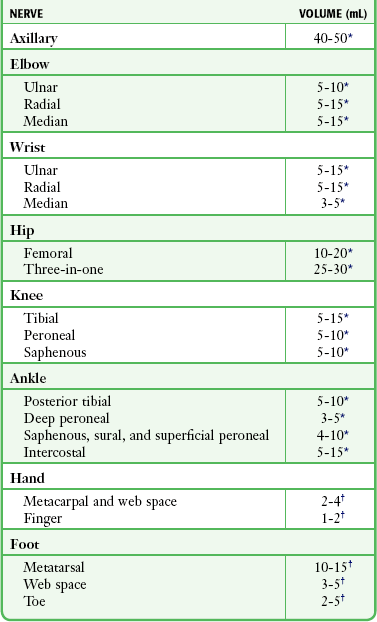
Nerve Blocks of the Thorax and Extremities
General Concepts
For most lacerations and injuries seen in the emergency department (ED), local infiltrative anesthesia is adequate and more efficient than using a nerve block (see Chapter 29). Patients who require extensive repair and anesthesia of the entire extremity are often referred to a specialist, who may prefer to examine an unanesthetized limb. A nerve block is indicated when it will provide advantages over other techniques. Scenarios in which this requirement is met include the following:
• When distortion from local infiltration hampers closure (e.g., facial wounds) or compromises blood flow (e.g., fingertip)
• When anesthesia is required over a large area and multiple injections would be painful or when the large amount of anesthetic needed for local infiltration exceeds the recommended dose
• When a nerve block is the most efficacious form of treatment, such as an intercostal block for treating a rib fracture or a patient with chronic obstructive pulmonary disease
• When local infiltration of the wound would be more painful than a regional nerve block, such as in the plantar surface of the foot or the palm of the hand
• When the block is performed to decrease pain during finger or toe dislocation or reduction
• When extensive limb surgery or manipulation is required (e.g., extensive tendon repair) and other options are not available
Preparation
Choice of Anesthetic
Factors influencing the choice of anesthetic agent for nerve blocks are similar to those for local infiltration (see Chapter 29 for extensive discussion). In general, most nerve blocks are done for the repair of painful traumatic injuries that are likely to cause pain long after the repair is completed. In such cases, select the anesthetic with the longest duration of action to maximize the patient’s analgesia. For most of the blocks described in this chapter, 0.25% bupivacaine is suggested as the anesthetic of choice, but equal volumes of 1% lidocaine with epinephrine can be substituted. The use of epinephrine on end-organ areas has traditionally been discouraged (e.g., tip of the nose, peripheral ear pinna, distal end of the penis), although the theoretical risk is unsubstantiated in clinical practice. Recent literature describes the use and confirms the safety of lidocaine with epinephrine (1 : 100,000 concentration) for digital blocks.1 It would be prudent to avoid epinephrine-containing anesthetics in injuries involving vascular compromise or for those with obvious peripheral artery disease. Higher concentrations of lidocaine (≤2%) or bupivacaine (0.5%) are commonly used for large nerves. Ropivacaine is a relatively new amide anesthetic with a rapid onset and a long duration of action (several hours). It has been reported to have fewer cardiotoxic and central nervous system effects than bupivacaine does.2,3 Take care to avoid exceeding the recommended dosages of the anesthetic chosen. Buffering the anesthetic is strongly encouraged to lessen the pain of infiltration (see Chapter 29).
Locating the Nerve
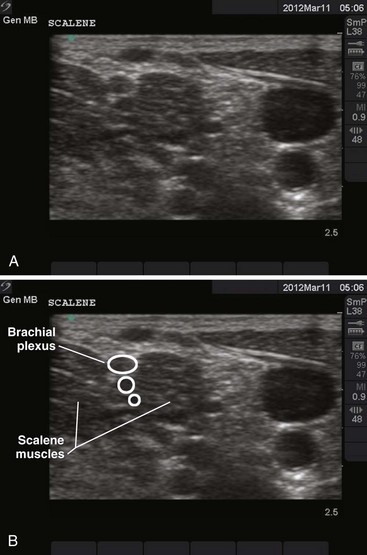
Ultrasound
Use of ultrasound to identify injection sites for peripheral nerve blocks has been gaining popularity. Ultrasound guidance has been used successfully to locate and block nerves in the neck (e.g., interscalene and phrenic nerve blocks), lower extremity (e.g., femoral and saphenous nerve blocks), upper extremity (e.g., radial, ulnar, and median nerve blocks at the elbow), and the lumbar plexus.4–7 Ultrasonographic guidance negates the effects of anatomic variability, provides real-time needle guidance, and allows the operator to visualize the “spread” of local anesthetic.
Paresthesia
A common technique to ensure that the tip of the needle is in close proximity to the nerve is to elicit a paresthesia. Touching and mechanically stimulating the nerve with movement of the needle tip produces a tingling sensation or jolt known as a paresthesia, and it is felt along the distribution of the nerve. In practice, the jolt of a true paresthesia is often difficult to distinguish from the “ouch” of a pain-sensitive structure. When blocking proximal nerves at the elbow or axilla, the paresthesia travels far enough away from the injection site that it can be reliably distinguished from locally induced pain. Paresthesias at the level of the hand and wrist are more difficult to distinguish from pain. In both cases, paresthesia is a subjective feeling that requires intelligent and cooperative patients to understand what they are expected to feel and to remain relaxed and attentive so that they can distinguish an “ouch” from a jolt. Before the procedure, a simple explanation of what the patient should or may feel will facilitate cooperation. While eliciting paresthesias is generally reliable in demonstrating that the needle is close to its target, some authors believe that it may theoretically increase the rate of complications as a result of mechanical trauma or intraneural injection.8–10 Once the paresthesia is elicited, it is important to withdraw the needle 1 to 2 mm before injecting the anesthetic. If a paresthesia persists, stop the injection and reposition the needle.
Complications and Precautions
Nerve Injury
Nerve injury is rare but can occur secondary to (1) chemical irritation from the anesthetic, (2) direct trauma from the needle, or (3) ischemia as a result of intraneural injection. Overall, the incidence of serious neuronal injury is rare and occurs in 1.9 per 10,000 blocks.11 Given that placement of a nerve block is a blind procedure, nerve injuries do not necessarily represent an error in technique.
Chemical neuritis from the anesthetic is the most common nerve injury.9,10 The patient may complain of pain and varying degrees of nerve dysfunction, including paresthesia or motor or sensory deficit. Most cases are transient and resolve completely. Supportive care and close follow-up are the mainstays of treatment. Emergency clinicians should not exceed the recommended doses and concentrations of anesthetic (Table 31-1). In general, lidocaine 1% or 2% or bupivacaine 0.25% or 0.5% is safe for nerve blocks performed in the ED.
Intravascular Injection
Intraarterial injection of anesthetics with epinephrine may cause peripheral vasospasm and further compromise injured tissue. Intravascular anesthetic is not toxic to the limb itself, although it may produce transient blanching of the skin by displacing blood from the vascular tree. Epinephrine, however, can cause prolonged vasospasm and subsequent ischemia if it is injected into an artery. This is especially worrisome when anesthetizing areas with little collateral circulation, such as the toes, fingers, penis, and tip of the nose. Severe epinephrine-induced tissue blanching or vasospasm may be reversed with local or intravascular injection of phentolamine (see extensive discussion in Chapter 29).
Vasospasm associated with the epinephrine in anesthetic solutions is rare, but experience in related clinical situations can help guide therapy. Roberts and Krisanda used a total of 5 mg of phentolamine infused intraarterially to reverse arm ischemia following 3 mg of epinephrine inadvertently administered into the brachial artery during cardiac resuscitation.12 Digital ischemia from inadvertent epinephrine autoinjection (Epi-Pen) has been treated both by proximal “digital block” with 2 mg of phentolamine and by local infiltration at the ischemic site with 1.5 mg of phentolamine.13,14
The route of phentolamine administration should be guided by the clinical situation. Phentolamine must reach the site of vasospasm. Local infiltration may be effective for ischemia in a single toe or finger, whereas arterial injection has the advantage of delivering the medication directly to the arteries exhibiting spasm. For larger areas of involvement or in instances in which local infiltration is ineffective, use intraarterial injection. A dose of 1.5 to 5 mg appears to be effective in most cases,12–14 although a total of 10 mg may be used for local infiltration. Phentolamine, 5 mg, can be mixed with 5 to 10 mL of either normal saline or lidocaine. The small volume of the distal pulp space may limit the volume of the infiltration dose to 0.5 to 1.5 mL in the fingertip. Larger volumes and dosages can be used with proximal infiltrations. For intraarterial infusion of the radial artery at the wrist or the dorsalis pedis at the ankle, dosages of 1.5 to 5 mg of phentolamine are suitable. Slow infusion or graded dosages of 1 mg may provide enough phentolamine to reverse the ischemia without excessive systemic effects such as hypotension.
Systemic Toxicity
The incidence of systemic toxicity with local anesthetics has diminished significantly in the past 30 years. Interestingly, peripheral nerve blocks have been reported to have the highest incidence of systemic toxicity.11 Allergic reactions account for only 1% of untoward reactions (see Chapter 29).15
Specific Nerve Blocks
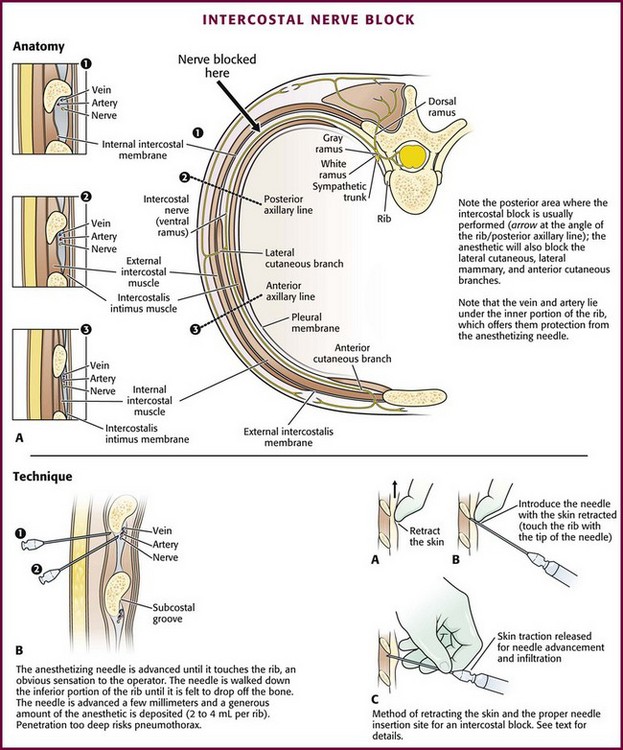
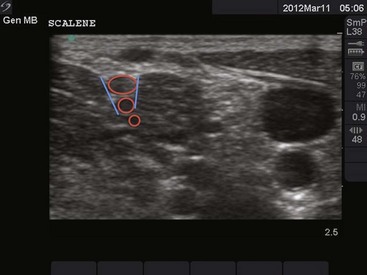
Blocking the intercostal nerves produces anesthesia over an area of their cutaneous distribution (Fig. 31-1) and provides considerable pain relief for patients with rib contusions or fractures. Rib fractures are typically quite painful and cause the patient to try to splint respirations to avoid excessive movement of the injured site. The resulting hypoventilation, atelectasis, and poor expectoration from splinting respirations may cause hypoxia or lead to pneumonia. This is particularly true in patients with preexisting pulmonary disease and minimal respiratory reserve, in whom further impairment of function may cause significant respiratory compromise.
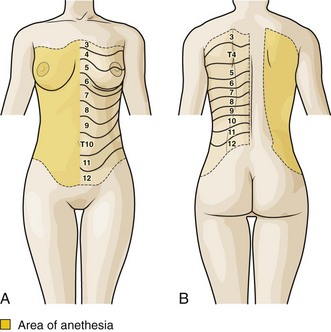
Figure 31-1 A and B, Intercostal nerve block: area of anesthesia and cutaneous distribution of the intercostal nerves.
Theoretically, anesthetizing injured ribs eases pain and facilitates deep breathing and coughing. Unfortunately, no controlled studies have compared intercostal blocks and oral analgesics in patients with the types of rib fractures that are commonly managed on an outpatient basis. However, studies do suggest that intercostal blocks may be superior to analgesics in patients who have undergone thoracotomy.16–18 In these studies, those receiving intercostal nerve blocks had better results on pulmonary function tests, greater oxygenation, and earlier ambulation and discharge than did those receiving opioid analgesics.
Finally, a wrongly perceived high incidence of pneumothorax and unsuccessful blocks deters many clinicians from performing intercostal nerve blocks in the ED. The true incidence of pneumothorax after intercostal nerve blocks is very low and not significant enough to prohibit the procedure. Moore reported that in more than 10,000 individual rib blocks performed, the incidence of pneumothorax was less than 0.1%.19 However, Shanti and associates reported that the incidence of pneumothorax was 1.4% for each individual intercostal nerve blocked.20 If more than one nerve requires blockade, the incidence of pneumothorax may be greater. The suggested approach to discussing intercostal blocks is to give patients the facts with regard to the duration of analgesia and possible complications and then allow them to decide on the method for themselves. Frequently, they prefer oral analgesics initially but may return for further relief of pain, at which time they are more amenable to a nerve block.
Anatomy
Each thoracic nerve exits the spine through the intervertebral foramen, which lies midway between adjacent ribs (Fig. 31-2A). It immediately gives off the posterior cutaneous branch, which supplies the skin and muscles of the paraspinal area. The intercostal nerve then continues around the chest wall and gives off lateral cutaneous branches at the midaxillary line. These branches are the sensory supply to the anterior and posterior lateral chest wall.
Technique
To achieve adequate analgesia for most rib fractures, the lateral cutaneous branch needs to be anesthetized. Therefore, perform blocks between the posterior axillary and midaxillary line at a point proximal to the origin of this branch (see Fig. 31-2A, arrow). Explain the procedure and its benefits and its risks, including potential pneumothorax, systemic toxicity, and ineffective block, before proceeding.
Use a 10-mL syringe with a 3.75-cm, 25-gauge needle. Prepare the area to be injected in the usual aseptic manner. Use the index finger of the nondominant hand to retract the skin at the lower edge of the rib cephalad and pull it up and over the rib (see Fig. 31-2B). With the syringe in the opposite hand, puncture the skin close to the tip of the finger that is retracting the skin over the rib. Keep the syringe at an 80-degree angle to the chest wall with the needle pointing cephalad, and rest the hand holding the syringe on the chest wall for stability. In this position, the depth of needle penetration is well controlled. Slowly advance the needle until it comes to rest on the lower border of the rib. The bone should be felt through the tip of the needle.
Precautions
If the clinician inadvertently causes a pneumothorax, treatment depends on its size. Many pneumothoraces from this procedure are small and require no specific intervention. Those smaller than 20% may be observed for 6 hours.21 During this time, administer a high concentration of oxygen to help decrease the size of the pneumothorax. If the pneumothorax does not enlarge, the patient may be released home with arrangements for close follow-up. Needle or catheter aspiration of larger pneumothoraces may be all that is needed. A chest tube is necessary if this method fails (see Chapter 10).
Nerve Blocks of the Upper Extremity
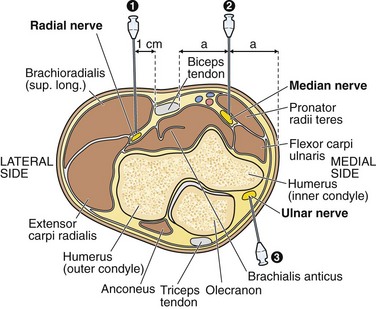
Nerve Blocks at the Elbow
The median, ulnar, and radial nerves can be blocked at the elbow to provide anesthesia to the distal end of the forearm and hand (Fig. 31-3). For most injuries extensive enough to require a nerve block at the elbow, all three nerves must be blocked for successful anesthesia because of the variable and overlapping innervation of the forearm. Furthermore, injuries to the proximal and middle aspects of the forearm may require additional circumferential subcutaneous field blocks of the lateral, medial, and posterior cutaneous nerves.
Ulnar Nerve: Anatomy and Technique (Fig. 31-4A): The ulnar nerve can be palpated in the ulnar groove on the posteromedial aspect of the elbow between the olecranon and the medial condyle of the humerus. This nerve supplies innervation to the small finger, the ulnar half of the ring finger, and the ulnar aspect of the hand.
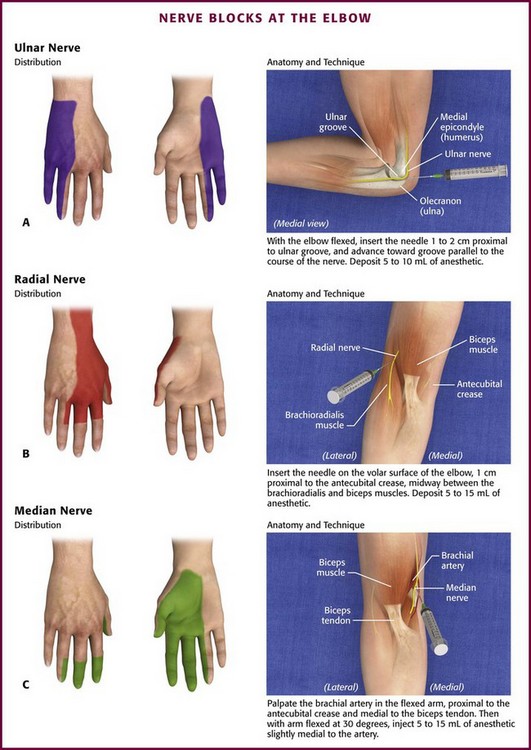
Figure 31-4 Nerve blocks at the elbow.
Radial Nerve: Anatomy and Technique (Fig. 31-4B): The radial nerve and sensory branch of the musculocutaneous nerve run together in the sulcus between the biceps and brachioradialis muscles on the anterolateral aspect of the elbow. The block produces anesthesia of the lateral dorsum of the hand and the lateral aspect of the forearm.
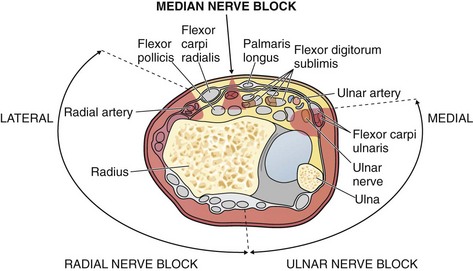
Nerve Blocks at the Wrist
The anatomy and technique for blocking each nerve follow. Note that the median nerve lies in the midline and deep to the fascia and the ulnar and radial nerves lie on their respective sides and have branches that wrap around dorsally. Blocking all three nerves at the wrist requires a block that when viewed end-on, roughly resembles a horseshoe straddling a horseshoe stake (Fig. 31-5).
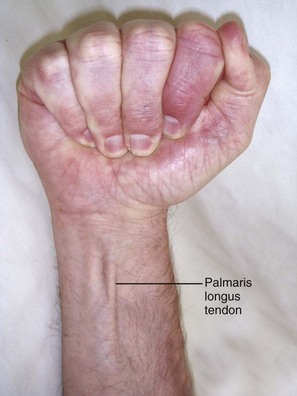
Median Nerve: Anatomy and Technique (Fig. 31-6A): In the wrist, the median nerve lies just below the palmaris longus tendon or slightly radial to it between the palmaris longus and flexor carpi radialis tendons. Both tendons are easily palpated, but the palmaris longus may be absent in up to 20% of patients, in which case the nerve is found about 1 cm in the ulnar direction from the flexor carpi radialis tendon. The nerve lies deep to the fascia of the flexor retinaculum, but at a depth of 1 cm or less from the skin. The superficial position of the median nerve at the wrist is emphasized because a major cause of failure of this block is to instill the anesthetic too deep.
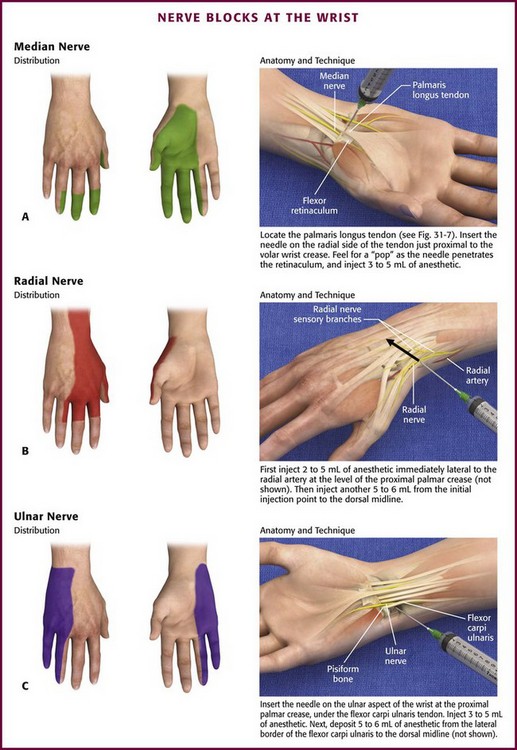
Figure 31-6 Nerve blocks at the wrist.
The palmaris longus tendon is located by having the patient make a fist with the wrist flexed against resistance (Fig. 31-7). Insert a 3.75-cm, 25-gauge needle perpendicular to the skin on the radial border of the palmaris longus tendon just proximal to the proximal wrist crease. Advance the needle slowly until a slight “pop” is felt as the needle penetrates the retinaculum and a paresthesia is produced. If no paresthesia ensues, it may be elicited in a more ulnar direction under the palmaris longus tendon. If a paresthesia is still not elicited, deposit 3 to 5 mL of anesthetic in the proximity of the nerve at a depth of 1 cm under the tendon. Although the nerve is surprisingly close to the skin, it is better to err slightly on the deep side of the retinaculum and continue depositing anesthetic as the needle is withdrawn because the retinaculum is an effective barrier to a successful nerve block from superficially injected anesthetic.
Radial Nerve: Anatomy and Technique (Fig. 31-6B): The radial nerve follows the radial artery into the wrist but gives off sensory nerve branches proximal to the wrist. These branches wrap around the wrist and fan out to supply the dorsal and radial aspect of the hand.
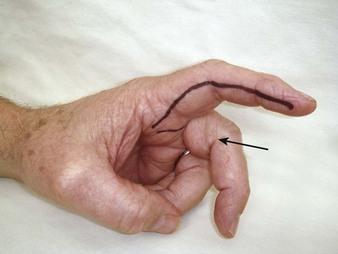
Ulnar Nerve: Anatomy and Technique (Fig. 31-6C): The ulnar nerve follows the ulnar artery into the wrist, where they both lie deep to the flexor carpi ulnaris tendon. The flexor carpi ulnaris tendon is easily palpated just proximal to the prominent pisiform bone by having the patient flex the wrist against resistance. At the level of the proximal palmar crease, the artery and nerve lie just off the radial border of the flexor carpi ulnaris tendon; however, the nerve lies between the tendon and the artery and deep to the artery, which makes it difficult to approach the nerve from the volar aspect of the wrist without involving the artery.
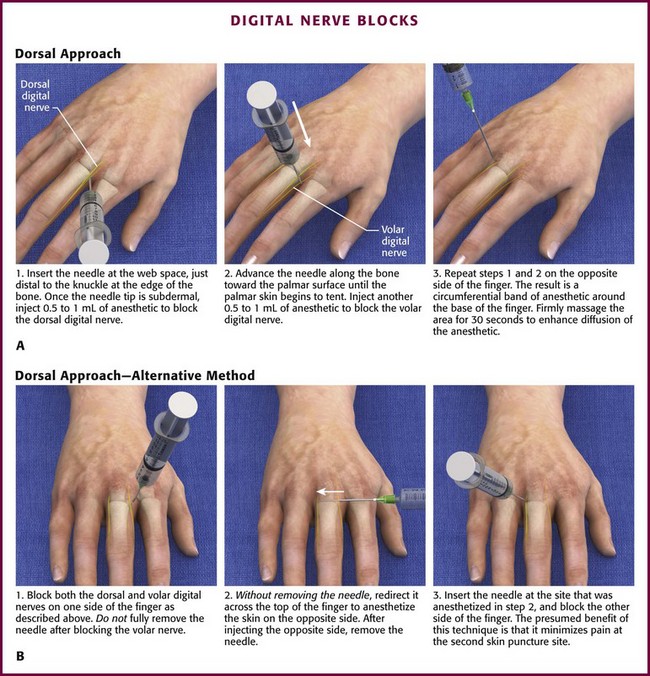
Nerve Blocks of the Digits
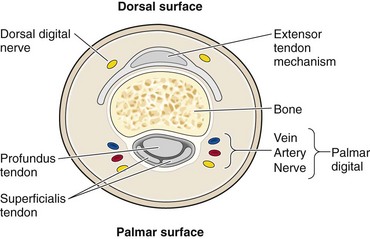
Anatomy: Each finger is supplied by two sets of nerves. These nerves, the dorsal and palmar digital nerves, run alongside the phalanx at the 2- and 10-o’clock positions and the 4- and 8-o’clock positions, respectively (Fig. 31-8).
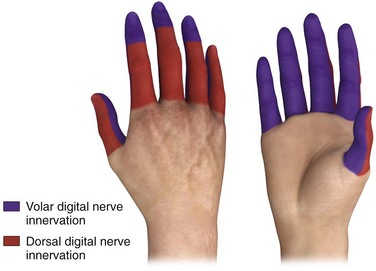
The principal nerves supplying the finger are the palmar digital nerves, also called the common digital nerves. These nerves originate from the deep volar branches of the ulnar and median nerves, where they branch in the wrist. The palmar digital nerves follow the artery along the volar lateral aspect of the bone, one on each side, and supply sensation to the volar skin and interphalangeal joints of all five digits (Fig. 31-9). In the middle three fingers, these nerves also supply the dorsal distal aspect of the finger, including the fingertip and nail bed. Although many clinicians routinely block both sets of digital nerves, in the presence of normal anatomy, only the volar (palmar) branches must be blocked to obtain adequate anesthesia of the middle three fingers distal to the distal interphalangeal joint.
The dorsal digital nerves originate from the radial and ulnar nerves, which wrap around to the dorsum of the hand. They supply the nail beds of the thumb and small finger and the dorsal aspect of all five digits up to the distal interphalangeal joints. Unlike the middle three fingers, which require blocking of only the two volar (palmar) digital nerves, all four nerves are usually blocked in the thumb and fifth finger, particularly to obtain anesthesia of the fingertip and nail bed (Fig. 31-10).
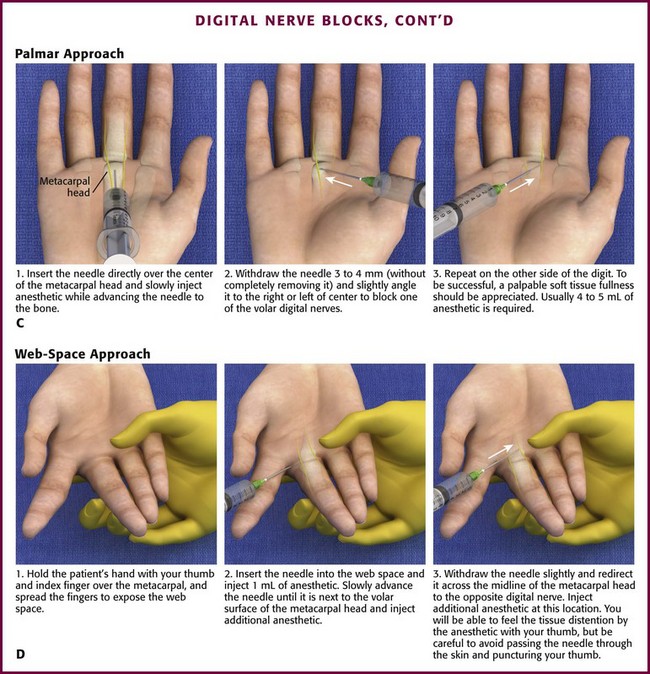
Technique: The digital nerves can be blocked anywhere in their course, including sites in the finger, in the web space between the fingers, and between the metacarpals in the hand. There are a variety of approaches to the nerves, including the dorsal and palmar approaches and the web space approach. Each has its merits., and the technique is similar at each level.
The dorsal approach can be used in the dorsum of the hand at the metacarpals, just proximal to the finger webs at the proximal end of the proximal phalanx or distal to the web space. Clinical situations may dictate which site to use; however, given equal circumstances, the preferred site is just proximal to the finger web. Here, the nerve’s location is more consistent than in the hand, and there is more soft tissue space to accommodate the volume of injected anesthetic than there is in the distal end of the finger. Digital block at the web space is more efficacious in onset and requires less time to achieve anesthesia than does a metacarpal block done proximal to the metacarpophalangeal joint.22
The clinician must first decide whether two or four digital nerves require blocking (see earlier discussion). As noted previously, the authors recommend performing the block from the dorsal surface where the skin is thinner, easier to penetrate, and less sensitive than skin on the volar surface. Insert a 3.75-cm, 25- or 27-gauge needle at the web space, just distal to the knuckle at the lateral edge of the bone (Fig. 31-11A). Once the tip of the needle is subdermal, it usually contacts the bone. At this point, create a skin wheal by injecting 0.5 to 1 mL of anesthetic without epinephrine. This serves to block the dorsal digital nerve and provide anesthesia at the injection site. Pass the needle lateral to the bone and toward the palmar surface until the palmar skin starts to tent slightly. Withdraw the needle 1 mm and inject 0.5 to 1.5 mL of anesthetic. This procedure is repeated on the opposite side of the finger. The result is a circumferential band of anesthetic at the base of the finger. Firm massage of the injected area for 15 to 30 seconds enhances diffusion of the anesthetic through the tissue to the nerves.
A variation of the dorsal approach is performed as follows. After injecting one side of the finger, pull the needle back slightly (without removing it) and redirect it across the top of the digit to anesthetize the skin on the opposite side (see Fig. 31-11B). Completely withdraw the needle and reinsert it at the site that was just anesthetized, and continue the block as described earlier. The presumed advantage of this method is that it minimizes the pain of the second skin puncture. However, because this technique requires the needle to be placed across the dorsal aspect of the finger, it increases the risk for extensor tendon puncture and trauma.
The palmar and web space approaches can be used most successfully for the middle three fingers when only a single puncture is required to block both volar nerves. This technique takes advantage of the anatomic fact that only the volar digital nerves must be blocked to obtain anesthesia of the total finger (except the proximal dorsal surface). If the thumb or fifth finger must be anesthetized, the dorsal branches must also be blocked to obtain anesthesia of the fingertip and fingernail area (see Fig. 31-10).
The palmar approach requires an injection in the palm, which is more painful than an injection in the dorsal skin. Insert the needle directly over the center of the metacarpal head and slowly inject the anesthetic as the needle is advanced to the bone (see Fig. 31-11C). At this point, withdraw the needle 3 to 4 mm and redirect it slightly to the left and right of center to block both digital nerves without withdrawing the needle. To be successful, a palpable soft tissue fullness should be appreciated. The technique requires 4 to 5 mL of anesthetic.
With the web space approach, hold the patient’s hand with your thumb and index finger over the dorsal and volar surface of the metacarpal head, respectively. Use your third finger to separate the patient’s fingers to expose the web space while your fourth and fifth fingers support the patient’s finger being anesthetized (Fig. 31-11D). Insert the needle into the web space and inject 1 mL of anesthetic. Slowly advance the needle until it is next to the lateral volar surface of the metacarpal head and inject additional anesthetic. Withdraw the needle slightly and redirect it across the midline of the metacarpal head to the opposite digital nerve. Use the index finger to palpate “a fullness” as the anesthetic is injected. Again, firm massage of the injected area for 15 to 30 seconds enhances diffusion of the anesthetic through the tissue to the nerves. When needed, redirect the needle to the adjacent finger without withdrawing it to block both fingers with a single puncture (Fig. 31-12).
Alternative Techniques
Jet Injection Technique: Jet injection for a digital nerve block can be used effectively and is less painful than standard needle techniques.23 The technique described by Ellis and Owens uses 0.15 mL of 1% lidocaine delivered by a jet injector at 2600 psi.23 Make three injections in the lateral aspect of the proximal phalanx: the first, midway between the volar and dorsal surfaces; the second, dorsal to this; and the third, volar. Administer a combined total of 0.45 mL to each side of the phalanx at the 2-, 3-, and 4-o’clock positions and the 8-, 9-, and 10-o’clock positions in relation to the bone.
Transthecal Digital Block Technique: A transthecal block is performed by making a single injection into the flexor tendon sheath, which produces rapid and complete finger anesthesia. It was first described by Chiu in 1990, who noted rapid finger anesthesia after injection treatment of a trigger finger.24 Cadaver studies suggest that the injected fluid diffuses out of the tendon sheath and around the phalanx and all four digital nerves.
Palpate the flexor tendon in the palm proximal to the metacarpophalangeal joint. Introduce a 25-gauge needle attached to a 3-mL syringe at a 45-degree angle and advance it toward the tendon sheath while maintaining constant slight pressure on the plunger of the syringe (Fig. 31-13). When the sheath has been entered, the anesthetic should flow freely. If it does not, it is presumed that the tendon has been entered. If this happens, withdraw the syringe slowly (while keeping slight pressure on the plunger) until anesthetic flows smoothly and easily. Inject a total of 2 mL of anesthetic solution (smaller volumes should be used in children). After the needle is removed, apply pressure over the tendon proximally to facilitate distal spread. The average onset of anesthesia is 3 minutes.25
The advantage of this technique is a single injection. However, Hill and colleagues found the technique to be “clinically equal” to traditional digital blocks.26 Other authors have stated that the traditional digital block is easier to perform and produces less pain during and after injection.27 Theoretically, the technique may increase risk for injury to the tendon.
Complications and Precautions: The injection should go in smoothly, without resistance during injection. Although the finger is forgiving of transient pressure from excessive anesthetic, if the injection site becomes excessively tense, digital perfusion may be compromised. Even if epinephrine-containing solutions are used for a digital block in otherwise healthy individuals without peripheral vascular disease, it is unlikely that serious ischemic injury will occur.28 Significant vasoconstriction generally lasts less than 60 minutes, within the time interval for which an ischemic tourniquet can safely be used in the same area.29 However, if the entire digit remains blanched for more than 15 minutes, it is prudent to reverse the α-agonism of epinephrine with phentolamine (see Chapter 29). Using a pulse oximeter on the affected finger may help quantitate the degree of ischemia.30
The small size of the digital arteries and nerves makes intravascular or intraneural injection less likely. Inadvertent intravascular injection may cause digital ischemia from vasospasm or displacement of blood out of the capillary bed by the anesthetic. Blanching of the finger as the anesthetic is injected suggests intravascular injection. If this is observed, immediately discontinue the injection. Usually, the ischemia is transient and self-resolving, and serious complications are rare. Massage or topical application of nitroglycerin paste may be attempted if the ischemia persists.31
Nerve Blocks of the Lower Extremity
Femoral Nerve Block (Three-In-One Block)
A femoral nerve block provides significant analgesia to the proximal end of the femur and complete analgesia to the femoral shaft. It has been used to supplement anesthesia for a variety of surgical procedures on the anterior aspect of the thigh and knee and to provide postoperative analgesia after hip surgery.32 In the ED, this block is primarily used to provide analgesia for patients with hip fractures. It can be especially helpful in the management of elderly patients and those with respiratory compromise or poor pulmonary reserve, in whom high doses of opiate analgesics may be problematic.
Because the femoral and three-in-one nerve blocks are technically similar and associated with the same potential complications, the fact that the three-in-one nerve block provides better analgesia of the femoral neck and hip joint would seem to make it the logical choice. In clinical practice, however, the lateral femoral cutaneous nerve is less likely to be blocked than the femoral nerve, and the obturator nerve is frequently left unblocked despite proper technique.33 Nevertheless, because of potentially better analgesia obtained with the three-in-one nerve block and no clinically significant downside in comparison to a femoral nerve block, the remainder of the section will focus on performing the three-in-one nerve block.
Anatomy (Fig. 31-14A): The femoral nerve is formed from the posterior branches of L2-L4 and is the largest branch of the lumbar plexus. The nerve emerges from the psoas muscle and descends between the psoas and iliacus muscles. It passes under the inguinal ligament in the groove formed by these muscles lateral to the femoral artery and divides into anterior and posterior branches. The anterior branches innervate the anterior aspect of the thigh, and the posterior branches innervate the quadriceps muscle and continue below the knee as the saphenous nerve to provide sensory innervation from the medial side of the calf to the medial malleolus.
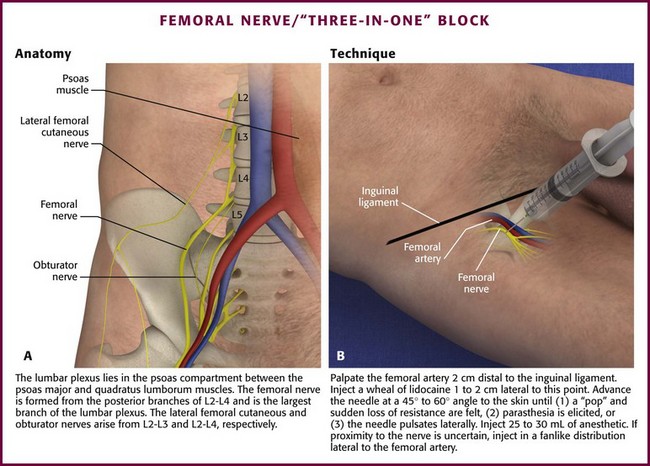
Figure 31-14 The femoral nerve/“three-in-one” block.
Technique (Fig. 31-14B): Place the patient in a supine position and prepare the skin overlying the femoral triangle in the usual fashion. Palpate the femoral artery 1 to 2 cm distal to the inguinal ligament and inject a subcutaneous wheal of local anesthetic 1 to 2 cm lateral to this point. Keep the nondominant hand on the femoral artery throughout the remainder of the procedure. Insert a 3.75-cm 25- to 22-gauge needle just lateral to the artery at a 45- to 60-degree angle to the skin. Slowly advance the needle cephalad until one of the following occurs: a “pop” with sudden loss of resistance (signifying penetration into the femoral nerve sheath) is felt, a paresthesia is elicited, or the needle pulsates laterally, which signifies a position adjacent to the femoral artery. Inject 25 to 30 mL of anesthetic. The block usually takes 15 minutes to take effect. If proximity to the nerve is uncertain (e.g., a pop is not appreciated, a paresthesia is not elicited, or the needle does not move with pulsation of the femoral artery), inject the anesthetic in a fanlike distribution lateral to the femoral artery in an attempt to anesthetize the nerve.
Some experts recommend applying finger pressure 2 to 4 cm below the injection site to help spread the local anesthetic proximally to the obturator and lateral femoral cutaneous nerves. However, an imaging study suggested that blockade occurs through lateral (lateral femoral cutaneous nerve) and medial (obturator nerve) spread of injected anesthetic.34
Nerve Blocks of the Ankle
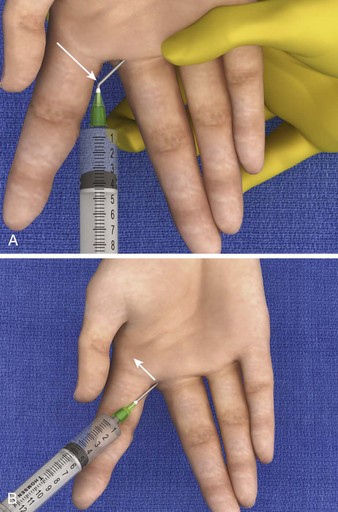
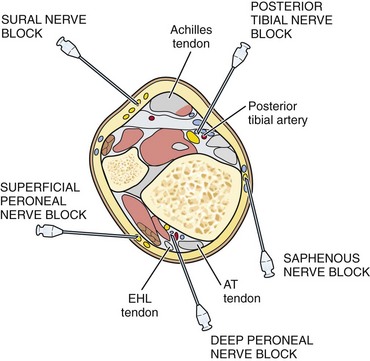
Anatomy: The foot is supplied by the five nerve branches of the principal nerve trunks. Three nerves are located anteriorly and supply the dorsal aspect of the foot. Two nerves are located posteriorly and supply the volar aspect.
The anteriorly located nerves are the superficial peroneal, deep peroneal, and saphenous nerves (Fig. 31-15A). The superficial peroneal nerve (also called the dorsal cutaneous or musculocutaneous nerve) actually consists of multiple branches that supply a large portion of the dorsal aspect of the foot. These nerves are located superficially between the lateral malleolus and the extensor hallucis longus tendon, which is easily palpated by having the patient dorsiflex the big toe. The deep peroneal nerve (also called the anterior tibial nerve) supplies the web space between the big and second toes. In the ankle it lies under the extensor hallucis longus tendon. The saphenous nerve runs superficially with the saphenous vein between the medial malleolus and the tibialis anterior tendon, which is prominent when the patient dorsiflexes the foot. The saphenous nerve supplies the medial aspect of the foot near the arch.
The posteriorly located nerves are the posterior tibial and sural nerves (see Fig. 31-15B). The sural nerve runs subcutaneously between the lateral malleolus and the Achilles tendon and supplies the lateral border, both volar and dorsal, of the foot. The posterior tibial nerve runs with the posterior tibial artery, which can be palpated between the medial malleolus and the Achilles tendon. It lies slightly deep and posterior to the artery.
Technique: A complete nerve block of the foot requires blocking three subcutaneous nerves and two deeper nerves (Fig. 31-16). Once familiar with the anatomy, an experienced clinician can anesthetize all five nerves quickly by placing subcutaneous band blocks around 75% of the ankle circumference and two deep injections: one next to the palpable posterior tibial artery and the other under the extensor tendon of the big toe.
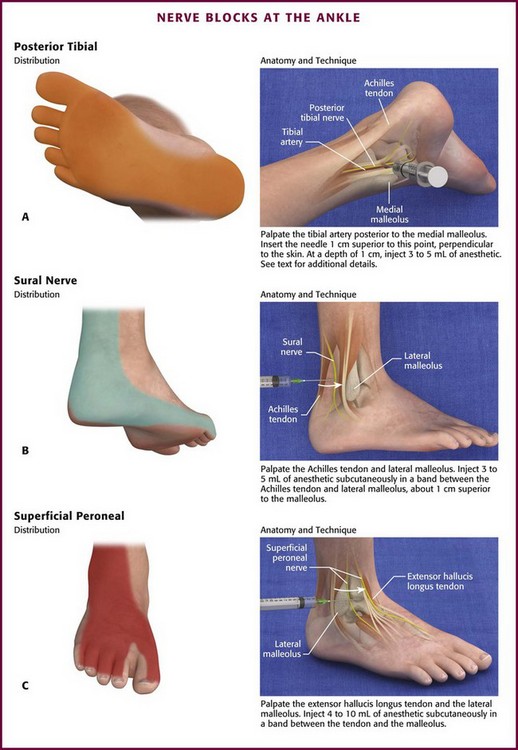
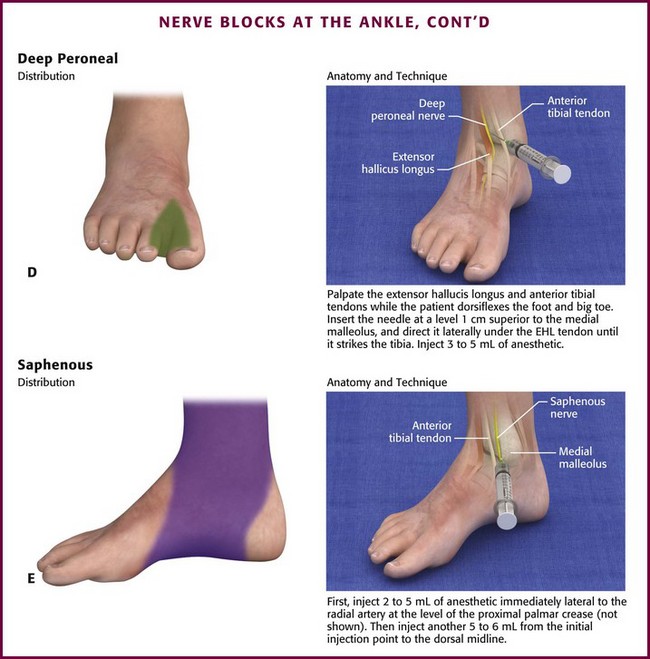
Posterior Tibial Nerve (Fig. 31-17A): Block the posterior tibial nerve in the medial aspect of the ankle between the medial malleolus and the Achilles tendon. Palpate the tibial artery just posterior to the medial malleolus. The injection site is 0.5 to 1.0 cm superior to this point. If the artery is not palpable, use a point 1 cm above the medial malleolus and just anterior to the Achilles tendon.
Sural Nerve (Fig. 31-17B): Block the sural nerve on the lateral aspect of the ankle between the Achilles tendon and the lateral malleolus. Inject 3 to 5 mL of anesthetic subcutaneously in a band about 1 cm above the lateral malleolus between the Achilles tendon and the lateral malleolus.
Superficial Peroneal Nerves (Fig. 31-17C): Block the superficial peroneal nerves on the anterior aspect of the ankle between the extensor hallucis longus tendon and the lateral malleolus by subcutaneously injecting 4 to 10 mL of anesthetic in a band between these landmarks.
Deep Peroneal Nerve (Fig. 31-17D): Block the deep peroneal nerve anteriorly beneath the extensor hallucis longus tendon. The injection site is 1 cm above the base of the medial malleolus between the extensor hallucis longus and anterior tibial tendons. Palpate the tendons by having the patient dorsiflex the big toe and foot, respectively. Create a lidocaine wheel at the injection site. Direct the needle about 30 degrees laterally and under the extensor hallucis longus tendon until it strikes the tibia (at a depth of <1 cm). Withdraw the needle 1 mm and inject 3 to 5 mL of anesthetic.
Nerve Blocks of the Metatarsals and Toes
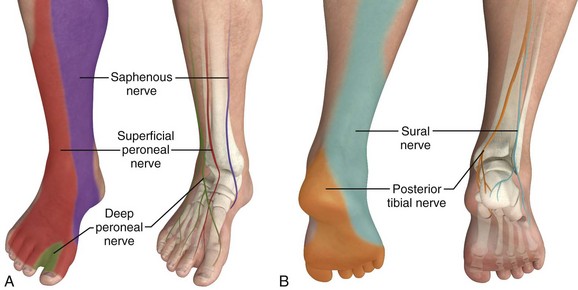
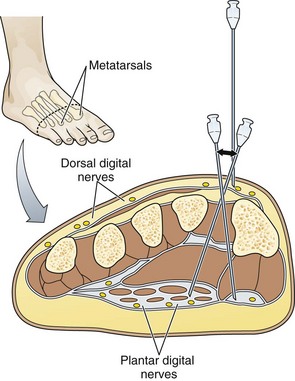
Anatomy: Each toe is supplied by two dorsal and two volar nerves, which are branches of the major nerves of the ankle. The dorsal digital nerves are the terminal branches of the deep and superficial peroneal nerves. The volar nerves are branches of the posterior tibial and sural nerves.
The location of the nerves in relation to the bones varies with the site of the foot. In the toes, the nerves lie at the 2-, 4-, 8-, and 10-o’clock positions in close relationship to the bone. In the proximal part of the foot, the nerves run with the tendons and are not in close relationship with the bones (Fig. 31-18).
Technique: The digital nerves can be blocked at the metatarsals, interdigital web spaces, or toes. The bones of the foot can be palpated easily from the dorsum and are used as the landmarks for estimating the location of the nerves. Proximally, the nerves’ relationship to the bones is less consistent, which makes definitive needle placement and successful block less reliable. In the toes, the position of the nerves is more consistent; however, minimal subcutaneous tissue space is available for the injected solution. At the web space, the nerves are located in close relationship to the bone, and ample space is available for injecting the anesthetic; hence, for most procedures the web space is the preferred site for a digital nerve block.
The technique for toe and metatarsal blocks is similar (Fig. 31-19). All four nerves supplying each toe are usually blocked because of their sensory overlap. Perform the block from the dorsal surface, where the skin is thinner and less sensitive. Start by placing a 1-mL skin wheal dorsally between the metatarsal bones. Advance the needle until the volar skin tents slightly, and inject 2 mL of anesthetic as the needle is withdrawn. Without removing it, redirect the needle in a different volar direction, and repeat the procedure. Deposit a total of 5 mL of anesthetic in a fanlike pattern in each metatarsal space. Again, because of sensory overlap, two or more spaces need to be anesthetized for each toe to be blocked.
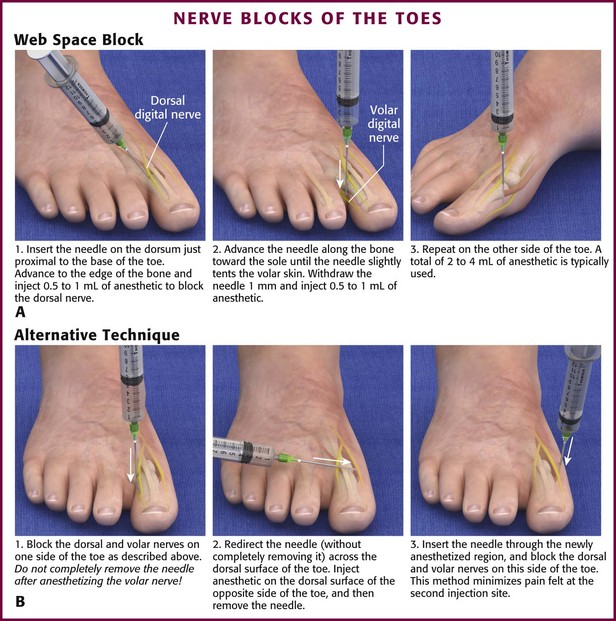
Figure 31-19 Nerve blocks of the toes.
Complications and Precautions: Complications of lower extremity nerve blocks are similar to those associated with nerve blocks performed in the upper extremity and include intravascular injection, local anesthetic toxicity, nerve trauma, hematoma formation, and failure of the block.
The precautions that apply to the hand and fingers apply to the foot and toes. Ischemic complications can be avoided by paying attention to changes in the skin during the injection. Blanching heralds possible intravascular injection or vascular compression. If the skin blanches, halt the procedure and reevaluate the position of the needle and the amount and content of the injected solution. The total volume of anesthesia should not exceed the recommended amount. The literature suggests that epinephrine-containing anesthetics are safe for digital nerve blocks,30 but some clinicians opt for epinephrine-free alternatives because of the theoretical risk for ischemic complications (see the “Complications and Precautions” subsection and Chapter 29).
References
1. Chowdhry, S, Seidenstricker, L, Cooney, DS, et al. Do not use epinephrine in digital blocks: myth or truth? Part II. A retrospective review of 1111 cases. Plast Reconstr Surg. 2010;126:2031.
2. Markham, A, Faulds, D. Ropivacaine: a review of its pharmacology and therapeutic use in regional anaesthesia. Drugs. 1996;52:429.
3. McClellan, KJ, Faulds, D. Ropivacaine: an update of its use in regional anaesthesia. Drugs. 2000;60:1065.
4. Gray, AT, Schafhalter-Zoppoth, I. Ultrasound guidance for ulnar nerve block in the forearm. Reg Anesth Pain Med. 2003;28:335.
5. Gray, AT, Collins, AB. Ultrasound-guided saphenous nerve block. Reg Anesth Pain Med. 2003;28:148.
6. Liebmann, O, Price, D, Mills, C, et al. Feasibility of forearm ultrasonography-guided nerve blocks of the radial, ulnar, and median nerves for hand procedures in the emergency department. Ann Emerg Med. 2006;48:558.
7. Sites, BD, Beach, ML, Spence, BC, et al. Ultrasound guidance improves the success rate of a perivascular axillary plexus block. Acta Anaesthesiol Scand. 2006;50:678.
8. Auroy, Y, Narchi, P, Messiah, A, et al. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology. 1997;87:479.
9. Selander, D, Dhuner, KG, Lundberg, G. Peripheral nerve injury due to injection needles used for regional anesthesia. An experimental study of the acute effects of needle point trauma. Acta Anaesthesiol Scand. 1977;21:182.
10. Selander, D, Edghage, S, Wolff, T. Paresthesia or no paresthesia? Nerve lesions after axillary blocks. Acta Anaesthesiol Scand. 1979;23:27.
11. Faccenda, KA, Finucane, BT. Complications of regional anaesthesia. Incidence and prevention. Drug Saf. 2001;24:413–442.
12. Roberts, JR, Krisanda, TJ. Accidental intra-arterial injection of epinephrine treated with phentolamine. Ann Emerg Med. 1989;18:424.
13. Maguire, WM, Reisdorff, MD. Epinephrine-induced vasospasm reversed by phentolamine digital block. J Emerg Med. 1990;8:46.
14. McCauley, WA, Gerace, RV, Scilley, C. Treatment of accidental digital injection of epinephrine. Ann Emerg Med. 1991;20:665.
15. McCaughey, W. Adverse effects of local anaesthetics. Drug Saf. 1992;7:178.
16. Bergh, WB, Pottori, O, Axisonherf, B, et al. Effect of intercostal block on lung function after thoracotomy. Acta Anaesthesiol Scand. 1966;24:85.
17. Delikan, AE, Lee, CK, Young, WK, et al. Postoperative local analgesia for thoracotomy with direct bupivacaine intercostal blocks. Anaesthesia. 1973;28:561.
18. Crawford, ED, Skinner, DG. Intercostal nerve block with thoracoabdominal and flank incisions. Urology. 1982;19:25.
19. Moore, DC. Complications of regional anesthesia. Clin Anesth. 1969;2:281.
20. Shanti, CM, Carlin, AM, Tyburski, JG. Incidence of pneumothorax from intercostal nerve block for analgesia in rib fractures. J Trauma. 2001;51:536.
21. Weissberg, D, Refaely, Y. Pneumothorax: experience with 1,199 patients. Chest. 2000;117:1279.
22. Knoop, K, Trott, A, Syverud, S. Comparison of digital versus metacarpal blocks for repair of finger injuries. Ann Emerg Med. 1994;23:1296.
23. Ellis, GL, Owens, A. The efficacy and acceptability of using a jet injector in performing digital blocks. Am J Emerg Med. 1993;11:648.
24. Chiu, DT. Transthecal digital block: flexor tendon sheath used for anesthetic infusion. J Hand Surg [Am]. 1990;15:471.
25. Morrison, WG. Transthecal digital block. Arch Emerg Med. 1993;10:35.
26. Hill, RG, Jr., Patterson, JW, Parker, JC, et al. Comparison of transthecal digital block and traditional digital block for anesthesia of the finger. Ann Emerg Med. 1995;25:604.
27. Low, CK, Wong, HP, Low, YP. Comparison between single injection transthecal and subcutaneous digital blocks. J Hand Surg [Br]. 1997;22:582.
28. Roth, RD. Utilization of epinephrine containing anesthetic solutions in the toes. J Am Podiatr Assoc. 1981;71:189.
29. Green, D, Walter, J, Heden, R, et al. The effects of local anesthetics containing epinephrine on digital blood perfusion. J Am Podiatr Med Assoc. 1992;82:98.
30. Eastwood, DW. Digital nerve blocks and pulse oximeter signal detection. Anesth Analg. 1992;74:931.
31. Gibbs, NM, Oh, TE. Nitroglycerine ointment for dopamine induced peripheral digital ischemia. Lancet. 1983;2:290.
32. Fletcher, AK, Rigby, AS, Heyes, FLP. Three-in-one femoral nerve block as analgesia for fractured neck of the femur in the emergency department: a randomised controlled trial. Ann Emerg Med. 2003;41:227–233.
33. Reilley, TE, Terebah, VD, Gerhardt, MA. Regional anesthesia techniques for the lower extremity. Foot Ankle Clin North Am. 2004;9:349–372.
34. Marhofer, P, Nasel, C, Sitzwohl, C, et al. Magnetic resonance imaging of the distribution of local anesthetic during the three-in-one block. Anesth Analg. 2000;90:119–124.