Monitoring integrity of the neuromuscular junction
Neuromuscular transmissions
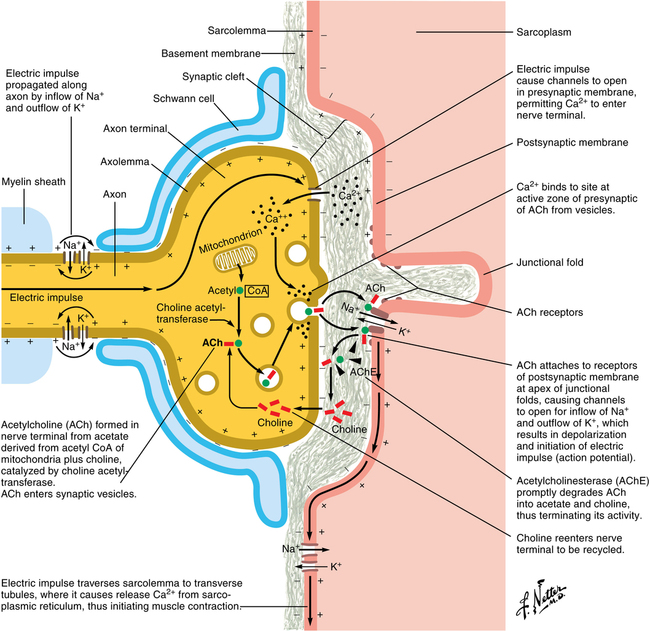
When a nerve impulse arrives at the neuromuscular junction, voltage-gated ion channels open, leading to an influx of calcium within the terminal that causes several hundreds of vesicles of acetylcholine to fuse with the nerve membrane (Figure 19-1). The acetylcholine within these vesicles is released into the synaptic cleft, combining with and activating nicotinic receptors on the motor endplate, the activation of which opens ion channels on the muscle membrane and depolarizes the membrane. The release of calcium from intracellular stores stimulates an interaction between actin and myosin, resulting in muscle contraction.