Minimum alveolar concentration
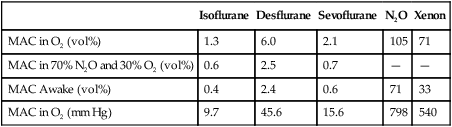
MAC has been determined in different age groups, under different conditions, and for all inhalation anesthetic agents (Table 62-1), allowing for comparison of the potency of the different agents. MAC is inversely related to anesthetic potency and, therefore, with its lipid solubility (Meyer-Overton theory). MAC is analogous to the pharmacologic effective dose (ED50) of drugs.
Table 62-1
Minimum Alveolar Concentration (MAC) and MACawake of Inhalation Anesthetics at Ambient Pressure of 760 mm Hg
| Isoflurane | Desflurane | Sevoflurane | N2O | Xenon | |
| MAC in O2 (vol%) | 1.3 | 6.0 | 2.1 | 105 | 71 |
| MAC in 70% N2O and 30% O2 (vol%) | 0.6 | 2.5 | 0.7 | — | — |
| MAC Awake (vol%) | 0.4 | 2.4 | 0.6 | 71 | 33 |
| MAC in O2 (mm Hg) | 9.7 | 45.6 | 15.6 | 798 | 540 |
Important concepts related to minimum alveolar concentration
Alveolar concentration
Ambient pressure
MAC values are conventionally given as a percentage of alveolar anesthetic concentration at 1 atm. They either have been determined at sea level or, ideally, have been corrected to sea level when determined at higher altitudes. One has to bear in mind that anesthetic potency and uptake are directly related to the partial pressure of the anesthetic agent (see Table 62-1). At higher altitude, as compared with at sea level, the same concentration of an inhalation anesthetic agent will exert a lower partial pressure within the alveolus and, consequently, a reduced anesthetic effect. Modern variable bypass vaporizers compensate for this effect because, although the dials are marked in “percent,” partial pressure is what is actually determined. At an altitude at which the pressure is one half of sea level, a variable bypass vaporizer set to 1% would deliver 2%, though the actual partial pressure of anesthetic agent delivered would be the same. For example, at sea level, with a barometric pressure of 760 mm Hg, the partial pressure of the agent would be 7.6 mm Hg; at an altitude with a barometric pressure of 380 mm Hg, a variable bypass vaporizer set at 1% would actually deliver 2% of the agent (2% of 380 = 7.6 mm Hg partial vapor pressure).
Factors affecting minimum alveolar concentration
Numerous physiologic and pharmacologic factors, disease states, and conditions can change the anesthetic sensitivity and, therefore, raise or lower MAC (Table 62-2). Not all the underlying mechanisms are yet clear (decrease of MAC in pregnancy or increase in redheads). Nevertheless, anesthetic requirements seem to correlate with cerebral metabolic rate, whereas factors decreasing cerebral metabolic rate (temperature, age, severe hypoxia, hypotension, various drugs) decrease MAC.
Table 62-2
Impact of Pharmacologic Agents and Physiologic Factors on Minimum Alveolar Concentration (MAC)
| Decreased MAC ↓ | MAC ↑ |
| Medications | |
| Opioids Benzodiazepines Barbiturates Propofol Ketamine α2-Agonists Intravenously administered local anesthetic agents |
Inhibition of catecholamine reuptake (amphetamines, ephedrine) |
| Alcohol | |
| Acute ethanol ingestion | Chronic ethanol abuse |
| Physiologic Conditions | |
| Increasing age for patients >1 year of age Pregnancy | In the first months of life for infants <6 months of age |
| Pathophysiologic Conditions | |
| Hypothermia Severe hypotension Severe hypoxemia Severe anemia Acute metabolic acidosis Sepsis |
Hyperthermia Hyperthyroidism Increased extracellular Na+ in central nervous system |
| Genetic Factors | |
| None established*† | Genotype related to red hair |
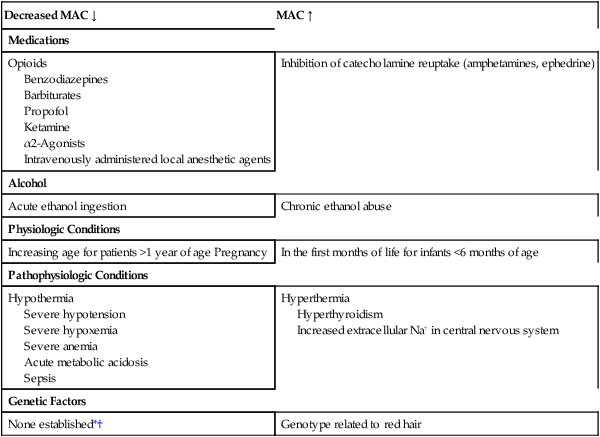
*Gender does not change MAC except in elderly Japanese population in whom MAC might be slightly lower in women.
†No good data comparing MAC in different ethnic groups exist.
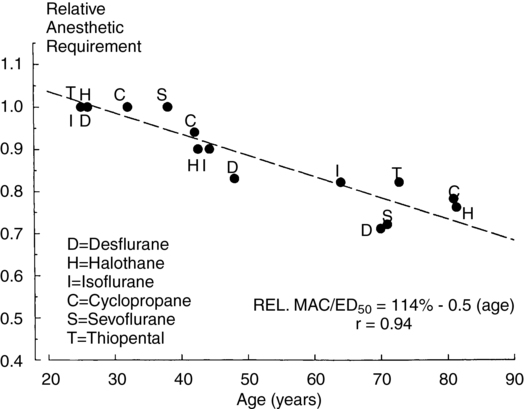
MAC is age dependent (Figure 62-1). The MAC value is highest in infants 3 to 6 months of age. For patients older than 1 year, MAC decreases by approximately 6% to 7% with each increasing decade of life.
Anesthetic requirement to blunt responses to various stimuli
MACawake is the concentration of an inhaled anesthetic agent at which half of patients will open their eyes to command. It is an index of the hypnotic potency of an inhaled anesthetic agent. The knowledge of MACawake is helpful to prevent intraoperative awareness. The MACawake is approximately one third of MAC for isoflurane, desflurane, and sevoflurane but is higher for N2O and xenon (see Table 62-1). Differences in the ratio of MAC to MACawake among different anesthetic agents probably reflect different mechanisms of action. The decrease of MACawake with age is parallel to that of MAC itself. Drugs that suppress central nervous system activity (e.g., fentanyl and clonidine) reduce the MACawake.






