Cardiovascular effects of the inhalation agents
Timothy S.J. Shine, MD and Neil G. Feinglass, MD, FCCP, FASE
There is no one perfect anesthetic agent, though inhalation agents come closest to providing the components of a complete anesthetic (i.e., analgesia, amnesia, hypnosis, and muscle relaxation) as a single agent. All of the inhalation agents depress the cardiovascular system in a dose-dependent fashion (Figure 66-1) through one or more mechanisms, the overall effect of which is a decrease in mean arterial pressure.
Systemic vascular resistance
The decrease in blood pressure that occurs with the use of halothane is due to a reduction in myocardial contractility, heart rate, and systemic vascular resistance (SVR). Isoflurane, sevoflurane, and desflurane decrease blood pressure primarily by decreasing SVR. Isoflurane and desflurane are potent vasodilators (Figure 66-2), with halothane causing a more modest reduction in SVR at equipotent doses. Isoflurane causes up to a 50% reduction in SVR at 1.9 minimum alveolar concentration.
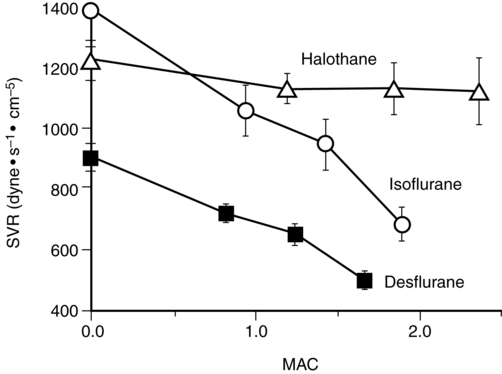
 ) with those of isoflurane (O) and halothane (Δ) on systemic vascular resistance (SVR) in healthy young men. MAC, Minimum alveolar concentration. (From Weiskopf RB, Cahalan MK, Eger EI II, et al. Cardiovascular actions of desflurane in normocarbic volunteers. Anesth Analg. 1991;73:143-156.)
) with those of isoflurane (O) and halothane (Δ) on systemic vascular resistance (SVR) in healthy young men. MAC, Minimum alveolar concentration. (From Weiskopf RB, Cahalan MK, Eger EI II, et al. Cardiovascular actions of desflurane in normocarbic volunteers. Anesth Analg. 1991;73:143-156.)Heart rate
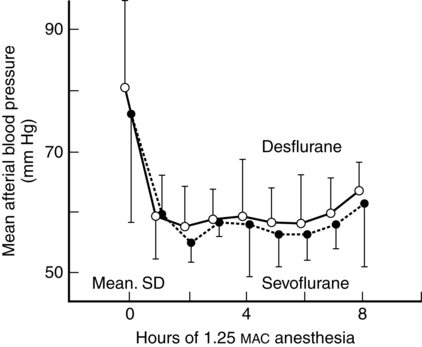
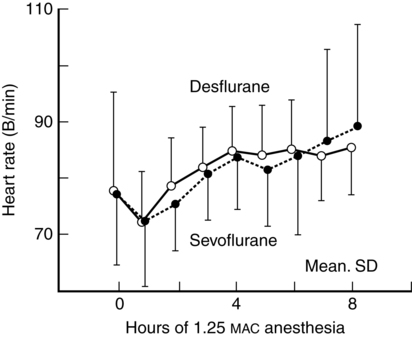
Isoflurane, sevoflurane, and desflurane may increase heart rate (Figure 66-3). Halothane may cause no change or a decrease in heart rate because it impairs baroreceptor function. Isoflurane is less depressant to the baroreflex, and, with a decrease in SVR, a compensatory increase occurs in heart rate even though isoflurane also depresses sympathetic nervous system activity; however, halothane has less effect on the parasympathetic system than on the sympathetic nervous system. Isoflurane anesthesia appears, clinically, to have less effect on cardiac chronicity in patients younger than 40 years of age, as compared with older patients.
Myocardial contractility
As mentioned previously, halothane directly depresses myocardial contractility and stroke volume by altering concentrations of intracellular calcium (Ca2+) at several subcellular targets, whereas the inhalation agents currently used in the United States have fewer or no effects on myocardial contractility (isoflurane = desflurane = sevoflurane) (Table 66-1). Isoflurane can decrease stroke volume, but if a compensating increase in heart rate occurs, cardiac output is maintained. Unfortunately, many patients receive potent opioids that often decrease cardiac chronotropy, and, as noted above, older patients, even in the absence of opioids, most commonly do not have a compensating increase in heart rate. Because cardiac output is preserved with the use of isoflurane, desflurane, and sevoflurane, perfusion of the myocardium and brain are relatively preserved during anesthesia with these agents.
Table 66-1
Cardiovascular Effects of Inhalation Anesthetic Agents
| Agent | Contractility | PVR | SBP |
| Halothane | ↓ | — | ↓ |
| Enflurane | ↓ | ↓ | ↓↓ |
| Isoflurane, desflurane, sevoflurane | — | ↓ | ↓ |
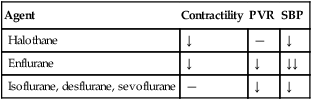
PVR, Peripheral vascular resistance; SBP, systolic blood pressure.
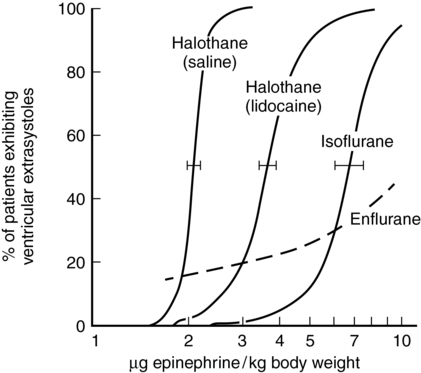
Sensitivity to epinephrine
All of the inhalation agents sensitize the myocardium to the effects of epinephrine, with halothane having the greatest effect, as compared with isoflurane and desflurane. Children are less likely to exhibit this effect than are adults. Drugs that block the reuptake of norepinephrine, such as cocaine and ketamine, also increase the arrhythmogenicity of the inhalation agents. One half the dose of epinephrine required to produce three or more premature ventricular contractions is considered safe (e.g., 1 μg/kg of epinephrine during halothane anesthesia and 3 μg/kg during isoflurane anesthesia are unlikely to cause arrhythmias) (Figure 66-4).