48 Manual Therapy
Certainly many of our patients equate manual therapy exclusively with the manipulative thrust or high-velocity, low-amplitude (HVLA) maneuver practiced by clinicians in the diverse professions of physical therapy, medicine, chiropractic, osteopathy, naprapathy, traditional Chinese medicine, and naturopathy as part of their legislated scope of practice. However, manual therapy, in fact, also encompasses a great variety of other techniques. The American Physical Therapy Association (APTA) has defined manual therapy techniques as “skilled hand movements intended to improve tissue extensibility, increase range of motion, induce relaxation, mobilize or manipulate soft tissue and joints, modulate pain, and reduce soft tissue swelling, inflammation, or restriction”. Techniques matched with these proposed indications for manual therapy include massage, manual lymphatic drainage, manual traction, mobilization/manipulation, and passive range of motion (ROM).1 Although within physical therapy in the United States, defined synonymously as “a manual therapy technique comprised of a continuum of skilled passive movements to joints and/or related soft tissues that are applied at varying speeds and amplitudes, including a small amplitude/high velocity therapeutic movement”, more commonly the term manipulation is used to describe a thrust technique performed at a pathologic end of range of a joint, whereas mobilization describes a nonthrust, sustained or oscillatory, low-velocity movement within or at the end of range of joint motion.1 Additional specified manual therapy interventions include soft tissue and neural mobilization, joint stabilization, and self-mobilization exercises.2
History of Manual Therapy
Early Medicine
Manual therapy is among the oldest recorded interventions in medicine. Documentation of its practice dates back over 4000 years to Egyptian scrolls (Edwin Smith papyrus) and its use was also depicted in ancient Thai sculptures.3 The first mention of massage appears in the Nei Ching, the oldest existing medical work, dedicated to the Chinese Emperor Huang Ti in 2598 BC. Ancient Indian and Greek texts, including the work of Hippocrates, describe massage as an effective therapy for treating injuries resulting from war or sports.4 Hippocrates (460-385 BC) also described a combination of traction and manipulation on the back of a patient lying prone on a wooden bed in his treatise, On Setting Joints by Leverage.5 Whether Hippocrates solely attempted by this method to reposition traumatically displaced vertebrae or if he intended to manipulate slightly luxated vertebrae for a variety of indications, to this day remains a matter of debate.6 The Roman physician Galen (131 to 202) commented on Hippocrates’ techniques in 18 of his 97 surviving treatises, as did the influential Arabic physician Abu Ali ibn Sina, better known as Avicenna (980 to 1037). In 1656, Friar Thomas described manipulative techniques for the extremities in his book, The Complete Bone Setter, and in as late as 1674, Johannes Scultetus still included descriptions of Hippocrates’ manipulative methods in his text, The Surgeon’s Storehouse.7
Manipulation fell out of favor in medicine when Sir Percival Pott (1714 to 1788) described tuberculosis of the spine and condemned traction and manipulation as not only useless but dangerous.5–7 However, manipulation in the form of bone setting continued to be practiced with some of its lay practitioners attaining great notoriety including Sarah Mapp in 18th century and Sir Albert Baker in 20th century England, who both counted royalty among their patients. In the United States, the male members of the Rhode Island Sweet family were reputed to possess hereditary skills in bone setting. One of them, Waterman Sweet, in 1829 published a text called, An Essay on the Science of Bone Setting. Bone setting continues to be practiced today in large parts of the world by lay practitioners as a form of folk medicine.8
During this time, manual therapy in medicine was relegated to a number of fringe clinicians, foremost among them the 1784 Edinburgh University graduate Edward Harrison. Harrison published in the London Medical and Physical Journal on a proposed pathophysiologic connection between spinal subluxations and visceral disease and adjusted vertebrae by pressing on the spinous or transverse processes with his thumbs or with a device.5,6,9 In 1828, Glasgow physician, Thomas Brown, popularized in the medical community the concept of “spinal irritation”. Brown proposed that a shared nerve supply could implicate the spine in visceral disease and nervous conditions, which led him to target the spine with nonmanipulative heroic medicine interventions including local blistering, application of leeches, and cautery. Dr. Isaac Parrish of Philadelphia introduced the concept of spinal irritation in North America with an article on the topic in The American Journal of Medical Sciences.9,10 Riadore, a prominent London physician practicing manipulation, stated in 1842, “if an organ is insufficiently supplied with nervous energy or blood, its function is decreased and sooner or later its structure becomes endangered.5 With their theories acceptable even to many eminent 19th century medical physicians, it is easy to understand how first osteopathy after 1874 and then chiropractic after 1895 and its offshoots, naturopathy after 1902 and naprapathy after 1905, rapidly gained widespread acceptance among the American general population.
Early Physical Therapy
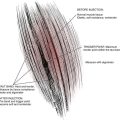
Meanwhile, there was also renewed interest from the medical community in manual therapy. In 1867, the British Medical Journal reported on a lecture by Dr. James Paget, On the Cases that Bonesetters Cure. In 1871, Dr. Wharton Hood wrote a series complementary to bone setting for the Lancet based on his experiences with a bone setter named Hutton, and in 1882 there was a discussion of bone setting at the 50th annual meeting of the British Medical Association.5,7 One reason for this renewed interest might have been the influx and successful establishment of thriving practices by the earliest Swedish-educated physical therapists in various countries, including the United Kingdom. Physical therapy as a government-sanctioned, university-educated profession began when, in 1813, in Stockholm Pehr Hendrik Ling (1776 to 1839) founded the Kungliga Gymnastiska Centralinstitutet or Royal Central Institute for Gymnastics (RCIG) in Stockholm.11 Students at the RCIG were either noblemen or belonged to the upper echelons of society; most were also army officers. They were instructed in physical education, military gymnastics (mainly fencing), and physical therapy or medical gymnastics. The medical gymnastics taught and practiced included a strong manual therapy component, leading Ottoson12 to describe physical therapy as the world’s oldest manual therapy profession (Figs. 48-1 to 48-3). Although, by today’s standards, the manual therapy component instructed in Ling’s system can hardly be called segment specific, clinicians educated at the RCIG certainly further developed and published more specific manipulative interventions.13
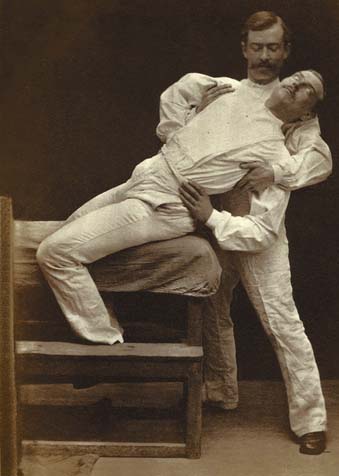
Figure 48-1 Lumbar mobilization ad modem Ling.
(Reproduced with kind permission from Dr. Anders Ottoson, National Archives of Sweden, http://www.chronomedica.se).
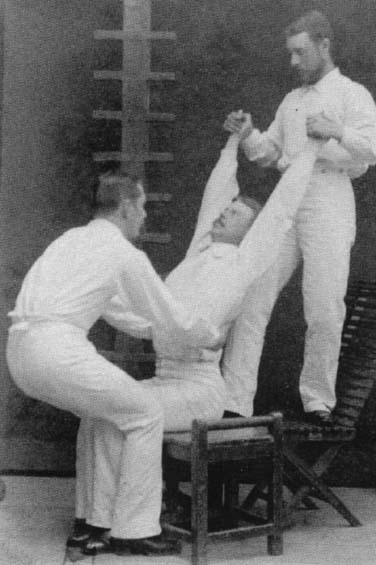
Figure 48-2 Thoracic traction ad modem Ling.
(Reproduced with kind permission from Dr. Anders Ottoson, National Archives of Sweden, http://www.chronomedica.se).

Figure 48-3 Temporomandibular joint mobilization ad modem Ling.
(Reproduced with kind permission from Dr. Anders Ottoson, National Archives of Sweden, http://www.chronomedica.se).
Empowered by their scientific training and propelled by an unwavering conviction that physical therapy could positively affect many conditions including (and thereby not unlike osteopathy and chiropractic) a multitude of nonmusculoskeletal pathologies, RCIG graduates traveled around the globe to disseminate their approach to patient management based on what they considered current best evidence. As early as the 1830s they started establishing clinics in many European cities. A great number of foreign doctors and laymen traveled to Stockholm to study physical therapy with Ling’s successor Lars Gabriel Branding (1799 to 1881). Meanwhile in Sweden, an 80-year turf war erupted between these early physical therapists and the fledgling orthopedic medicine specialization, from which the orthopedic physicians at the Karolinska Institute eventually emerged victorious.11,14 Physical therapy education in Sweden and eventually worldwide was restructured to a technical education producing allied health technicians. In English-language countries, physical therapy was often practiced by nurses with additional course work in massage and exercise therapy. In other Western European countries, physical education teachers with additional course work in rehabilitative exercise, often begrudgingly gave up their previous professional independence for support from the medical profession in their search for societal recognition.15
In rapid succession, national associations arose from these physical therapy technicians. In 1889 in the Netherlands, physical therapists founded the world’s first professional association, the Society for Practising Heilgymnastics in the Netherlands. In 1894, in Great Britain, the Society of Trained Masseuses was founded and in 1906 in Australia, the Australasian Massage Association.15,16 Physical therapy in the United States had a relatively late start with the founding of the American Women’s Physical Therapeutic Association in 1921. When the United States entered World War I, it did not, in contrast to its European allies, have a military with an established division of physical therapy. By command of the Surgeon General, a number of university physical education programs, instituted physiotherapy “War Emergency Courses” to train women who could physically rehabilitate returning soldiers. As a result, 90% of World War I physical therapists came from schools of physical education; in fact, the physician then in charge of the Army Physiotherapy Division stipulated that all therapists have 4-year university degrees in physical education in addition to their physical therapy training. When in 1922 the military reduced therapy services as a result of government cutbacks, many therapists previously employed by the military were forced into the private sector. This led to conflicts with other manual medicine practitioners including nurses, osteopaths, and chiropractors all claiming to practice physical therapy. It was this early conflict especially with the chiropractic profession that caused therapists to align themselves more closely with medical physicians. To garner physician support, U.S. physical therapists in 1930 voluntary relinquished their right to see patients without physician referral.17
In the United States, this close alliance with the medical profession and the adversarial relationship between physicians, and especially chiropractors, also had physical therapists in their communication with physicians deemphasize the use of manual therapy in their clinical practice—although these interventions continued to be used and further developed within the profession with various publications during this period in the U.S. professional physical therapy literature.18 In Western Europe and Scandinavia, this adversarial stance never developed. Instead, medical physicians embraced osteopathy, chiropractic, and other manual medicine approaches indigenous to Europe. Throughout Europe, postgraduate manual medicine training institutes were well attended by physicians and even academic chairs in manual medicine were established.19
These European physicians also educated their physical therapy technicians in manual therapy. Dr. James Mennell (1880 to 1957), the medical officer at St. Thomas Hospital in London, taught manipulation to physical therapists as of 1916. His son, Dr. John McMillan Mennell (1916 to 1992) educated physicians and physical therapists worldwide in manipulation and, with Dr. Janet Travell, cofounded the North American Academy of Manipulative Medicine. Dr. James Henry Cyriax (1904 to 1985), Mennell’s successor at St. Thomas, stated that physical therapists were the most apt professionals to learn manipulative techniques. Mennell is most known for developing and instructing therapists and physicians worldwide. His system of orthopedic medicine emphasized clinical diagnosis and conservative management by way of mainly friction massage, exercise, manipulation, and infiltration. Less well known is his link to early Swedish physical therapy, although his father (Dr. Edgar Cyriax 1874 to 1955), and his maternal grandfather (Jonas Henrik Kellgren 1837 to 1916), were both RCIG graduates. Another influential person teaching manipulation to therapists at this time at the London School of Osteopathy was Dr. Allan Stoddard, qualified in medicine and osteopathy. Therapists and physicians were also educated in manual therapy at the British School of Osteopathy as of 1920.7
Manual Therapy Approaches
Kaltenborn-Evjenth Approach
Without a doubt the most important person to again increase the emphasis on manual therapy within the profession of physical therapy was Norwegian-born Freddy Kaltenborn (1928-). Already trained as a physical education teacher he was admitted as the first male student to the Norwegian program in physical therapy in 1948. Educated in London in orthopedic medicine by Dr. James Cyriax from 1952 to 1954 and qualifying in chiropractic in Germany in 1958 and in osteopathy at the London School of Osteopathy with Dr. Stoddard in 1962, Kaltenborn -from 1968 on associated with physical therapist Olav Evjenth—developed an eclectic manual therapy system known as the Kaltenborn-Evjenth approach.14 With Kaltenborn the first clinician to apply the new science of arthrokinematics to manual therapy,7 central to the Kaltenborn-Evjenth approach is the emphasis on restoration of the gliding component of a normal joint roll-gliding movement. Also central is the concept of a treatment plane defined as the plane across the concave joint surface. With manual translatoric techniques defined in this system as encompassing traction, compression, and gliding techniques, traction and compression are performed perpendicular to this treatment plane, whereas gliding techniques induce movement parallel to this plane. Mobilization and manipulation techniques are used to reduce pain and increase ROM. Joint restrictions are classified as periarticular, articular, intraarticular, or combined in etiology. Periarticular restrictions owing to adaptive shortening of neuromuscular and inert structures (including skin, retinacula, and scar tissue) and articular structures (capsule and ligaments) are treated with sustained mobilization techniques, whereas periarticular restriction due to arthrogenic muscle hypertonicity is managed with neurophysiologic inhibitory techniques including thrust techniques.20 Intraarticular restrictions are best treated with (traction) manipulation initiated from the actual resting position.21
Maitland (Australian) Approach
In Australia, physical therapist Geoff Maitland (1924-) after studying abroad with Cyriax and Stoddard and physical therapists Gregory Grieve and Jennifer Hickling developed his own approach and started teaching a manual therapy system at the University of Adelaide in the entry-level physical therapy program. The world’s first 3-month certificate program was offered in 1965. In 1974, 12-month postgraduate diploma courses in manipulative therapy were offered at physical therapy programs in Australia. This approach to manual therapy is now referred to as the Maitland or Australian approach.22 Although it is often associated with variations of the nonthrust posteroanterior pressure technique (Fig. 48-4), the Maitland system uses a whole spectrum of thrust and nonthrust techniques. Perhaps its greatest contribution is its emphasis on structured clinical reasoning. History-taking is used to gather information that is used in the subsequent physical examination to establish the patient’s concordant or comparable signs. A concordant sign consists of pain or other symptoms reproduced on physical examination that are indicated by the patient as a chief complaint or reason to seek therapy.23 A thorough history-taking allows the clinician to distinguish between concordant and discordant signs. Discordant signs are findings on physical examination seemingly implicating a source of symptoms that are, however, in no way related to the chief complaint.24 Unique to the Maitland approach are also the frequent immediate postintervention reevaluations of the deemed most relevant concordant or so-called asterisk signs to guide further management.
Paris Approach
In 1960, physical therapist Stanley Paris from New Zealand received a scholarship from the New Zealand Workers Compensation Board to study with Freddy Kaltenborn and Allan Stoddard. On his return to New Zealand, he organized courses and introduced, among others, later influential physical therapists Robin McKenzie and Brian Mulligan to manual therapy before leaving to teach and practice in the United States. Paris became the voice of manual therapy as a specialization within orthopedic physical therapy within the United States and worldwide. Denied access—for being a physical therapist and not a physician—to the North American Academy of Manipulative Medicine by Dr. Janet Travell, he founded the North American Academy of Manipulative Therapy in 1968, which was disbanded in 1974 to become the Manual Therapy Special Interest Group in Canada and the Orthopedic Section of the APTA in the United States. Together with, among others, physical therapists Grieve, Kaltenborn, Lamb, and Maitland, Paris also founded in Montreal in 1974, the International Federation of Orthopaedic Manipulative Therapists (IFOMT), the first recognized subgroup of the World Confederation of Physical Therapy. At the urging of Kaltenborn, Paris was again involved in 1991 in organizing the American Academy of Orthopedic Manual Therapy.5,7,14 Most relevant to U.S. physicians referring for manual therapy is that fellows in this organization (designated FAAOMPT) have demonstrated advanced proficiency in manual therapy skills and knowledge. Paris also developed an eclectic system of manual therapy. In addition to a unique diagnostic classification system, and central to this system, is the emphasis not on addressing pain but on treating dysfunction defined as a state of altered mechanics, either an increase or decrease from the expected normal, or the presence of an aberrant motion.25
Mechanical Diagnosis and Therapy: McKenzie Approach
Although emphasizing patient independence by way of specific exercise self-treatment, physical therapist Robin McKenzie of New Zealand has developed a strongly research-based approach to management of spinal and extremity conditions called the McKenzie or Mechanical Diagnosis and Therapy (MDT) approach that incorporates examination and treatment by way of sustained and repeated movements and, if required, mostly nonthrust manual therapy interventions. Classification into postural, dysfunction, or derangement syndromes is guided by patient report of pain during repeated movement examination occurring within range or at end range and by the possible occurrence of centralization and peripheralization. Unique to the MDT concept and indicative of the derangement syndrome—strongly associated in the spine with discogenic dysfunction—centralization is defined as “the situation in which pain arising from the spine and felt laterally from the midline or distally is reduced and transferred to a more central or near midline position when certain movements are performed”. Peripheralization describes the opposite condition, whereby movements cause pain to be felt more distally or laterally from the midline.26
Mulligan Approach
New Zealand physical therapist Brian Mulligan suggested minor positional faults as an etiology for joint dysfunction thought to respond to a unique manual therapy intervention called mobilizations with movement (MWM).27 With an MWM, the therapist applies a sustained accessory glide, long-axis rotation, or combination while the patient actively performs a previously, but now no longer painful, movement (Fig. 48-5). The Mulligan approach shares with the Kaltenborn approach an emphasis on restoration of the gliding component of the normal joint roll-gliding movement.28 Central to both is also the concept of the treatment plane but, whereas Kaltenborn emphasizes gliding techniques in the direction normally associated with the restricted physiologic motion, Mulligan often starts with a sustained glide at a right angle to this physiologic glide. An iterative process then tests glides in different directions or long-axis rotation before settling on the most effective direction allowing for pain-free active ROM or isometric muscle contraction, together constituting the MWM.28,29 Although Mulligan’s NAGs or natural apophyseal glides, mid to end-range facet joint mobilizations applied anterosuperiorly along the treatment plane, are perhaps less unique, the SNAGs or sustained natural apophyseal glides that combine active movement with therapist-applied mobilization certainly are. The techniques are supported by a home program of self-mobilization and corrective taping.27
Neural Mobilization
Based to a large extent on pioneering work by Breig,30 Australian physical therapists Robert Elvey, David Butler, and Michael Shacklock have contributed greatly to our understanding of the possible role of impaired neural mobility in the etiology of neuromusculoskeletal dysfunction.31,32 Also used in diagnosis, interventional neural mobilization techniques attempt to restore normal neural mobility or neurodynamic function in relation to the structures surrounding the nerve by inducing stretch or tension in the affected nerves or by mobilizing the surrounding tissues (Fig. 48-6).2 Butler has more recently expanded on this approach by integrating new insights with regard to pain physiology.33
Other Manual Therapy Systems: Canadian, Grimsby, and Dutch Approaches
Other manual therapy systems relevant mostly to North America include eclectic systems such as the Grimsby, Canadian, and Dutch manual therapy approaches. The Grimsby approach developed by Norwegian physical therapist Ola Grimsby and the Canadian approach initially developed by Canadian and English physical therapists David Lamb, Erl Pettman, Cliff Fowler, Jim Meadows, Ann Hoke, and Diane Lee are derived mainly from the Kaltenborn-Evjenth approach but continue to be developed into progressively more distinct systems of diagnosis and management.34–39 Most characteristic of the Grimsby approach is its emphasis on very specific exercise progressions. The Canadian approach (and its U.S. counterpart instructed at the North American Institute of Orthopaedic Manual Therapy or NAIOMT) emphasizes the use of screening examinations to guide further examination and diagnosis. The Dutch manual therapy system40 combines various manual therapy approaches developed within medicine, physical therapy, chiropractic, and osteopathy and bases diagnosis and management greatly on assumptions with regard to three-dimensional motion behavior of joints and on extrapolations related to somato-somatic and somato-autonomic neuroanatomic connections.
Massage and Soft-Tissue Mobilization
Although often erroneously associated with Pehr Hendrik Ling, Swedish massage was again popularized in the late 19th century as a viable medical treatment by Dr. Johan Georg Mezger (1838 to 1909), a Dutch physical education teacher turned physician.15 Also called traditional or —when applied to athletes—sports massage,41 most therapists do not consider Swedish massage a systematic manual therapy approach but rather a preparatory modality consisting of effleurage or rhythmic stroking hand movements, petrissage or kneading, tapotement or manual percussive massage, friction or deep penetrating pressure delivered through the finger tips, and vibration or shaking.4
James Cyriax promoted deep friction massage transverse to the fiber direction for the treatment of ligament and tendon injuries3 and from this various instrumented-assisted versions have developed including most prominently Graston technique and ASTYM (assisted soft tissue mobilization). The ASTYM method was developed by sports physician Dr. Tom Sevier, who not only has taken great care to investigate and support the method with basic and applied research evidence but who has also created a national outcome database to help therapists establish a research-based prognosis. Unlike Graston technique, initially marketed by Dr. Sevier’s former instrument maker, Mr. Dave Graston, ASTYM is not simply an instrument-assisted locally applied cross friction technique but is used to treat the whole kinetic chain involved with established protocols that are adapted by the clinician based on patient presentation (Fig. 48-7).

Figure 48-7 Assisted soft tissue mobilization (ASTYM) treatment for lateral epicondylalgia.
(Reproduced with kind permission from Dr. Tom Sevier, www.astym.com).
As do bodywork therapists, physical therapists also use soft-tissue mobilization, which includes techniques intended to affect muscles and connective tissues such as stretching, myofascial release, trigger point techniques, and deep tissue techniques.2 Myofascial release and deep tissue techniques are discussed in more detail in the chapter on bodywork and movement therapies. Active release technique (ART) is a form of deep tissue technique developed by the chiropractor P. Michael Leahy. In ART, protocols based on symptom patterns are linked to manual treatment of specific anatomic sites. Specific techniques are then used for release of proposed soft tissue adhesions that consist of applying deep digital tension, usually with the thumb or two fingers combined with both active and passive passage of the tissue through this area of deep tension. An active home stretching program follows this manual treatment.42
Stretching techniques performed by therapists in the context of manual therapy intervention can take the form of static or facilitated stretching. In the 1950s, physical therapists Margaret Knott & Dorothy Voss43 developed proprioceptive neuromuscular facilitation (PNF) that by way of a combination of isometric contractions and mid through end range movements in three-dimensional naturally occurring spiral and diagonal patterns used reflexogenic activation and relaxation for specific stretching, strengthening, and stabilization. Postisometric relaxation is a European manual medicine technique similar to a PNF hold-relax-stretch technique in that the patient is asked to gently contract a muscle from a slightly lengthened position followed by a further gentle stretch on relaxation.44
Manual trigger point therapy is an intervention often used in physical therapy. In the late 1930s, Dr. Janet Travell, at that time a cardiologist and medical researcher, became interested in muscle pain. In the early 1960s, physiatrist Dr. David Simons and his wife, physical therapist Lois Simons, started collaborating with Travell, which eventually resulted in the Trigger Point Manuals, consisting of two volumes on the upper and the lower half of the body.45,46 Although initially, in addition to spray-and-stretch techniques, heavy ischemic pressure was advocated as a manual technique for treatment of myofascial trigger points, the updated second edition of the first volume instead suggested the use of gentle digital pressure or trigger point pressure release.47
Physical therapists sometimes use other systems of massage and soft tissue mobilization that propose effects beyond those solely on the neuromusculoskeletal system. Those include, but are not limited to, Japanese Shiatsu acupressure massage, connective tissue massage, and Rolfing.48,49 Acupressure massage uses a rationale for management choices that is consistent with that used for acupuncture in traditional Chinese medicine. Connective tissue massage was developed by German physical therapists Elisabeth Dicke and Hede Teirich-Leube and physician W. Kohlrausch. In 1929, Dicke had serious endarteritis obliterans and amputation of her leg was considered. Noticing an increased tension in the skin and subcutaneous tissue of her lumbosacral region, she attempted to reduce the discomfort there by applying a stroking massage. She not only noted a sharp local sensation, but also itching and a feeling of warmth spreading into her affected leg. Continued self-treatment resulted in improvement of her ischemic complaints. Connective tissue massage is a reflex therapy that uses a manually applied shear force at connective tissue interfaces in the skin. This has been proposed to stimulate autonomic nerve endings, thereby restoring balance between the sympathetic and parasympathetic components of the autonomic nervous system. By way of cutaneovisceral responses evoked in segmentally related skin areas, this form of massage has also been hypothesized to affect internal organ function.49–51 Manual lymphatic drainage is a light-touch massage technique combined with patient education and compressive garments developed in the 1930s in France by the Danish psychologist Dr. Emil Vodder. It is primarily intended to have an effect on soft tissue edema.52
Mechanical Effects
Although it is not possible to separate mechanical and neurophysiologic effects in clinical research, disruption of articular and/or periarticular adhesions, release of entrapped synovial folds or plicae, reduction of displaced nuclear fragments, and unbuckling of motion segments have all been suggested as mechanical effects of thrust techniques.53 Peak force magnitudes used during spinal thrust techniques easily exceed body weight and are attained within 100 to 200 msec.54 Increased strain rates with thrust techniques lead to increased stiffness in collagenous tissues, possibly resulting in failure or disruption of adhesions with decreased joint excursion when compared to low-velocity techniques. Alternatively, mobility restrictions owing to collagenous shortening, fibrosis, or hyperplasia would likely benefit more from the viscoelastic deformation produced by sustained or oscillatory nonthrust articular and soft tissue techniques.53
The synovial fluid is composed of 15% suspended gases, 80% of which is carbon dioxide and the rest mainly oxygen and nitrogen. Thrust techniques cause a rapid distraction of the joint cavity resulting in a similarly rapid drop by some 3.5 atmosphere in intraarticular pressure. Although the joint will unsuccessfully try to adapt with invagination of capsular tissue into the joint cavity, the sudden local reduction of pressure will cause a process called cavitation whereby the previously suspended gases are released from solution and form a gas bubble within the joint. The cavitation process itself or the subsequent collapse of this gas bubble is what causes the audible release that often accompanies thrust techniques.55 Manipulation of a joint is followed by a refractory period of some 15 to 30 minutes during which the gas is again reabsorbed into the synovial fluid and no new cavitation can be produced.56 The joint distention due to the presence of nonsuspended gases in the synovial fluid during this period has been hypothesized to result in viscoelastic deformation of restricted capsuloligamentous structures.57
Although the traction component of thrust techniques seems a plausible mechanism for unbuckling or restoring appropriate alignment of displaced joint partners, research has not supported this proposed mechanism.53 Similarly, research so far has also failed to support the minor positional fault mechanism postulated by Mulligan.29 Evans53 suggested that release of entrapped synovial folds or inclusions is also unlikely and proposed neurophysiologic effects on persistent associated muscle spasm after such a mechanical event had occurred and spontaneously resolved.
Cyriax58 suggested that manipulation might restore displaced nuclear fragments to a more central location within the intervertebral disc (IVD). However, although various case reports have described positive effects of thrust techniques on carefully selected patients with IVD lesions,59 others have suggested that positive outcomes may be more related to natural history than to a mechanical effect of the manipulation. In fact, manipulation of a segment with a disc affected by trauma or degeneration, especially a noncontained herniation where the outer annulus is compromised, might lead to further injury, extrusion, and progressive neurologic compromise.60 In contrast to the equivocal mechanical effects of thrust techniques of the IVD and as initially proposed by McKenzie26 as a mechanical explanation for the effect of repeated movements, research on asymptomatic human subjects does show movement of the nucleus of the lumbar IVD anteriorly with extension and posteriorly with flexion in nondegenerated discs.60 Although research on symptomatic subjects is limited, Donelson and coworkers61 have shown the ability to differentiate with repeated movement testing between patients with a competent and noncompetent outer annulus suggesting similar mechanical effects in degenerated discs.
Friction massage has been hypothesized to stimulate tissue healing by way of local mechanical effects. Research has indeed shown cellular responses in the sense of increased fibroblast recruitment and activation and mechanical responses indicative of accelerated tissue healing with instrument-assisted deep friction massage.62–64 Swedish or sports massage has been hypothesized—although it is unclear whether this effect is mediated mechanically or neurophysiologically—to affect muscle tissue healing and recovery. However, a review on this topic showed limited and conflicting evidence for effects of massage on muscle blood flow and indicated that an effect of massage on lactate clearance was unlikely. Massage did result in significant decreases in delayed-onset muscle soreness (DOMS) but again, the evidence for an increased rate of post-DOMS force recovery—possibly indicative of accelerated muscle repair processes due to massage—was limited. There was also insufficient evidence for the effects of massage on recovery from muscle fatigue, although a trend was noted for endurance more so than strength performance.41
Neurophysiologic Effects
To this day, in some approaches to manual therapy, mechanical explanations for the mechanism of action of manual therapy interventions are considered more relevant than neurophysiologic explanations. However, the firmly held convictions that clinicians are able to apply segment-specific interventions and that such specific interventions are always required for optimal patient outcome, have not been supported by the available research. Segmental specificity is a biomechanical impossibility when applying the central posteroanterior pressures associated with the Maitland system. In the lumbar spine, for example, posteroanterior pressures resulted in motion of the entire lumbar region,65,66 whereas in the cervical spine, the same technique produced minimal, if any, intervertebral motion when applied at C2 or C6.67 Beffa and Mathews68 noted an equal distribution of cavitation induced from the sacroiliac to the L3-4 joints with thrust techniques aimed at either the sacroiliac or the L5-S1 joints. Ross and associates69 noted that manipulation of the lumbar and thoracic spine produced cavitation at the targeted joint only about 50% of the time; however, most procedures resulted in multiple cavitations, thereby including the target segment. Reggars70 showed that a thrust technique directed at C3-4 resulted in multiple-level cavitations in 82% of subjects, showing the lack of segmental specificity also for this cervical technique.
With regard to the need for specificity of the manual therapy technique for optimal results, Chiradejnant and colleagues71 noted no between-group differences on any of the outcome measures used in a group of patients with low back pain (LBP), who were treated with either unilateral or central posteroanterior or transverse pressures that had been selected by the therapist based on examination findings or randomly generated. In a case series, Cleland and colleagues72 noted favorable outcomes in patients who fit a prediction rule for sacroiliac joint manipulation in LBP, even though they were treated with a rotational technique aimed at the lumbar spine. Van Schalkwyk and Parkin-Smith73 found no between-group postintervention differences in patients with mechanical neck pain and segmental restriction when using either a rotational or lateral break manipulation technique. In their systematic review of randomized controlled trials investigating manual therapy for patients with nonspecific LBP, Kent and associates74 noted that studies in which the clinician was not given the choice of treatment technique actually had better short-term outcomes with regard to pain and activity limitation than those studies in which the clinicians were given a treatment choice; long-term outcomes were equal in both types of studies. Haas and colleagues75 showed that there were no short-term between-group differences in pain and stiffness ratings when patients with neck pain were manipulated at a segment with decreased segmental mobility or at a randomly generated segment. Although this research evidence in no way disproves the notion that for some patients specific manual therapy interventions will, in fact, provide better outcomes, it does indicate the need for all clinicians to more seriously consider possible neurophysiologic mechanisms of action for manual therapy interventions.
Input for neurophysiologic effects of manual therapy likely occurs by stimulation of cutaneous, musculotendinous, and capsuloligamentous receptors. Stimulation of thick fiber afferent neurons might explain analgesia by way of activation of the gate control mechanism postulated by Melzack and Wall.76 The persistent postcavitation distention of the joint capsule has been hypothesized to cause depolarization of the thick fiber afferent type III articular mechanoreceptors with resultant inhibitory effects on periarticular muscles.57 Massage has been shown to reduce motor neuron excitability as measured by a decreased H-reflex in both neurologically normal subjects and in subjects with spinal cord injury.77–79 Although Herzog54 suggested this was due to an artifact related to positional changes, manipulation research has produced similar decreases in motor neuron excitability in healthy subjects that were even more pronounced in subjects with chronic pain.2 Of course, we cannot exclude supraspinal influences as causing or contributing to this decreased motor neuron excitability but, considering the seemingly increased motor neuron excitability related to those higher-level systems discussed subsequently, this reduction in excitability would seem caused by segmental mechanisms.
Because of the synaptic connections between low-threshold joint and muscle mechanoreceptors, the dorsal periaqueductal gray (PAG) area of the midbrain may also have a role in manipulation-induced analgesia by way of descending inhibitory mechanisms. This PAG plays an important integrative role with regard to the response to stress, pain, and other stimuli by coordination of the nociceptive, autonomic, and motor systems. Its hypothesized role has been supported by manipulation studies showing sympathoexcitation and central postmanipulation motor facilitation—the latter also evidenced by muscle activation remote from the area of manipulation occurring some 50 to 200 msecs after manipulation.54,80,81 The ventrolateral PAG exerts its descending inhibitory influence by way of an opioid mechanism but research has been equivocal when it has come to detecting elevated plasma beta-endorphin levels after manipulation or massage. Similarly, intravenously administered opioid antagonists have not been shown to reverse the hypoalgesic effect of at least nonthrust manual therapy interventions.82 Although one can question relevance of plasma samples to extrapolate regarding the central role of endorphins in manipulation-induced analgesia with endorphins too large to penetrate the blood-brain barrier, recently the endocannabinoid system has been suggested as relevant to the analgesic but also mood-enhancing effects of manual therapy interventions.83,84
Animal research has also indicated a role for the neuropeptide oxytocin in the plasma and in the PAG in the analgesia produced by massage. Blockade of the oxytocin receptors either in the PAG or systemically was shown to reduce the analgesic effects of massage. Massage in human subjects has been shown to decrease cortisol and increase serotonin levels.2 Animal research also has implicated central mechanisms working by way of serotonin and norepinephrine in the analgesia produced by nonthrust joint mobilization but no role for gamma-aminobutyric acid (GABA) or endogenous opioids.85
Psychological Effects
Massage has also been shown to have significant positive effects on mood states including depression and anxiety in various patient populations.86–90 Whether this is a psychological effect or whether it is mediated by endogenous opioid or endocannabinoid, actions related to descending inhibitory systems is unclear. For thrust techniques, the occurrence of an audible release due to cavitation has been suggested as relevant to the patient experiencing a psychological therapeutic effect.57 Preliminary evidence, however, suggests that occurrence or nonoccurrence of this phenomenon has no effect on the short-term outcome with regard to pain, function, or ROM in patients with mechanical LBP91 or neck pain92 and on 4-week outcomes in patients with LBP.93
Examination and Diagnosis
Manual Therapy Examination
Even though research has generally not shown these tests to be reliable or valid,94 positional palpation tests to establish the presence of possible malposition related to joint dysfunction are still advocated and used within some manual therapy approaches. Palpation for changes in tissue texture thought to be indicative of segmental dysfunction have shown some interrater reliability but abnormalities are found in symptomatic and asymptomatic subjects indicating likely limited diagnostic value.
Joint play tests assess for ROM, symptom reproduction, resistance through range and at end range (the latter also known as end feel), and overall impression during passive accessory motion testing of the extremity joints. Various types of motion palpation tests (Table 48-1) assess for similar qualities in the spine and sacroiliac joints (Figs. 48-8 and 48-9). Intrarater agreement for isolated spinal motion palpation tests varies from less than chance to generally moderate or substantial agreement, whereas interrater agreement only rarely exceeds poor to fair agreement. Rating scales for mobility are less reliable than rating for pain. Given the neurophysiologic mechanisms of action described for manual therapy and the lack of a need, in at least some patients, for segmental specificity of the manual therapy intervention, knowing there is a joint dysfunction may be more relevant than knowing the exact location and direction of the dysfunction. Thus, even less reliable tests might provide appropriate guidance for manual therapy management.95 In contrast to data on isolated tests, pragmatic combinations of various motion palpation tests left to clinician discretion have shown high predictive validity for pain relief with zygapophyseal infiltrations in the cervical and lumbar spine.96,97
| Type of Palpation | Description |
|---|---|
| Active motion palpation | Assessment technique in which the clinician palpates bony landmarks while guiding the patient through cardinal plane motions of the trunk |
| Passive motion palpation | Assessment technique whereby one vertebra is moved in physiologic ranges on another (PPIVM) |
| Assessment technique whereby segmental mobility is assessed through the translatory motions associated with physiologic motions (PAIVM) | |
| PAIVM tests that specifically test for accessory motions that should not or minimally be present in a normal motion segment (PAIVM) |
PAIVM, passive accessory intervertebral motion palpation; PPIVM, passive physiological intervertebral motion palpation.

Figure 48-9 Passive physiologic intervertebral motion (PPIVM) test for segmental unilateral cervical extension.
Provocation tests have more consistently demonstrated sufficient reliability and diagnostic accuracy.94 Laslett and coworkers23 studied concurrent criterion-related validity of a comprehensive examination consisting of an MDT repeated movement evaluation combined with a cluster of SIJ provocation tests including the distraction, compression, thigh thrust, pelvic torsion, and sacral thrust tests. The rating scale for the individual tests was dichotomous; the subjects were diagnosed with SIJD when three or more tests were positive after exclusion of discogenic complaints with the repeated movement evaluation. The gold standard test was a fluoroscopically guided double SIJ block with at least 80% pain reduction. The authors reported positive LR of 6.97 (95% CI 2.70 to 20.27) and a negative LR of 0.11 (95% CI 0.02 to 0.44). Excluding the discogenic patients yielded a positive LR of 4.16 (95% CI 2.16 to 8.39) and a negative LR of 0.12 (95% CI 0.02 to 0.49).
Acknowledging the relevance of clusters of tests rather than isolated tests in clinical reasoning and patient management, recent research within manual therapy has emphasized the development and validation of clinical prediction rules. Clinical prediction rules (CPR) are decision-making tools that contain predictor variables obtained from patient history, examination, and simple diagnostic tests; they can assist in making a diagnosis, establishing prognosis, or determining appropriate management.98 As Childs and Flynn99 pointed out, if studies included in a systematic review or meta-analysis use no patient classification other than the broad category of nonspecific low back (or neck) pain, the resultant heterogeneous study samples likely preclude finding real effects of any intervention. CPR research is one method to identify a more homogeneous diagnostic subgroup of patients that is expected to respond to manual therapy intervention. Relevant CPRs are discussed under treatment-based diagnostic classification.
Diagnostic Classification in Manual Therapy
Findings from the history and physical examination (and possibly data from imaging and additional medical diagnostic data) are evaluated to establish a manual therapy diagnosis. Diagnosis is classification of patients based on predetermined defining characteristics and as such, diagnosis requires a classification system that, to be useful for manual therapy diagnosis within physical therapy, must meet the following criteria1:
Classification systems are clinimetric indices: rating scales and other expressions are used to measure symptoms, physical signs, and other phenomena in clinical medicine. Clinimetric indices relevant to classification systems used for manual therapy diagnosis include status indices, prognostic indices, clinical guideline indices, and mixed indices.100
Status and Mixed Indices
Status indices are classification systems used to define patient problems. The most common clinically used example is the International Classification of Diseases (ICD), a taxonomy of diagnostic labels for the purpose of standardizing nomenclature of diagnoses for statistical and administrative reasons. Because the ICD-manual does not describe the procedures used to apply the diagnostic labels, reliability of assigning ICD-9 codes is low.100 The traditional medical, structure-based model is also a status index: It assumes a direct correlation between underlying pathology and signs and symptoms and uses a pathoanatomic classification system.101 Indicating its limited value to manual therapy diagnosis, the structure-based medical model is unable to provide up to 85% of patients with LBP with a specific diagnosis owing to the weak association between symptoms, pathologic changes, and results from imaging tests.102,103 Still, manual therapy diagnosis, at times, does use this structure-based or pathoanatomic model. Diagnostic labels include facet joint syndrome, sacroiliac joint syndrome, and disc lesions. The classifications developed by the “Quebec Task Forces on Spinal Disorders and on Whiplash-Associated Disorders” are mixed indices, designed to help make clinical decisions, establish prognosis, and evaluate the quality of care for patients with low back pain or whiplash injuries.100
Prognostic Indices
A prognostic index allows the clinician to predict rehabilitation potential and is intended to aid in making decisions on referral for other services and/or manual therapy management. Research into the predictive validity of (clusters of) signs and symptoms is required to produce prognostic indices. By way of example of prognostic indices relevant to manual therapy management, Jull and Stanton104 identified patients with cervicogenic headache, who did or did not achieve a 50% to 79% or 80% to 100% reduction in headache immediately and 12 months postintervention. Only the absence of lightheadedness indicated higher odds of achieving either a 50% to 79% (OR = 5.45) or 80% to 100% (OR = 5.7) reduction in long-term headache frequency. As noted earlier, Donelson and associates61 established the prognostic validity of the centralization phenomenon with repeated movement examination in the management of patients with discogenic LBP. Hancock and colleagues105 identified three predictor variables for recovery in patients with mechanical LBP receiving spinal manual therapy and diclofenac. Of patients with baseline pain ≤ 7/10, (and) duration of the current episode ≤ 5 days, and number of previous episodes ≤ 1, 60% can be expected to recover (defined as 0 to 1 pain level on 0 to 10 pain scale for 7 days) at 1 week, whereas 95% will recover at 12 weeks.
Clinical Guideline Indices: Mechanism and Treatment-Based Classification
A clinical guideline index is a diagnostic classification system designed specifically to provide instructions on treatment. Most relevant to manual therapy diagnosis are the mechanism- and treatment-based classification systems. The mechanism-based classification system is based on the premise that dysfunctions identified during examination are the cause of pain and decreased function.106 The intent of mechanism-based manual therapy diagnosis is to identify the joint(s) and/or soft tissues implicated, the extent of damage to the tissue, the possible neuroreflexive extension of the local impairment, and the levels of reactivity and ability for a targeted or selective response to intervention within the nervous system.40
In the treatment-based system, a cluster of signs and symptoms from the patient history and physical examination ideally derived from CPR or other relevant research is used to classify patients into subgroups with specific implications for management. In manual therapy, the once predominant mechanism-based system is increasingly supplemented by treatment-based classification systems. The most extensively researched treatment-based classification systems are the MDT approach as proposed by McKenzie and the treatment-based classification system for patients with neck pain and LBP originated at the University of Pittsburgh presented in Tables 48-2 and 48-3.107–110 Vicenzino and colleagues111 have provided preliminary suggestions for a treatment-based classification system for patients with lateral epicondylalgia.
Table 48-2 Treatment-Based Classification for Patients with Neck Pain
| Classification | Examination Findings | Proposed Matched Interventions |
|---|---|---|
| Mobility |
Table 48-3 Treatment-Based Classification for Patients with Low Back Pain
| Classification | Examination Findings | Proposed Matched Interventions |
|---|---|---|
| Specific exercise | ||
| Stabilization | ||
| Manipulation | ||
| Traction |
Clinical Prediction Rules
Various CPRs have been produced related to management within the treatment-based classification system for patients with neck pain and low back pain discussed previously. Flynn and associates112 developed a clinical prediction rule consisting of five predictor criteria to identify a subgroup of patients with nonspecific LBP, who were likely to benefit from thrust manipulation (Fig. 48-10). This rule was subsequently validated by Childs and colleagues,113 who calculated an adjusted OR of 114.7 at the 1-week follow-up and one of 60.8 for a positive functional outcome at the 4-week follow-up for patients who were positive on the rule (≥ 4 predictor criteria present) and received manipulation versus those patients who were negative on the rule and received exercise. Fritz and coworkers114 derived a subsequent 2-factor rule from this prediction rule and reported a positive LR of 7.2 for a positive outcome in patients with LBP who were positive on both predictor variables and treated with manipulation. Fritz and associates115 reported preliminary evidence that there is a subgroup of patients with LBP likely to benefit from traction characterized by leg symptoms, signs of nerve root compression, and peripheralization with extension movements or a positive crossed straight-leg raise test. Hicks and colleagues116 identified four variables relevant to predicting success with stabilization exercises for patients with LBP: age < 40, average straight-leg raise test > 91(o), presence of aberrant motions, and a positive prone instability test (Fig. 48-11). The presence of three or more variables indicated the greatest likelihood of success with a positive LR of 4.0 (95% CI 1.6 to 10.0). Variables associated with failure were negative prone instability test, absence of aberrant motions, absence of hypermobility on lumbar spring testing, and a Fear Avoidance Beliefs Questionnaire Physical Activity (FABQ-PA) subscale score of < 9. Two or more of these variables present carried a negative LR of 0.18 (95% CI 0.08 to 0.38). Similarly, Fritz and colleagues117 identified longer symptom duration, symptoms in the leg or buttock, absence of lumbar hypomobility, less hip rotation ROM, less side-to-side discrepancy in hip internal rotation ROM, and a negative pelvic torsion test as predictors of lack of success with manipulation.

Figure 48-10 Sacroiliac thrust manipulation as used in lumbar manipulation derivation and validation clinical prediction rule studies112,113: lumbar spine is protected by locking into extension-rotation and thrust is delivered to anterior superior iliac spine imparting posterior innominate rotation.
Tseng and associates118 identified six predictor variables for an immediate positive response to cervical manipulation (Fig. 48-12) in patients with neck pain including patients diagnosed with cervical spondylosis with or without radiculopathy, cervical herniated disc, myofascial pain syndrome, and cervicogenic headache. An increasing number of predictor variables present led to progressively higher positive likelihood ratios of an immediate positive response to manipulation: four predictor variables present yielded an LR of 5.33 and an 89% probability of a successful manipulation. Cleland and colleagues119 derived six predictor variables in patients with mechanical neck pain without neurologic involvement, indicating a likely positive response to a combination of three different thoracic thrust manipulations (Fig. 48-13 and 48-14), one simple cervical ROM exercise, and patient education. They suggested using a criterion of three of six variables present as a sufficient research-based indication for the use of thoracic manipulation in patients with mechanical neck pain: three of six variables present yielded a positive LR of 5.5 and an 86% probability of a successful outcome. Raney and coworkers120 developed a five-factor CPR for response to cervical traction and exercise and reported a positive LR of 4.8 (95% CI 2.2 to 11.4) for the patient reporting a great deal of improvement if three or more predictor variables were present. Table 48-4 provides the predictor variables in the various manual therapy-related CPRs.
| CPR to Identify Patients with LBP Most Likely to Benefit from Manipulation |
CPR, clinical prediction rule; FABQPA, Fear Avoidance Beliefs Questionnaire Physical Activity Subscale; FABQW, Fear Avoidance Beliefs Questionnaire Work Subscale; LBP, low back pain; NDI, Neck Disability Index.
CPRs have also been developed although not validated, related to the use of manual therapy in patients with lateral epicondylalgia, patellofemoral syndrome, knee osteoarthritis, chronic tension-type headache, shoulder pain, and ankle inversion sprain.121–126 For a review of relevant clinical prediction rules, the reader is referred to Glynn and Weisbach.127
Indications and Outcomes Research
Indications
The APTA definition of manual therapy1 provided in the introduction to this chapter comprehensively discusses the most common indications for manual therapy interventions within physical therapy. Unlike indications for manual therapy found in, for example, contemporary chiropractic and osteopathy, all of these indications concern neuromusculoskeletal dysfunction. In North America, connective tissue massage is most frequently used for orthopedic problems; however, indications are also suggested for cardiac and respiratory diseases, peripheral circulatory deficits, neurologic pathologies, gynecologic and obstetric problems, and disorders of the digestive system and urinary tract.50,51 Indications suggested for the other less mainstream forms of massage including acupressure massage likewise may extend beyond the neuromusculoskeletal realm. The clinician should keep in mind that all these common indications were developed based mostly on the proposed mechanisms of action for manual therapy interventions discussed earlier. In the era of evidence-informed clinical practice, such extrapolations and assumptions based on scientific evidence need to be supplemented by clinical outcome studies available for the various interventions.
Mechanical Neck Pain
Relevant to the management of patients with mechanical neck pain, in a systematic review Ezzo and associates128 noted that all (quasi) randomized trials included had studied multimodal interventions and that, therefore, the sole effectiveness of massage for patients with mechanical neck pain remained unknown. Systematic reviews on the effectiveness of manual therapy for mechanical neck pain have indicated positive outcomes on pain and function for (non) thrust interventions only when combined with exercise and only in subacute and chronic conditions.129,130 Hoving and colleagues131 reported no significant between-group differences for pain, perceived recovery, and function in patients with neck pain managed by their family physician, exercise and stretching, or nonthrust techniques, and stabilization exercises at 1 year but they noted short-term effectiveness significantly improved for the manual therapy group at 7 weeks. Further indicating the cost-effectiveness of manual therapy management for patients with mechanical neck pain, an economic evaluation alongside this randomized controlled trial (RCT) also showed significantly lower cost for the manual therapy intervention when compared to both other therapies.132 Consistent with the CPR research discussed earlier,119 a meta-analysis showed significant short-term improvements with thoracic thrust manipulation with regard to neck pain, disability, and cervical ROM in specific subgroups.133 A systematic review identified one RCT on the use of the MDT approach for patients with neck pain that showed similar results to exercise therapy.134 Suggesting an indication for manual therapy intervention also in patients with cervical radiculopathy, in a multicenter RCT, Young and colleagues135 studied the effect of true versus sham mechanical traction for cervical radiculopathy. Although they found no between-group differences for pain and function, both groups also received cervical and thoracic nonthrust techniques, thoracic thrust techniques, postural education, and cervical mobility and cervical and scapulothoracic strengthening exercises resulting in both statistically and clinically significant improvements in pain and function.
Cervicogenic Dizziness
A systematic review of randomized and noncontrolled clinical trials found consistent significant improvements with soft tissue, nonthrust, and thrust interventions for patients with cervicogenic dizziness.136 A subsequent RCT in patients with cervicogenic dizziness treated with a Mulligan cervical SNAG intervention showed clinically and statistically significant reduced dizziness, neck pain, and dizziness-related disability over the group treated with detuned laser.137
Headache
A systematic review noted moderate evidence for short-term efficacy of spinal manipulation similar to amitriptyline in patients with migraine and chronic tension-type headache, whereas there was no added benefit if manipulation was added to massage in patients with episodic tension-type headache.138. Bronfort and associates138 also reported moderate evidence that spinal manipulation was more effective for cervicogenic headache than was massage. A systematic review yielded two RCTs that showed significant effects of spinal thrust interventions on headache intensity and duration and medication intake in patients with cervicogenic headache.139 Another systematic review concluded that there was limited evidence for massage and connective tissue mobilization in patients with tension-type headache, whereas the evidence for spinal manipulation, manual traction, and craniosacral therapy was inconclusive.140 An RCT showed that twice weekly 45-minute massage and trigger point release sessions resulted in significant decreases in headache frequency, intensity, and duration and headache-related disability in patients with tension-type headache with these effects lasting into the 3-week follow-up period.141 Fernandez-de-las-Penas and colleagues122 developed a CPR to identify patients with chronic tension-type headache, who might benefit from manual trigger point therapy consisting of varied combinations of pressure release, muscle energy, and soft tissue techniques combined with progressive, low-load deep cervical flexor and extensor muscle strengthening exercises. Relevant improvement was defined as an at least 50% reduction in either headache intensity, frequency, or duration and an increase of ≥ 5 points on a 15-point global rating of change or patient satisfaction scale. Four variables predicted benefit at 1 week after discharge: headache duration < 8.5 hours per day, headache frequency < 5.5 days per week, Short Form-36 bodily pain domain score < 47, and SF36 vitality domain score < 47.5. With three variables present, the positive LR was 3.4 (95% CI 1.4 to 8.0). With all four present, the positive LR increased to 5.9 (95% CI 0.8 to 42.9). Two variables predicted benefit one month postdischarge: headache frequency < 5.5 days per week and SF36 bodily pain domain score < 47. With one variable present, the positive LR was 2.2 (95% CI 1.2 to 3.8); two variables present yielded a positive LR of 4.6 (95% CI 1.2 to 17.9). Although migraine headache might seem to present less of an indication for manual intervention, a prospective cohort study showed significant improvements in headache frequency, intensity, duration, and disability after 2 months of thrust interventions as indicated by the clinician to the whole spine; at 12 months there were still significant improvements when compared to baseline for headache frequency, intensity, and duration and medication use.142 An RCT comparing spinal manipulation to interferential current showed significant between-group differences favoring manipulation for headache frequency, duration, disability, and medication use during the 2-month postintervention follow-up in patients with migraine headache.143
Temporomandibular Dysfunction
A systematic review of RCTs144 reported significant between-group differences favoring manual therapy combined with exercise over occlusal splint therapy with regard to pain and mouth opening range in patients with arthrogenous temporomandibular dysfunction owing to an anteriorly displaced intraarticular disc. A systematic review including randomized and nonrandomized trials145 showed immediate postintervention effects of manual therapy on mouth opening and reduction in periarticular EMG signals; multiple cohort designs with up to 6 months’ follow-up showed significant effects on pain, mouth opening, and perceived recovery with a multimodal program including active exercise, postural correction, relaxation training, hot pack application, and manual therapy. Kalamir and coworkers146 reported that cervical manipulation might be beneficial for patients with temporomandibular disorders, although this recommendation was based solely on case studies.
Thoracic Dysfunction
Aspegren and associates147 noted in a case report that Graston technique and thrust techniques to the thoracic spine and ribs might be of benefit to patients with acute costochondritis. However, and indicating the lack of research effort in this area, a systematic review found no research evidence from RCTs for the effect of thoracic manipulation on thoracic spine conditions.133
Mechanical Low-Back Pain
In their systematic review of randomized trials, Furlan and colleagues148 noted that massage (and most notably acupressure-type massage) was beneficial with regard to pain and function in patients with mechanical LBP for up to 1 year postintervention. Effects improved if massage was combined with exercise and patient education. Hammer and Pfefer,149 reported on the use of Graston technique in a patient with a clinical diagnosis of subacute lumbar compartment syndrome. Older systematic reviews and meta-analyses noted either no evidence that spinal manipulation was superior to other therapies for patients with acute or chronic LBP;150 insufficient evidence for superior outcomes over physical therapy without manipulative interventions, exercise, or medical care in patients with subacute LBP;151 or statistically (but likely not clinically significant) superior outcomes over placebo or nonsteroidal antiinflammatory medication in patients with chronic LBP.152 Insufficiently homogeneous study samples likely have impaired our ability to detect a true effect of manipulation and more recent CPR research into identifying treatment-based subgroups of patients with mechanical LBP. Further indicating the importance of reliable subclassification, a systematic review of RCTs noted that the MDT approach for patients with LBP resulted in greater short-term reductions in pain and disability when compared to “standard” treatments.134 With regard to manual therapy interventions in patients with lumbar spinal stenosis, Reinman and colleagues153 reviewed randomized, cohort, and case studies and series and reported potential benefit of mainly nonthrust interventions to the lumbar and thoracic spine, pelvis, and lower extremities. With regard to cost-effectiveness, at the 6-month follow-up in the manipulation CPR validation study, patients who had received manipulation had significantly lower health care utilization, medication use, and time off from work due to LBP than those receiving exercise only.113 Similarly, the UK BEAM trial that compared medical management to manipulation or manipulation combined with exercise showed that manipulation or manipulation combined with exercise was the most cost-effective approach to the management of patients with mechanical LBP.154
Shoulder Dysfunction
Massage has been shown to result in significant improvements over wait list controls with regard to pain, function, and ROM in patients with shoulder pain.155 In a case report, Hammer156 described the use of Graston technique in a patient with supraspinatus tendinopathy. A systematic review of RCTs noted limited evidence to support thoracic manipulation for shoulder problems.133 However, cohort studies have shown immediate posttreatment effect of thoracic and rib thrust techniques with regard to pain and shoulder ROM in patients with subacromial impingement157,158 but also medium- and long-term (up to 1 year) benefits of thrust and nonthrust interventions to the cervicothoracic spine, ribs, shoulder, and shoulder girdle over or in addition to exercise, medical care, and steroid infiltration.159,160 Recent systematic reviews including a Cochrane Review161,162 have supported a combination of manual therapy and exercise for patients with impingement for improvements in pain and function. A systematic review of RCTs on patients with painful shoulder conditions noted significant increases in ROM favoring manual therapy including Mulligan MWM techniques, Maitland midrange oscillations, and Kaltenborn glide mobilizations to the glenohumeral joint, a trend for manual therapy in reducing pain, but inconclusive evidence for effects on quality of life or function.163 A case series and an RCT have shown significant effects of nonthrust glenohumeral techniques on ROM and disability maintained for 9 to 12 months in patients with adhesive capsulitis with end-range mobilizations seemingly more effective than midrange techniques.164,165
Elbow Dysfunction
A cohort study with a heterogeneous group of patients with upper extremity overuse syndromes including lateral epicondylalgia of the elbow reported significant changes with regard to pain and function after 4 weeks of ART intervention.42 In a case report, Howitt166 reported on the successful rehabilitation of a patient with chronic lateral epicondylalgia using Graston and ART combined with exercise and modalities. Haller and associates167 reported on the successful use of ASTYM in a patient with chronic lateral epicondylalgia. A Cochrane Review168 noted no consistent benefit of deep friction massage over other physical therapy approaches with regard to pain or grip strength in patients with epicondylalgia but a more recent RCT showed significant between-group differences favoring deep friction massage and Mill’s manipulation of the elbow over diclofenac, phonophoresis, and supervised exercise with regard to (pain-free) grip strength and function at 4 weeks.169 A systematic review noted insufficient evidence for long-term effects of manual therapy but evidence for positive immediate effects of elbow manipulation.170 A more recent RCT comparing MWM techniques to the elbow combined with exercise to corticosteroid infiltration and “wait-and-see” showed that the manual therapy intervention was superior to wait-and-see at 6 weeks and superior to the infiltration after 6 weeks with high recurrence rates in the latter group.171 In an RCT Struijs and colleagues172 compared palmar scaphoid gliding manipulation and passive wrist ROM with a control treatment of friction massage, ultrasound, and strengthening for lateral epicondylalgia and reported a significant between-group difference on a global measure of improvement at 3 weeks and on pain at 6 weeks—both favoring the manipulation group. Earlier we discussed the preliminary development of a treatment-based classification for patients with lateral epicondylalgia.111
Wrist and Hand Dysfunction
Burke and coworkers173 found no significant between-group differences when comparing Graston technique with manual soft tissue techniques in patients with carpal tunnel syndrome (CTS) at 6 weeks but significant within-group effects for both groups on electrodiagnostic findings, wrist strength, and wrist ROM, which were maintained at 3 months. In a case report, Baker and Wilson174 reported on successful management of a patient with chronic bilateral carpal tunnel syndrome using the ASTYM method. In patients with CTS scheduled for surgery, Tal-Akabi and Rushton175 compared neurodynamic mobilization or carpal gliding mobilization and flexor retinaculum stretching to a control group. They reported significant within-group improvements with regard to pain and ROM for both mobilization groups and significant between-group differences favoring both experimental groups over the control group with regard to pain. Six of seven subjects in the control group proceeded with surgery, whereas 11 of 14 in the mobilization groups cancelled surgery. Two systematic reviews176,177 have since recommended carpal bone mobilization for the management of patients with CTS. The efficacy of manual therapy for patients after distal radius fracture with regard to ROM and pain is less clear: A systematic review noted that manual mobilization for Colles fracture was not supported by an RCT but did show positive outcomes in a case series design.178 Nonthrust traction and gliding mobilization of the metacarpophalangeal (MCP) joints after metacarpal fracture has shown significant effects with regard to ROM and joint stiffness over a home exercise program in an RCT.179 Two case reports have described the use of MWM techniques after MCP I dysfunction.29,180 Also in a case report, Howitt and associates181 described the use of Graston and ART in a patient with flexor pollicis longus tenosynovitis.
Hip Dysfunction
In an RCT Hoeksma and colleagues182 showed significant effects on perceived improvement, pain, stiffness, hip function, and ROM persisting at 29 weeks after 5 weeks of muscle stretching, nonthrust hip mobilization, and thrust traction manipulation to the hip joint over specific exercise instruction in patients with osteoarthritis of the hip. Similar results were found in a case series replicating this intervention.183 The outcome of this manual therapy intervention was better in patients with mild or moderate versus severe osteoarthritis.184
Knee Dysfunction
A Cochrane Review168 noted no benefit for friction massage over other physical therapy management for patients with iliotibial band friction syndrome at the knee. Henry and colleagues185 reported on the positive outcomes use of ASTYM in a patient with bilateral total knee arthroplasty. Also in a case report, Henry and associates186 described the successful treatment of a patient postpatellar fracture with ASTYM after 3 months of failed conventional therapy. A cohort study in patients with anterior knee pain showed no immediate postintervention effect of ART on muscle inhibition and strength of the quadriceps muscle.187 In an RCT, Wilson and colleagues188 showed superior outcomes on patient-reported pain and function for treatment of patellar tendinopathy using ASTYM and a home program over a similar home program and stretching, deep friction massage, and modalities at therapist discretion. An RCT showed significant between-group differences with regard to walking distance and various WOMAC scores at 4 weeks in patients with knee osteoarthritis favoring manual therapy techniques to the lumbar and lower extremity joints combined with a home program over subclinical ultrasound. In the experimental group, these improvements over baseline were maintained at 1 year and only 5% of the experimental group versus 20% of the control group proceeded to have knee arthroplasty surgery.189 Also in an RCT, Pollard and coworkers190 reported significant between-group differences for treatment with soft tissue and thrust techniques to the tibiofemoral and patellofemoral joints over sham manipulation with regard to knee pain and self-report of crepitus, mobility, and function at 6 weeks in patients with osteoarthritic knee pain.
Ankle and Foot Dysfunction
In a case report, Hammer156 reported on the use of Graston technique in the management of patients with plantar fasciitis and Achilles tendinosis. Also in a case report, Howitt and associates191 described the use of Graston and ART in a patient with posterior tibial strain. Melham and colleagues192 reported in a case report on the effective use of ASTYM in a patient with a chronic painful fibrotic ankle. A systematic review reported an initial positive effect on dorsiflexion ROM for the use of Mulligan MWM, Kaltenborn glide mobilization, and manipulation of the ankle mortise in patients after ankle sprain.193 In contrast, adding talar glide mobilization to other physical therapy management did not result in significant between-group differences with regard to function or quality of life in an RCT with patients after isolated ankle fracture.194
Systemic Conditions
Holey49 noted that there was no evidence for the use of connective tissue massage in patients with subacute asthma but that it has been shown to reduce menopausal symptoms. Brantberg and colleagues195 reported significant differences in pain and quality of life favoring connective tissue massage over group counseling in patients with fibromyalgia.
Lymphedema
A systematic review noted that there was some evidence to suggest that compressive therapy and manual lymphatic drainage might improve lymphedema related to breast cancer surgery.196 A systematic review including randomized, cohort, pilot, and case studies indicated that manual lymphatic drainage resulted in significant positive effects on pain, edema, and ROM after ankle sprains and on edema in wrist fractures.197
Contraindications and Evidence on Risk of Harm
Contraindications
Even in massage therapy textbooks, contraindications and precautions for massage vary greatly and generally are not based on research evidence.198 However, common sense can serve as a guide. Vigorous massage would seem contraindicated in patients with bleeding disorders, low platelet counts, and those on anticoagulant medication. Massage should not be done in areas where there are skin infections, abscesses, open wounds, fractures, weakened bones, or blood clots (including deep venous thrombosis, severe varicose veins, and thrombophlebitis). Recent surgical scars serve as a precaution. There is no evidence of adverse effects of massage in patients with cancer but direct deep pressure over a tumor would seem unwise and patients should likely consult their oncologist prior to massage treatments.50,199 Although often noted as a contraindication, Bauer and associates200 showed no deleterious effect of massage on heart rate and blood pressure even in patients as early as 48 to 72 hours postmyocardial infraction.
Gibbons & Tehan56 emphasized appropriate patient selection and appropriate technique as perhaps the most important method for preventing—or at least limiting—adverse events with manipulation. They also provided a list of precautions and contraindications to manipulation that also equally apply to nonthrust techniques and other manual therapy interventions (Table 48-5).
Table 48-5 Contraindications and Precautions for Manipulation
| Contraindications | Bone | Any pathology that may lead to significant bone weakening |
Modified from Gibbons and Tehan 2001.
Evidence on Risk of Harm Associated with Massage
Perhaps more relevant to the risk-benefit analysis involved in clinical decision-making than the contraindications and precautions just mentioned is research evidence on risk of harm. In a systematic review, Ernst48 reported adverse events, including a cerebrovascular accident, displacement of a urethral stent, kidney embolization, hepatic and musculoskeletal hematoma, leg ulcers, nerve damage including posterior interosseus syndrome, pseudoaneurysm, pulmonary embolism, thyrotoxicosis in a patient with Hashimoto syndrome, and various pain syndromes. Another systematic review201 added to these myositis ossificans in a patient treated for a thigh contusion, unilateral sensorineural hearing loss after trapezius massage, and perforation of the sigmoid colon. Ernst48 noted that serious adverse events were associated mostly with massage techniques other than Swedish massage and generally involved unlicensed practitioners and only very rarely licensed massage therapists. Based on his systematic review, Grant201 cautioned against treatment in patients using anticoagulant medication or with implanted medical devices and suggested caution with work near superficial nerves and the use of manual lymphatic drainage only over contusions.
Minor Adverse Events Associated with Manipulation
For decision-making with regard to manual therapy interventions, clinicians should again combine the previously mentioned common sense precautions and contraindications with research evidence on risk of harm. Manual therapy frequently results in minor adverse events that are of short duration and the ill effects of which fully resolve. A retrospective survey of Maitland-trained physical therapists reported on 228,050 thrust techniques compared to nonthrust spinal techniques.202 Of all patients treated with manipulation, 29 noted 52 adverse events. Four of these occurred with lumbar and thoracic manipulation and included sciatic pain, an increase in LBP, and—admittedly less minor—two rib fractures. Cervical thrust techniques resulted in 12 patients complaining of postmanipulation dizziness, 11 of nausea, 10 of severe headache, 3 each of nystagmus, blurred vision, vomiting, and brachialgia, and 1 each of brachialgia with neurologic deficit, loss of consciousness, and acute wry neck. Average recovery time was 6.3 days and there were no lasting sequelae. Of patients treated with mobilization techniques, 58 had 129 complications: 39 complained of dizziness, 35 of severe headache, 28 of nausea, 6 of brachialgia with neurologic deficit, 4 of simple brachialgia, 5 of blurred vision, 4 of vomiting, 3 of nystagmus or increased pain lasting more than 2 weeks, and one of immediate postintervention skin clamminess. Somewhat counter to assumptions about comparative safety, one cervical mobilization (not manipulation) session was temporally associated with a cerebrovascular accident (CVA) with limited but prolonged neurologic deficits. Michaeli202 calculated an incidence of one adverse event per 3020 cervical manipulations, whereas he noted only one adverse event per 38,137 lumbothoracic manipulations.
In a prospective study on 283 patients seeing physiotherapists, osteopaths, and chiropractors for manipulative interventions, 60.9% of patients reported at least one postmanipulative reaction. Most common were headache (19.8%), stiffness (19.5%), local discomfort (15.2%), radiating discomfort (12.1%), and fatigue (12.1%). Less common were muscle spasm (5.84%), dizziness (4.28%), and nausea (2.72%). Most of these reactions began within 4 hours and generally disappeared within the next 24 hours. Upper cervical manipulation (OR 3.20, 95% CI 1.89 to 7.77), use of medication (OR 2.20, 95% CI 1.31 to 3.69), female gender (OR 1.66, 95% CI 1.01 to 2.75), and increasing age (OR 1.02, 95% CI 1.00 to 1.05) were found to be independent predictors of headache after spinal manipulation.203
In an RCT studying patients with mechanical neck pain and comparing chiropractic upper thoracic and/or cervical mobilization to manipulation, both with or without modalities, 280 of 336 (83%) subjects responded to a questionnaire sent 2 weeks after treatment. Of these 280, 85 subjects reported 212 adverse reactions: 48 patients treated with manipulation noted 120 symptoms, whereas 37 patients with mobilization noted 92 symptoms. Increased neck pain or stiffness was most common (25%). Headache, tiredness or fatigue, and radiating pain or discomfort were reported by 15.7%, 10%, and 6.1% of subjects, respectively. Less common but still reported by at least 1% of subjects were dizziness or imbalance, extremity weakness, ringing in the ears, depression or anxiety, nausea or vomiting, blurred or impaired vision, and confusion or disorientation. The majority of symptoms started within 24 hours of the manual therapy treatment, disappeared within 24 hours of onset, and did not greatly impair normal activities. Subjects receiving manipulation were more likely than those receiving mobilization to report an adverse reaction (OR 1.44, 95% CI 0.85 to 2.43). Manipulation subjects also were more likely to have symptoms commencing within 24 hours of treatment and with higher severity levels (OR 1.44, 95% CI 0.83 to 2.49). Subjects with moderate to severe headaches were more likely than those with only mild to no headaches to report headache as an adverse treatment reaction (OR 5.18, 95% CI 1.88 to 14.3). Patients with Neck Disability Index scores indicative of moderate to severe neck disability were more likely than those with less neck disability to report dizziness, nausea, blurred or impaired vision, ringing in the ears, extremity weakness, and confusion (OR 3.15, 95% CI 1.01 to 9.80) possibly indicative of more serious neurovascular pathology.204
Minor adverse events after manual therapy seem very common. It should be noted that fatigue, drowsiness, headache, dizziness, nausea, and difficulty concentrating are among the most common nonspecific drug-related adverse effects and that these symptoms are frequently reported even by subjects in the placebo arm of drug trials. In general population studies, up to 75% report these symptoms in preceding 3 days.204 Still, clinicians can use these data to educate patients on the possible occurrence of these short-lived side-effects. With the Michaeli202 survey constituting a lower level of evidence than the Hurwitz and colleagues RCT,204 it would seem that, especially in the cervical spine, thrust techniques produce more adverse reactions than nonthrust techniques, although the nonthrust techniques are certainly implicated in producing minor and also major adverse events. The predictor variables derived from the above studies can help in patient and technique selection. Hurwitz and coworkers204 suggested that clinicians should be cautious about using cervical spine manipulation, especially in those patients with more severe neck-related disability.
Major Adverse Events Associated with Manipulation
Of course, major adverse events characterized by prolonged and only partially reversible or irreversible sequelae can also occur after spinal manipulation. Systematic reviews205–209 have reported clinically worsened disc herniation or cauda equina syndrome with lumbar manipulation and rib fractures with thoracic manipulation. Dissection of the vertebral and carotid arteries, dural tears, nerve injury including phrenic nerve palsy, cervical disc herniation, epidural or flaval ligament hematoma, spinal cord injuries (myelopathy, quadriparesis, central cord syndrome or paraparesis), and fractures involving a spondylotic cervical fusion, a cervical transverse process, the C2, C5, and C6 vertebral bodies, and the odontoid process have all been associated with cervical manipulation.
Van Tulder and associates208 indicated that the risk of serious adverse events with lumbar spine manipulation is limited when the intervention is used by a trained clinician. Earlier we discussed limited evidence for the therapeutic effect of manipulation on disc herniation and we noted disc herniation as a precaution, although not a contraindication to manual therapy interventions. The major adverse event associated with lumbar manipulation is progression of a disc herniation perhaps even leading to progression of neurologic compromise including radiculopathy and cauda equina syndrome. Based on a systematic review of the literature, Oliphant59 calculated a highest risk estimate for developing a disc herniation or cauda equina attributable to treatment of lumbar disc herniation by spinal manipulation as one in 3.72 million manipulations. Despite this low-risk estimate, careful patient selection and consideration of other management options are strongly indicated.
Evidence linking cervical manipulation to cervical (vertebral and internal carotid) artery dysfunction (CAD) and subsequent CVA has included multiple narrative reviews of case reports found in the literature.210–213 Hurwitz and colleagues214 acknowledged the likely high underreporting bias and noted an estimated risk adjusted for an only 10% reporting rate in the literature of 5 to 10 per 10 million for all complications, 6 in 10 million for serious complications, and 3 in 10 million for the risk of death. Haneline and coworkers215 found 13 cases of internal carotid artery dissection temporally associated with cervical manipulation in a 1966 to 2000 Medline review and estimated the chance of developing CAD in this artery postmanipulation at 1 in 601,145,000.
The possible cause-and-effect relationship between cervical manipulation and CAD remains a contentious issue.216 Research into risk of harm is wrought with methodologic shortcomings and not only because of the obvious ethical concerns with studies that would prospectively expose patients to a suspected risk factor.217 In the context of risk of harm, it would seem prudent to consider the epidemiologic Bradford-Hill criteria that state a cause-and-effect relationship becomes likely when the following criteria are all met:213
Although opinions certainly and justifiably differ, case reports and narrative reviews provided by authors in diverse geographic locations temporally linking possible mechanical trauma of the cervical arteries owing to manipulation to CAD would seem to qualify as supporting the first three criteria. Exploring the criterion of a correlation between exposure to manipulation and occurrence of CAD, Rothwell and associates218 compared 582 patients with vertebrobasilar accidents over the period 1993 to 1998 with age and sex-matched controls from the provincial insurance database in Ontario, Canada. They also determined exposure to chiropractic using this same database. These authors found that subjects younger than 45 years were five times more likely (95% CI 1.31 to 43.87) to have visited a chiropractor in the month preceding the stroke. This same age group was also five times (95% CI 1.34 to 18.57) more likely to have had three or more visits with cervical or thoracic spine-related complaints or headache in the month prior to the stroke. No significant association was noted for subjects older than 45 years. However, Cassidy and colleagues219 used a very similar study design comparing 818 patients with vertebrobasilar accidents to age- and sex-matched controls from a provincial insurance database and also found an OR of 3.13 (95% CI 0.52 to 1.32) for having visited a chiropractor in the month before the stroke in those younger than 45 years, whereas the OR was 0.83 (95% CI 0.52 to 1.32) for those older than 45 years. In addition, these researchers looked at visits to general medical practitioners preceding the stroke and found an OR of 3.57 (95% CI 2.17 to 5.86) for those under 45 years and 2.67 (95% CI 2.25 to 3.17) for patients having visited their medical doctor in the month preceding the vertebrobasilar accident. Cassidy and coworkers219 suggested that the similar association between chiropractic and medical visits might indicate that patients with an undiagnosed dissection seek clinical care for headache and neck pain before having a CVA versus lending credence to an exposure-and-occurrence relationship between manipulation and CAD.
With regard to the criterion of other plausible explanations, CAD can occur associated with major trauma but more relevant in this context is spontaneous CAD defined as dissection associated with minor trauma, including but not limited to, sporting activities, whiplash injury, stretches, sudden neck movements, severe coughing, all in addition to cervical manipulation.220 Even without a conclusive answer with regard to a causal relationship between manipulation and CAD, it would certainly seem prudent for clinicians to be vigilant for patients presenting with signs and symptoms of a cervical artery dissection in progress. Table 48-6 provides diagnostic information on nonischemic presentations of internal carotid and vertebral artery dysfunction.221,222
Table 48-6 Nonischemic and Ischemic Signs and Symptoms of Cervical Artery Dysfunction
| Vertebral and Basilar Arteries | Internal Carotid Artery | |
|---|---|---|
| Nonischemic |
Conclusion
Manual therapy has a long history within the profession of physical therapy and physical therapists have greatly contributed to the current diversity in manual therapy approaches and techniques. Although initially mechanical explanations were favored to explain the mechanisms by which manual therapy interventions were thought to work, there is increasing research evidence for intricate neurophysiologic mechanisms and we should also not overlook the beneficial psychological effects of providing hands-on examination and intervention. Manual therapy diagnosis still uses a variety of diagnostic classification models with mechanism and increasingly, treatment-based classification models favored within the physical therapy profession. Research evidence abounds for the effectiveness of manual therapy interventions for a wide variety of neuromusculoskeletal diagnoses and clinical prediction rules and other research intended to establish relevant treatment-based subgroups hold great promise for expanding this evidence base. Even within the domain of physical therapy, risk of harm with manual therapy interventions is certainly present but a common sense approach to patient and technique selection combined with proven adequate orthopedic diagnostic skills223 seems appropriate for minimizing manual therapy-related adverse events and optimizing the risk-benefit ratio with regard to the use of manual therapy interventions.
1. Guide to Physical Therapist Practice. 2nd ed. American Physical Therapy Association. Phys Ther. 2001;81:9.
2. Sluka K.A., Milosavljevic S. Manual therapy. In: Sluka K.A., editor. Mechanisms and Management of Pain for the Physical Therapist. Seattle: IASP Press; 2009:p 205.
3. Cyriax J.H. 8th ed. Textbook of Orthopaedic Medicine, Vol. 1. London: Bailliere Tindall. 1982.
4. Goats G.C. Massage: The scientific basis of an ancient art: Part 1. The techniques. Br J Sports Med. 1994;28:149.
5. Paris S.V. A history of manipulative therapy through the ages and up to the current controversy in the United States. J Manual Manipulative Ther. 2000;8:66.
6. Lomax E. Manipulative therapy: A historical perspective from ancient times to the modern era. In: Goldstein M., editor. The Research Status of Spinal Manipulative Therapy. Bethesda: US Dept. of Health Education and Welfare; 1975:11.
7. Pettman E. A history of manipulative therapy. J Man Manip Ther. 2007;15:165.
8. Oths K.S., Hinojosa S.Z., editors. Healing by Hand: Manual Medicine and Bonesetting in a Global Perspective. Walnut Creek: Calif. Altamira Press, 2004.
9. Terrett A. The search for the subluxation: an investigation of medical literature to 1985. Chiropr Hist. 1987;7:29.
10. Gevitz N. The D.O.’s: Osteopathic Medicine in America. Baltimore: Johns Hopkins University Press; 1982.
11. Ottoson A. Sjukgymnasten-Vart Tog Han Vågendiss. Göteborg: Historiska Institutionen, Göteborgs Universitet; 2005.
12. Ottoson A. When the physiotherapist was a doctor of physiotherapy or why physiotherapists don’t know about their history: Swedish Physiotherapy 1813–1934. Kos: Poster presentation: Conference of the International Society of Medical History; 2008.
13. Kellgren A. Technics of Ling’s System of Manual Treatment. Edinburgh: Young J. Pentland; 1890.
14. Kaltenborn F. Early history of phsysiotherapy in Sweden and Norway: Implications for professional autonomy and direct-access clinical practice. Tijdschrift voor Manuele Therapie. 2008;5(2):6.
15. Terlouw T.J.A. Roots of physical medicine, physical therapy, and mechanotherapy in the Netherlands in the 19th century: A disputed area within the health care domain. J Man Manip Ther. 2007;15:E23.
16. Huijbregts P.A. Chiropractic legal challenges to the physical therapy scope of practice: anybody else taking the ethical high ground? J Man Manip Ther. 2007;15:69.
17. Linker B. Strength and science: Gender, physiotherapy, and medicine in early twentieth-century America. J Women’s Hist. 2005;17:105.
18. Paris S.V. Thirty-Seventh McMillan Lecture: In the best interests of the patient. Phys Ther. 2006;86:1541.
19. Sollmann A.H., Blaurock-Busch E. Manipulative therapy of the spine: the development of ‘manual medicine’ in Germany and Europe. Chiropr Hist. 1981;1:37.
20. Kaltenborn F.M., Evjenth O., Baldauf Kaltenborn T., et al. The Extremities, 6th ed. Manual Mobilization of the Extremity Joints: Joint Examination and Basic Treatment, Vol. I. Oslo: Norli. 2007.
21. Kaltenborn F.M., Baldauf Kaltenborn T., Vollowitz E. Manual Mobilization of the Joints: Joint Examination and Basic Treatment. Traction-Manipulation of the Extremities and Spine, Vol. III. Basic Thrust Techniques. Oslo: Norli. 2008.
22. Bentley P., Dunstan D. Physiotherapy in Australia to the 1980s: The Path to Professionalism. Victoria: Australian Physiotherapy Association; 2006.
23. Laslett M., Young S.B., Aprill C.N., McDonald B. Diagnosing painful sacroiliac joints: A validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother. 2003;49:89.
24. Cook C.E. Orthopaedic Manual Therapy: An Evidence-Based Approach. Upper Saddle River: Pearson Prentice Hall; 2007.
25. Paris S.V. Mobilization of the spine. Phys Ther. 1979;59:988.
26. McKenzie R.A. The Lumbar Spine: Mechanical Diagnosis and Therapy. Waikanae, Spinal Publications. 1981.
27. Mulligan B.R. Manual Therapy: “NAGS”, “SNAGS”, “MWMS”, 5th ed. Wellington, New Zealand: Plane View Services Ltd; 2004.
28. Exelby L. Peripheral mobilisations with movement. Man Ther. 1996;1:118.
29. Hsieh C.Y., Vicenzino B., Yang C.H., et al. Mulligan’s mobilization with movement for the thumb: a single case report using magnetic resonance imaging to evaluate the positional fault hypothesis. Man Ther. 2002;7:44.
30. Shacklock M., editor. Biomechanics of the Nervous System: Breig Revisited. Adelaide, Australia: Neurodynamic Solutions, 2007.
31. Butler D.S. Mobilisation of the Nervous System. Melbourne, Australia: Churchill Livingstone; 1991.
32. Shacklock M. Clinical Neurodynamics: A New System of Musculoskeletal Treatment. Edinburgh: Elsevier; 2005.
33. Butler D.S. The Sensitive Nervous System. Adelaide, New Zealand: NOI Group; 2000.
34. Pettman E. Manipulative Thrust Techniques. Abbotsford, Canada: Aphema Publishing; 2006.
35. Sanzo P., MacHutchon M. Length Tension Testing of the Lower Quadrant. Thunder Bay, Canada: Active Potential; 2007.
36. Sanzo P., MacHutchon M. Length Tension Testing of the Upper Quadrant. Thunder Bay, Canada: Active Potential; 2007.
37. Whitmore S., Gladney K., Driver A. The Upper Quadrant: A Workbook of Manual Therapy Techniques. Guelph, Canada: Whitmore Physiotherapy; 2004.
38. Whitmore S., Gladney K., Driver A. The Lower Quadrant: A Workbook of Manual Therapy Techniques. Guelph, Canada: Whitmore Physiotherapy; 2005.
39. Grimsby O., Rivard J., editors. Applied Science and Theory. Science, Theory and Clinical Application in Orthopaedic Manual Physical Therapy, Vol. 1. Taylorsville, Utah: The Academy of Graduate Physical Therapy. 2008.
40. Van der El A. Orthopaedic Manual Therapy Diagnosis: Spine and Temporomandibular Joints. Sudbury, Mass: Jones & Bartlett Publishers; 2010.
41. Moraska A. Sports massage: A comprehensive review. J Sports Med Phys Fitness. 2005;45:370.
42. Schiottz-Christensen B., Mooney V., Azad S., et al. The role of active release manual therapy for upper extremity overuse syndromes: A preliminary report. J Occup Rehab. 1999;9:201.
43. Voss D.E., Knott M. Proprioceptive Neuromuscular Facilitation. San Francisco: Harper & Row; 1956.
44. Lewit K., Simons D. Myofascial pain: relief by post-isometric relaxation. Arch Phys Med Rehabil. 1984;65:452.
45. Travell J.G., Simons D.G. Myofascial Pain and Dysfunction: The Trigger Point Manual, Vol. 2. Baltimore: Williams & Wilkins. 1992.
46. Travell J.G., Simons D.G. Myofascial Pain and Dysfunction: The Trigger Point Manual, Vol. 1. Baltimore: Williams & Wilkins. 1983.
47. Simons D.G., Travell J.G., Simons L.S. 2nd ed. Travell and Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual, Vol. 1. Baltimore: Williams & Wilkins. 1999.
48. Ernst E. The safety of massage therapy. Rheumatol. 2003;42:1101.
49. Holey E.A. Connective tissue massage: A bridge between complementary and orthodox approaches. J Bodywork Movement Ther. 2000;4:72.
50. Goats G.C., Keir K.A.I. Connective tissue massage. Br J Sports Med. 1991;25:131.
51. Piet J.F.M., Sachs J.J., Sachs-Piet I.M.A. Bindweefselmassage, 3rd ed. Lochem: De Tijdstroom; 1987.
52. Little L., Porche D.J. Manual lymph drainage. J Assoc Nurses AIDS Care. 1998;9:78.
53. Evans D.W. Mechanisms and effects of spinal high-velocity, low-amplitude thrust manipulation: previous theories. J Manipulative Physiol Ther. 2002;25:251.
54. Herzog W. Physiological effects of manual therapy: Two commentaries. “High-speed-low-amplitude” spinal manipulative treatments. Orthop Div Rev. Sept/Oct:29, 2005.
55. Protapapas M.G., Cymet T.C. Joint cracking and popping: understanding noises that accompany articular release. J Am Osteopath Assoc. 2002;102:283.
56. Gibbons P., Tehan P. Spinal manipulation: Indications, risks and benefits. J Bodywork Movement Ther. 2001;5:110.
57. Paris S.V., Loubert P.V. Foundations of Clinical Orthopaedics. St. Augustine, 3rd ed. University Press. 1999.
58. Cyriax J.H. 9th ed. Textbook of Orthopaedic Medicine, Vol. 2. London: Balliere Tindall. 1974.
59. Oliphant D. Safety of spinal manipulation in the treatment of lumbar disk herniations: a systematic review and risk assessment. J Manipulative Phyiol Ther. 2004;27:197.
60. Huijbregts P.A. Fact and fiction of disc reduction: A literature review. J Manual Manipulative Ther. 1998;6:137.
61. Donelson R., Aprill C., Medcalf R., Grant W. A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine. 1997;22:1115.
62. Davidson C.J., Ganion L., Gehlsen G.M., et al. Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc. 1997;29:313.
63. Gehlsen G.M., Ganion L.R., Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999;31:531.
64. Loghmani M.T., Warden S.J. Instrument-assisted cross-fiber massage accelerates knee ligament healing. J Orthop Sports Phys Ther. 2009;39:506.
65. Kulig K., Landel R., Powers C.M. Assessment of lumbar spine kinematics using dynamic MRI: a proposed mechanism of sagittal plane motion induced by manual posterior-to-anterior mobilization. J Orthop Sports Phys Ther. 2004;34:57.
66. Powers C.M., Kulig K., Harrison J., Bergman G. Segmental mobility of the lumbar spine during a posterior to anterior mobilization: assessment using dynamic MRI. Clin Biomech. 2003;18:80.
67. McGregor A.H., Wragg P., Gedroyc W.M. Can interventional MRI provide an insight into the mechanics of a posterior-anterior mobilisation? Clin Biomech. 2001;16:926.
68. Beffa R., Mathews R. Does the adjustment cavitate the targeted joint? An investigation into the location of cavitation sounds. J Manipulative Physiol Ther. 2004;27:e2.
69. Ross J.K., Bereznick D.E., McGill S.M. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific? Spine. 2004;29:1452.
70. Reggars J.W. The manipulative crack. Frequency analysis. Australas Chiropr Osteopathy. 1996;5:39.
71. Chiradejnant A., Maher C.G., Latimer J., Stepkovitch N. Efficacy of “therapist-selected” versus “randomly selected” mobilisation techniques for the treatment of low back pain: a randomized controlled trial. Aust J Physiother. 2003;49:233.
72. Cleland J.A., Fritz J.M., Whitman J.M., et al. The use of a lumbar spine manipulation technique by physical therapists in patients who satisfy a clinical prediction rule: a case series. J Orthop Sports Phys Ther. 2006;36:209.
73. Van Schalkwyk R., Parkin-Smith G.F. A clinical trial investigating the possible effect of the supine cervical rotatory manipulation and the supine lateral break manipulation in the treatment of mechanical neck pain: a pilot study. J Manipulative Physiol Ther. 2000;23:324.
74. Kent P., Marks D., Pearson W., Keating J. Does clinician treatment choice improve the outcomes of manual therapy for non-specific low back pain: A metaanalysis. J Manipulative Physiol Ther. 2005;28:312.
75. Haas M., Groupp E., Panzer D., Partna L., et al. Efficacy of cervical endplay assessment as an indicator for spinal manipulation. Spine. 2003;28:1091.
76. Melzack R., Wall P.D. Pain mechanisms: a new theory. Science. 1965;150:971.
77. Goldberg J., Sullivan S.J., Seaborne D.E. The effect of two intensities of massage on H-reflex amplitude. Phys Ther. 1992;72:449.
78. Goldberg J., Seaborne D.E., Sullivan J.S., Leduc B.E. The affect of therapeutic massage on H-reflex amplitude in persons with spinal cord injury. Phys Ther. 1994;74:728.
79. Sullivan S.J., Williams L.R., Seaborne D.E., Morelli M. Effects of massage on alpha motoneuron excitability. Phys Ther. 1991;71:555.
80. Dishman J.D., Ball K.A., Burke J. Central motor excitability changes after spinal manipulation: a transcranial magnetic stimulation study. J Manipulative Physiol Ther. 2002;25:1.
81. Wright A. Physiological effects of manual therapy: Two commentaries. “High-speed-low-amplitude” spinal manipulative treatments. Orthop Div Rev. Sept/Oct:33, 2005.
82. Paungmali A., O’Leary S., Souvlis T., Vicenzino B. Naloxone fails to antagonize initial hypoalgesic effect of a manual therapy treatment for lateral epicondylalgia. J Manipulative Physiol Ther. 2004;27:180.
83. Dietrich A., McDaniel W.F. Endocannabinoids and exercise. Br J Sports Med. 2004;38:536.
84. McPartland J.M., Giuffrida A., King J., et al. Cannabimimetic effects of osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105:283.
85. Skyba D.A., Radhakrishnan R., Rohlwing J.J., et al. Joint manipulation reduces hyperalgesia by activation of monoamine receptors but not opioid or GABA receptors in the spinal cord. Pain. 2003;136:159.
86. Weinberg R., Jackson A., Kolodny K. The relationship of massage and exercise to mood enhancement. Sports Psychol. 1988;2:202.
87. Field T., Grizzle N., Scafidi F., Schanberg S. Massage and relaxation therapies’ effects on depressed adolescent mothers. Adolescence. 1996;31:903.
88. Field T., Schanberg S., Kuhn C. Bulimic adolescents benefit from massage therapy. Adolescence. 1998;33:555.
89. Hernandez-Reif M., Field T., Krasnegor J., et al. High blood pressure and associated symptoms were reduced by massage therapy. J Bodywork Movement Ther. 2000;4:31.
90. Diego M.A., Field T., Hernandez-Reif M., et al. Aggressive adolescents benefit from massage therapy. Adolescence. 2002;37:597.
91. Flynn T.W., Fritz J.M., Wainner R.S., Whitman J.M. The audible pop is not necessary for succesful spinal high-velocity thrust manipulation in individuals with low back pain. Arch Phys Med Rehabil. 2003;84:1057.
92. Cleland J.A., Flynn T.W., Childs J.D., Eberhart S. The audible pop from thoracic spine thrust manipulation and its relation to short-term outcomes in patients with neck pain. J Man Manip Ther. 2007;15:143.
93. Flynn T.W., Childs J.D., Fritz J.M. The audible pop from high-velocity thrust manipulation and outcome in individuals with low back pain. J Manipulative Physiol Ther. 2006;29:40.
94. Huijbregts P.A. Sacroiliac joint dysfunction: Evidence-based diagnosis. Orthop Div Rev. May/June:18, 2004.
95. Huijbregts P.A. Spinal motion palpation: A review of reliability studies. J Man Manip Ther. 2002;10:24.
96. Jull G., Bogduk N., Marsland A. The accuracy of manual diagnosis for cervical zygapophyseal joint pain syndromes. Med J Aust. 1988;148:233.
97. Phillips J., Twomey L. A comparison of manual diagnosis compared with a diagnosis established by a uni-level lumbar spinal block procedure. Man Ther. 1996;2:82.
98. Laupacis A., Sekar N., Stiell I. Clinical prediction rules. A review and suggested modification of methodological standards. JAMA. 1997;277:488.
99. Childs J.D., Flynn T.W. Spinal manipulation for low back pain. Ann Intern Med. 2004;140:665.
100. Riddle D.L. Classification and low back pain: a review of the literature and critical analysis of selected systems. Phys Ther. 1998;78:708.
101. Fritz J.M. A research-based approach to low back pain. Holland, Michigan; October 12, 1999. Presented at the Distinguished Lectures in Sports Medicine Series
102. Deyo R.A., Rainville J., Kent D.L. What can the history and physical examination tell us about low back pain? JAMA. 1992;268:760.
103. van den Hoogen H.M., Koes B.W., van Eijk J.T., Bouter L.M. On the accuracy of history, physical examination, and erythrocyte sedimentation rate in diagnosing low back pain in general practice. A criteria-based review of the literature. Spine. 1995;20:318.
104. Jull G.A., Stanton W.R. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2005;25:101.
105. Hancock M.J., Maher C.G., Latimer J., et al. Can rate of recovery be predicted in patients with a cute low back pain? Development of a clinical prediction rule. Eur J Pain. 2009;13:51.
106. Van Dillen L.R., Sahrmann S.A., Norton B.J., et al. Reliability of physical examination items used for classification of patients with low back pain. Phys Ther. 1998;78:979.
107. Childs J.D., Fritz J.M., Piva S.R., Whitman J.M. Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther. 2004;34:686.
108. Delitto A., Erhard R.E., Bowling R.W. A treatment-based classification approach to low back syndrome: Identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470.
109. Donelson R. Rapidly Reversible Low Back Pain: An Evidence-Based Pathway to Widespread Recoveries and Savings. Hanover, NH: Self Care First LLC; 2007.
110. Fritz J.M., Brennan G.P., Clifford S.N., et al. An examination of the reliability of a classification algorithm for subgrouping patients with low back pain. Spine. 2006;31:77.
111. Vicenzino B., Cleland J.A., Bisset L. Joint manipulation in the management of lateral epicondylalgia: a clinical commentary. J Man Manip Ther. 2007;15:50.
112. Flynn T., Fritz J., Whitman J., et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27:2835.
113. Childs J.D., Fritz J.M., Flynn T.W., et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141:920.
114. Fritz J.M., Childs J.D., Flynn T.W. Pragmatic application of a clinical prediction rule in primary care to identify patients with low back pain with a good prognosis following a brief spinal manipulation intervention. BMC Fam Pract. 2006;6:29.
115. Fritz J.M., Lindsay W., Matheson J.W., et al. Is there a subgroup of patients with low back pain likely to benefit from mechanical traction? Results of a randomized clinical trial and subgrouping analysis. Spine. 2007;32:E793.
116. Hicks G.E., Fritz J.M., Delitto A., McGill S.M. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86:1753.
117. Fritz J.M., Whitman J.M., Flynn T.W. Factors related to the inability of individuals with low back pain to improve with a spinal manipulation. Phys Ther. 2004;84:173.
118. Tseng Y.L., Wang W.T., Chen W.Y. Predictors for the immediate responders to cervical manipulation in patients with neck pain. Man Ther. 2006;11:306.
119. Cleland J.A., Childs J.D., Fritz J.M., et al. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9.
120. Raney N.H., Petersen E.J., Smith T.A., et al. Development of a clinical prediction rule to identify patients likely to benefit from cervical traction and exercise. Eur Spine J. 2009;18:382.
121. Currier L.L., Froehlich P.J., Carow S.D., et al. Development of a clinical prediction rule to identify patients with knee pain and clinical evidence of knee osteoarthritis who demonstrate a favorable short-term response to hip mobilization. Phys Ther. 2007;87:1106.
122. Fernández-de-las-Peñas C., Cleland J.A., Cuadrado M.L., Pareja J.A. Predictor variables for identifying patients with chronic tension type headache who are likely to achieve short-term success with muscle trigger point therapy. Cephalalgia. 2008;28:264.
123. Iverson C.A., Sutlive T.G., Crowell M.S., et al. Lumbopelvic manipulation for the treatment of patients with patellofemoral pain syndrome: development of a clinical prediction rule. J Orthop Sports Phys Ther. 2008;38:297.
124. Vicenzino B., Smith D., Cleland J., Bisset L. Development of a clinical prediction rule to identify initial responders to mobilisation with movement and exercise for lateral epicondylalgia. Man Ther. 2009;14:550.
125. Mintken P.E., Cleland J.A., Carpenter K.J., et al. Some factors predict successful short-term outcomes in individuals with shoulder pain receiving cervicothoracic manipulation: a single-arm trial. Phys Ther. 2010;90:26.
126. Whitman J.M., Cleland J.A., Mintken P.E., et al. Predicting short-term response to thrust and non-thrust manipulation and exercise in patients post inversion ankle sprain. J Orthop Sports Phys Ther. 2009;39:188.
127. Glynn P.E., Weisbach P.C. Clinical Prediction Rules: A Physical Therapy Reference Manual. Sudbury, Mass: Jones & Bartlett; 2011.
128. Ezzo G., Haraldsson B.G., Gross A.R., et al. Massage for mechanical neck disorders: a systematic review. Spine. 2007;32:353.
129. Gross A.R., Hoving J.L.K., Haines T.A., et al. A Cochrane review of manipulation and mobilization for mechanical neck disorders. Spine. 2004;29:1541.
130. Sarigiovannis P., Hollins B. Effectiveness of manual therapy in the treatment of non-specific neck pain: A review. Phys Ther Rev. 2005;10:35.
131. Hoving J.L., de Vet H.C., Koes B.W., et al. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: long-term results from a pragmatic randomized controlled clinical trial. Clin J Pain. 2006;22:370.
132. Korthals-de Bos I.B., Hoving J.L., van Tulder M.W. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trial. BMJ. 2003;326:911.
133. Walser R.F., Meserve B.B., Boucher T.R. The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta-analysis of randomized clinical trials. J Man Mani Ther. 2009;17:237.
134. Clare H.A., Adams R., Maher C.G. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004;50:209.
135. Young I.A., Michener L.A., Cleland J.A., et al. Manual therapy, exercise, and traction for patients with cervical radiculopathy: a randomized clinical trial. Phys Ther. 2009;89:632.
136. Reid S.A., Rivett D.A. Manual therapy treatment of cervicogenic dizziness: a systematic review. Man Ther. 2005;10:4.
137. Reid S.A., Rivett D.A., Katekar M.G., Callister R. Sustained natural apophyseal glides (SNAGs) are an effective treatment for cervicogenic dizziness. Man Ther. 2008;13:357.
138. Bronfort G., Assendelft W.J.J., Evenas R., et al. Efficacy of spinal manipulation for chronic headache: a systematic review. J Manipulative Physiol Ther. 2001;24:457.
139. Fernández-de-las-Peñas C., Alonso-Blanco C., Cuadrado M.L., Pareja J.A. Spinal manipulative therapy in the management of cervicogenic headache. Headache. 2005;45:1260.
140. Fernández-de-las-Peñas C., Alonso-Blanco C., Cuadrado M.L., et al. Are manual therapies effective in reducing pain from tension-type headache?: a systematic review. Clin J Pain. 2006;22:278.
141. Moraska A., Chandler C. Changes in clinical parameters in patients with tension-type headache following massage therapy: a pilot study. J Manual Manipulative Ther. 2008;16:106.
142. Tuchin P.J. A twelve month clinical trial of chiropractic spinal manipulative therapy for migraine. Australas Chiropr Osteopathy. 1999;8:61.
143. Tuchin P.J., Pollard H., Bonello R. A randomized controlled trial of chiropractic spinal manipulative therapy for migraine. J Manipulative Physiol Ther. 2000;23:91.
144. McNeely M.L., Armijo Olivo S., Magee D.J. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther. 2006;86:710.
145. Medlicott M.S., Harris S.R. A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorder. Phys Ther. 2006;86:955.
146. Kalamir A., Pollard H., Vitiello A.L., Bonello R. Manual therapy for temporomandibular disorders: A review of the literature. J Bodyw Mov Ther. 2007;11:84.
147. Aspegren D., Hyde T., Miller M. Conservative treatment of a female collegiate volleyball player with costochondritis. J Manipulative Physiol Ther. 2007;30:321.
148. Furlan A.D., Brosseau L., Imamura M., Irvin E. Massage for low-back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine. 2002;27:1896.
149. Hammer W.I., Pfefer M.T. Treatment of a case of subacute lumbar compartment syndrome using the Graston technique. J Manipulative Physiol Ther. 2005;28:199.
150. Assendelft W.J., Morton S.C., Yu E.I., et al. Spinal manipulative therapy for low back pain. A meta-analysis of effectiveness relative to other therapies. Ann Intern Med. 2003;138:871.
151. Ferreira M.L., Ferreira P.H., Latimer J., et al. Efficacy of spinal manipulative therapy for low back pain of less than three months’ duration. J Manipulative Physiol Ther. 2003;26:593.
152. Ferreira M.L., Ferreira P.H., Latimer J., et al. Does spinal manipulative therapy help people with chronic low back pain. Aust J Physiother. 2002;48:277.
153. Reinman M.P., Harris J.Y., Cleland J.A. Manual therapy interventions for patients with lumbar spinal stenosis: A systematic review. New Zealand J Physiother. 2009;37:17.
154. UK BEAM Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ. 2004;329:1377.
155. van den Dolder P.A., Roberts D.L. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain. Aust J Physiother. 2003;49:183.
156. Hammer W.I. The effect of mechanical load on degenerated soft tissue. J Bodyw Mov Ther. 2008;12:246.
157. Boyles R.E., Ritland B.M., Miracle B.M., et al. The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Man Ther. 2009;14:375.
158. Strunce J.B., Walker M.J., Boyles R.E., Young B.A. The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. J Man Manip Ther. 2009;17:230.
159. Bang M.D., Deyle G.D. 2000 Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther. 2000;30:126.
160. Bergman G.J.D., Winters J.C., Groenier K.H., et al. Manipulative therapy in addition to usual medical care for patients with shoulder dysfunction and pain: a randomized, controlled trial. Ann Intern Med. 2004;141:432.
161. Faber E., Kuiper J.I., Burdorf A., et al. Treatment of impingement syndrome: a systematic review of the effects on functional limitations and return to work. J Occup Rehabil. 2006;16:7.
162. Green S., Buchbinder R., Hetrick S.E. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003. Issue 2 Art No CD004258
163. Camarinos J., Marinko L. Effectiveness of manual physical therapy for painful shoulder conditions: a systematic review. J Man Manip Ther. 2009;17:206.
164. Vermeulen H.M., Obermann W.R., Burger B.J., et al. End-range mobilization techniques in the treatment of adhesive capsulitis of the shoulder joint: A multiple-subject case report. Phys Ther. 2000;80:1204.
165. Vermeulen H.M., Rozing P.M., Obermann W.R., et al. Comparison of high-grade and low-grade mobilization techniques in the management of adhesive capsulitis of the shoulder: randomized clinical trial. Phys Ther. 2006;86:355.
166. Howitt S.D. Lateral epicondylosis: a case study of conservative care using ART and rehabilitation. J Can Chiropr Assoc. 2006;50:182.
167. Haller K.H., Helfst R.H., Wilson J.K., Sevier T.L. Treatment of chronic elbow pain. Phys Ther Case Rep. 1999;2(5):195.
168. Brosseau L., Casimiro L., Milne S., et al. Deep transverse friction massage for treating tendonitis. Cochrane Database Syst Rev. 4, 2002.
169. Nagrale A.V., Herd C., Ganvir S., Ramteke G. Cyriax physiotherapy versus phonophoresis with supervised exercise in subjects with lateral epicondylalgia: a randomized clinical trial. J Man Manip Ther. 2009;17:171.
170. Bisset L., Paungmali A., Vicenzino B., Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. 2005;39:411.
171. Bisset L., Beller E., Jull G., et al. Mobilisation with movement, corticosteroid injection, or wit and see for tennis elbow: randomised trial. BMJ. 2006;333:939.
172. Struijs P.A., Damen P.J., Baller E.W., et al. Manipulation of the wrist for management of lateral epicondylitis: a randomized pilot study. Phys Ther. 2003;83:608.
173. Burke J., Buchberger D.J., Carey-Loghmani M.T., et al. A pilot study comparing two manual therapy interventions for carpal tunnel syndrome. J Manipulative Physiol Ther. 2007;30:50.
174. Baker D., Wilson J.K. Bilateral carpal tunnel syndrome in a piano teacher. Phys Ther Case Rep. 1999;2(2):73.
175. Tal-Akabi A., Rushton A. An investigation to compare the effectiveness of carpal bone mobilisation and neurodynamic mobilisation as methods of treatment for carpal tunnel syndrome. Man Ther. 2000;5:214.
176. Muller M., Tsui D., Schnurr R., et al. Effectiveness of hand therapy interventions in the primary management of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17:210.
177. O’Connor D., Marshall S.C., Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003. Issue 1. Art. No.: CD003219
178. Michlovitz S.L., Harris B.A., Watkins M. Therapy interventions for improving joint range of motion: A systematic review. J Hand Ther. 2004;17:118.
179. Randall T., Portney L., Harris B.A. Effects of joint mobilization on joint stiffness and active motion of the metacarpal-phalangeal joint. J Orthop Sports Phys Ther. 1992;16:30.
180. Folk B. Traumatic thumb injury management using mobilization with movement. Man Ther. 2001;6:178.
181. Howitt S., Wong J., Zabukovec S. The conservative treatment of trigger thumb using Graston Techniques and Active Release Techniques. J Can Chiropr Assoc. 2006;50:249.
182. Hoeksma H.L., Dekker J., Ronday H.K., et al. Comparison of manual therapy and exercise therapy in osteoarthritis of the hip: a randomized clinical trial. Arthritis Rheum. 2004;51:722.
183. MacDonald C.W., Whitman J.M., Cleland J.A., et al. Clinical outcomes following manual physical therapy and exercise for hip osteoarthritis: A case series. J Orthop Sports Phys Ther. 2006;36:588.
184. Hoeksma H.L., Dekker J., Ronday H.K., et al. Manual therapy in osteoarthritis of the hip: outcome in subgroups of patients. Rheumatology. 2005;44:461.
185. Henry P., Panwitz B., Wilson J.K. Treatment of a bilateral total knee replacement using augmented soft tissue mobilization. Phys Ther Case Rep. 1999;2(1):27.
186. Henry P., Panwitz B., Wilson J.K. Rehabilitation of a post-surgical patella fracture: A case study. Physiother. 2000;86(3):139.
187. Drover J.M., Forand D.R., Herzog W. Influence of active release technique on quadriceps inhibition and strength: a pilot study. J Manipulative Physiol Ther. 2004;27:408.
188. Wilson J.K., Sevier T.L., Helfst R.H., et al. Comparison of rehabilitation methods in the treatment of patellar tendinitis. J Sport Rehabil. 2000;9:304.
189. Deyle G.D., Henderson N.E., Matekel R.L., et al. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med. 2000;132:173.
190. Pollard H., Ward G., Hoskins W., Hardy K. The effect of a manual therapy knee protocol on osteoarthritic knee pain: a randomised controlled trial. J Can Chiropr Assoc. 2008;52:229.
191. Howitt S., Jung S., Hammonds N. Conservative treatment of a tibialis posterior strain in a novice triathlete: a case report. J Can Chiropr Assoc. 2009;53:23.
192. Melham T.J., Sevier T.L., Malnofski M.J., et al. Chronic ankle pain and fibrosis successfully treated with a new noninvasive augmented soft tissue mobilization technique (ASTM): a case report. Med Sci Sports Exerc. 1998;30:801.
193. van der Wees P.J., Lenssen A.F., Hendriks E.J., et al. Effectiveness of exercise therapy and manual mobilisation in acute ankle sprain and functional instability: a systematic review. Aust J Physiother. 2006;52:27.
194. Lin C.W., Moseley A.M., Haas M., et al. Manual therapy in addition to physiotherapy does not improve clinical or economic outcomes after ankle fracture. J Rehabil Med. 2008;40:433.
195. Brattberg G. Connective tissue massage in the treatment of fibromyalgia. Eur J Pain. 1999;3:235.
196. Kligman L., Wong R.K., Johnston M., Laetsch N.S. The treatment of lymphedema related to breast cancer: a systematic review and evidence summary. Support Care Cancer. 2004;12:421.
197. Vairo G.L., Miller S.J., McBrier N.M., Buckley W.E. Systematic review of efficacy of manual lymphatic drainage techniques in sports medicine and rehabilitation: an evidence-based practice approach. J Man Manip Ther. 2009;17:E80.
198. Batavia M. Contraindications for therapeutic massage: Do sources agree? J Bodyw Mov Ther. 2004;8:48.
199. Vickers A., Zollman C. ABC of complementary medicine. Massage therapies. BMJ. 1999;319:1254.
200. Bauer W.C., Dracup K.A. Physiological effects of back massage in patients with acute myocardial infarction. Focus on Critical Care. 1987;14(6):42.
201. Grant K.E. Massage safety: Injuries reported in Medline relating to the practice of therapeutic massage 1965-2003. J Bodyw Mov Ther. 2003;7:207.
202. Michaeli A. Reported occurrence and nature of complications following manipulative physiotherapy in South Africa. Aust J Physiother. 1993;39:309.
203. Cagnie B., Vinck E., Beernaert A., Cambier D. How are side effects of spinal manipulation and can these side effects be predicted? Man Ther. 2004;9:151.
204. Hurwitz E.L., Morgenstern H., Vassilaki M., Chiang L.M. Frequency and clinical predictors of adverse reactions to chiropractic care in the UCLA neck pain study. Spine. 2005;30:1477.
205. Assendelft W.J., Bouter L.M., Knipschild P.G. Complications of spinal manipulation: a comprehensive review of the literature. J Fam Pract. 1996;42(5):475.
206. Ernst E. Adverse effects of spinal manipulation: a systematic review. J R Soc Med. 2007;100:330.
207. Kraft C.N., Conrad R., Vahlensieck M., et al. Nicht-zerebrovaskuläre Komplikationen der chirotherapeutischen HWS-Manipulation. Z Orthop. 2000;138:8.
208. van Tulder M.W., Koes B., Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J. 2006;15:S64.
209. Cherkin D.C., Sherman K.J., Deyo R.A., Shekelle P.G. A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage, and spinal manipulation for back pain. Ann Intern Med. 2003;138:898.
210. DiFabio R.P. Manipulation of the cervical spine: risks and benefits. Phys Ther. 1999;79:50.
211. Ernst E. Manipulation of the cervical spine: a systematic review of case reports of serious adverse events, 1995-2001. Med J Aust. 2002;176:376.
212. Terrett A.G.J. Vertebrobasilar stroke following spinal manipulation therapy. In: Murphy D.R., editor. Conservative Management of Cervical Spine Syndromes. New York: McGraw-Hill; 2000:553-578.
213. Triano J.J., Kawchuk G. Current Concepts: Spinal Manipulation and Cervical Arterial Incidents. Clive, Iowa: NCMIC; 2006.
214. Hurwitz E.L., Aker P.D., Adams A.H. Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine. 1996;21:1746.
215. Haneline M.T., Croft A.C., Frishberg B.M. Association of internal carotid artery dissection and chiropractic manipulation. Neurologist. 2003;9:35.
216. Huijbregts P.A., Oostendorp R.A.B. Cervical artery dissection and manipulation: a review of relevant research with implications for diagnosis and management. Interdiv Rev Jan/Feb:23. 2010.
217. Rubinstein S.M., Peerdeman S.M., van Tulder M.W., et al. A systematic review of the risk factors for cervical artery dissection. Stroke. 2005;36:1575.
218. Rothwell D.M., Bondy S.J., Williams J.I. Chiropractic manipulation and stroke: a population-based case control study. Stroke. 2001;32:1054.
219. Cassidy J.D., Boyle E., Cote P., et al. Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine. 2008;33:S176.
220. Debette S., Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009;8:668.
221. Kerry R., Taylor A.J. Cervical arterial dysfunction assessment and manual therapy. Man Ther. 2006;11:243.
222. Kerry R., Taylor A.J., Mitchell J., et al. Manual therapy and cervical arterial dysfunction, directions for the future: a clinical perspective. J Man Manip Ther. 2008;16:39.
223. Childs J.D., Whitman J.M., Sizer P.S., et al. A description of physical therapists’ knowledge in managing musculoskeletal conditions. BMC Musculoskelet Disord. 2005;6:32.