Management of acute spinal cord injury
Cardiovascular considerations
Depending on the level and severity of injury, spinal shock may occur and last up to 6 weeks as a result of a loss of vascular tone and of the vasopressor reflex. Injury to the spinal cord from the level of the T1 to L2 damages the sympathetic nervous system (see Chapter 40) and may result in orthostatic hypotension and, potentially, bradycardia. The bradycardia results from the loss of cardiac acceleration fibers. Prompt treatment of spinal shock with intravascular fluids and vasoactive agents (see Chapter 88) to maintain a mean arterial pressure of 65 mm Hg to 75 mm Hg can potentially improve neurologic outcome.
Anesthetic management
Preoperative management
Airway management
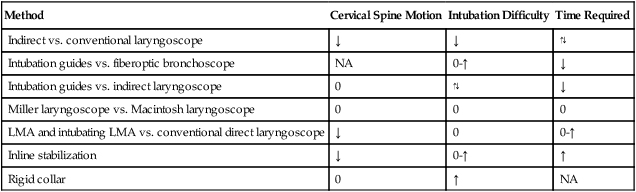
Intubation maneuvers (Table 140-1) can be gauged in accordance with the time needed and the amount of cervical neck manipulation associated with the use of a laryngoscope versus a fiberoptic bronchoscope.
Table 140-1
Comparison of Options for Anesthesia Management of Spinal Injury Procedures
| Method | Cervical Spine Motion | Intubation Difficulty | Time Required |
| Indirect vs. conventional laryngoscope | ↓ | ↓ | ⇅ |
| Intubation guides vs. fiberoptic bronchoscope | NA | 0-↑ | ↓ |
| Intubation guides vs. indirect laryngoscope | 0 | ⇅ | ↓ |
| Miller laryngoscope vs. Macintosh laryngoscope | 0 | 0 | 0 |
| LMA and intubating LMA vs. conventional direct laryngoscope | ↓ | 0 | 0-↑ |
| Inline stabilization | ↓ | 0-↑ | ↑ |
| Rigid collar | 0 | ↑ | NA |
Cardiovascular considerations
In summary, the goals in the treatment of a patient with spine cord injury are the following:










