Chapter 97A Liver transplantation
Indications and general considerations
Overview
It is difficult to identify any one cause for the increase in success. The contribution of better surgical and anesthetic techniques, improved postoperative care, and availability of better immunosuppressive agents have all contributed to the improvements in survival (see Chapter 97B). In addition, understanding of both indications and contraindications for the procedure have improved such that major surgery is not carried out in patients with virtually no chance of surviving, and patients are referred for transplantation at a stage when they are likely to have the greatest chance of success.
General Indications
Absolute Contraindications to Transplantation
• The patient is not fit enough to withstand surgery, for example, because of advanced cardiac or pulmonary disease.
• The patient is unlikely to survive the procedure, such as with active sepsis.
• Survival after transplantation may be too short to justify the risks of transplantation, as in the case of metastatic disease.
• Active alcoholism and substance misuse is present, evident by noncompliance with medical advice ascertained on psychiatrist or psychologist evaluation.
• The postoperative quality of life may be unacceptable to the patient, for example, as with severe, intractable depression.
• Surgery is technically impossible, as in patients with extensive venous thromboses.
Relative Contraindications to Transplantation
• Age may be an issue, and age restrictions vary at transplant centers; biologic age, rather than chronologic, is more important.
• Cholangiocarcinoma is sometimes a contraindication; transplant may still be considered, but only in highly selected patients because of the high risk of early recurrence.
• Chronic or refractory infections may preclude transplantation, depending on the nature of the infection and whether it is amenable to cure with available therapy.
• Poor social support may be a contraindication, particularly in biologically older patients with prolonged recovery anticipated after transplantation.
General Aspects
Nutrition
Malnutrition is a common finding in end-stage cirrhosis, with a prevalence of 81% (Caregaro et al, 1996). Malnutrition in these patients has many causes: the disease depletes the patient, and the situation is compounded by poor intake, malabsorption, and dietary restrictions that are often inappropriate. Malnutrition is associated with increased susceptibility to infection and poor healing. Although in liver disease, the degree of malnutrition may be difficult to quantify, malnourished patients fare poorly, with reported mortality of 15% (Campillo et al, 2003). Although no convincing evidence proves that improvement in nutrition alters the outcome, it seems prudent to optimize nutrition (Figueiredo et al, 2000), and it is sensible to correct vitamin and other nutrition deficiencies.
Psychologic Assessment
Transplantation is associated with major psychologic stress, both for the patient and the family. More than half of those in the liver transplant candidate population have a wide range of psychologic health problems (Day et al, 2009). Initially, many centers arranged for full psychologic and psychiatric assessment of all potential transplant candidates, but this is rarely undertaken. Chronic ill health, possible subclinical encephalopathy, and future uncertainties all combine to make it difficult to accurately predict a patient’s outcome. In addition, when a history of psychiatric illness is present, expert assessment is required. Some patients with psychiatric illness that is unresponsive to therapy and those with a history of recurrent episodes of self-harm may not be suitable candidates for transplantation.
Age
There is no agreed upper age limit, but advanced age is associated independently with mortality after transplant (Burroughs et al, 2006). The concept of biologic age has superseded that of chronologic age, although the former cannot readily be defined or quantified.
Previous Abdominal Surgery
The presence of adhesions, especially in the presence of portal hypertension, adds considerably to the difficulties of surgery and may affect outcome, especially when this involves surgery to the biliary tree (Neuberger et al, 1999).
Infection
Human Immunodeficiency Virus
Although early studies showed patients with HIV infection fared poorly (Rubin et al, 1987; Tzakis et al, 1990), with the introduction of highly active antiretroviral therapy (HAART), the natural history of HIV infection has been greatly altered (Roland & Stock, 2006), although patients with hepatitis C virus (HCV) coinfection are at high risk for developing end-stage liver disease (Graham et al, 2001). Short-term outcomes in patients with HIV are encouraging (Fung et al, 2004), but the procedure remains limited to a few centers. Indications are becoming better defined (Samuel et al, 2003) and include 1) end-stage liver disease, 2) low or undetectable levels of HIV RNA, 3) no autoimmune deficiency syndrome (AIDS)-defining complication, and 4) a CD4 count greater than 200/mL.
Cardiovascular Disease
As with other diseases, the prognosis of patients with cardiovascular diseases will dictate whether liver replacement is an appropriate therapy. Multivessel, moderate to severe coronary artery disease is present in 15% of patients with end-stage liver disease (Tiukinhoy-Laing et al, 2006). Preoperative assessment of cardiovascular status is, at best, imprecise, as no clear guidelines exist to define limits below which grafting is unsafe. When it is possible to correct coronary artery disease, this should be undertaken prior to transplantation.
Respiratory Function
Arterial hypoxemia, an oxygen saturation less than 92% or arterial oxygen pressure less than 70 mm Hg, may be found in up to 70% of patients with liver disease. Several possible causes for this hypoxemia include ventilation-perfusion mismatch, diffusion limitation, alveolar hypoventilation, shunt, and diffusion-perfusion abnormality (Krowka & Cortese, 1990). Furthermore, pulmonary dysfunction is present in up to 2% of patients with advanced liver disease. The presence of significant pulmonary disease is usually apparent on history and examination, but significant pulmonary disease may be cryptic. The many possible causes for these abnormalities include 1) diseases unrelated to the liver, such as those caused by smoking; 2) organic liver disease, such as α1-antitrypsin deficiency; 3) respiratory conditions associated with certain liver disease, such as fibrosing alveolitis associated with primary biliary cirrhosis; 4) the effects of the liver disease on respiratory function, such as ascites that causes a pleural effusion or simple lung compression; 5) hepatopulmonary syndrome, and 6) portopulmonary hypertension.
Hepatopulmonary Syndrome
Hepatopulmonary syndrome is characterized by abnormal intrapulmonary vascular dilation (Hoeper et al, 2004). Clinically, it encompasses a triad of arterial deoxygenation, intrapulmonary vascular dilation, and liver disorder. The diagnosis is suggested by showing orthodeoxia, a fall in arterial blood oxygen when standing, and the presence of intrapulmonary shunting, demonstrated by either bubble echocardiography or nuclear medicine scanning.
Portopulmonary Hypertension
Portopulmonary hypertension results from pulmonary vasoconstriction and leads to vascular remodeling, which results in pulmonary hypertension (Hoeper et al, 2004). Diagnostic criteria include presence of liver disease that results in portal hypertension; mean pulmonary arterial pressure of more than 25 mm Hg at rest or 30 mm Hg during exercise; mean pulmonary artery occlusion pressure of less than 15 mm Hg; and pulmonary vascular resistance more than 240 dyn/sec/cm−5 (Krowka, 2003).
No clear guidelines are available that establish when liver transplantation is contraindicated because of pulmonary disease (Krowka et al, 2004). A preoperative partial pressure of oxygen of less than 50 mm Hg and a lung scan with brain uptake of more than 20% (Arguedas et al, 2003) strongly predict mortality, although these patients may be candidates for a triple transplant of heart, lung, and liver. Similar considerations apply to those with cystic fibrosis, cystic lung disease, and liver disease. Long-term oxygen therapy is the most frequently recommended therapy for symptomatic hypoxemic patients, but the use of drugs and transjugular intrahepatic shunt (TIPS) requires validation in this setting.
Coexisting Disease
The presence of coexisting disease may affect the decision to offer the patient a liver graft, either because the prospects of recovery are adversely affected, or because long-term survival may be reduced (Volk et al, 2007). Diabetes mellitus (DM) is commonly found in patients with chronic liver disease, especially in those with HCV infection. DM may occur as a consequence of the insulin intolerance associated with advanced liver disease; if so, it will resolve after successful transplantation. Concerns for those with diabetes center upon the possible microvascular complications. Evidence of a proliferative retinopathy, diabetic nephropathy, or autonomic neuropathy—evidenced by simple tests, such as abnormal beat-to-beat variation on Valsalva maneuver or postural hypotension—may be relative contraindications for transplantation. The presence of advanced microvascular disease puts the patient at risk of major autonomic disruption during the procedure, and the survival of such patients is relatively poor (Haydon & Neuberger, 2001).
Hyponatremia is a common finding in patients with advanced chronic liver disease, and it usually occurs either as a consequence of injudicious diuretic therapy or because of the reduced free-water clearance. Grafting patients with severe hyponatremia (serum sodium <120 mmol/L) has shown an increased risk of central pontine myelinolysis (Yun et al, 2009). Significant hyponatremia should be corrected prior to transplantation, either by simple water restriction and, if appropriate, cessation of diuretic therapy or, if more rapid correction is required, by use of renal support (Elias & McMaster, 1987). The role of aquaretics may also be helpful in this situation (O’Leary & Davis, 2009).
Renal disease may occur either as a consequence of the hepatorenal syndrome or as a result of intrinsic kidney damage. In the hepatorenal syndrome, the kidney is not structurally damaged, and once good liver function is reestablished, the kidney will function normally; so although the prognosis may be poorer in the presence of advanced renal insufficiency (Rimola et al, 1987), the hepatorenal syndrome is not an absolute contraindication to transplantation. When coexisting advanced renal disease is evident, it may be advisable to consider combined liver and kidney transplantation, as renal function remains a major predictive factor for the outcome after transplantation (Nair et al, 2002). It is uncertain whether pretransplant correction of renal parameters—for example, by dialysis—is associated with an improvement in survival.
Past history of malignancy is a relative contraindication to transplantation, because the effect of surgery and the consequent immunosuppression may predispose the patient to early recurrence of tumor (Penn, 1993; Saigal et al, 2001). In 1993, Penn identified those tumors that have a high risk of recurrence after transplantation (Box 97A.1). Most centers will offer transplantation when the risk of recurrence is below 10% at 5 years; however, recurrence rates with other kinds of malignancies—colorectal cancer (18.8%), nonmelanoma skin cancers (23.5%), thyroid carcinoma (25%), oral squamous carcionoma (33%), vulvovaginal cancers (33%), and breast carcinoma (33%)—are associated with a higher risk following liver transplantion (Benten et al, 2008). In only exceptional cases should patients with any of the above extrahepatic malignancies be considered suitable candidates for transplantation.
Box 97A.1
Effect of Immunosuppression on Tumor Recurrence
From Penn I, 1993: The effect of immunosuppression on pre-existing cancers. Transplantation 55:742-747.
Bone Disease
Many patients with chronic liver disease will have bone disease. The occurrence of osteomalacia as a consequence of vitamin D malabsorption is low and can readily be corrected by parenteral administration of vitamin D; however, osteoporosis is a far greater problem and is particularly seen in female patients with chronic cholestatic disease. In many cases, successful transplantation will halt or retard the progression and may even improve bone mineralization (Guichelaar et al, 2007). The presence of severe osteoporosis may result in additional complications in the presence of significant thoracic or lumbar vertebral collapse or fractures. The development of severe osteoporosis may well be an indication for transplantation in itself.
Specific Diseases
Fulminant Hepatic Failure (See Chapter 97C)
In recent years it has been realized that liver transplantation is an effective form of therapy for patients with fulminant hepatic failure (FHF), that is, the presence of encephalopathy occurring within 8 weeks of the onset of symptoms in a patient with previously normal liver (Peleman et al, 1987; Chapter 97C). FHF requiring transplantation accounts for less than 5% of liver transplantations. In those with severe FHF and grade 4 hepatic encephalopathy, the mortality approaches 80%. Common causes of FHF include paracetamol (acetaminophen) overdose; viral infections, such as hepatitis A, B, E, and rarely C; drug and xenobiotic toxicity, including those caused by herbal remedies; Wilson disease; and liver diseases of pregnancy.
Patients with FHF develop early multiorgan failure and require intensive supportive therapy. The common causes of death are cerebral edema, multiorgan failure, sepsis (bacterial or fungal), cardiac arrhythmia or arrest, and respiratory failure (Ostapowicz et al, 2002). Indeed, FHF poses a difficult problem, because the window is very narrow between the time when it is apparent that the patient’s survival is likely to be poor in the absence of transplantation and the onset of irreversible complications that preclude a successful outcome.
Several groups have now published prognostic factors, and based on those, criteria for super-urgent transplantation in the United Kingdom have been published; these are listed in Table 97A.1 (Bismuth et al, 1987; Neuberger et al, 2008; O’Grady et al, 1989). The King’s College model has been validated in other centers and was found to be robust, although it is likely that with advances in the medical management of patients with FHF, these prognostic factors will require modification. The inclusion of serum lactate in the King’s College prognostic criteria provides greater accuracy (Riordan & Williams, 2002).
Table 97A.1 Current Transplant Criteria in the United Kingdom for Registration as a Super-Urgent Transplantation for Fulminant Hepatic Failure
| Category | Etiology |
|---|---|
| 1 | Acetaminophen poisoning with pH <7.25 >24 h after overdose and after fluid resuscitation |
| 2 | Acetaminophen poisoning with PT >100 sec, or INR >6.5 and serum creatinine >300 mmol/L, or anuria and grade 3 to 4 encephalopathy |
| 3 | Acetaminophen poisoning with serum lactate level >24 h after overdose >3.5 mmol/L on admission or >3.0 mmol/L after fluid resuscitation |
| 4 | Acetaminophen poisoning with 2 of the 3 criteria from category 2 with clinical evidence of deterioration (e.g., increased ICP, Fio2 >50%, increasing inotrope requirements) in the absence of clinical sepsis |
| 5 | Seronegative hepatitis, hepatitis A, hepatitis B, or an idiosyncratic drug reaction with PT >100 sec or INR >6.5 and any grade of encephalopathy |
| 6 | Seronegative hepatitis, hepatitis A, hepatitis B, or an idiosyncratic drug reaction; any grade of encephalopathy; and any three from the following: unfavorable etiology (idiosyncratic drug reaction, seronegative hepatitis), age >40 years, jaundice to encephalopathy time >7 days, serum bilirubin >300 mmol/L, PT >50 sec or INR >3.5 |
| 7 | Acute presentation of Wilson disease or Budd-Chiari syndrome, a combination of coagulopathy, and any grade of encephalopathy |
| 8 | Hepatic artery thrombosis on days 0 to 21 after liver transplantation |
| 9 | Early graft dysfunction on days 0 to 7 after liver transplantation with at least two of the following: AST >10,000 IU/L, INR >3.0, serum lactate >3 mmol/L, absence of bile production |
| 10 | Severe liver failure in any liver donor within 4 weeks of a donor operation |
AST, aspartate aminotransferase; Fio2, inspired oxygen concentration; ICP, intracranial pressure; INR, international normalized ratio; PT, prothrombin time
Modified from Neuberger et al, 2008: Selection of patients for liver transplantation and allocation of donated livers in the UK. Gut 57(2):252-257.
One of the best guides to progression is given by serial estimation of the prothrombin time (Harrison et al, 1990) or factor V levels (Bernuau et al, 1986), because in the absence of extraneous blood products, these best represent the synthetic function of the liver. Initial improvement in the prothrombin time followed by deterioration suggests the presence of sepsis; therefore such patients should no longer be considered potential candidates. In addition, the patient remains at risk of developing complications related to raised ICP for up to 48 hours after successful transplantation (Dabos et al, 2004; Keays et al, 1991).
Because many of the extrahepatic manifestations of FHF may be a consequence of the presence of large amounts of necrotic tissue, some centers have advocated the use of a two-stage procedure, whereby the failed liver is removed, and the patient remains anhepatic until a suitable graft can become available (Ringe et al, 1993). Although there is little doubt that following hepatectomy, the patient’s condition may well improve, few convincing data are available at present to suggest that this approach improves outcome; however, such a procedure may be indicated in a patient who is rapidly deteriorating for whom a graft has been found, but logistic conditions may enforce some delay before the graft can be successfully performed.
One of the dilemmas in considering liver transplantation in patients with acute liver failure is that if the liver does recover, a complete return to normal structure and function is likely. The use of auxiliary transplantations, such as auxiliary partial orthotopic liver transplantation, or partial transplantations may allow the earlier use of liver grafting as a safety net; because if the patient’s liver does recover, the donor liver can be removed or allowed to atrophy, and the patient can return to a life of good liver function free of immunosuppression. The use of artificial liver support devices (Chapter 72) remains uncertain, but systems such as the molecular absorbent recirculation system (MARS; Gambro AB, Sweden) may offer a bridge to transplantation (Mitzner et al, 2002).
Metabolic Diseases
A number of metabolic diseases account for less than 5% of liver transplantations in adults, and these may be corrected by liver transplantation (Table 97A.2). In some cases, where the metabolic defect arises in the liver, transplantation will correct that defect. This is seen, for example, with Wilson disease or hemophilia. In other conditions, such as some types of hypercholesterolemia, the metabolic defect occurs within the liver, but the heart is the organ affected. Some centers have advocated the use of liver transplantation to prevent the onset of severe coronary artery disease, although when cardiac disease is already present, combined heart and liver transplantations may also be performed. Similar considerations apply to hyperoxaluria that requires liver and kidney replacement. In other conditions, such as hemophilia, with alternative therapies such as replacement with factor VIII, transplantation should only be considered if liver disease is extensive, such as may occur with HCV infection transmitted via blood products.
Table 97A.2 Inborn Errors of Metabolism that Have Been Treated by Liver Transplantation
| Liver Affected | Other Organs Also Affected |
| α1-Antitrypsin deficiency | Primary hyperoxaluria |
| Wilson disease | Crigler-Najjar syndrome |
| Protoporphyria | Primary hypercholesterolemia |
| Tyrosinosis | Niemann-Pick disease |
| Tyrosinemia | Sea-blue histiocyte disease* |
| Galactosemia | Hemophilia A and B |
| Glycogen storage disease types I and IV | Protein C deficiency Protein S deficiency |
| Byler disease | |
| Hemochromatosis* | |
| Cystic fibrosis | |
| Gaucher disease* | |
| Urea cycle enzyme deficiencies |
Budd-Chiari Syndrome
The role of liver transplantation in patients with Budd-Chiari syndrome remains uncertain (Chapter 77). There may be underlying thrombotic disorders, such as deficiencies in proteins C or S, Factor V Leiden mutation, lupus anticoagulant, polycythemia, or myeloproliferative disorders; some of these will be corrected by transplantation, whereas others will carry the risk of complications, such as malignant transformation (Menon et al, 2004). The early use of anticoagulants and interventional radiology has changed the management of these patients (Darwish Murad et al, 2009). In general, transplantation should be considered when portal decompression has failed, when it is not feasible, or in the presence of established cirrhosis.
Chronic Liver Disease
Although intractable pruritus is a valid indication for transplantation, if all other measures for treatment are unsuccessful, lethargy often fails to improve and so is not, in itself, an indication; it is important to exclude extrahepatic disorders, such as coexistent myxedema or therapy that may cause lethargy. Recent evidence (Piche et al, 2005) suggests that ondansetron may be effective in improving the fatigue associated with chronic liver disease.
Most centers consider transplantation appropriate when the estimated length of life in the absence of transplantation is limited to 1 year; however, in practice, this is very difficult to assess for most patients (Box 97A.2). Mostly, chronic liver disease runs a fairly predictable course, although the patient’s life may be threatened by unpredictable events, such as sepsis or variceal hemorrhage. It is for this reason that timing of transplantation remains an inexact science. A further feature to be considered is that many of the factors predicting a poor survival in patients with cirrhosis are different from those that predict outcome after transplantation.
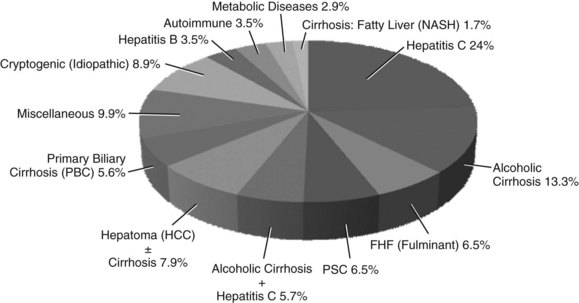
Box 97A.2 Indications for Transplantation in Patients with Cirrhosis
The use of prognostic models have helped define those variables that predict outcome, but such models do have disadvantages. First, most prognostic models are defined from retrospective studies that use patient data either at referral or at a certain point in the course of the illness, and it may be inappropriate to reapply these models sequentially, unless time-dependent models are used. Second, models provide data for populations, and their application to an individual is limited by relatively wide confidence intervals. Nonetheless, the Child-Turcotte-Pugh (CTP) classification does provide a useful guide, although it may not be sufficiently detailed for estimation of short-term survival. The MELD score is also a useful marker of short-term prognosis and may be more accurate than the CTP score (Freeman et al, 2004; Olthoff et al, 2004). The onset of hepatic decompensation is often a useful clinical marker of a poor prognosis. Indications for consideration of transplantation are shown in Figure 97A.1 and Box 97A.2.
The development of complications may often precipitate referral for transplantation. Thus the development of severe ascites, spontaneous bacterial peritonitis, recurrent variceal hemorrhage, and intractable encephalopathy are all indications that hepatic reserve is limited (Gines et al, 1988; see Chapter 70A, Chapter 70B, Chapter 72, Chapter 73, Chapter 74 ). Both the CTP classification and the MELD score are relatively poor prognostic guides to survival after grafting; however, data suggest that transplantation of a patient with a MELD score less than 12 in those without malignancy is associated with a reduction in survival at 1 year (Neuberger, 2004).
Other centers have concentrated on functional tests of the liver (Chapter 2), and although tests such as the aminopyrine breath test, the monoethyl glycine xylidide (MEGX) test, and the galactosamine elimination clearance have their advocates, none has added greatly to clinical and serologic assessment, and none has been applied widely (Burdelski et al, 1991; Mericel et al, 1992).
Primary Biliary Cirrhosis
The prognostic criteria for transplantation in primary biliary cirrhosis (PBC) are well defined; it accounts for less than 5% of liver transplantations, and a decreasing trend has been observed. Since the early paper by Schaffner and coworkers (Shapiro et al, 1979), it has become clear that the serum bilirubin is the best guide to prognosis. Once the serum bilirubin exceeds 150 µmol/L, median survival in the absence of transplantation is approximately 18 months.
A number of prognostic models have been developed, including both static and time-dependent models (Neuberger, 1989), and these are helpful in defining those variables that predict survival, both in the absence of transplantation and following transplantation (Box 97A.3). From these models, an estimate of survival can be made; however, these models must be used with some care, because the confidence intervals are relatively wide, and any information derived from such models must be made in conjunction with clinical judgment. Ursodeoxycholic acid (UDCA) is now licensed for use in patients with PBC and is associated with a significant delay in transplantation. In most patients, there is a fall in serum bilirubin, but the prognostic models remain valid when applied 6 months after introduction of treatment.
Box 97A.3 Prognostic Models for Estimating Survival in Patients with Primary Biliary Cirrhosis
The causes for lethargy in patients with PBC are numerous: depression is common and often responds to antidepressant medication. Celiac disease is found in 3% of patients with PBC (Kingham & Parker, 1998) and may cause lethargy if unrecognized and untreated. Low levels of antibodies to gliadin are common in patients with liver disease, so celiac disease should be tested for by measuring antiendomysial antitransglutaminase antibodies; in addition, a small bowel biopsy should be taken when these antibodies are present. Coexisting myxedema should be excluded by measuring serum thyroid-stimulating hormone (TSH), and the patient should be tested for Addison disease if appropriate.
Primary Sclerosing Cholangitis (See Chapter 41)
In contrast to PBC, the natural history of primary sclerosing cholangitis (PSC) is far less clear and predictable (Ludwig et al, 1990) and accounts for about 6% of all transplantations. For many patients, the disease runs a fluctuating course with exacerbations and remissions that may be due to episodes of spontaneously occurring bacterial cholangitis. Underlying these fluctuations in liver function is a persistent and relentless progression toward liver failure.
As with other chronic liver diseases, serum bilirubin and serum albumin remain useful markers of progression, and prognostic models will help in timing the procedure (see Box 97A.4). The CTP classification and MELD score are as reliable as the Mayo model (Shetty et al, 1997; see Chapter 70B).
Box 97A.4 Mayo Prognostic Model for Estimating Survival in Patients with Primary Sclerosing Cholangitis
Most cases of PSC are associated with inflammatory bowel disease, usually ulcerative colitis. Patients with PSC and colitis are at increased risk of colonic cancer, compared with those with colitis alone; because the cancers tend to be in the ascending colon, a full colonoscopy is recommended in all potential transplant candidates to exclude colonic neoplasia and to assess the degree of colitis. Quiescent colitis is not a contraindication to transplantation, but active colitis should be treated before transplantation. When surgical treatment is required to control the colitis, this can safely be done at the time of the transplant procedure. Colectomy either before or during transplantation confers a protective effect against recurrent PSC in subsequent grafts (Alabraba et al, 2009).
PSC is a premalignant condition with the patient at increased risk of developing cholangiocarcinoma in any part of the biliary tree (Rosen & Nagorney 1991), and up to 20% of patients with PSC may develop a cancer, especially smokers (see Chapter 50A). Bile duct dysplasia may identify a group of patients at special risk, but this is still controversial. It is often difficult to be certain whether a sudden deterioration in the patient is due to the development of cholangitis, the natural history of the disease, or the development of cholangiocarcinoma (Bergquist et al, 1998).
Methods of detection of cholangiocarcinoma are often unrewarding: serum markers such as carcinoembryonic antigen (CEA) are relatively nonspecific and insensitive; elevated levels of carbohydrate antigen (CA) 19-9 may be more helpful but are not specific (Qin et al, 2004). Imaging techniques including CT, magnetic resonance imaging (MRI), ultrasound, and angiography are often unreliable and miss even quite large tumors. Although the presence of dilated intrahepatic bile ducts is often a useful sign of cholangiocarcinoma, it also is too insensitive and nonspecific for routine use.
The biliary tree can usually be well visualized by magnetic resonance cholangiopancreatography (MRCP), which gives images almost as good as those obtained at endoscopic retrograde cholangiopancreatography (ERCP); however, MRCP does not allow tissue to be taken for histology or cytology (see Chapters 17 and 18). ERCP may be helpful if brushing for bile cytology is combined with biopsy of structures. Although the specificity is high, the sensitivity is relatively low, and the procedure is not without risk of precipitating severe cholangitis. Directed percutaneous biopsy or aspiration cytology again may give a positive diagnosis, but negative findings do not exclude the possibility of cholangiocarcinoma.
It must be emphasized that ERCP in the presence of advanced PSC may lead to sudden deterioration, presumably as a result of the introduction of biliary sepsis. If cholangiocarcinoma is known to be present prior to transplantation, survival is poor; thus clinicians at most centers believe the patient who is known to have cholangiocarcinoma should not be considered for transplantation, although a very small proportion of patients with cholangiocarcinoma may benefit from an aggressive approach with brachytherapy and chemotherapy (Heimbach et al, 2004).
No effective medical treatment is currently available for PSC, although encouraging claims have been made for the use of UCDA at high doses (>20 mg/kg body weight/day), but this has been challenged (Lindor et al, 2009). Surgical intervention may be helpful, although endoscopic dilation or stenting should usually be considered only in the presence of a single, dominant extrahepatic stricture. The use of biliary diversion and reconstruction is associated with a poorer result following transplantation. In our experience in Birmingham, United Kingdom, the 1-year survival of patients with PSC without prior biliary surgery was significantly better (Ismail et al, 1991). Analysis of the Mayo Clinic database suggests that the prognostic markers for patients with PSC after transplantation include disease severity, previous biliary or shunt surgery, concurrent bile duct cancer, and the presence of inflammatory disease (Wiesner et al, 1996; Chapter 42A). Our own analysis confirms these observations, but we did find that although ulcerative colitis was associated with a better outcome, Crohn disease was associated with an adverse outcome (Neuberger et al, 1999).
Alcoholic Liver Disease
Selected patients with alcoholic liver disease are excellent candidates for transplantation, accounting for 13% as a single indication and 19% with HCV. Initial concerns were that these patients would continue to drink alcohol to excess, comply poorly with follow-up, and be unreliable about taking immunosuppression medications. Furthermore, the ravages of alcohol include not only damage to the liver, other organs—including heart, brain, pancreas, and bone marrow—may be affected. Finally, patients with alcoholic liver disease are often more likely to have associated psychiatric problems; however, in 1988, Starzl and colleagues reported an estimated survival of more than 70% in 41 patients transplanted for alcoholic liver disease. Of these patients, only 2 returned to alcohol abuse and subsequently died. The survival rates of these patients were similar to other patients with cirrhosis. Following these encouraging results, other centers started to consider patients with alcoholic liver disease for transplantation, and most centers now do consider such patients as candidates for the procedure (Kumar et al, 1990). Nonetheless, there remains a decreasing body of opinion that takes the view that, because alcoholic liver disease is a self-induced injury, and in view of the expense of the procedure and the limited supply of donor organs, such candidates should not be considered. In the view of most transplant units, however, this is not considered appropriate, because patients with alcoholic liver disease are not necessarily alcohol dependent; there exists a large number of self-induced diseases, and it would be no more appropriate to deny a patient with alcohol-induced liver disease transplantation for the reason it is self-induced than to deny treatment for a broken limb in a rugby player or mountain climber.
In addition to the usual criteria for transplantation and contraindications to the procedure, other specific factors need to be considered for patients with alcoholic liver disease: the first is the effect of alcohol abstinence, which undoubtedly improves survival in patients who are seen initially without compensated or decompensated cirrhosis. Although those who come to medical attention with variceal hemorrhage or severe ascites often only have limited benefit after abstinence from alcohol, those with mild ascites or other complications may have a significant improvement in both quality and quantity of life once they abstain from drinking (Suterakis et al, 1973). Furthermore, because it is now becoming apparent that those who do not abstain from alcohol are more likely to return to drinking excessively following transplantation and are less likely to comply with follow-up (Beresford et al, 1990), some centers insist on an abstinent period of 6 months. No robust justification exists for this period of abstinence, and the duration of abstinence correlates poorly with posttransplant abstinence. Furthermore, the disease may progress before the stipulated period of abstinence is over. In particular, patients with liver failure are unlikely to survive if they do not recover within the first 3 months of abstinence (Veldt et al, 2002). A period of abstinence is helpful in part to ensure that the native liver will not recover to such an extent that transplantation is no longer required, but also to identify why the person has drunk excessively and to put in place appropriate measures so that there will be a lower risk of recurrence after transplantation. So the period of abstinence must be considered in the light of the patient’s condition, and transplantation is offered to the patient who has remained abstinent after being so advised (Neuberger et al, 2002).
On the physical side, in addition to the routine workup, the extrahepatic effects of alcohol must be assessed, and those with advanced alcoholic cardiomyopathy or pancreatitis may not be suitable on such grounds. Psychiatric assessment is used extensively in some centers (Beresford et al, 1990), and these centers have suggested that patients who are not alcohol dependent, who have found alternative substitutes for alcohol, who have a job, who have taken part in rehabilitation programs, and who have an understanding of their problems often do very well following transplantation. Thus, patients with alcoholic liver disease are certainly potential candidates, and as such they do require appropriate referral for consideration.
Hepatitis B Viral Infection
Patients with hepatitis B virus (HBV) infection can be considered for transplantation either because of FHF or because of chronic liver disease, accounting for less than 5% of transplantations (see Chapter 64). Of those with FHF, the conventional criteria apply as indicated above. Because it is thought that the liver failure in these patients is due to the rapid clearance of virus-infected hepatocytes, most patients at the time of transplantation are HBV DNA negative and, as such, the disease recurs less commonly than in those with chronic HBV infection.
However, different considerations apply to those with chronic liver disease. Those who are HBV DNA positive at the time of transplantation are much more likely, if untreated, to have recurrence of disease following transplantation, and this is associated with a significantly poorer outcome (Freeman et al, 1991; O’Grady et al, 1992; Rizetto et al, 1991); thus patients with high HBV DNA positivity prior to transplantation are not suitable candidates. The management of these patients has been revolutionized by the introduction of effective antiviral therapy (Kim et al, 2004) that has significantly reduced the need for liver transplantation; patients with active viral disease should be treated with antivirals. At present, there are seven approved treatments for chronic HBV, and choice of treatment is based on the e-antigen status, resistance pattern, adverse events, and cost (Lok & McMahon, 2009). Treatment with HBV immunoglobulin (HBIg) and lamivudine or other antiviral agent must be continued after transplantation.
Hepatitis C Viral Infection
The indications for transplantation of patients with HCV infection are increasing, similar to those with cryptogenic cirrhosis (see Chapter 64). After 20 years of infection, up to 20% of HCV-infected patients progress to cirrhosis (Freeman et al, 2001). The optimal time to treat is before onset of advanced fibrosis or liver failure, because 5-year survival is only 50% after the onset of hepatic failure (Fattovich et al, 1997). Patients with detectable HCV at the time of transplant will almost invariably develop recurrent disease, although the extent of graft damage is variable. Many factors—host, donor, and immunosuppressive—are associated with the extent and rate of graft damage.
Because of the effect of recurrence in the graft, some have tried antiviral therapy with pegylated interferon and ribavirin prior to transplant (Everson, 2004). When this can be done safely, a sustained viral response (SVR) is associated with a much lower risk of graft infection and damage, and 5-year survival after transplantation is similar to patients grafted for other causes of cirrhosis, although concerns remain whether survival in the longer term will be adversely affected by recurrent disease. Treatment with interferon and ribavirin may be effective in selected groups, but SVR is often hard to achieve, and treatment is poorly tolerated.
Patients with hemophilia and HCV infection pose a special problem. Although liver transplantation will correct the defect in hemophilia, this itself is not an indication for liver transplantation. Many patients will have contracted HCV through contaminated blood products. Provided the patient is supported with adequate amounts of the appropriate blood products, liver transplantation poses no major problem, and many patients will not need support beyond 72 hours (McCarthy et al, 1996).
Hepatocellular Carcinoma (Chapters 80 and 97D)
Hepatocellular carcinoma (HCC) may occur in a noncirrhotic liver, but in the Western population, it more commonly arises in the context of cirrhosis and accounts for 8% of transplants, 5.6% in those with cirrhosis. A number of approaches to the treatment of HCC have been adopted and include chemotherapy, resection, embolization, transarterial chemoembolization (TACE), injection with ethanol, cryotherapy, radiofrequency ablation (RFA), and transplantation (see Chapters 83 through 86 and 88). In those with HCC, some have argued that resection should be considered first with salvage liver transplantation used where there is tumor recurrence (Belghiti et al, 2003; Sala et al, 2004). Indications include a normal serum bilirubin and absence of portal hypertension. Such an approach remains controversial. Very few well-conducted prospective randomized trials of treatment have been conducted, and most reports are based on selected patients and compared with historic controls. It must also be remembered that in those with HCC arising in a cirrhotic liver, the optimal treatment will depend not only on the natural history of the HCC but also on the severity and extent of the liver disease.
Transplantation for patients with HCC raises a number of questions, and at the present time, few hard data are available upon which to base a logical strategy. Most centers currently adopt the Milan criteria for accepting a patient for transplantation (Mazzaferro et al, 1996). These criteria are a single tumor of less than 5 cm in diameter or, in those with multiple tumors, no more than three tumors, all less than 3 cm in diameter. The analysis was based on a small number of patients, but the results have been confirmed in larger series. Extrapolation for these observations to current practice must be done with caution, as imaging techniques have improved, so more lesions are being detected. Thus, it may be inappropriate to extrapolate conclusions based on studies done in the late 1990s.
It is clearly not the size of the tumor per se that is important, but that the size reflects the likelihood of tumor microinvasion and spread and thereby reflects the chance of recurrence after transplant; of course, this is not strictly recurrence but persistence. Indeed, other groups have suggested that these criteria are too strict and should be expanded. Thus, the University of California—San Francisco group (Yao et al, 2002) has suggested that the indications should be expanded to include either a solitary tumor at or less than 6.5 cm diameter or three or fewer nodules, with the largest lesion at or less than 4.5 cm and a total tumor diameter at or less than 8 cm; vascular invasion would preclude transplantation. Whether indications for transplant with cadaveric donor livers should be the same as for living donated livers is controversial.
Klintmalm (1998) published the outcome of the findings of the International Registry of Hepatic Tumors in Liver Transplantation that included the outcome of 410 patients with HCC and 12 with the fibrolamellar variant. Of these patients, 40% had incidental tumors—that is, tumors detected on explantation—and 60% had a transplant for known HCC. Overall, after transplantation, 190 patients had died during follow-up, 99 (23.5%) were free of tumor, and in 91 (21.6%), tumor was the cause of death, although many who died early were presumed to be tumor free after transplantation. The 1-year survival was 72%, and 5-year survival was 44%. Univariate analysis identified four factors that predicted patient survival and poor outcome: 1) tumor size greater than 5 cm, 2) vascular invasion, 3) positive lymph nodes, and 4) histologic grade with poor differentiation.
Incidental tumors, fibrolamellar variants, and bilobar tumors were not found to correlate with outcome. When multivariate analysis was used, only histologic grade and known tumors were significantly related to survival. For incidental tumors, survival was negatively influenced by multifocality and age greater than 60 years; tumor histologic grade and size greater than 5 cm were negatively linked to tumor-free survival. Although this report gives invaluable data in selecting patients for transplantation, these findings must be interpreted with some caution, because the data come from 53 units in 21 countries, where there are differences in the etiology of the cirrhosis, in detection, and in management of patients. Many of these factors are interrelated, so a poorly differentiated HCC may be more likely to grow rapidly and metastasize early. Not all single-center experience will confirm the registry report (Rose et al, 1998), however: for example, Achkar et al (1998) found that routine screening of cirrhotic patients will detect small, early stage tumors and that such patients do well after transplantation.
Transplantation is indicated for unresectable HCCs in noncirrhotic livers with no evidence of extrahepatic spread. Although most HCC arises in cirrhotic livers, occasionally HCC may occur in the absence of underlying hepatic parenchymal cirrhosis. In such cases, transplantation is one option usually reserved for those patients in whom other forms of treatment—such as resection, chemotherapy, chemoembolization, RFA, or TACE—are not indicated, and where the characteristics of the HCC fulfill the current indications for transplantation. In those patients with cirrhosis, the decision to resect (if possible) or transplant is more uncertain, because most HCCs in this situation are usually multifocal. Transplantation may offer a survival benefit (Sarasin et al, 1998) that is also cost-effective, provided the delay from diagnosis to transplantation is less than 6 to 10 months.
The role of pretransplant therapy remains uncertain (see Chapter 83). Some centers are undertaking interventions with either RFA or TACE, but no controlled trials show that such interventions offer a survival benefit; indeed, it is not clear whether any reported benefit is derived from the intervention itself, or whether the delay will help identify those with rapidly growing tumors, those likely to be already outside the liver at the time of transplantation. As RFA and TACE will induce necrosis of the tumor, these and similar interventions may be of help when the waiting time is greater than 6 months in patients with stable liver functions (Bruix & Sherman, 2005). Evaluation involves ultrasound to look for evidence of extrahepatic spread together with CT and/or MRI scan of both the chest and the abdomen along with bone scans to exclude extrahepatic metastasis. Laparoscopy may reveal the presence of nodules ulcerating through the capsule, but it is not usually done. Tumor infiltrating the portal vein, in our view, contraindicates transplantation.
The role of liver biopsy to establish the diagnosis of HCC or assess the biologic characteristics must be considered. Because the risk of tumor seeding may be 2% to 4% along the needle biopsy tract (Navarro et al, 1998), biopsy should be considered only when there is uncertainty as to the diagnosis. This might occur, for example, in the presence of a hepatoma arising in the noncirrhotic liver. It is not usually possible to be sure whether the tumor is malignant or if it is indeed a liver primary. The clear-cell variant of HCC is often difficult to distinguish from pancreatic and renal neoplasm. In contrast, in a patient with known cirrhosis, a primary space-occupying lesion, and rapidly elevating serum α-fetoprotein (AFP) level, there can be little doubt as to the diagnosis; because percutaneous biopsy would only increase the risk of metastasis, it should be avoided.
Cholangiocarcinoma
As indicated above, cholangiocarcinoma (see Chapters 50A, 50B, and 97E) is not usually considered to be an indication for transplantation, because the recurrence rates are high; thus in a literature review, Jeyarajah and Klintmalm (1998) reported a 1-year patient survival of 53% but a 3-year disease-free survival of only 13%. Only in the incidental tumor found at laparotomy is transplantation to be considered, although cures are sometimes possible (Iwatsuki et al, 1998). Some centers have achieved excellent survival after transplantation in highly selected patients treated with an aggressive protocol of radiotherapy and chemotherapy (Hassoun et al, 2002).
Secondary Liver Cancers
With few exceptions, we feel transplantation is not indicated for metastatic liver because of the high rate of recurrence (see Chapter 97E). The major exception is carcinoid and other neuroendocrine tumors, as long-term results are good, and symptomatic relief is rapid (Makowka et al, 1989; see Chapters 81B and 97E). Of 103 patients with unresectable neuroendocrine tumors, the 5-year survival rate was 47%, although the disease-free recurrence rate was only 24% (Lehnert, 1998). In this analysis, multivariate factors that identified a better prognosis included age less than 50 years, primary location in lung or bowel, and pretransplant somatostatin therapy. Multivariate analysis showed that age greater than 50 years, upper abdominal exenteration, and Whipple procedure at the time of transplantation were all associated with a poor outcome.
Pediatric Transplantation
The medical indications for liver transplantation in children are similar to those in adults (see Chapters 40, 71, 82, and 98C), although additional indications include growth retardation and the development of metabolic bone disease. The commonest indication for transplantation in children remains disorders of the biliary system, of which biliary atresia (Chapters 40 and 98C) is the commonest. The procedure of portoenterostomy may be effective in some children if performed early, but if performed after 2 months, the chance of a successful outcome is limited; thus if bile drainage is not established soon after surgery, the child should be considered for transplantation rather than have the surgeon make further attempts to reconstruct the bile duct system in an attempt to establish bile flow. Other disorders of the biliary tree that may require transplantation include Alagille syndrome, Byler disease, and nonsyndromatic intrahepatic biliary hypoplasia. Disorders of metabolism are the next commonest indication for transplantation, and these include Wilson disease, tyrosinemia, glycogen storage disease, galactosemia, and Gaucher syndrome.
Assessment of Patients for Liver Transplantation
Cardiopulmonary function is difficult to assess. ECG, echocardiography, and simple lung function tests may be adequate to recognize pathology that requires further investigation. For example, in a patient with possible ischemic heart disease, if appropriate, we will proceed with an echocardiogram, an exercise ECG test prior to thallium scanning, and coronary angiography or other imaging as indicated. Measurement of arterial blood gases is important; if the arterial oxygen is low, these tests must be repeated after exercise and after giving 100% oxygen to gain guidance as to the extent of intrapulmonary shunting (Krowka & Cortese 1990).
Management of Patients Awaiting Transplantation
The presence of ascites may be an indication for treatment; not only do ascitic patients remain catabolic, but the risk of spontaneous bacterial peritonitis is also present. In the presence of ascites, patients should be treated with prophylactic antibiotics, such as ciprofloxacin or co-amoxiclav, which have been shown to be not only efficacious and cost-effective but also without major risk of developing bacterial resistance. In patients with severe ascites that is resistant to therapy with diet and diuretics, requiring repeated episodes of paracentesis, a TIPS may be considered (see Chapter 76E). The role of such shunts prior to transplantation remains uncertain; they have been shown to reduce portal hypertension and thereby improve ascites and the risk of variceal hemorrhage, but insertion is not without risk, not only of sepsis but also of perforation and portal vein thrombosis.
Patients with recurrent variceal hemorrhage pose a particular problem (see Chapter 75A, Chapter 75B, Chapter 75C ). Injection sclerotherapy in the 2 weeks prior to transplantation is associated with a risk of paraesophageal abscesses following transplantation. Variceal banding is preferable for the treatment of bleeding esophageal varices, and again, the role of TIPS is valuable in selected patients. If successful, TIPS procedure will reduce portal hypertension, but it is not free of risks, which include perforation and portal vein thrombosis; however, current evidence suggests that the benefits outweigh the risks. Patients with portal hypertension and varices should be considered for β-blocker therapy with propranolol or carvedilol, because this will reduce the risk of both primary and secondary hemorrhage and does not impair response to anesthesia.
Achkar JP, et al. Undetected hepatocellular carcinoma: clinical features and outcome after liver transplantation. Liver Transplant Surgery. 1998;4:477-482.
Alabraba E, et al. A re-evaluation of the risk factors for the recurrence of primary sclerosing cholangitis in liver allografts. Liver Transpl. 2009;15(3):330-340.
Arguedas MR, et al. Prospective evaluation of outcomes and predictors of mortality in patients with hepatopulmonary syndrome undergoing liver transplantation. Hepatology. 2003;37:192-197.
Belghiti J, et al. Resection prior to liver transplantation for hepatocellular carcinoma. Ann Surg. 2003;238:885-892.
Benten D, et al. Low recurrence of pre-existing extrahepatic malignancies after liver transplantation. Liver Transpl. 2008;14(6):789-798.
Beresford TP, et al. A rational approach to transplantation for the alcoholic patient. Psychosomatics. 1990;31:241-254.
Bergquist A, et al. Risk factors and clinical presentation of hepatobiliary carcinoma in patients with primary sclerosing cholangitis. Hepatology. 1998;27:311-316.
Bernuau J, et al. Multivariate analysis of prognostic factors in fulminant hepatitis B. Hepatology. 1986;6:648-651.
Bismuth U, et al. Emergency liver transplantation for fulminant hepatic failure. Ann Int Med. 1987;197:337-341.
Bruix J, Sherman M. Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208-1236.
Burdelski M, et al. The role of dynamic liver function tests in liver transplantation. In: Lentze, M, Reichen, J. Paediatric Cholestasis. Kluwer: Dordrecht; 1991:215-224.
Burroughs AK, et al. 3-month and 12-month mortality after first liver transplant in adults in Europe: predictive models for outcome. Lancet. 2006;367(9506):225-232.
Campillo B, et al. Evaluation of nutritional practice in hospitalized cirrhotic patients: results of a prospective study. Nutrition. 2003;19:515-521.
Caregaro L, et al. Malnutrition in alcoholic and virus-related cirrhosis. Am J Clin Nutr. 1996;63:602-609.
Dabos KJ, et al. Biochemical prognostic markers of outcome in non-paracetamol–induced fulminant hepatic failure. Transplantation. 2004;77(2):200-205.
Darwish Murad S, et al. Etiology, management, and outcome of the Budd-Chiari syndrome. Ann Intern Med. 2009;151(3):167-175.
Day E, et al. Predictors of psychological morbidity in liver transplant assessment candidates: is alcohol abuse or dependence a factor? Transplant Int. 2009;22(6):606-614.
Elias E, McMaster P. Liver transplantation: indications and preoperative prognostic factors. Schweiz Med Wochenschr. 1987;117:1053-1060.
Everson GT. Treatment of chronic hepatitis C in patients with decompensated cirrhosis. Rev Gastroenterol Disord. 2004;4(Suppl 1):S31-S38.
Fattovich G, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463-472.
Figueiredo F, et al. Impact of nutritional status on outcomes after liver transplantation. Transplantation. 2000;70:1347-1352.
Freeman AJ, et al. Estimating progression to cirrhosis in chronic hepatitis C virus infection. Hepatology. 2001;34:809-816.
Freeman RB, et al. Serological and DNA follow up data from HBsAg-positive patients treated with orthotopic liver transplantation. Transplantation. 1991;51:793-797.
Freeman RBJr, et al. Improving liver allocation: MELD and PELD. Am J Transplant. 2004;4(Suppl 9):114-131.
Fung J, et al. Liver transplantation in patients with HIV infection. Liver Transpl. 2004;10(Suppl 10):S39.
Gines P, et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1988;7:122-128.
Graham CS, et al. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection: a meta-analysis. Clin Infect Dis. 2001;33:562-569.
Guichelaar M, et al. Fractures and avascular necrosis before and after orthotopic liver transplantation: long-term follow-up and predictive factors. Hepatology. 2007;46(4):1198-1207.
Harrison PM, et al. Serial prothrombin time as prognostic indicator in paracetamol induced fulminant hepatic failure. Br Med J. 1990;301(6758):964-966.
Hassoun Z, Gores G, Rosen C. Preliminary experience with liver transplantation in selected patients with unresectable hilar cholangiocarcinoma. Surg Oncol Clin North Am. 2002;11:909-921.
Haydon G, Neuberger J. Liver transplantation in cirrhotic patients with diabetes mellitus. Liver Transpl. 2001;7(3):234-237.
Heimbach JK, et al. Liver transplantation for unresectable perihilar cholangiocarcinoma. Semin Liver Dis. 2004;24(2):201-207.
Hoeper MM, Krowka MJ, Strassburg CP. Portopulmonary hypertension and hepatopulmonary syndrome. Lancet. 2004;363:1461-1468.
Iwatsuki S, et al. Treatment of hilar cholangiocarcinoma (Klatskin tumors) with hepatic resection or transplantation. J Am Coll Surg. 1998;187:358-364.
Jeyarajah DR, Klintmalm GB. Is liver transplantation indicated for cholangiocarcinoma? J Hepatobiliary Pancreat Surg. 1998;5:48-51.
Keays R, et al. Intracranial and cerebral perfusion pressure changes before, during and immediately after liver transplantation for fulminant hepatic failure. Q J Med. 1991;289:335-430.
Kim WR, et al. Outcome of liver transplantation for hepatitis B in the United States. Liver Transpl. 2004;10(8):968-974.
Kingham JGC, Parker DR. The association between primary biliary cirrhosis and coeliac disease: a study of relative prevalences. Gut. 1998;42:120-122.
Klintmalm GB. Liver transplantation for hepatocellular carcinoma: a registry report of the impact of tumor characteristics on outcome. Ann Surg. 1998;228:479-490.
Krowka M, Cortese M. Hepatopulmonary syndrome. Hepatology. 1990;11:138-142.
Krowka MJ. Portopulmonary hypertension: diagnostic advances and caveats. Liver Transpl. 2003;9:1336-1337.
Krowka MJ, et al. Hepatopulmonary syndrome and portopulmonary hypertension: a report of the multicenter liver transplant database. Liver Transpl. 2004;10:174-182.
Kumar S, et al. The results of liver transplantation in 73 alcoholics with end-stage liver disease. Hepatology. 1990;11:159-164.
Lehnert T. Liver transplantation for metastatic neuroendocrine carcinoma: an analysis of 103 patients. Transplantation. 1998;66:1307-1312.
Lindor KD, et al. High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis. Hepatology. 2009;50(3):808-814.
Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50(3):661-662.
Ludwig J, LaRusso N, Wiesner R. The syndrome of primary sclerosing cholangitis. Prog Liver Dis. 1990;9:555-566.
Makowka L, et al. Transplantation of the liver for metastatic endocrine tumors of the intestine and pancreas. Surg Gynecol Obstet. 1989;168:107-111.
Mazzaferro V, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699.
McCarthy M, et al. Liver transplantation for haemophiliacs with hepatitis C cirrhosis. Gut. 1996;39:870-875.
Menon KV, Shah V, Kamath PS. The Budd-Chiari syndrome. N Engl J Med. 2004;350(6):578-585.
Mericel C, et al. Aminopyrine breath test in the prognostic evaluation of patients with cirrhosis. Gut. 1992;33:836-842.
Mitzner SR, et al. Extracorporeal support of the failing liver. Curr Opin Crit Care. 2002;8(2):171-177.
Nair S, Verma S, Thuluvath PJ. Pretransplant renal function predicts survival in patients undergoing orthotopic liver transplantation. Hepatology. 2002;35:1179-1185.
Navarro F, et al. Diaphragmatic and subcutaneous seeding of hepatocellular carcinoma following fine-needle aspiration. Liver. 1998;18:251-254.
Neuberger J. Predicting the prognosis of primary biliary cirrhosis. Gut. 1989;30:1519-1522.
Neuberger J. Allocation of donor livers—is MELD enough? Liver Transpl. 2004;10:908-910.
Neuberger J, et al. Pretransplant prediction of prognosis after liver transplantation in primary sclerosing cholangitis using a Cox regression model. Hepatology. 1999;29:1375-1379.
Neuberger J, et al. Transplantation for alcoholic liver disease. J Hepatol. 2002;36:130-137.
Neuberger J, et al. Selection of patients for liver transplantation and allocation of donated livers in the UK. Gut. 2008;57(2):252-257.
O’Grady J, et al. Early indications of prognosis in fulminant hepatic failure. Gastroenterology. 1989;97:439-445.
O’Grady J, et al. Hepatitis B virus infection after orthotopic liver transplantation. J Hepatol. 1992;14:104-111.
O’Leary JG, Davis GL. Conivaptan increases serum sodium in hyponatremic patients with end-stage liver disease. Liver Transpl. 2009;15(10):1325-1329.
Olthoff KM, et al. Summary report of a national conference: evolving concepts in liver allocation in the MELD and PELD era. Liver Transpl. 2004;Suppl 10:A6.
Ostapowicz GA, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:945-954.
Peleman R, et al. Orthotopic liver transplantation for acute and subacute hepatic failure in adults. Hepatology. 1987;7:484-489.
Penn I. The effect of immunosuppression on pre-existing cancers. Transplantation. 1993;55:742-747.
Piche T, et al. Effect of ondansetron, a 5-HT3 receptor antagonist, on fatigue in chronic hepatitis C: a randomized, double-blind, placebo-controlled study. Gut. 2005;54:1169-1173.
Qin XL, et al. Utility of serum CA19-9 in diagnosis of cholangiocarcinoma: in comparison with CEA. World J Gastroenterol. 2004;10(3):427-432.
Rimola A, et al. Effects of renal impairment on liver transplantation. Gastroenterology. 1987;93:148-156.
Ringe B, et al. Total hepatectomy and liver transplantation as two-stage procedure. Ann Surg. 1993;218(1):3-9.
Riordan SM, Williams R. Blood lactate and outcome of paracetamol-induced acute liver failure. Lancet. 2002;360:573.
Rizetto M, Recehia S, Salizzoni M. Liver transplantation in carriers of HBsAg. J Hepatology. 1991;13:5-7.
Roland ME, Stock PG. Liver transplantation in HIV-infected recipients. Semin Liver Dis. 2006;26(3):273-284.
Rubin RH, et al. The acquired immunodeficiency syndrome and transplantation. Transplantation. 1987;44:1A.
Saigal S, et al. Successful outcome of orthotopic liver transplantation in patients with preexisting malignant states. Liver Transpl. 2001;7(1):11-15.
Sala M, Varela M, Bruix J. Selection of candidates with HCC for transplantation in the MELD era. Liver Transplant. 2004;10(Supp l):S4.
Samuel D, et al. Liver transplantation in patients with HIV infection. J Hepatol. 2003;39(1):3-6.
Sarasin FP, et al. Partial hepatectomy or orthotopic liver transplantation for the treatment of resectable hepatoma? A cost-effectiveness perspective. Hepatology. 1998;28:436-442.
Shapiro J, Smith H, Schaffner F. Serum bilirubin: a prognostic factor in primary biliary cirrhosis. Gut. 1979;20:139-140.
Shetty K, Rybicki L, Carey WD. The Child-Pugh classification as a prognostic indicator for survival in primary sclerosing cholangitis. Hepatology. 1997;25:1049-1053.
Soterakis J, Resnick R, Iber F. Effect of alcohol abstinence in survival in cirrhotic portal hypertension. Lancet. 1973;ii:65-67.
Starzl TE, et al. Orthotopic liver transplantation for alcoholic cirrhosis. JAMA. 1988;260:2542-2544.
Tiukinhoy-Laing SD, et al. Cardiac hemodynamic and coronary angiographic characteristics of patients being evaluated for liver transplantation. Am J Cardiol. 2006;98:178-181.
Veldt BJ, et al. Indication of liver transplantation in severe alcoholic liver cirrhosis: quantitative evaluation and optimal timing. J Hepatol. 2002;36:93-98.
Volk ML, et al. Modified Charlson comorbidity index for predicting survival after liver transplantation. Liver Transpl. 2007;13:1515.
Wiesner RH, et al. Liver transplantation for primary sclerosing cholangitis: impact of risk factors on outcome. Liver Transplant Surg. 1996;2(Suppl 1):99-108.
Yao FY, et al. Liver transplantation for hepatocellular carcinoma: comparison of the proposed UCSF criteria with the Milan crieria and the Pittsburgh modified TNM criteria. Liver Transpl. 2002;8:765-774.
Yun BC, et al. Impact of pretransplant hyponatremia on outcome following liver transplantation. Hepatology. 2009;49(5):1610-1615.