15 Intramuscular manual therapy: Dry needling
Introduction
Intramuscular manual therapy or dry needling, as it is more commonly known, is a relatively new intervention in the treatment of patients diagnosed with myofascial pain and myofascial trigger points. In the US, the American Physical Therapy Association has suggested that the term ‘intramuscular manual therapy’ is the preferred term to be used when physical therapists employ dry needling techniques, while physical therapists in Spain have recommended the term ‘invasive physical therapy’ (Mayoral del Moral 2005). Since dry needling is within the scope of practice of multiple disciplines, including medicine, physical therapy, chiropractic and acupuncture, the terminology used may vary between disciplines. It is important to note that dry needling is just a technique, which does not define or represent any particular profession or discipline. Comprehensive dry needling techniques are rarely covered in entry-level educational programmes and post-graduate training is generally indicated. In medical practice, the term trigger point needling is commonly used, but in many jurisdictions physicians appear to prefer trigger point injections (Peng & Castano 2005). A few States in the US, including Maryland, have ruled that dry needling is within the scope of chiropractic practice. Acupuncturists are qualified to use dry needling techniques but, as with other disciplines, acupuncture training programmes rarely include specific education about trigger point management (Dommerholt et al. 2006b).
Acupuncture
There is controversy about the possible correspondences between the location of acupuncture points and the location of trigger points. The traditional concept of acupuncture is based on a mixture of natural laws, metaphysical beliefs, and the practice of bloodletting, and the specific body points in Chinese medicine have similarities with points traditionally used in Ayurvedic and Arabic mediaeval medicine. The original 365 classical acupuncture points and meridians were based on the cosmological relationship between the number of points and the days of the year, and the sun’s annual journey across the celestial sphere. Nevertheless, there are close resemblances between ancient acupuncture point maps and maps for blood-letting (Unschuld 1987, 1999, Pas, 1998, Whorton, 2004, Kavoussi 2009).
Throughout the centuries, the number of points used in the various schools and traditions of acupuncture has increased to over 2500, with all schools claiming therapeutic efficacy (Ma et al. 2005). Yet, the existence of acupuncture points and meridians has never been confirmed scientifically, in spite of numerous histological, biochemical, imaging, philosophical and electrical studies (Liu et al. 1975, Rabischong et al. 1975, Bossy 1984, Ramey 2000, Langevin & Yandow 2002, Dorsher 2009, Dorsher & Fleckenstein 2009). Mann, co-founder of the British Medical Acupuncture Society, concluded that acupuncture points simply do not exist. Instead of focusing on acupuncture points, he recommended to either needle anywhere on the body, needle in the dysfunctional quadrant, needle in a neighbouring dermatome, myotome or sclerotome, needle in a small circumscript area near the location of pain, or needle trigger points, in order of increasing specificity (Mann 2000).
With regard to trigger points, there is also no evidence or even any indication that they have defined anatomical locations. The locations of trigger points, initially reported by Travell, have been duplicated by many; however, Travell never suggested that trigger points would be limited to these locations or that these locations would somehow be absolute (Travell & Rinzler 1952, Travell & Simons 1992, Simons et al. 1999). Several authors have suggested that trigger points are comparable to so-called ashi points in traditional Chinese acupuncture or kori in Japanese acupuncture (Hong 2000, Audette & Blinder 2003, Cardinal 2004, Campbell 2006, Amaro 2007, Seem, 2007). Ashi points are defined as points where the patient expresses pain and discomfort in response to pressure. Kori is defined as a tight myofascial constriction that may or may not elicit discomfort with palpation, but which can be felt by the practitioner. In the acupuncture nomenclature, ashi points or kori are not located on the traditional meridians or channels. Others suggested that trigger point dry needling is similar to treating musculotendinous meridian points (Amaro 2007, Seem 2007). Even if topographical correspondences could be confirmed, considering the metaphysical origin of acupuncture points, and the lack of distinct anatomical locations of acupuncture points and trigger points, there is no reason to believe that such assumed correspondences would have any meaningful relevancy or alter the clinical management of patients with myofascial pain. Dry needling does not require any knowledge of traditional acupuncture theory or Chinese medicine (White 2009).
Trigger points
Trigger point therapy is particularly suited to improve abnormal pain processing (Dommerholt 2005, Dommerholt et al. 2006a). Individuals with myofascial trigger points were found to have abnormal central processing with enhanced brain activity in somatosensory and limbic regions, suppressed activity in the hippocampus, and hyperalgesia in response to electrical stimulation and compression of the trigger point (Niddam et al. 2007, 2008). There is increasing evidence that trigger points contribute to the development of central sensitization and as such may cause or contribute to various pain syndromes (Fernández de las Peñas et al. 2007, 2009, Giamberardino et al. 2007, Cuadrado et al. 2008). Muscle nociceptors are more effective at inducing neuroplastic changes in wide-dynamic-range dorsal horn neurons than cutaneous receptors (Wall & Woolf 1984).
Inactivating trigger points with a needle requires an excellent kinesthetic sense and awareness, based on training, experience and anatomical knowledge. The clinician must know the exact location of the tip of the needle to assure that needling procedures are safe. Experienced clinicians will be able to appreciate changes in structures and accurately identify skin, the subcutaneous connective tissue and fascial layers, the muscle, and ultimately the taut band and trigger point with a needle (Dommerholt et al. 2006b). Invasive trigger point therapies can be divided into dry needling and injections. Dry needling can be divided into superficial and deep dry needling techniques (Dommerholt et al. 2006b). Superficial dry needling techniques are performed over a trigger point without aiming to elicit local twitch responses (Baldry 2002).
Injections are administered with a hypodermic syringe; dry needling is administered with a solid filament needle. Injections are performed with either an anaesthetic, such as procaine, lidocaine, mepivacaine, bupivacaine, levobupivacaine, or ropivacaine, botulinum toxin, or serotonin antagonists, including tropisetron (Travell et al. 1942, Müller & Stratz 2004, Göbel et al. 2006, Zaralidou et al. 2007, Garcia-Leiva et al. 2007). When using lidocaine, the recommendation is to use a 0.25% lidocaine solution, which was found to be more effective than stronger solutions (Iwama & Akama 2000, Iwama et al. 2001). Stronger concentrations of 0.5%, 1%, or even 2% solutions are frequently reported (Carlson et al. 1993, Hong 1994, Kamanli et al. 2005, Peng & Castano 2005). There is no evidence of any advantage of administering injections with vitamin B12, non-steroidal anti-inflammatories or steroids (Dommerholt & Gerwin 2010). Although there are no trigger point studies, there are some indications that injections with bee venom may be beneficial, as bee venom has an anti-nociceptive and anti-inflammatory effect through activation of brainstem catecholaminergic neurons and activation of the α2-adrenergic and serotonergic pathways of the descending inhibitory system (Kwon et al. 2001a, 2001b, Kim et al. 2005).
Sham needling
It is very difficult, if not impossible, to perform studies with sham needling procedures and create meaningful control groups. Any needling will have a physiological effect, including a release of endorphins, a change in pain thresholds, or an expectancy of a positive outcome. Therefore, studies comparing needling with sham needling may actually compare active treatment regimens with little value for clinical practice (Pariente et al. 2005, Birch 2006, Lund & Lundeberg 2006, Wang et al. 2008, Lund et al. 2009, Lundeberg et al. 2009). In some studies, sham needling is attempted by tapping a von Frey monofilament on the skin. However, both needling and tapping induce specific but different brain responses. Needling procedures can trigger strong placebo responses (Wager et al. 2004, Bausell et al. 2005, Pariente et al. 2005, Kong et al. 2009). Even light touch of the skin can stimulate mechanoreceptors coupled to slow conducting unmyelinated C-fibre afferents, and activate the insular region (Olausson et al. 2002). White and Cummings suggested discontinuing the use of sham needling procedures, and instead to compare the clinical efficacy of invasive procedures with other interventions using standardized outcome measures (White & Cummings 2009).
Evidence of intramuscular manual therapy
Although recent meta-reviews of acupuncture, dry needling and trigger point injections in the management of myofascial trigger points showed only limited evidence (Garvey et al. 1989, Berman et al. 1999, Ezzo et al. 2000, Cummings & White, 2001, Scott et al. 2009, Tough et al. 2009), there are several studies that offer support for including dry needling in the treatment of individuals with low back and pelvic pain (Furlan et al. 2005). Meta-reviews often conclude that there is a lack of high-quality studies, and they tend to be limited in their scope and conclusions, partly because only double-blind randomized controlled studies are included even though in the context of evidence-based medicine multiple levels of evidence are recognized. An authoritative Cochrane meta-review concluded that dry needling is a potentially useful adjunct in the treatment of individuals with chronic low back pain, although the researchers agreed that more high-quality studies are needed (Furlan et al. 2005). Two studies compared trigger point injections with dry needling using hypodermic needles in both interventions and concluded that dry needling with a syringe caused more post-needling soreness (Hong 1994, Kamanli et al. 2005). A more recent study looked at trigger point injections in comparison with dry needling using a solid filament needle. This study showed that the effectiveness of trigger point injections is comparable to intramuscular manual therapy but the dry needling procedures had a longer-lasting effect (Ga et al. 2007).
Shah and colleagues observed that the abnormal concentrations of especially substance P and calcitonin gene-related peptide in the immediate region of active trigger points decreased significantly after eliciting a local twitch response with a needle, suggesting that the effects of trigger point dry needling are at least partially due to the reduction of nociceptive input into muscle receptors (Shah et al. 2005, 2008). The positive effects of dry needling are also related to the reduction of endplate noise (Chen et al. 2001), which is the summation of miniature endplate potentials found in myofascial trigger points (Hong & Simons 1998, Simons 2004). Eliciting local twitch responses by dry needling reduced the endplate noise associated with trigger points in rabbits (Chen et al. 2001). The prevalence of endplate noise in a trigger point region has been correlated with the pain intensity of that trigger point (Kuan et al. 2007).
As described in Chapters 9, 11, 12, 13 and 14, many studies, reviews and case reports have confirmed a correlation between trigger points and chronic pelvic pain. The European Association of Urology and the Society of Obstetricians and Gynaecologists of Canada recommended that trigger points be considered in the diagnosis of chronic pelvic pain (Jarrell et al. 2005, Fall et al. 2009). There is, however, no evidence for the often assumed pain–spasm–pain cycle, which suggests that pain would lead to muscle spasms, which in turn would increase pain. Quite the contrary, muscle pain is more likely to inhibit the contractile activity of muscles (Mense & Simons 2001).
Few studies have explored the effects of needling therapies in patients with these diagnoses. As a general rule, needling therapies increase the specificity of the stimulus. Several papers explored the use of acupuncture and electro-acupuncture for patients with endometriosis, vulvodynia, piriformis syndrome, prostatitis, urinary tract infections and constipation, among others (Aune et al. 1998, Powell & Wojnarowska 1999, Wang 2001, Chen & Nickel, 2004, Spiller 2007, Lee et al. 2008, Lundeberg & Lund 2008, Wayne et al. 2008, Han et al. 2009, Lee & Lee 2009). Abdominal trigger point injections were very effective in the treatment of myofascial pain (Kuan et al. 2006) and the efficacy of superficial dry needling was confirmed in a randomized study of subjects with chronic lumbar trigger points (Macdonald et al. 1983). Giamberardino and colleagues established that patients with visceral referred pain and hyperalgesia are likely to have clinically relevant abdominal trigger points (Giamberardino et al. 1999).
Nearly 90% of women with pelvic pain, interstitial cystitis or incontinence have painful trigger points in the pelvic floor muscles, abdominal and gluteal muscles (Weiss 2001, FitzGerald & Kotarinos 2003). The International Continence Society and European Association of Urology suggested that pelvic pain can be divided into pelvic pain of muscular origin and pelvic floor muscle pain syndrome (Abrams et al. 2003, Fall et al. 2009); however, trigger points in the abdominal, gluteal, obturator internus, piriformis, psoas, iliacus, quadratus lumborum and lumbar multifidi muscles frequently refer pain to the pelvic floor, perineum, vagina, labia, clitoris, scrotum and penis (Segura et al. 1979, King Baker 1993, Zermann et al. 1999, King & Goddard 1994, Doggweiler-Wiygul & Wiygul 2002, Prendergast & Weiss 2003, Doggweiler-Wiygul 2004). Empirical data suggest that pain and trigger points in the perineal or lower abdominal region can be treated successfully by inactivating the more remote trigger points which frequently is the first step in reducing pain levels. Inactivation of trigger points in the perineal muscles, such as the bulbospongiosus and ischiocavernosus muscles, is not commonly indicated after trigger points in the low back, gluteal and abdominal regions have been inactivated. Langford and colleagues described intravaginal trigger point injection techniques for the levator ani muscles using an Iowa trumpet pudendal needle guide (Langford et al. 2007). Thirty percent of the subjects were completely pain-free following the injection. Thirteen out of 18 subjects reported significant improvement (Langford et al. 2007).
It seems reasonable to consider dry needling studies in other regions of the body, but some caution is warranted in applying the findings of these studies to the pelvic area. Dry needling of trigger points in the infraspinatus muscle decreased the pain intensity of the shoulder, increased active and passive shoulder internal rotation, and increased the pressure pain threshold of myofascial trigger points in the ipsilateral anterior deltoid and extensor carpi radialis longus muscles (Hsieh et al. 2007). A recent study by Anderson and colleagues offers support for first treating muscles that refer pain and other paraesthesia into the pelvic area (Anderson et al. 2009), but fascial releases of the vaginal and perineal areas may still be indicated (FitzGerald & Kotarinos 2003). In reverse, it is also conceivable that treatment of trigger points in the perineal region may have an impact on trigger points outside the perineal region, which means that clinicians should not become too dogmatic in the order of treatment. Dry needling of trigger points in the extensor carpi radialis longus reduced the irritability of trigger points in the ipsilateral trapezius muscle, the overall pain intensity and improved range of motion (Tsai et al. 2009).
Trigger point dry needling and stretching restored normal muscle activation patterns in a study of the effects of latent trigger points on muscle activation patterns in the shoulder region (Lucas et al. 2004). After only four dry needling treatments of patients with shoulder pain following a cerebrovascular accident, patients reported significantly less frequent and less intense pain, had more restful sleep, decreased the use of analgesic medications, and increased compliance with the rehabilitation programme compared to patients who received the regular rehabilitation programme (Dilorenzo et al. 2004). Another randomized prospective study concluded that the combination of dry needling and stretching was more effective than stretching only or no treatment (Edwards & Knowles 2003). A multicentre study of the feasibility to conduct myofascial pain studies confirmed that trigger point therapy is effective in chronic pelvic pain syndromes (FitzGerald et al. 2009).
General guidelines
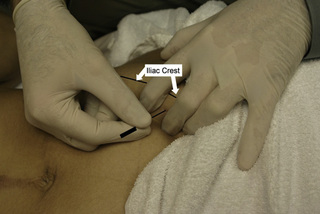
To reduce the risk of vasodepressive syncope, patients are lying down during any needling procedures. Anatomical landmarks must be identified before any needling procedures. After the needle is tapped into the skin, it is moved in and out of the region of the trigger point to elicit so-called local twitch responses (Hong 1994). Following needling procedures, haemostasis must be accomplished to prevent or minimize local bleeding, help restore and maintain range of motion, and facilitate a return to normal function. It is recommended to apply ice or heat following the treatment for patient comfort and to reduce the risk of haematoma.
Low back and hip muscles
Semispinalis/multifidus/rotatory muscle (deep) (Figures 15.3 and 15.4)
Adductor muscles
Abdominal muscles
External oblique, internal oblique, transverse abdominus, rectus abdominis muscles (Figure 15.13) 
Hip flexors
Pelvic floor (perineal) muscles
Abrams P., Cardozo L., Fall M., Griffiths D., Rosier P., Ulmsten U., et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61:37-49.
Amaro J.A. When acupuncture becomes “dry needling”. Acupuncture Today. 2007.
Anderson R.U., Sawyer T., Wise D., Morey A., Nathanson B.H. Painful myofascial trigger points and pain sites in men with chronic prostatitis/chronic pelvic pain syndrome. J. Urol.. 2009;182:2753-2758.
Audette J.F., Blinder R.A. Acupuncture in the management of myofascial pain and headache. Curr. Pain Headache Rep.. 2003;7:395-401.
Aune A., Alraek T., Lihua H., Baerheim A. Acupuncture in the prophylaxis of recurrent lower urinary tract infection in adult women. Scand. J. Prim. Health Care. 1998;16:37-39.
Baldry P. Superficial versus deep dry needling. Acupunct. Med.. 2002;20:78-81.
Bausell R.B., Lao L., Bergman S., Lee W.L., Berman B.M. Is acupuncture analgesia an expectancy effect? Preliminary evidence based on participants’ perceived assignments in two placebo-controlled trials. Eval. Health Prof.. 2005;28:9-26.
Berman B.M., Ezzo J., Hadhazy V., Swyers J.P. Is acupuncture effective in the treatment of fibromyalgia? J. Fam. Pract.. 1999;48:213-218.
Birch S. A review and analysis of placebo treatments, placebo effects, and placebo controls in trials of medical procedures when sham is not inert. J. Altern. Complement. Med.. 2006;12:303-310.
Bossy J. Morphological data concerning the acupuncture points and channel network. Acupunct. Electrother. Res.. 1984;9:79-106.
Campbell A. Point specificity of acupuncture in the light of recent clinical and imaging studies. Acupunct. Med.. 2006;24:118-122.
Cardinal S. Points détente et acupuncture: approche neurophysiologique. Montreal: Centre Collégial de Développement de Matériel Didactique, 2004.
Carlson C.R., Okeson J.P., Falace D.A., Nitz A.J., Lindroth J.E. Reduction of pain and EMG activity in the masseter region by trapezius trigger point injection. Pain. 1993;55:397-400.
Chen J.T., Chung K.C., Hou C.R., Kuan T.S., Chen S.M., Hong C.Z. Inhibitory effect of dry needling on the spontaneous electrical activity recorded from myofascial trigger spots of rabbit skeletal muscle. Am. J. Phys. Med. Rehabil.. 2001;80:729-735.
Chen R.C., Nickel J.C. Acupuncture for chronic prostatitis/chronic pelvic pain syndrome. Curr. Urol. Rep.. 2004;5:305-308.
Cuadrado M.L., Young W.B., Fernandez-De-Las-Penas C., Arias J.A., Pareja J.A. Migrainous corpalgia: body pain and allodynia associated with migraine attacks. Cephalalgia. 2008;28:87-91.
Cummings T.M., White A.R. Needling therapies in the management of myofascial trigger point pain: a systematic review. Arch. Phys. Med. Rehabil.. 2001;82:986-992.
Dilorenzo L., Traballesi M., Morelli D., Pompa A., Brunelli S., Buzzi M.G., et al. Hemiparetic shoulder pain syndrome treated with deep dry needling during early rehabilitation: a prospective, open-label, randomized investigation. J. Musculoskeletal Pain. 2004;12:25-34.
Doggweiler-Wiygul R. Urologic myofascial pain syndromes. Curr. Pain Headache Rep.. 2004;8:445-451.
Doggweiler-Wiygul R., Wiygul J.P. Interstitial cystitis, pelvic pain, and the relationship to myofascial pain and dysfunction: a report on four patients. World J. Urol.. 2002;20:310-314.
Dommerholt J. Persistent myalgia following whiplash. Curr. Pain Headache Rep.. 2005;9:326-330.
Dommerholt J., Gerwin R.D. Neurophysiological effects of trigger point needling therapies. In: Fernández De Las Peñas C., Arendt-Nielsen L., Gerwin R.D., editors. Diagnosis and management of tension type and cervicogenic headache. Boston: Jones & Bartlett, 2010.
Dommerholt J., Bron C., Franssen J.L.M. Myofascial trigger points; an evidence-informed review. J. Man. Manip. Ther.. 2006;14:203-221.
Dommerholt J., Mayoral O., Gröbli C. Trigger point dry needling. J. Man. Manip. Ther.. 2006;14:E70-E87.
Dorsher P.T. Myofascial referred-pain data provide physiologic evidence of acupuncture meridians. J. Pain. 2009;10:723-731.
Dorsher P.T., Fleckenstein J. Trigger points and classical acupuncture points part 3: Relationships of myofascial referred pain patterns to acupuncture meridians. Dt. Ztschr. Akup.. 2009;52:10-14.
Edwards J., Knowles N. Superficial dry needling and active stretching in the treatment of myofascial pain: a randomised controlled trial. Acupunct. Med.. 2003;21:80-86.
Ezzo J., Berman B., Hadhazy V.A., Jadad A.R., Lao L., Singh B.B. Is acupuncture effective for the treatment of chronic pain? A systematic review. Pain. 2000;86:217-225.
Fall M., Baranowski A.P., Elneil S., Engeler D., Hughes J., Messelink E.J., et al. EAU Guidelines on Chronic Pelvic Pain. Eur. Urol. 2009.
Fernández De Las Peñas C., Cuadrado M., Arendt-Nielsen L., Simons D., Pareja J. Myofascial trigger points and sensitization: an updated pain model for tension-type headache. Cephalalgia. 2007;27:383-393.
Fernández De Las Peñas C., Galán Del Rio F., Fernández Carnero J., Pesquera J., Arendt-Nielsen L., Svensson P. Bilateral widespread mechanical pain sensitivity in women with myofascial temporomandibular disorder: evidence of impairment in central nociceptive processing. J. Pain. 2009;10:1170-1178.
Fitzgerald M.P., Kotarinos R. Rehabilitation of the short pelvic floor. II: Treatment of the patient with the short pelvic floor. Int. Urogynecol. J. Pelvic Floor Dysfunct.. 2003;14:269-275. discussion 275
Fitzgerald M.P., Anderson R.U., Potts J., Payne C.K., Peters K.M., Clemens J.Q., et al. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J. Urol.. 2009;182:570-580.
Furlan A., Tulder M., Cherkin D., Tsukayama H., Lao L., Koes B., et al. Acupuncture and dry-needling for low back pain: an updated systematic review within the framework of the Cochrane Collaboration. Spine. 2005;30:944-963.
Ga H., Koh H.J., Choi J.H., Kim C.H. Intramuscular and nerve root stimulation vs lidocaine injection to trigger points in myofascial pain syndrome. J. Rehabil. Med.. 2007;39:374-378.
Garcia-Leiva J.M., Hidalgo J., Rico-Villademoros F., Moreno V., Calandre E.P. Effectiveness of ropivacaine trigger points inactivation in the prophylactic management of patients with severe migraine. Pain Med.. 2007;8:65-70.
Garvey T.A., Marks M.R., Wiesel S.W. A prospective, randomized, double-blind evaluation of trigger-point injection therapy for low-back pain. Spine. 1989;14:962-964.
Giamberardino M.A., Affaitati G., Iezzi S., Vecchiet L. Referred muscle pain and hyperalgesia from viscera. J. Musculoskeletal Pain. 1999;7:61-69.
Giamberardino M.A., Tafuri E., Savini A., Fabrizio A., Affaitati G., Lerza R., et al. Contribution of myofascial trigger points to migraine symptoms. J. Pain. 2007;8:869-878.
Göbel H., Heinze A., Reichel G., Hefter H., Benecke R. Efficacy and safety of a single botulinum type A toxin complex treatment (Dysport) for the relief of upper back myofascial pain syndrome: results from a randomized double-blind placebo-controlled multicentre study. Pain. 2006;125:82-88.
Han Y.F., Hou L.H., Zhou Y.J., Wu X.K. A survey of TCM treatment for endometriosis. J. Tradit. Chin. Med.. 2009;29:64-70.
Hong C.Z. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am. J. Phys. Med. Rehabil.. 1994;73:256-263.
Hong C.Z. Myofascial trigger points: pathophysiology and correlation with acupuncture points. Acupunct. Med.. 2000;18:41-47.
Hong C.Z., Simons D.G. Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Arch. Phys. Med. Rehabil.. 1998;79:863-872.
Hsieh Y.L., Kao M.J., Kuan T.S., Chen S.M., Chen J.T., Hong C.Z. Dry needling to a key myofascial trigger point may reduce the irritability of satellite MTrPs. Am. J. Phys. Med. Rehabil.. 2007;86:397-403.
Iwama H., Akama Y. The superiority of water-diluted 0.25% to near 1% lidocaine for trigger-point injections in myofascial pain syndrome: a prospective, randomized, double-blinded trial. Anesth. Analg.. 2000;91:408-409.
Iwama H., Ohmori S., Kaneko T., Watanabe K. Water-diluted local anesthetic for trigger-point injection in chronic myofascial pain syndrome: evaluation of types of local anesthetic and concentrations in water. Reg. Anesth. Pain Med.. 2001;26:333-336.
Jarrell J.F., Vilos G.A., Allaire C., Burgess S., Fortin C., Gerwin R., et al. Consensus guidelines for the management of chronic pelvic pain. J. Obstet. Gynaecol. Can.. 2005;27:781-826.
Kamanli A., Kaya A., Ardicoglu O., Ozgocmen S., Zengin F.O., Bayik Y. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol. Int.. 2005;25:604-611.
Kavoussi B. The untold story of acupuncture. Focus Altern. Compliment. Ther.. 2009. in press
Kim H.W., Kwon Y.B., Han H.J., Yang I.S., Beitz A.J., Lee J.H. Antinociceptive mechanisms associated with diluted bee venom acupuncture (apipuncture) in the rat formalin test: involvement of descending adrenergic and serotonergic pathways. Pharmacol. Res.. 2005;51:183-188.
King Baker P. Musculoskeletal origins of chronic pelvic pain; diagnosis and treatment. In: Contemporary Management of Chronic Pelvic Pain. Philadelphia: W.B. Saunders Company; 1993.
King J.C., Goddard M.J. Pain rehabilitation. 2. Chronic pain syndrome and myofascial pain. Arch. Phys. Med. Rehabil.. 1994;75:S9-S14.
Kong J., Kaptchuk T.J., Polich G., Kirsch I., Vangel M., Zyloney C., et al. An fMRI study on the interaction and dissociation between expectation of pain relief and acupuncture treatment. Neuroimage. 2009;47:1066-1076.
Kuan L.C., Li Y.T., Chen F.M., Tseng C.J., Wu S.F., Kuo T.C. Efficacy of treating abdominal wall pain by local injection. Taiwan J. Obstet. Gynecol.. 2006;45:239-243.
Kuan T.S., Hsieh Y.L., Chen S.M., Chen J.T., Yen W.C., Hong C.Z. The myofascial trigger point region: correlation between the degree of irritability and the prevalence of endplate noise. Am. J. Phys. Med. Rehabil.. 2007;86:183-189.
Kwon Y.B., Kim J.H., Yoon J.H., Lee J.D., Han H.J., Mar W.C., et al. The analgesic efficacy of bee venom acupuncture for knee osteoarthritis: a comparative study with needle acupuncture. Am. J. Chin. Med.. 2001;29:187-199.
Kwon Y.B., Lee J.D., Lee H.J., Han H.J., Mar W.C., Kang S.K., et al. Bee venom injection into an acupuncture point reduces arthritis associated edema and nociceptive responses. Pain. 2001;90:271-280.
Langevin H.M., Yandow J.A. Relationship of acupuncture points and meridians to connective tissue planes. Anat. Rec.. 2002;269:257-265.
Langford C.F., Udvari Nagy S., Ghoniem G.M. Levator ani trigger point injections: An underutilized treatment for chronic pelvic pain. Neurourol. Urodyn.. 2007;26:59-62.
Lee S.H., Lee B.C. Electroacupuncture relieves pain in men with chronic prostatitis/chronic pelvic pain syndrome: three-arm randomized trial. Urology. 2009;73:1036-1041.
Lee S.W., Liong M.L., Yuen K.H., Leong W.S., Chee C., Cheah P.Y., et al. Acupuncture versus sham acupuncture for chronic prostatitis/chronic pelvic pain. Am. J. Med.. 2008;121(79):e1-e7.
Liu Y.K., Varela M., Oswald R. The correspondence between some motor points and acupuncture. Am. J. Chin. Med.. 1975;3:347-358.
Lucas K.R., Polus B.I., Rich P.S. Latent myofascial trigger points: their effect on muscle activation and movement efficiency. J. Bodyw. Mov. Ther.. 2004;8:160-166.
Lund I., Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct. Med.. 2006;24:13-15.
Lund I., Naslund J., Lundeberg T. Minimal acupuncture is not a valid placebo control in randomised controlled trials of acupuncture: a physiologist’s perspective. Chin. Med.. 2009;4:1.
Lundeberg T., Lund I. Is there a role for acupuncture in endometriosis pain, or ’endometrialgia’? Acupunct. Med.. 2008;26:94-110.
Lundeberg T., Lund I., Sing A., Naslund J. Is placebo acupuncture what it is intended to be? Evidence Based Complement. Altern. Med. 2009.
Macdonald A.J., Macrae K.D., Master B.R., Rubin A.P. Superficial acupuncture in the relief of chronic low back pain. Ann. R. Coll. Surg. Engl.. 1983;65:44-46.
Mann F. Non-existent acupuncture points. Reinventing Acupuncture. second ed. Oxford: Butterworth-Heinemann; 2000.
Mayoral Del Moral O. Fisioterapia invasiva del síndrome de dolor miofascial. Fisioterapia. 2005;27:69-75.
Ma Y.T., Ma M., Cho Z.H. Biomedical acupuncture for pain management; an integrative approach. St. Louis: Elsevier, 2005.
Mense S., Simons D.G. Muscle pain; understanding its nature, diagnosis, and treatment. Philadephia: Lippincott Williams & Wilkins, 2001.
Müller W., Stratz T. Local treatment of tendinopathies and myofascial pain syndromes with the 5-HT3 receptor antagonist tropisetron. Scand. J. Rheumatol.. 2004(Suppl.):44-48.
Niddam D.M., Chan R.C., Lee S.H., Yeh T.C., Hsieh J.C. Central modulation of pain evoked from myofascial trigger point. Clin. J. Pain. 2007;23:440-448.
Niddam D.M., Chan R.C., Lee S.H., Yeh T.C., Hsieh J.C. Central representation of hyperalgesia from myofascial trigger point. Neuroimage. 2008;39:1299-1306.
Olausson H., Lamarre Y., Backlund H., Morin C., Wallin B.G., Starck G., et al. Unmyelinated tactile afferents signal touch and project to insular cortex. Nat. Neurosci.. 2002;5:900-904.
Pariente J., White P., Frackowiak R.S., Lewith G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage. 2005;25:1161-1167.
Pas J.F. Historical dictionary of Taoism. Lanham: Rowman & Littlefield Publishing Group, 1998.
Peng P.W., Castano E.D. Survey of chronic pain practice by anesthesiologists in Canada. Can. J. Anaesth.. 2005;52:383-389.
Powell J., Wojnarowska F. Acupuncture for vulvodynia. J. R. Soc. Med.. 1999;92:579-581.
Prendergast S.A., Weiss J.M. Screening for musculoskeletal causes of pelvic pain. Clin. Obstet. Gynecol.. 2003;46:773-782.
Rabischong P., Niboyet J.E., Terral C., Senelar R., Casez R. Bases experimentales de l’analgesie acupuncturale. Nouv. Presse Med.. 1975;4:2021-2026.
Ramey D.W. A review of the evidence for the existence of acupuncture points and meridians. AAEP Proc.. 2000;46:220-224.
Scott N.A., Guo B., Barton P.M., Gerwin R.D. Trigger point injections for chronic non-malignant musculoskeletal pain: a systematic review. Pain Med.. 2009;10:54-69.
Seem M. A new American acupuncture; acupuncture osteopathy. Boulder: Blue Poppy Press, 2007.
Segura J.W., Opitz J.L., Greene L.F. Prostatosis, prostatitis or pelvic floor tension myalgia? J. Urol.. 1979;122:168-169.
Shah J.P., Phillips T.M., Danoff J.V., Gerber L.H. An in-vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J. Appl. Physiol.. 2005;99:1977-1984.
Shah J.P., Danoff J.V., Desai M.J., Parikh S., Nakamura L.Y., Phillips T.M., et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch. Phys. Med. Rehabil.. 2008;89:16-23.
Simons D.G. Review of enigmatic MTrPs as a common cause of enigmatic musculoskeletal pain and dysfunction. J. Electromyogr. Kinesiol.. 2004;14:95-107.
Simons D.G., Travell J.G., Simons L.S. Travell and Simons’ myofascial pain and dysfunction; the trigger point manual. Baltimore: Williams & Wilkins, 1999.
Spiller J. Acupuncture, ketamine and piriformis syndrome: a case report from palliative care. Acupunct. Med.. 2007;25:109-112.
Tough E.A., White A.R., Cummings T.M., Richards S.H., Campbell J.L. Acupuncture and dry needling in the management of myofascial trigger point pain: A systematic review and meta-analysis of randomised controlled trials. Eur. J. Pain. 2009;13:3-10.
Travell J., Rinzler S.H. The myofascial genesis of pain. Postgrad. Med.. 1952;11:425-434.
Travell J.G., Simons D.G. Myofascial pain and dysfunction: the trigger point manual. Baltimore: Williams & Wilkins, 1992.
Travell J., Rinzler S.H., Herman M. Pain and disability of the shoulder and arm: Treatment by intramuscular infiltration with procaine hydrochloride. J. Am. Med. Assoc.. 1942;120:417-422.
Tsai C.T., Hsieh L.F., Kuan T.S., Kao M.J., Chou L.W., Hong C.Z. Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am. J. Phys. Med. Rehabil.. 2009. in press
Unschuld P.U. Traditional Chinese medicine: some historical and epistemological reflections. Soc. Sci. Med.. 1987;24:1023-1029.
Unschuld P.U. The past 1000 years of Chinese medicine. Lancet. 1999;354(Suppl.):SIV9.
Wager T.D., Rilling J.K., Smith E.E., et al. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. 2004;303:1162-1167.
Wall P.D., Woolf C.J. Muscle but not cutaneous C-afferent input produces prolonged increases in the excitability of the flexion reflex in the rat. J. Physiol.. 1984;356:443-458.
Wang S. Electroacupuncture treatment for constipation due to spasmodic syndrome of the pelvic floor: a report of 36 cases. J. Tradit. Chin. Med.. 2001;21:205-206.
Wang S.M., Kain Z.N., White P.F. Acupuncture analgesia: II. Clinical considerations. Anesth. Analg.. 2008;106:611-621.
Wayne P.M., Kerr C.E., Schnyer R.N., Legedza A.T., Savetsky-German J., Shields M.H., et al. Japanese-style acupuncture for endometriosis-related pelvic pain in adolescents and young women: results of a randomized sham-controlled trial. J. Pediatr. Adolesc. Gynecol.. 2008;21:247-257.
Weiss J.M. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J. Urol.. 2001;166:2226-2231.
White A. Western medical acupuncture: a definition. Acupunct. Med.. 2009;27:33-35.
White A., Cummings M. Does acupuncture relieve pain? BMJ. 2009;338:a2760.
Whorton J.C. Nature cures: the history of alternative medicine in America. New York: Oxford University press, 2004.
Zaralidou A.T., Amaniti E.N., Maidatsi P.G., Gorgias N.K., Vasilakos D.F. Comparison between newer local anesthetics for myofascial pain syndrome management. Methods Find. Exp. Clin. Pharmacol.. 2007;29:353-357.
Zermann D.H., Ishigooka M., Doggweiler R., Schmidt R.A. Chronic prostatitis: a myofascial pain syndrome? Infect. Urol.. 1999;12:84-92.