CHAPTER 9 The hip
Developmental Dislocation of the Hip (DDH)
This condition occurs in the perinatal period and involves displacement of the femoral head relative to the acetabulum; if untreated it disrupts the normal development of the hip joint which in the long term may lead to joint dysplasia, subluxation with gait disturbance, avascular necrosis, and osteoarthritis. The term ‘congenital dislocation of the hip’ (CDH), now less frequently used, is for the main part virtually synonymous. Note, however, that the contraction ‘DDH’ may be somewhat confusingly used for ‘developmental dysplasia of the hip’.
The term ‘neonatal instability of the hip’ (NIH) is of particular value as it is clearly defined: it describes a condition in which the hip is dislocated, able to be dislocated, or is unstable at examination during the first 5 days after delivery. Similarly, ‘late-diagnosed DDH’ is used to describe a dislocated or dislocatable hip diagnosed after the age of 1 week.
The condition is much more common in girls than in boys (80%) and in the first born; there is a familial tendency, and an increased frequency in those suffering from Down’s syndrome; and there is a well established geographical distribution of the disorder. It is commoner after breech presentations, and it may occur in conjunction with other congenital defects.
A simple test devised by Ortolani in the 1960s was found to show instability in the hips of some newborn children, and it was thought that this instability was directly related in every case to congenital dislocation of the hip. As a result, it was considered that if all newborns could be screened with this test, and treated promptly if instability were found, that the condition would no longer pose a problem. Unfortunately, later experience showed that a number of children who had passed the screening test went on to develop hip dislocations. It also became clear that some unstable hips could resolve without treatment; and that treatment itself (in an abduction splint) was not free from complications (about 10% developing avascular necrosis). When ultrasound screening is added to the clinical examination, there is a dramatic increase in the number of positive results, most of which resolve without treatment.
To accommodate these confusing facts, a number of regimens have been developed. One typical example recommends the following:
Note that in an increasing number of centres ultrasound screening is performed routinely. With this there is a predictable rise in false positives which are weeded out during routine after-care surveillance. It has been shown that this can significantly reduce the need for subsequent surgical procedures, hospitalisation and late presenting cases.
DDH in the Older Child
This must be suspected in any child where there is disturbance of gait or posture, shortening of a limb, or indeed any complaint in which the hip might be implicated. If dislocation of the hip is diagnosed late, treatment is aimed at restoring the hip to as near normal as possible. Each case must be assessed on its own merits, but the general principles of treatment are common to all:
DDH in the Adult
Where treatment in childhood has been unsuccessful, or even where the condition has not been diagnosed, a patient may seek help during the third and fourth decades of life. Symptoms may arise from the hips or the spine. In the hips, secondary arthritic changes occur in the false joint that may form between the dislocated femoral head and the ilium with which it comes in contact. In the spine, osteoarthritic changes are a result of long-standing scoliosis (in the unilateral case), increased lumbar lordosis (in both unilateral and bilateral cases), or excessive spinal movements that occur in walking. In a few cases hip replacement surgery may be considered, otherwise the treatment follows the lines for the conservative management of osteoarthritis of the hips and spine.
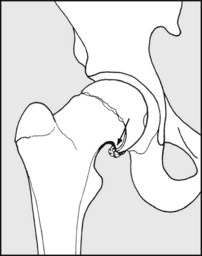
The Dysplastic Hip
Hip dysplasia is a condition in which the principal feature is that the femoral head is imperfectly contained by the acetabulum. The slope of the acetabulum is frequently greater than normal, and it may be relatively small in comparison with the femoral head. In early life this may be a major factor in developmental dislocation of the hip, but if the hip does not dislocate it may nevertheless give trouble later in life. In the dysplastic hip the central area only of the femoral head transmits the forces of weightbearing to the acetabulum, increasing the joint loadings and predisposing the hip to osteoarthritis and in some cases instability. The symptoms are those of osteoarthritis of the hip, and they may present during the second and third decades of life. Rapid deterioration is the rule. In the younger patient a Chiari osteotomy of the pelvis, an acetabular shelf operation or a high femoral osteotomy may improve the containment of the femoral head, relieve symptoms and slow the onset of osteoarthritis. In the older patient, replacement arthroplasty may be considered.
The Irritable Hip
In childhood there are a number of conditions affecting the hip which may be indistinguishable in their initial stages. They all give rise to a limp, restriction of movements, and sometimes pain in the joint (irritable hip). Children with this history are admitted routinely and treated by light traction until a firm diagnosis has been made. The commonest conditions responsible for irritable hip are transient synovitis, Perthes’ disease and tuberculosis of the hip.
Transient Synovitis
This is the commonest cause of the irritable hip syndrome. The child presents with a limp, and there is sometimes a history of preceding minor trauma which in some cases at least is coincidental. Raised interferon levels have been found, which suggests that a viral synovitis may often be the cause. There is restriction of extension and internal rotation in the affected joint, but there is no systemic upset and the sedimentation rate is generally normal. Radiographs of the hip sometimes give confirmatory evidence of synovitis, as does ultrasound examination, but no other pathology is usually demonstrable. Aspiration and culture of synovial fluid (which is not routinely performed) generally fail to provide any evidence of bacterial infection. A full recovery after 3–6 weeks’ bed rest is the rule. In a number of cases that have been slow to respond there have been positive faecal cultures of Campylobacter, and it is advised that this examination be performed routinely.
Perthes’ Disease
In this condition there is a disturbance of the blood supply to the epiphysis of the femoral head, so that a variably sized portion undergoes a form of avascular necrosis. The cause is unknown. It is five times commoner in boys than in girls, and in 12% of cases it is bilateral: and when both hips are affected they may be involved simultaneously or with an interval between them. It commonly presents between the ages of 4 and 6, and there is an association with anteversion of the femoral neck.
It usually presents with a limp, frequently accompanied by complaint of vague pains in the region of the hips, thighs or knees. Clinically, Perthes’ disease may be suspected by the history, the child’s age and sex, and by the restriction of rotation in the affected hip. As a rule, radiological changes are well established by the time the child presents with symptoms, and these will confirm the diagnosis. (Ultrasound examination shows capsular distension due to synovial thickening, with both hips being generally affected at the earliest stages (as opposed to the findings in transient synovitis).) A pattern where the age of onset is very late (i.e. over 12) has been described and is noted for its poorer prognosis.
The severity of the condition is dependent on the age of onset and the position and extent of the area of the femoral head involved. When a large part of the epiphysis is affected, there is a tendency to flattening and lateral subluxation of the femoral head; these changes are mirrored by the acetabulum, and the resultant deformity predisposes the hip to osteoarthritis later in life. If there is some doubt regarding the extent of these changes, an MRI scan will allow an accurate assessment. Thereafter, as a guide to management and prognosis, the investigative findings are used in an attempt to grade the severity of the case and form a prognosis. This can be difficult in practice, and the results not always consistent. Systems for the classification of cases of Perthes’ disease have been devised by Catterall (Frames 9.86–9.87), Stulberg et al.,1 Salter-Thompson and Herring (Frame 9.91), and all have their advocates. Most recently a radiological index has been proposed by Nelson et al. (Frame 9.92) to grade these cases.
Half of all cases of Perthes’ disease do well irrespective of any treatment, and this is especially the case in the younger age groups (i.e. under 6). Cases which have their onset in the older child, particularly over the age of 9, generally do badly. The long-term results are dependent on the growth of the femoral head, and it is unfortunately the case that treatment has not been shown to materially affect this, or to influence the ultimate outcome. Nevertheless the aims of treatment can be clearly summarised as the relief of symptoms, the containment of the femoral head, and the restoration of movements. It is accepted that in all cases the acute symptoms of pain and severe restriction of movements should be treated by bed rest and traction, followed by physiotherapy. In mild cases, where the prognosis by grading is judged to be good, no further treatment (apart from prolonged observation) is generally advocated, although some prescribe weight-relieving measures for a further period of some months to reduce the chances of weight-bearing stresses leading to further deformation of the femoral head. The results of intervention in those cases judged to carry a poor prognosis are perhaps less clear. The lines of treatment frequently advocated aim at improving the congruity of the femoral head and acetabulum, and improving the effective range of movements in the hip (e.g. by a varus osteotomy of the femoral neck, or a Salter innominate osteotomy).
Tuberculosis
Tuberculosis of the hip remains rare in the UK. The affected child walks with a limp and often complains of pain in the groin or knee. Night pain is a feature. Hip rotation becomes limited, a fixed flexion deformity develops and muscle wasting occurs. Radiographs of the hip in the early stages show rarefaction of bone in the region of the hip and widening of the joint space. As the disease advances there is progressive joint destruction, with abscess formation and sometimes dislocation. The diagnosis is usually confirmed by histological and bacteriological examination of synovial biopsy specimens, or by bacteriological examination of the aspirate.
In early cases complete resolution may be hoped for by antituberculous therapy, bed rest and traction. In the advanced case, joint debridement is carried out with efforts to obtain a bony fusion of the joint.
Acute Pyogenic Arthritis of the Hip
Staphylococcus is the organism most frequently responsible for acute infections in the hip joint. The infection is blood-borne and the diagnosis seldom difficult. The onset is rapid, with high fever and toxaemia. All movements of the hip are severely impaired and accompanied by great pain and protective muscle spasm. The most important diagnostic features distinguishing it from synovitis are fever and elevation of the ESR and C-reactive protein.
The organism responsible may be isolated by blood culture or joint aspiration. Treatment is by use of the appropriate antibiotics in doses large enough to obtain high local concentrations. Bed rest and immobilisation are also essential.
Slipped Femoral Epiphysis
This is a disease of adolescence and is commoner in boys than in girls. The attachment of the femoral epiphysis to the femoral neck loosens, so that the head appears to slide downwards on the femoral neck, giving rise eventually to a coxa vara deformity of the hip. The cause is unknown. In a number of cases there is a history of preceding trauma. A striking feature, however, is that in a high proportion of cases there is the suggestion of a hormonal disturbance. Many are fat, having the appearance of those suffering from the Frölich syndrome. Some cases have been noted to occur in association with hypothyroidism. The condition is frequently bilateral (25% at first presentation, rising later to 60%), and it is essential that the contralateral hip be kept under careful surveillance, particularly during the first 3 months.
Pain may occur in the groin or knee, and if the onset is very acute weight-bearing may become impossible. There is usually restriction of internal rotation and abduction in the affected hip. The diagnosis is confirmed radiographically, the earliest changes being seen in the lateral projections. Late complications of slipped femoral epiphysis include avascular necrosis of the femoral head and chondrolysis.
Slight degrees of slip are treated by internal fixation of the epiphysis without reduction. If there is a large amount of acute displacement a gentle reduction may be attempted before fixation, although some are unwilling to undertake this as they are of the opinion that it may increase the risks of avascular necrosis. If the slip is long standing, osteotomy of the femoral neck (to correct the deformity) is often advised. If only one hip is affected, prophylactic pinning of the other is sometimes undertaken, but this is not advocated unless the risks are judged to be especially high.
Primary Osteoarthritis of the Hip
Primary osteoarthritis of the hip occurs in the middle-aged and elderly, and is often associated with overweight and overwork, although in many cases no obvious cause may be found.
Pain is often poorly localised in the hip, groin, buttock or greater trochanter, and may be referred to the knee. There is increasing difficulty in walking and standing. Sleep is often disturbed, and the general health of the patient becomes undermined as a result. Stiffness may first declare itself when the patient notices difficulty in putting on stockings and cutting the toenails.
Fixed flexion and adduction contractures are common, with apparent shortening of the affected limb. In the early stages weight reduction, physiotherapy and analgesics may be helpful; total hip replacement is the treatment of choice if the condition is advanced.
Secondary Osteoarthritis of the Hip
The symptoms of secondary osteoarthritis of the hip are identical to those of primary osteoarthritis. The condition occurs most frequently as a sequel to developmental dislocation of the hip, congenital coxa vara, hip dysplasia, Perthes’ disease, tuberculous or pyogenic infections, slipped femoral epiphysis, and avascular necrosis secondary to femoral neck fracture or traumatic dislocation of the hip.
In secondary osteoarthritis a younger age group is generally involved than in the case of primary osteoarthritis. In the young patient, where it is thought desirable to avoid the uncertain long-term morbidity of total hip replacement, a hip joint fusion may be considered in unilateral cases. Where pain is more a problem than stiffness, McMurray’s osteotomy of the hip may sometimes be of value.
Rheumatoid Arthritis
The hip joints are frequently involved in rheumatoid arthritis. When both hips and knees are affected, the disability may be profound. In the well selected case, replacement of one or both hips may give a striking improvement in the patient’s symptoms and mobility.
Other Conditions Affecting the Hip
Of the rarer conditions affecting the hip joint, the following are not infrequently overlooked:
The following important points should always be remembered in dealing with the hip joint:
Conditions Associated with Total Hip Joint Replacement
Because of the success of hip joint replacement procedures many of these operations have been performed, and complications, which occur in about 5% of cases, are being seen with increasing frequency.
The most widely used replacement is the Charnley low-friction arthroplasty (LFA) or one of its many variants. In this, the socket is formed from high-density polyethylene and the replacement head from stainless steel. Both components are anchored with quick-setting acrylic cement. During the surgical approach to the hip the greater trochanter may be detached to gain better access; if so, it has to be reattached at the end of the operation; this often done with stainless steel wires.
There are a number of other replacements, which vary in the design of the parts, the materials used, and the techniques of their insertion. In some, the components are inserted without the use of acrylic cement, and the surgical exposure may be made without detachment of the trochanter. Where the functional requirements are not expected to be high (e.g. after intracapsular hip fractures in the very elderly) a hemiarthroplasty may be performed, where the femoral head is replaced with a stemmed prosthesis and the acetabulum is not interfered with.
Excluding complications that may arise in the immediate postoperative period, the problems which may subsequently occur may include the following:
1. Dislocation. The stability of the replacement is dependent on the precision with which the components have been aligned during their insertion, the design of the acetabular component (e.g. whether it has a posterior lip), the time that has elapsed since surgery and the degree of violence to which the components have been subjected. After any hip replacement, the fibrous capsule that forms round the artificial joint thickens and strengthens with time, leading to a progressive resistance to dislocation. In the first few months following surgery a badly aligned joint may dislocate under comparatively minor stress; in other cases, and at a later stage, considerable violence may be necessary. If dislocation occurs, weightbearing suddenly becomes impossible and there is usually marked pain. The limb shortens and may be externally rotated. The diagnosis is confirmed by X-ray examination. Treatment is by reduction (which occasionally needs to be an open one), usually followed by a period of traction until the hip becomes stable. In those cases where there is a major problem of component malalignment, a revision procedure may have to be considered should the dislocation recur.
2. Component failure. Socket failure is rare, but the stem of the femoral prosthesis may occasionally fracture. This is most likely when the patient is overweight or the component has a varus alignment, or loosens. Generally there is immediate loss of the ability to weightbear, and replacement of the fractured component becomes essential.
If the greater trochanter has been reattached with wires, these may fracture and fragment, giving rise to local discomfort and sometimes episodes of sharp, jagging pain. This may be treated by removal of the broken wires. The trochanter itself may fail to unite and may displace. This may cause local discomfort and a Trendelenburg gait. Normally there is slow, spontaneous improvement, but in the early case where the fragment is large and displaced, reattachment may be considered.
3. Fracture of the femur. The femur may fracture (as it may do without the presence of a stemmed prosthesis) as a result of direct or indirect violence, e.g. from a fall. In other cases the forces responsible for the fracture may be less than normal. The presence of the prosthesis considerably reduces the total elasticity of the femoral shaft, giving rise to high stress concentrations in the region of the tip of the prosthesis (one of the commonest sites of fracture); the bone may also be weakened by fretting at the cement–bone interface (where there may be abrasive particle formation), by cystic changes, and by infection (which may be chronic and low grade).
Treatment is dependent on many factors, including the site and pattern of the fracture, its cause, and the general health of the patient, but in the majority of cases further surgery will usually be advised.
4. Component loosening and infection. When this occurs, it is usually at the interface between the cement and bone. It is commonest in the area of the femoral stem, although both components may be affected. The complaint is of pain and impairment of function, and the diagnosis is usually made on the basis of the radiological appearances. Loosening may be the result of infection; in some cases this may be frank, and in others, organisms of low pathogenicity may be found in the affected area. In many cases, although an element of infection may be strongly suspected, no organism can be found and an alternative cause may be sought. In many, loosening may be associated with particulate wear debris, and in others tissue sensitivity to the metallic elements of the components of the prosthesis has been blamed.
Infection may be introduced at the time of the initial operation and grumble on thereafter, leading to loosening, bone absorption, and distal migration of the femoral component. There may be flare-ups accompanied by more acute pain, malaise, and sometimes abscess formation. In other cases, it would seem that late infections may arise as a result of infection being bloodborne from a septic focus elsewhere.
The treatment of these complications is highly specialised. In the (uncommon) case of secondary infection, investigations by blood culture and aspiration, immobilisation, and the prompt administration of the appropriate antibiotics may occasionally lead to resolution. In the case of loosening without the discovery of any organism, a revision procedure may be advised. Where there is evidence of a low-grade infection, a very thorough debridement under antibiotic cover, followed by the insertion of a fresh prosthesis of a pattern designed to accommodate any migration or loss of bone stock, may be attempted (either as a one- or two-stage procedure). Additional measures to control recurrence of local infection may include the use of antibiotic-loaded cement. Where infection is well established, removal of the components and cement may be the only solution which will allow the infection to be overcome, even though limb function will obviously be seriously compromised. In some of these cases, however, once the infection has been eradicated a further replacement procedure may be contemplated.
Assessment of Hip, Knee and Lower Limb Function
For over 50 years attempts have been made to devise a system whereby overall lower limb function might be assessed, so that the extent and progress of any disability might be assessed and the results of surgery evaluated. Over 80 rating systems have been suggested, but unfortunately the lack of standardisation has in many cases prevented the direct comparison of reported series.
There is general agreement on the basic functional parameters which should be assessed. These include pain, stiffness and the ability to perform certain activities of daily living. In some systems there is also inclusion of social and emotional factors (such as the return to work and any noted restrictions), joint movements and X-ray appearances. There have been problems over the weight placed on each of the items assessed, on how to evaluate subjective findings such as pain, and how to reduce systems to manageable levels: many have been abandoned because of their complexity and time involved in their analysis. The presently popular WOMAC (Western Ontario and McMaster Universities Osteoarthritis)2 Index is in fact a self-assessment questionnaire which has been simplified and modified1 to help improve the patient’s assessment of the standard 24 questions asked. It is mainly used to evaluate osteoarthritis and rheumatoid arthritis of the hip and knee, before and after joint replacement therapy. The WOMAC Index is available in 65 alternative language forms and has been well validated.
The initial lower limb assessments were developed specifically for the hip at the time when rapid developments were occurring in hip joint surgery, particularly in the field of joint replacements. The Harris System,3 although frequently modified, has stood the test of time. In it, a normal hip is rated as scoring 100 points, while the hip being examined is described as being so many percent of this theoretical normal. Pain (which is subjective and hard to assess with accuracy) is allocated 44 points. Function, which is highly detailed, is broken down into gait, the use of supports and activities, and merits 47 points. Range of movements attracts only 5 points, and absence of deformity 4 points.
If a hip scoring system is being used to assess the results of a hip replacement (and this is one of the commonest indications), then it is desirable to include details of the radiographic appearances which are so important. The terminology has been described as standard and unalterable in its definition, so that without weighting results can be readily compared between series. Although use of the full list (described in the reference) may have to be considered where publication is intended, the questions in the clinical assessment are of such value in assessing any case that they are appended here.
Pain
Level of activity
Time walked
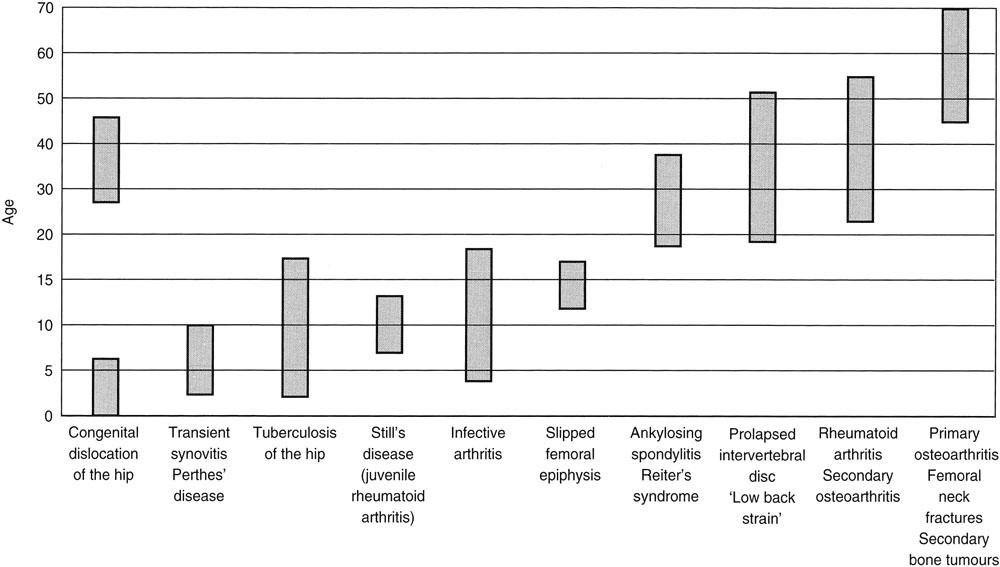
Table 9.1 Age distribution of common hip pathology
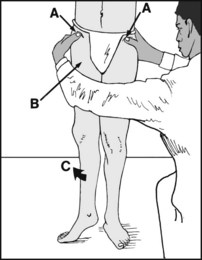
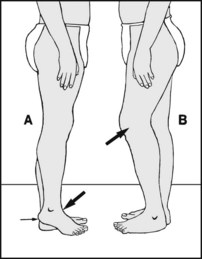
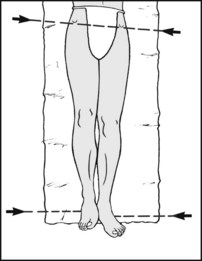
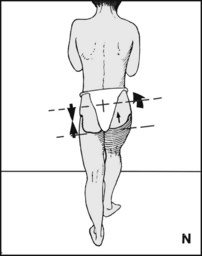
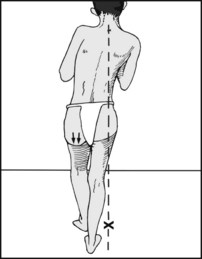
Examine the standing patient from the front. Note (A) any pelvic tilting (e.g. from adduction or abduction deformity of the hip, short leg, scoliosis), (B) muscle wasting (e.g. secondary to infection, disuse, polio), (C) rotational deformity (common in osteoarthritis).
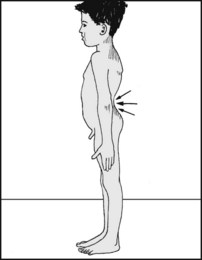
Examine the patient from the side. Note any increased lumbar lordosis suggestive of fixed flexion deformity of the hip(s).
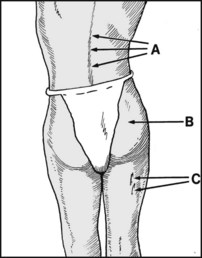
Look at the patient from behind. Note (A) any scoliosis (possibly secondary to pelvic tilting from, for example, an adduction deformity of the hip), (B) gluteal muscle wasting (e.g. from disuse, infection), (C) sinus scars (e.g. secondary to tuberculosis).
Observe the gait from the front, sides and behind. Analysis grows from experience. Try to assess the stride and dwell time on each side, and the possible factors of pain, stiffness, shortening and gluteal insufficiency. Note that a shuffling gait (where each foot is dragged on the ground in the swing phase) or a stomping gait (where the foot hits the ground in a violent manner) may be seen in cases of posterior cord syndrome, and a broad-based gait in cases of spinal cord compression.
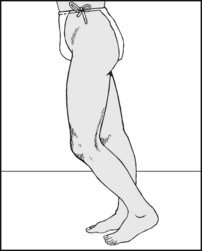
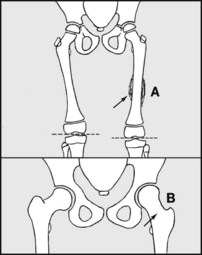
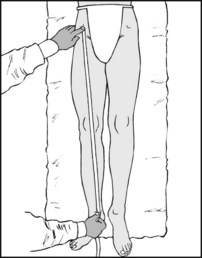
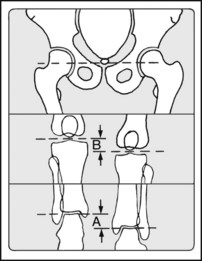
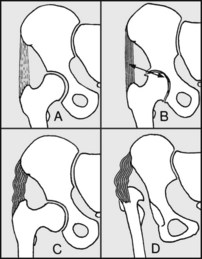
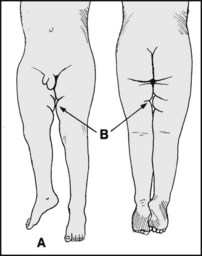
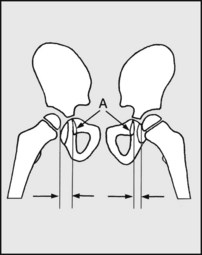
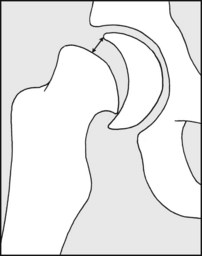
It is important in the examination of the hip and the lower limb to determine the presence or absence of shortening. In true shortening, the affected limb is physically shorter than the other. This may be caused by pathology (A) above or proximal to the greater trochanter or (B) distal to the trochanters.
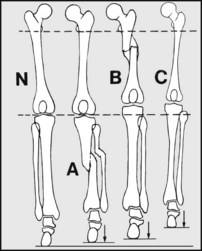
True shortening from causes distal to the trochanters most frequently results from (A) old fractures of the tibia or (B) of the femur; (C) growth disturbance (e.g. from polio, bone or joint infections, epiphyseal trauma, or one of many hereditary bone diseases. (N) = normal side for comparison. (Note that in children, likely leg discrepancies at skeletal maturity may be predicted using a number of methods, including that of multiplier factors devised by Dror Paley et al.)
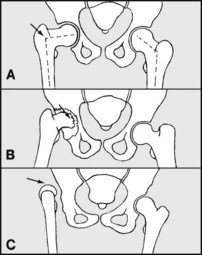
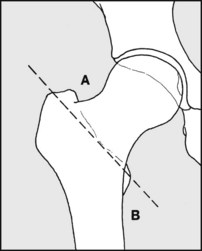
Above the trochanter causes include (A) coxa vara (e.g. from femoral neck fractures, slipped upper femoral epiphysis, Perthes’ disease, congenital coxa vara; (B) loss of articular cartilage (from infection, arthritis), (C) dislocation of the hip (e.g. secondary to developmental dislocation of the hip).
Very rarely lengthening of the other limb gives relative true shortening. This may be due to (A) stimulation of bone growth from increased vascularity (e.g. after long bone fracture in children, or a bone tumour); (B) coxa valga (e.g. following polio).
In apparent shortening the limb is not altered in length, but appears short as a result of an adduction contracture of the hip, which has to be compensated for by tilting of the pelvis.
Limb shortening may be compensated by (A) plantarflexion of the foot on the affected side, or by (B) flexion of the knee on the other side. Most frequently the discrepancy is countered by pelvic tilting. The latter may in turn be compensated for by the development of a lumbar scoliosis.
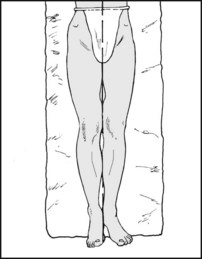
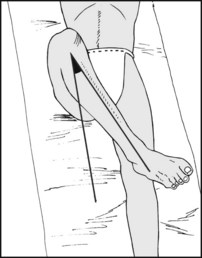
9.11. Shortening: examination (1):
The patient should be adjusted to lie squarely on the couch, with the trunk and legs parallel to its edge. The position of the pelvis should be observed (by the position of the anterior superior iliac spines) and adjusted where possible.
9.12. Shortening: examination (2):
In the normal patient the heels should be level, and the plane of the anterior superior iliac spines at right angles to the edge of the couch.
9.13. Shortening: examination (3):
Where there is significant true shortening the heels will not be level (the discrepancy is a guide to the amount of shortening) and the pelvis will not be tilted. The site and amount of shortening must now be further investigated.
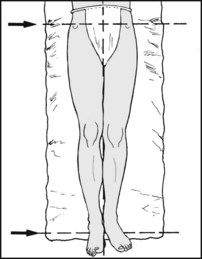
9.14. Shortening: examination (4):
Begin by hooking the thumbs under the anterior spines. Feel for the greater trochanters with the fingers. If the distance between the thumb and fingers is shorter on one side, this suggests that the pathology lies above the trochanters.

9.15. Shortening: examination (5):
If in the last test there was no evidence of shortening above the trochanter, look for causes below the trochanter. Slightly flex both knees and hips, and place a hand behind the heels to check that you now have them squarely together.
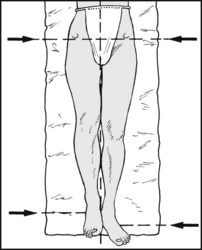
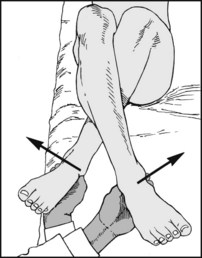
9.16. Shortening: examination (6):
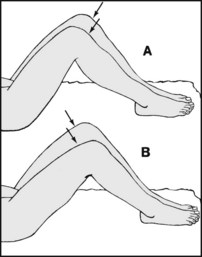
The position of the two knees should be compared. (A) This appearance suggests femoral shortening. (B) This appearance is suggestive of tibial shortening (in the diagram, the right side is as usual the site of the pathology).

9.17. Shortening: examination (7):
Further confirmation of tibial shortening may be made by direct measurement. Flex one knee, and with the thumb locate the prominences of the femur and tibia, with the joint line lying between. This is best performed on the medial side of the joint. Now mark the joint line, and repeat on the other side.

9.18. Shortening: examination (8):
Now measure from the mark to the tip of the medial malleolus. Compare the two sides. Any difference indicates true tibial shortening. Note also any obvious tibial irregularity suggestive of old fracture.
9.19. Shortening: examination (9):
Measurement of femoral shaft shortening can only be attempted in the thin patient where the tip of the greater trochanter is easily palpable. Measure from the trochanter to the lateral joint line and compare the sides.
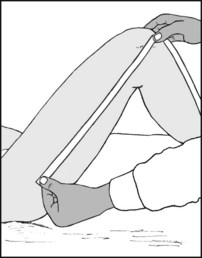
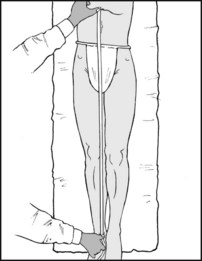
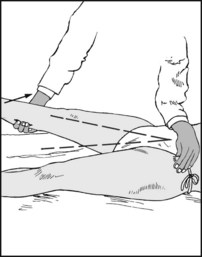
9.20. Shortening: examination (10):
Measurement of total (true) leg shortening is the most valuable single assessment, although in itself it gives no indication of site. Begin by placing the metal end of the tape over the anterior spine; now press it backwards until it hooks under its inferior edge. In this way the end of the tape comes into firm contact with the iliac spine, and there is less chance of having difficulty in getting a reliable, fixed measuring point at this level.
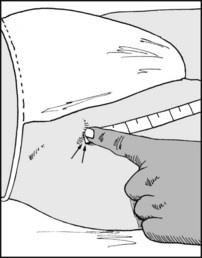
9.21. Shortening: examination (11):
Now measure to the middle or inferior border of the medial malleolus. Compare the sides, and always repeat the measurements until consistency is obtained. Deformity of the pelvis (which is rare) may sometimes lead to errors in assessment.
9.22. Shortening: examination (12):
When the patient is carefully positioned on the examination couch, and the pelvis is obviously tilted, try to correct this. If it cannot be levelled, then expect to find some apparent shortening of the limb; the discrepancy between the heels will give a measure of this. (Note, however, that as well as apparent shortening there may be some additional true shortening, which should be assessed by direct limb measurement as just described.)
9.23. Shortening: examination (13):
Apparent shortening may also be assessed by comparing the distances between the xiphisternum and each medial malleolus.
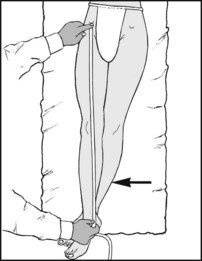
9.24. Shortening: examination (14):
When there is an adduction deformity of the hip, and the leg lengths are being measured to assess any accompanying true shortening, the good leg should be adducted by the same amount before commencing measurement between the anterior spines and malleoli.
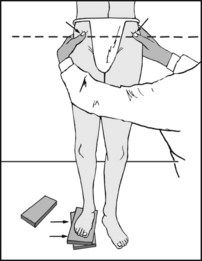
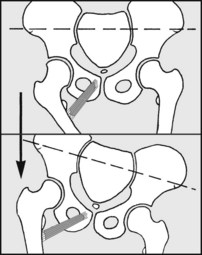
9.25. Shortening: examination (15):
True leg shortening may also be measured by blocking up the short leg until both anterior superior iliac spines and the iliac crests lie horizontally, and the natal cleft is vertical; a further check that the pelvis is level is to see that the posterior iliac spines remain horizontal when the patient flexes forwards.
9.26. Shortening: examination (16):
In the difficult case, sequential radiographs of the hips, knees and ankles, taken on a single plate without moving the patient, afford accurate comparison of the sides. For example, (A) indicates overall shortening, (B) indicates femoral shortening. (Note that in the older patient a discrepancy of 3–4 cm leads on walking to an increase in heart rate, ventilation and muscle activity which may seriously limit activity, especially if there is already some cardiac, pulmonary or neuromuscular impairment.)

Place the fingers over the head of the femur below the inguinal ligament, lateral to the femoral artery. Note any tenderness. Now rotate the leg medially and laterally. Crepitus arising in the hip joint may be detected in this way.

Palpate the origin of adductor longus. Tenderness occurs here in sports injuries (strain of adductor longus) and in patients developing adductor contractures in osteoarthritis of the hip.
Externally rotate the leg and palpate the lesser trochanter. Tenderness occurs here in strains of the iliopsoas as a result of athletic injuries.

Palpate the region of the ischial tuberosity looking for tenderness. Strain of the hamstring origin occurs as a result of athletic activities, especially in children. Less commonly athletic injuries may affect the anterior superior and inferior spines.
9.31. Movements: extension (1):
Place a hand behind the lumbar spine so that you can determine whether in the spine at rest there is any increase in lumbar lordosis, and later on in the course of the examination, whether this has been obliterated.

9.32. Movements: extension (2):
Now flex the good hip fully, observing with the hand that the lumbar curvature is fully obliterated.

9.33. Movements: extension (3):
If the hip being examined rises from the couch, this indicates loss of extension in that hip (also described as a fixed flexion deformity of the hip). Any loss should he measured and recorded. This test is usually referred to as Thomas’s test.

9.34. Movements: extension (4):
To check smaller losses of extension, especially when the other hip is normal, turn the patient over on to his face and steady the pelvis with one hand.

9.35. Movements: extension (5):
Lift each leg in turn and compare the range of movements.
Normal range of extension = 5–20°.
A loss affecting extension only is often the first detectable sign of an effusion in the hip joint.
The good hip is first flexed to obliterate the lumbar curve and to steady the pelvis. The patient is asked to hold the leg in this position.

The hip is then flexed, using a hand to check that no further pelvic movement occurs. Note the range of movement.
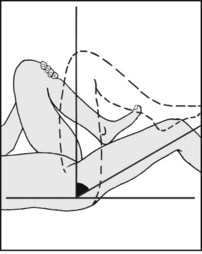
The range of flexion may be recorded in this example as ‘Flexion (R) hip: 30–90°’, or ‘Fixed flexion deformity of 30°, and hip flexes to 90°’. Flexion may also be tested with the patient lying on his side.
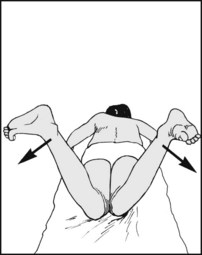
9.39. Movements: abduction (1):
A false impression of hip movement may be gained if the pelvis tilts during the examination, so first grasp the opposite anterior superior iliac spine with the fingers and thumb, and anchor the other spine with the forearm.
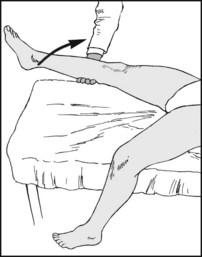
9.40. Movements: abduction (2):
An alternative way of fixing the pelvis is to flex the other leg over the edge of the couch and check that the pelvis does not move by holding the anterior superior iliac spine on the side being examined.
9.41. Movements: abduction (3):
Now, having fixed the pelvis, move the leg laterally and note the range achieved.
Normal range of abduction = 40°.
Abduction may also be tested from a starting position of 90° hip flexion (see also below). This is of particular value in suspected osteoarthritis of the hip or congenital dislocation.
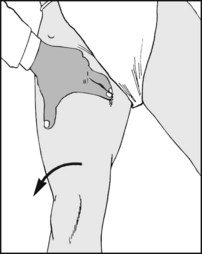
Basically, this is a variation of abducting the hip from a position of 90° flexion. Pain during the manoeuvre is regarded as being the very first sign of osteoarthritis in a hip. To perform (on the right), flex both hips and knees, place the right foot on the left knee and gently press down on the right knee. This is also known as the faber sign (flexion, abduction, external rotation).

9.43. Movements: adduction (1):
Ideally an assistant should lift the good leg out of the way to allow the affected leg to be adducted while in full extension.

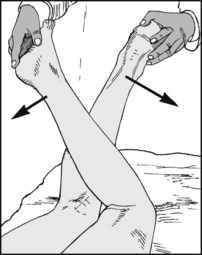
9.44. Movements: adduction (2):
If an assistant is not available, cross the leg being examined over the other. This brings the leg being examined into slight flexion, but is sufficiently accurate under most circumstances. If the hip is normal, the legs should cross about mid-thigh. Adduction may also be tested from a starting position of 90° hip flexion.

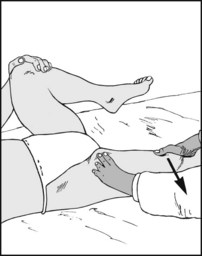
9.45. Movements: internal rotation at 90° flexion (1):
Steady the flexed hip by holding the knee with one hand, and move the foot laterally to produce internal rotation of the hip. Note that this is a never-ending source of confusion; be sure that this is clear in your own mind. Although the foot moves laterally (or externally), the hip rotates internally (or medially).
9.46. Movements: internal rotation at 90° flexion (2):
Measure the range of internal rotation by comparing the position of the leg and the midline.
Normal range of internal rotation at 90° flexion = 45°.
Compare the sides. Loss of internal rotation is common in most hip pathologies.
9.47. Movements: internal rotation at 90° flexion (3):
A sensitive comparison of the sides may be made by asking the patient to hold the knees together while you move both feet laterally.
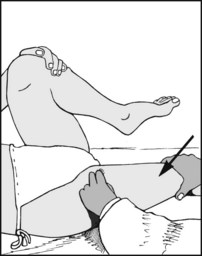
9.48. Movements: external rotation at 90° flexion (1):
The position of the hip is the same as for testing internal rotation, but in this case the foot is moved medially.
9.49. Movements: external rotation at 90° flexion (2):
Measure external rotation in the same general way.
Normal range of external rotation at 90° flexion = 45°.
External rotation becomes limited in most arthritic conditions of the hip.
9.50. Movements: external rotation at 90° flexion (3):
Comparison between the sides may be made by crossing one leg over the other.

9.51. Movements: rotation in extension (1):
For a rough comparison of the sides, roll each leg medially and laterally, observing and allowing, however, for any play at the knee.
9.52. Movements: internal rotation in extension:
For a more accurate assessment the patient should be prone, with the knees flexed. The two sides can easily be compared and measurements taken.
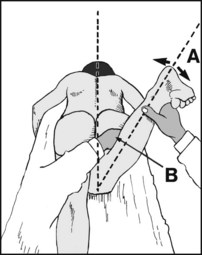
9.53. Anteversion of the femoral neck:
Anteversion may be assessed when the patient is in the same position. Hold the leg with one hand and rock it from side to side (A) while simultaneously feeling the prominence of the greater trochanter with the other (B). When the trochanter is facing truly laterally, anteversion is equal to the angle between the leg and the vertical. Anteverion may also be assessed by a number of radiological techniques.
9.54. Movements: external rotation in extension:
9.55. Movements: testing for hip fusion (1):
When there is doubt regarding the solidity of a hip fusion, it is sometimes helpful to test for protective muscle contraction. Flex the good hip and knee. Feel for involuntary adductor contracture while suddenly attempting to abduct the leg.
9.56. Movements: testing for hip fusion (2):
Repeat the test, this time feeling for flexor (iliopsoas) contraction while making a sudden gentle attempt to extend the hip.
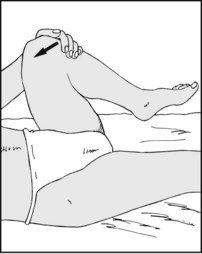
9.57. Trendelenburg’s test (1):
When standing on one leg (here the left), the centre of gravity (at S2) is brought over the stance foot by the hip abductors (gluteus medius and minimus). This tilts the pelvis and normally elevates the buttock of the non-stance side. The patient should be able to produce a greater pelvic tilt (by being asked to lift the side higher) and hold the position for 30 seconds.
9.58. Trendelenburg’s test (2):
Ask the patient to stand on the affected side: any support (stick or hand) must be on the same side. Now ask him to raise the non-stance leg further. Prevent excessive trunk movements (a vertical dropped from C7 should not fall beyond the foot). If the pelvis drops below the horizontal or cannot be held steady for 30 seconds, the test is positive. It is not valid below age 4: pain, poor cooperation or bad balance may give a false positive.
9.59. Trendelenburg’s test (3):
The test is positive as a result of (A) gluteal paralysis or weakness (e.g. from polio, muscle-wasting disease); (B) gluteal inhibition (e.g. from pain arising in the hip joint); (C) from gluteal inefficiency from coxa vara; or (D) developmental dislocation of the hip (DDH). Nevertheless, false positives have been recorded in about 10% of patients.
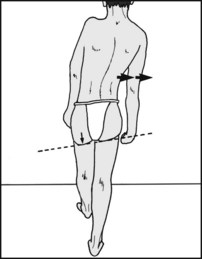
Note whether the patient, when walking, lurches to one side. If present, this is because the patient is trying to reduce pain by shifting his body weight over the hip. This is often also somewhat confusingly referred to as an abductor or Trendelenburg lurch. It is often associated with a positive Trendelenburg sign (ill), but not invariably.

Test the power of the hip abductors with the patient lying on his side, attempting to abduct the leg against resistance.

Test the power in gluteus maximus by asking the patient to extend the hip against resistance, at the same time feeling the tone in the contracting muscle.
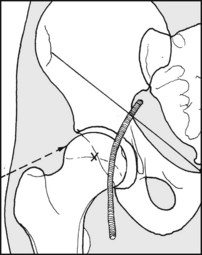
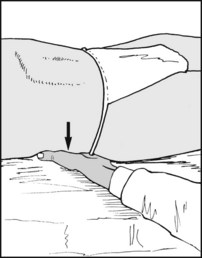
The hip may be aspirated by inserting a needle above the trochanter, allowing for femoral neck anteversion. Alternatively, a needle may be passed into the joint from in front, a little below the inguinal ligament and lateral to the femoral artery.

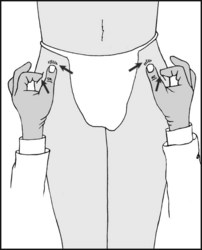
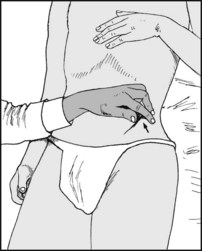
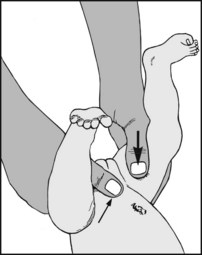
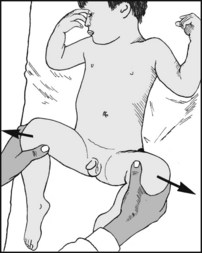
To be of any value the examination must be carried out on a relaxed child, preferably after feeding. Flex the knees and encircle them with the hands so that the thumbs lie along the medial sides of the thighs and the fingers over the trochanters.

Now flex the hips to a right angle and, starting from a position where the thumbs are touching, abduct the hips smoothly and gently.

If a hip is dislocated, as full abduction is approached the femoral head will be felt slipping into the acetabulum. An audible click may accompany the displacement, but in no way must this be considered an essential element of the test. Note that restriction of abduction may be pathological, and represent an irreducible dislocation. A positive Ortolani test is indicative of neonatal instability of the hip (NIH), and is usually an indication for splintage.
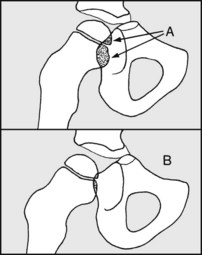
9.67. Barlow’s provocative test (1):
If the Ortolani test is negative the hip may nevertheless be unstable. Fix the pelvis between symphysis and sacrum with one hand. With the thumb of the other attempt to dislocate the hip by gentle but firm backward pressure. Check both sides.
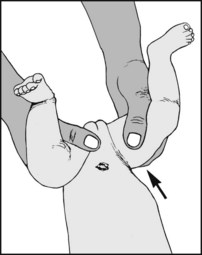
If the head of the femur is felt to sublux backwards, its reduction should be achieved by forward finger pressure or wider abduction. The movement of reduction should also be appreciated with the fingers. If Barlow’s test is positive (and Ortolani’s negative), recheck at weekly intervals. Instability persisting for more than 3 weeks is an indication for splintage, or for further investigation with ultrasound and X-ray.
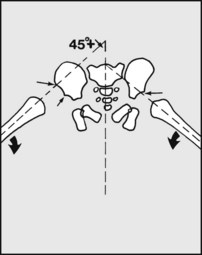
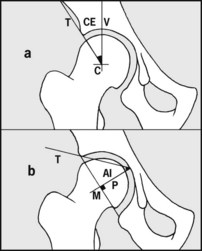
9.69. Radiographic examination of the neonate:
(a) van Rosen method: An AP view should be taken with the hips in at least 45° abduction and full internal rotation. A line projected along the line of the femur in the normal hip should strike the acetabulum and, in a case of dislocation, the region of the anterior superior spine. Note: To avoid radiation, this somewhat unreliable investigation should be done only where there is still uncertainty after clinical and ultrasound testing.
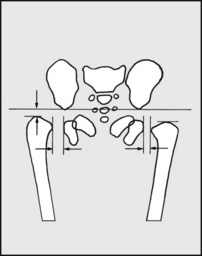
9.70. Radiographic examination:
(b) Edinburgh method: An AP film is taken with the child’s legs held parallel, with slight traction and no external rotation. Centre the beam at a standard distance of 100 cm. Measure the gap between the most medial part of the femur and the lateral edge of the ischium. This is normally 4 mm; over 5 mm is suspicious; 6 mm is regarded as diagnostic of DDH. Proximal migration can also be measured in the same film.
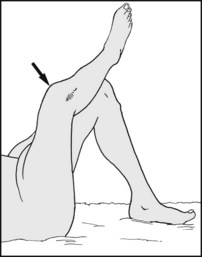
9.71. Developmental dislocation of the hip (DDH): The older child (1):
Appearance: (A) The affected leg in a case of unilateral dislocation of the hip may appear slightly shorter, and lie in external rotation. (B) There may be asymmetry of the skin folds in the thigh, although this sign is of limited reliability.
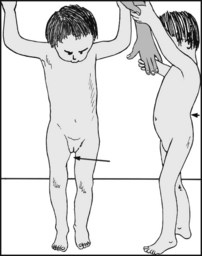
9.72. Developmental dislocation of the hip (DDH): The older child (2):
If both hips are involved there is usually widening of the perineum owing to the hip displacement. If the child has been walking, there will be a compensatory increase in lumbar lordosis.

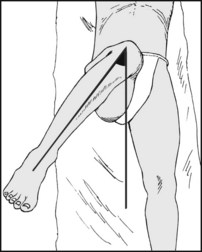
9.73. Developmental dislocation of the hip (DDH): The older child (3):
Trendelenburg’s test will be positive and the gait will be abnormal, with excessive shoulder sway. In unilateral cases the child will dip on the affected side; in bilateral cases the child will have a waddling gait.
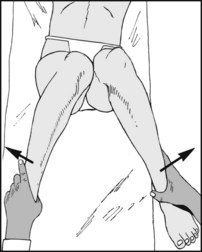
9.74. Developmental dislocation of the hip (DDH): The older child (4):
Test the range of abduction from a position of 90° flexion of the hip. In DDH abduction is restricted in this position, and of course is most obvious in the unilateral case. A 20° difference between the sides, or less than 60° of abduction, is regarded as highly significant, and further investigation is essential. The test should be performed routinely at 3 months, especially in a high-risk case.

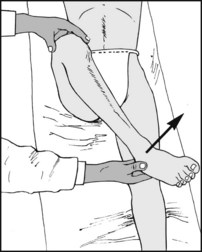
9.75. Developmental dislocation of the hip (DDH): The older child (5):
Attempt to elicit telescoping in the affected limb. Steady the pelvis with one hand, and push and pull along the axis of the femur with the other. Abnormal excursion of the limb is suggestive of DDH. Always compare the sides.
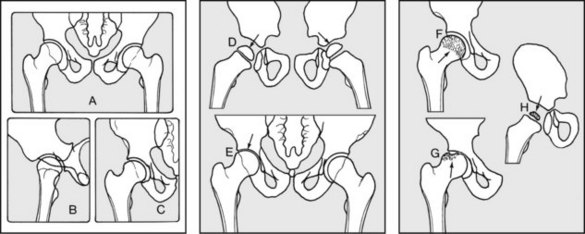
An anteroposterior view showing both hips (A) is the most useful single screening film, as it allows both sides to be compared. If the joint is strongly suspect, an additional lateral projection (B) and an anteroposterior (C), centred on the suspect hip, are essential. Note first in the films any disturbance of bone texture (e.g. in Paget’s disease, osteoporosis, tumour). Now note the joint space (which indicates the depth of articular cartilage and interposing fluid), which may be (D) increased in Perthes’ disease, synovitis and infection, and (E) decreased in the later stages of infection and arthritis. Note the relative density of the femoral head, which may be decreased, e.g. in rheumatoid arthritis, infection and osteoporosis, and increased in avascular necrosis (F), segmental avascular necrosis (G) and Perthes’ disease (H).
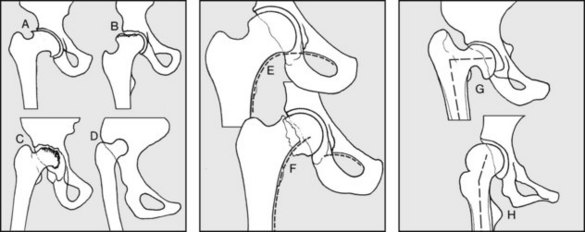
Now note the shape of the femoral head, which may, for example, be (A) buffer-shaped after Perthes’ disease, (B) flattened after avascular necrosis (total or segmental), (C) irregular or destroyed after infection, (D) atrophic in persistent developmental dislocation of the hip. Note Shenton’s line, which normally forms a smooth curve flowing from the superior pubic ramus to the femoral neck (E). Compare the sides if possible. Distortion occurs in many conditions involving the femoral neck and head, particularly fractures (F) and subluxations. Note the neck–shaft angle. This is decreased in congenital coxa vara (G), and coxa vara secondary to rickets, Paget’s disease, osteomalacia, fracture etc. It is increased in coxa valga secondary to polio (H) and other neurological disturbances.
9.80. The neck–shaft angle may be measured from lines drawn through the shaft and along the centre of the neck into the centre of the head.
Normal neck–shaft angle in males = 128°.
Normal neck–shaft angle in females = 127°.
The centre of the head may be easily found with the aid of an orthopaedic rule or similar transparent drawing template inscribed with concentric circles of different radii.

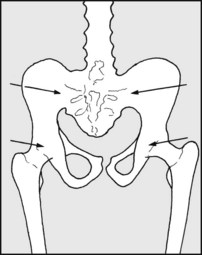
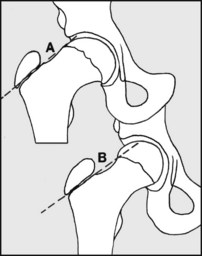
This may be localised and of the pattern found in protrusio acetabuli (A), which is often hereditary and frequently associated with osteoarthritis; or it may be generalised (B), leading to deformity of the pelvic inlet (triradiate pelvis): this is found in osteomalacia and other diseases accompanied by bone softening, such as rickets and Paget’s disease.
Note the presence of any of the changes commonly seen in osteoarthritis, such as (A) joint space narrowing, (B) marginal osteophytes, (C) marginal sclerosis, (D) cystic changes in the head of the femur and in the acetabulum.
9.83. Complete obliteration of the hip joint (bony ankylosis) is seen in ankylosing spondylitis (where there is invariably involvement of the sacroiliac joints). It is also seen as a late result of tuberculous and other infections, and after surgical fusion.
The earliest radiographic sign is an increase in joint space. (Note, however, that this is also seen in synovitis of the hip and in infective arthritis). Minor degrees of joint space widening may be detected by measuring the distance between (A) ‘the tear drop’ and the capital epiphysis on both sides.
If the ‘tear drop’ (formed by the anterior acetabular floor) is not clear, note (A) the overlap shadows of the head and neck on the acetabulum, comparing one hip with the other. Alteration (B) occurs in Perthes’ disease, synovitis and infection.
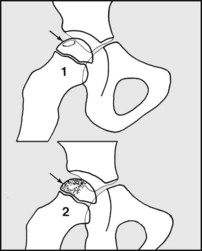
Catterall grading (a): This is the commonest method used to assess the severity of the bone changes when they appear. Grade 1: Cyst formation occurs in the anterolateral aspect of the capital epiphysis. Revascularisation may be completed without bone collapse, and the prognosis without treatment is good. Grade 2: A little more of the head is involved, and bony collapse is inevitable.
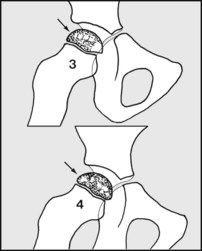
Catterall grading (b): Grade 3: Most of the head is involved. Grade 4: The whole head is affected. Bony collapse is inevitable in grades 3 and 4, and the prognosis is consequently poorer.
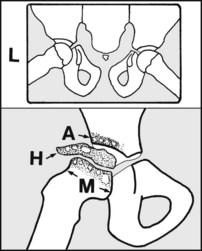
The so-called ‘frog’ lateral (Loewenstein projection, (L)) is routine in assessing these cases. Apart from the cystic changes that appear in the capital epiphysis, the acetabulum may be similarly affected (A); cystic changes may also occur in the metaphysis, which may widen (M). The femoral head may flatten and extrude laterally (H). MRI scanning allows more accurate grading.
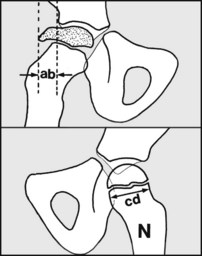
Lateral extrusion may be expressed as a percentage of the diameter of the metaphysis on the normal side (N): if ab/cd × 100 >20%, then the prognosis is poor. An accurate assessment of the amount of avascular bone may be made by radionuclide bone scanning. Prognosis is mainly dependent on the mass and degree of epiphyseal involvement (assessed, for example, by Catterall grading).
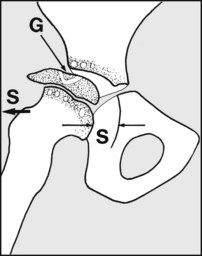
Other adverse factors placing the case in the ‘head-at-risk’ category include (a) presentation above the age of 4, (b) calcification seen lateral to the epiphysis or other evidence of major extrusion, (c) lateral subluxation (S), (d) a positive Gage sign (a sequestrum surrounded by a ‘V’ of viable epiphysis (G).
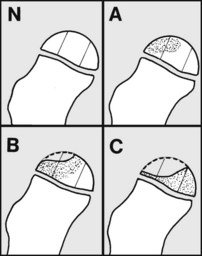
Herring lateral pillar classification: Divide the head into three columns during the fragmentation stage; then, if the lateral part is of normal height (Herring A), the prognosis is excellent. If the lateral part is depressed up to 50% (even with the central column involved) (Herring B), the results are generally good under age 9. In Herring C the lateral pillar is less than 50% and all develop permanent deformity.
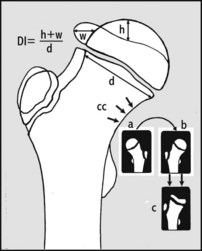
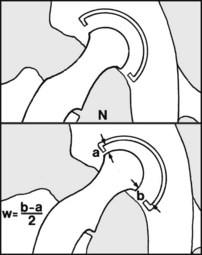
The Deformity Index (DI) is useful in unilateral cases. To use this, take a radiograph of the normal hip (a), reverse it (b), and superimpose it on a film of the affected side (c), lining up each calcar femorale. The DI expresses the flattening (h) and lateral extrusion of the epiphysis (w) as a fraction of the diameter of the femoral neck. Values in excess of 3.0 carry a poor prognosis.
9.93. Slipped femoral epiphysis (1):
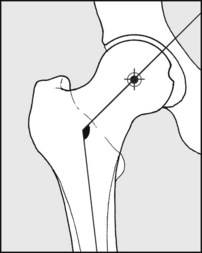
The earliest changes are seen in the lateral projection. A line drawn up through the centre of the neck fails to meet the midpoint of the base of the epiphysis. The distance between the centre of the base of the epiphysis (X) compared with the width of the base of the epiphysis may be used to calculate the degree of slip. Less than 1/3 may be classified as grade 2; grade 3 = 1/3 to 1/2; grade 4 = more than 1/2. (Grade 1 is used for pre-slip cases.)
9.94. Slipped femoral epiphysis (2):
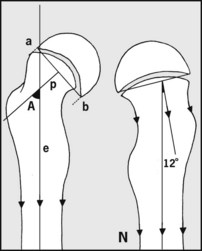
Southwick’s method of quantifying the severity of any slip: In the frog lateral draw a perpendicular (p) from a line (ab) drawn across the base of the epiphysis. Note the angle (A) between this and a line (e) drawn through the centre of the femoral shaft, and compare the sides. (If the condition is unilateral, subtract 12° to allow for the normal-shaft angle in this projection.) 30° is regarded as mild; 30–60° is moderate, and more than 60° severe.
9.95. Slipped femoral epiphysis (3):
Although the earliest radiographic changes are seen in the lateral, greater degrees of slip become detectable in the AP projections. The first sign is that a tangential line drawn on the upper femoral neck fails to strike the epiphysis (A), whereas in a normal well centred view such a tangent (B) includes part of the epiphysis.
9.96. Slipped femoral epiphysis (4):
In the later stages, some weeks after the initial slip (now the so-called ‘chronic slip’ stage) there is distortion of the inferior part of the femoral neck, with new bone formation (‘buttressing’).
9.97. Slipped femoral epiphysis (5):
Physeal separation: the frog lateral radiograph is again used. The distance between the anterior lip of epiphysis and the closest point of the metaphysis is measured. In the majority of cases of slipped femoral epiphysis there is in fact no physeal separation. If separation is present, it is seldom detected unless it exceeds 4 mm. Detected separations normally lie in the 4–12 mm range. Separation is a significant finding, as it tends to be associated with a high incidence of avascular necrosis.
9.98. Radiographs in the child (1):
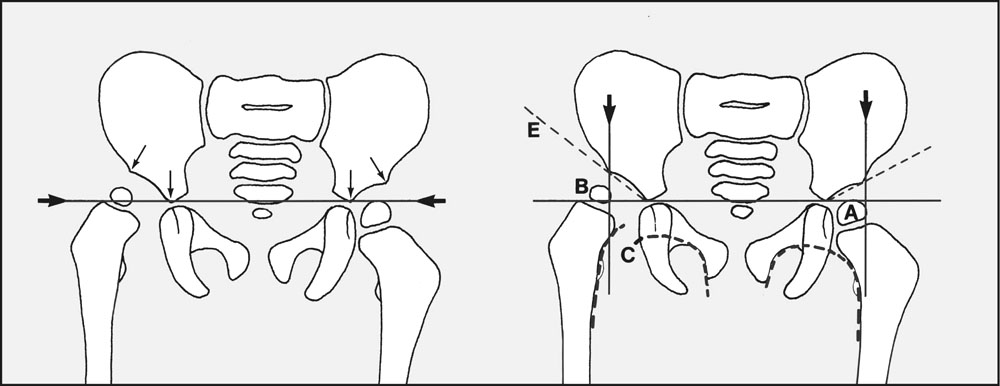
Interpretation of hip radiographs in the older child is dependent on the presence of ossification in the epiphysis of the femoral head. This normally appears between 2 and 8 months, but is often delayed in DDH. The position of the capital epiphysis in relation to the other pelvic elements must be determined. First draw a horizontal line (Hilgenreimer line) across the pelvis. On each side this should touch the downward-pointing apex of the acetabular element of the ilium. Vertical lines (Perkins’ lines) should then be drawn from the lateral limits of the acetabula. These lines divide the region of each hip into four areas. The epiphysis of the femoral head should normally lie within the lower and inner quadrant (A), but in DDH the head moves upwards and outwards (as at B). Shenton’s line (C) may be disturbed. Dysplasia of the acetabulum alters its slope (E), which decreases with growth (it usually does not exceed 30° at 6 months). There are a number of other measurements of a specialised nature that may be made (and compared with tables detailing average values relating to age and sex) when a more detailed assessment of hip dysplasia is required.
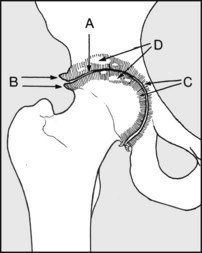
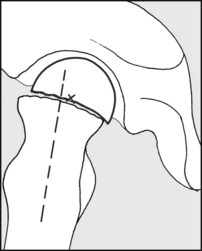
To assess joint development after treatment for DDH the following may be noted (a) the centre-edge angle (CE, of Wiberg); and (b) the acetabular index (AI angle). (V is a vertical, C the centre of the femoral head, T an acetabular edge tangent, M is the midpoint of a line joining the acetabular margins, P a vertical drawn from it.) Additional information regarding the head, acetabulum and limbus may be obtained by MRI scans or contrast arthrography.
9.100. Component loosening after total hip replacement:
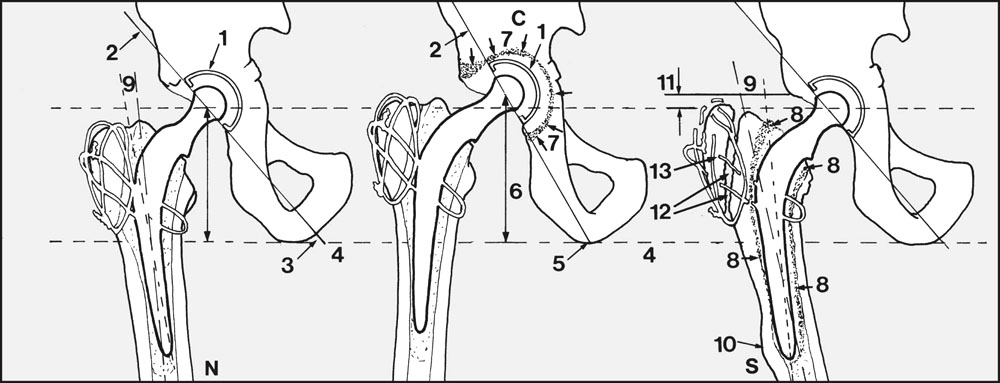
The cup (C): The wire marker (1) sunk within the radiolucent cup aids the analysis of any radiographic series. The plane (2) of the socket lies at an angle (3) to the plane of the pelvis (4), shown by a line drawn between the ischial tuberosities. This angle may be altered (5) by rotation of the cup if it loosens. The cup may also migrate proximally: look for any disturbance in the relationship between the wire marker and the fixed landmarks of the pelvis. An increase in the distance (6) between the centre of the cup and the ischium may be suggestive of migration, although errors of positioning and tube/film distances make this a little unreliable. Development of a radiolucent zone (7) (between cement and bone) exceeding 1 mm and extending right round the cup is a strong indicator of loosening. (Note that the appearance of a radiolucent line between the cement and a component is diagnostic of loosening.) The stem (S): Look for a radiolucent zone of more than 1 mm between cement and bone (8) or between the stem and the cement. Note any change in the angle between the axes of the femur and prosthetic stem (9), or any local bone disturbance (10). Check for sinking of the prosthesis, by noting the distance between the upper edge of the acetabulum and the greater trochanter (11). Non-union of the greater trochanter (12) and wire fracture and fragmentation (13) should also be recorded.
This is posing less of a problem than was originally anticipated by both surgeons and patients, but should be assessed. Wear involves the softer acetabular component; head wear is negligible. To determine wear, measure the gap between the prosthetic head and the wire marker at their upper and lower limits. Half the difference between these is a measure of wear in the wall of the cup, 3 mm or more being an appreciable amount.

In this (normal) Charnley total hip replacement, the stem of the prosthesis is well placed. The greater trochanter is uniting in good position, and the wires are intact. The head of the femoral component is concentric with the acetabular wire marker.

9.103. Hip radiographs: examples of pathology (1):
After a total hip replacement the floor of the acetabulum has given way and the cup is becoming centrally displaced.

After a total hip replacement the prosthetic stem has fractured, with loss of the ability to weightbear. Note the cement, which has extruded into the pelvis during the insertion of the device. There is some evidence of loosening of both the cup and the stem.

In this case of total hip replacement the trochanteric wires have broken; the trochanter has displaced proximally and failed to unite. The stem has loosened, and its distal end is in danger of broaching the femoral cortex. Note the extensive translucency at the bone–cement interface.

Following a dislocation of the hip which was successfully reduced, this patient complained of great stiffness in the hip. Note the extensive new bone formation around the joint.

Note the gross distortion of the pelvis.
Diagnosis: triradiate pelvis, in this case secondary to osteomalacia.

In the left hip (right of the illustration) the femoral epiphysis is smaller than on the other side, and the slope of the acetabulum greater. Shenton’s line is disrupted. If Perkins’ squares are constructed, the epiphysis of the femoral head will be seen to lie in the upper and outer quadrant. (Compare these findings with the other side.) There is some atrophy of the femoral shaft, suggesting a long-standing lesion.

There is distortion of both femoral heads, which have become buffer shaped, and there is alteration of the neck–shaft angles.

The left hip is dislocated and the femoral head atrophic; on the right the femoral head is poorly contained in the acetabulum, and there are early osteoarthritic changes in the joint. Both acetabula are poorly developed, and their slope is markedly increased.

There are widespread cystic changes in both femora and the pelvis.
Diagnosis: in this case the abnormal appearances are due to hyperparathyroidism.

This radiograph of the pelvis of an adolescent boy shows gross destruction of the right hip joint, with changes in both the head of the femur and the acetabulum.
Diagnosis: the appearances are typical of an infective arthritis. In this case the organism was the tubercle bacillus.

This lateral projection of the hip shows displacement of the proximal femoral epiphysis relative to the femoral neck.

The pointer marks a ringed area of bone in the femoral neck with a central nidus. This was the source of chronic, niggling bone pain.
Diagnosis: the history and X-ray appearance are typical of osteoid osteoma.

The complaint is of pain and stiffness of the hip following a hip fracture 2 years previously. The fracture was treated by nailing; the internal fixation device was subsequently removed, and there are some very minor changes only in bone texture to show its previous presence.
Diagnosis: collapse of the femoral head due to avascular necrosis. There are secondary osteoarthritic changes in the hip.

There is marked disturbance of the bony texture, mainly involving the right hemipelvis. There is a degree of protrusio acetabuli, and there is disturbance of the architecture of the hemipelvis, which is becoming centrally displaced.

The epiphysis of the right femoral head is small and of increased density. There is some broadening of the metaphysis, and there are some cystic changes in the roof of the acetabulum.

There is increased density of the capital epiphysis and some cystic change in the metaphysis, which is showing signs of broadening. There are also some cystic changes in the outer half of the acetabulum. The area of sclerosis along the inferior margin of the cyst is sometimes referred to as the ‘sagging rope’ sign.

There is separation and collapse of the lateral part of the epiphysis, with distortion of the epiphyseal plate and cystic changes in the metaphysis, which is broadened. The bone density, which was previously increased, is returning to normal.
Diagnosis: long-established Perthes’ disease. This would be described as grade C in the Herring classification of Perthes’ disease.

There are widespread changes in bone texture in the femur and pelvis, both having a moth-eaten appearance.
1. Stulberg S D, Cooperman D R, Wallenstein R. The natural history of Legg–Calvé–Perthes disease. J Bone Joint Surg Am. 1981;63:1095-1108.
2. Whitehouse S L, Lingard E A, Katz J N, Learmonth I D. Development and testing of a reduced WOMAC function scale. J Bone Joint Surg. 2003;85:706-709.
3. Harris W H. Traumatic arthritis of the hip. J Bone Joint Surg. 1969;81:737-755.