| Topical therapy |
|
 Fusidic acid or mupirocin for Staphylococcus aureus Fusidic acid or mupirocin for Staphylococcus aureus |
A |
 Retapamulin for Staphylococcus aureus Retapamulin for Staphylococcus aureus |
B |
 Mupirocin for eradication of S. aureus colonization of the nares; tea tree oil soap or body wash for body Mupirocin for eradication of S. aureus colonization of the nares; tea tree oil soap or body wash for body |
B |
 Povidone-iodine, acetic acid or gentamicin for P. aeruginosa Povidone-iodine, acetic acid or gentamicin for P. aeruginosa |
A |
 Permethrin cream for Demodex spp. Permethrin cream for Demodex spp. |
D |
 Metronidazole cream or gel for Demodex spp. Metronidazole cream or gel for Demodex spp. |
D |
 Corticosteroid for eosinophilic pustular folliculitis Corticosteroid for eosinophilic pustular folliculitis |
C |
 Tacrolimus for eosinophilic pustular folliculitis Tacrolimus for eosinophilic pustular folliculitis |
D |
| Oral therapy |
|
 Co-trimoxazole, clindamycin, doxycycline, fusidic acid for Staphylococcus spp. Co-trimoxazole, clindamycin, doxycycline, fusidic acid for Staphylococcus spp. |
B |
 Ciprofloxacin for Pseudomonas folliculitis Ciprofloxacin for Pseudomonas folliculitis |
C |
 Itraconazole for Pityrosporum spp. Itraconazole for Pityrosporum spp. |
C |
 Ivermectin or metronidazole for Demodex spp. Ivermectin or metronidazole for Demodex spp. |
D |
 Indometacin or cyclosporine for eosinophilic pustular folliculitis Indometacin or cyclosporine for eosinophilic pustular folliculitis |
B |
 Tetracycline for EGFR inhibitor-induced folliculitis Tetracycline for EGFR inhibitor-induced folliculitis |
B |







 Fusidic acid or mupirocin for Staphylococcus aureus
Fusidic acid or mupirocin for Staphylococcus aureus Retapamulin for Staphylococcus aureus
Retapamulin for Staphylococcus aureus Mupirocin for eradication of S. aureus colonization of the nares; tea tree oil soap or body wash for body
Mupirocin for eradication of S. aureus colonization of the nares; tea tree oil soap or body wash for body Povidone-iodine, acetic acid or gentamicin for P. aeruginosa
Povidone-iodine, acetic acid or gentamicin for P. aeruginosa Permethrin cream for Demodex spp.
Permethrin cream for Demodex spp. Metronidazole cream or gel for Demodex spp.
Metronidazole cream or gel for Demodex spp. Corticosteroid for eosinophilic pustular folliculitis
Corticosteroid for eosinophilic pustular folliculitis Tacrolimus for eosinophilic pustular folliculitis
Tacrolimus for eosinophilic pustular folliculitis Co-trimoxazole, clindamycin, doxycycline, fusidic acid for Staphylococcus spp.
Co-trimoxazole, clindamycin, doxycycline, fusidic acid for Staphylococcus spp. Ciprofloxacin for Pseudomonas folliculitis
Ciprofloxacin for Pseudomonas folliculitis Itraconazole for Pityrosporum spp.
Itraconazole for Pityrosporum spp. Ivermectin or metronidazole for Demodex spp.
Ivermectin or metronidazole for Demodex spp. Indometacin or cyclosporine for eosinophilic pustular folliculitis
Indometacin or cyclosporine for eosinophilic pustular folliculitis Tetracycline for EGFR inhibitor-induced folliculitis
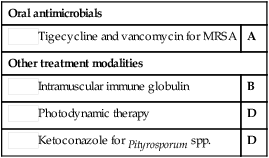
Tetracycline for EGFR inhibitor-induced folliculitis Tigecycline and vancomycin for MRSA
Tigecycline and vancomycin for MRSA Intramuscular immune globulin
Intramuscular immune globulin Photodynamic therapy
Photodynamic therapy Ketoconazole for Pityrosporum spp.
Ketoconazole for Pityrosporum spp.