Chapter 75 Electrical safety and injuries
Patients suffering from the consequences of electrocution and associated burns occasionally require intensive care unit (ICU) management. Patients and staff in the ICU are at risk of electrocution from faulty electrical equipment. The necessity of direct patient contact with electrical equipment increases this risk, and when therapy involves an invasive contact close to the heart, microshock is an additional hazard. Faulty electrical equipment can also result in power failures, fires and explosions. The use of mobile phones and related devices nearby patient equipment can lead to malfunctioning.
PHYSICAL CONCEPTS
A current flowing in a circuit produces electric and magnetic fields, which induce currents to flow in neighbouring circuits. When this results in a current flowing between the two circuits, it is called coupling. With capacitive coupling, high frequency currents are most easily passed, and the size of the current is greatest when the circuits are close. Inductive coupling can result from the strong magnetic fields produced by heavy duty electrical equipment, such as transformers, electric motors and magnetic resonance imaging machines. The most common problem associated with coupling is electrical interference or ‘noise’. Monitoring equipment is designed to ‘filter’ out this noise. However, in certain circumstances, such as the use of high frequency surgical diathermy and magnetic resonance, sufficient amperage can be induced to cause microshock and burns.1,2 Smaller electromagnetic fields emitted by hand-held devices, such as mobile phones, can affect the programming of microprocessors. Cases of patient equipment malfunctions have been reported.3
Static electricity has no free flow of electrons. Insulated objects can become highly charged, usually by repeated rubbing. The charge is dissipated by electrons jumping onto another neighbouring object of a different potential. ‘Jumping’ electrons ionise and heat the air through which they pass, causing a spark which may ignite an inflammable liquid or gas. Lightning is a type of static electrical discharge. Direct currents of 12 000–200 000 A and voltages in the millions are involved; however, flow lasts only a fraction of a second.4
PHYSIOLOGICAL CONSIDERATIONS
For a current to flow through the body, the body must complete a circuit. Usually this involves the current flowing from its source to ground through the body. The pathophysiological effects depend on the size of the current, and this depends on the voltage and electrical resistance of the body, most of which occurs in the skin. Dry skin has a resistance in excess of 100 000 O.5 However, skin resistance is markedly reduced (to 1000 O)6 if the skin is wet, or if a conductive jelly has been applied. Hence, fromOhm’s law, dry skin in contact with 240 V mains supply will result in a harmless 0.24 mA current flowing through the body, whereas moist or wet skin will result in a potentially lethal 240 mA current.
ELECTROCUTION
Most cases of electrocution occur in the workplace (about 60%) or at home (about 30%), where misuse of extension cables is the main culprit.6 Pathophysiological processes involved in true electrical injuries are poorly understood. The extent of injury depends on (i) the amount of current that passes through the body, (ii) the duration of the current, and (iii) the tissues traversed by the current (Table 75.1).
Table 75.1 Origin and pathophysiological effects of different levels of electrical injury
| Current (A) | Source | Effects on victim |
|---|---|---|
| 10–100 μA | Earth leakage | Microshock (ventricular fibrillation) |
| 300–400 μA | Faulty equipment | Tingling (harmless) |
| > 1 mA | Faulty equipment | Pain (withdraw) |
| > 10 mA | Faulty equipment | Tetany (cannot let go) |
| > 100 mA | Faulty equipment | Macroshock (ventricular fibrillation) |
| > 1 A | Faulty equipment | Burns and tissue damage |
| > 1000 A | High tension injury | Severe burns and loss of limbs |
| > 12 000 A | Lightning | Coma, severe burns and loss of limbs |
TISSUE HEAT INJURY
Currents in excess of 1 A generate sufficient heat energy to cause burns to the skin and occult thermal injury to internal tissues and organs. Blood vessels and nervous tissue appear to be particularly susceptible.6
DEPOLARISATION OF MUSCLE CELLS
An alternating current of 30–200 mA will cause ventricular fibrillation.7 Currents in excess of 5 A cause sustained cardiac asystole, which is the principle used in defibrillation. Apart from ventricular fibrillation, other arrhythmias may occur. Myocardial damage is common and may result in ST and T-wave changes. Global left ventricular dysfunction may occur hours or days later, despite initial minimal ECG changes.8,9 Myocardial infarction has also been reported.10 Specific markers of myocardial injury, such as cardiac troponin, should be checked in all suspected cases of electrical injury to the heart.11
Tetanic contractions of skeletal muscle occur with currents in excess of 15–20 mA. The threshold is particularly low with alternating currents at the household frequency of 50–60 Hz. Tetanic contraction will prevent voluntary release of the source of electrocution, and violent muscle contractions may cause fractures of long bones and spinal vertebrae.6
VASCULAR INJURIES
Blood vessels may become thrombosed and occluded as a result of the thermal injury. Compartment syndromes are seen secondary to tissue oedema, causing tissue ischaemia and necrosis. Affected limbs may even require amputation.12
NEUROLOGICAL INJURIES
Neurological injuries may be central or peripheral, and immediate or late in onset. Monoparesis may occur in affected limbs, and the median nerve is particularly vulnerable.6,13 Electrocution to the head may result in unconsciousness, paralysis of the respiratory centre, and late complications such as epilepsy, encephalopathy and parkinsonism.6,13 Spinal cord damage resulting in para- or tetraplegia can result from a current traversing both arms.6,13 Autonomic dysfunction may also occur, causing acute vasospasm or a late sympathetic dystrophy.6
MICROSHOCK
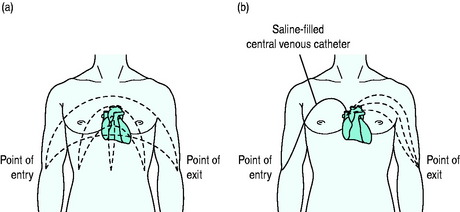
The above domestic/industrial electrocution is known as macroshock, when current flowing through the intact skin and body passes through the heart. In the ICU, potential microshock electrocution exists. Microshock occurs when there is a direct current path to the heart muscle. The pathway may be provided by a saline-filledmonitoring catheter, pulmonary artery catheter, or transvenous pacemaker wires. The current required to produce ventricular fibrillation in microshock is extremely small, in the order of 60 mA.15 Currents of 1–2 mA are barely perceptible and produce tingling of the skin (Table 75.1). Hence a lethal microshock may be transmitted to a patient via a staff member who is unaware of the conducted current. Microshock can result from direct contact with faulty electrical equipment, stray currents from capacitive coupling or earth leakage. Such small currents are potentially lethal because a high current density is produced at the heart (Figure 75.1).
HIGH TENSION AND LIGHTNING INJURIES
High tension electricity (> 1000 V) involves voltage much greater than domestic supply, usually many thousands of volts. Tissue damage is mainly due to the generation of heat, as high amperage currents are involved. Witnesses have described tissues actually exploding.16
Lightning injury is a type of high tension injury. It is rare and its incidence depends upon geographic location. Victims can be thrown several feet as a result of violent muscular contractions. Electrical arcing of the air causes intense heat, resulting in superficial burns and clothes igniting. Characteristic entrance and exit site burns are seen, which have a spider-like appearance with redness and blistering. Victims are usually unconscious in the initial phase. However, many victims survive,4 and good recovery has been reported despite initial hopeless neurological responsiveness (e.g. fixed dilated pupils).17 Immediate death usually results from cardiorespiratory arrest; asystole is more common than ventricular fibrillation.4
MANAGEMENT OF ELECTRICAL INJURIES
Treatment of electrical injuries is mainly supportive and includes the following.
INVESTIGATIONS
Investigations are indicated to detect damaged organs. They include ECG, echocardiography, CT of the head, EEG, X-rays of the spine and long bones, haemoglobin, serum electrolytes, creatine kinase and urine myoglobin to assess muscle damage, and nerve conduction studies. Arteriograms may help in the decision to amputate a limb.12
ELECTRICAL HAZARDS IN ICU
MICROSHOCK CURRENTS
EARTH LEAKAGE CURRENTS
Within all pieces of electrical equipment, stray low amperage electrical currents exist that usually flow to earth, called earth leakage currents. They originate from current leaks across imperfect insulation of wires, capacitive and inductive coupling within the equipment, and coupling from electric and magnetic fields that exist in the working environment, such as the 50–60 Hz mains supply. Normally these currents are small and harmless, but they have the potential to cause microshock.
PACING WIRES AND CENTRAL VENOUS LINES
In certain circumstances, sufficient current to cause microshock can be passed by capacitive and inductive coupling to intracardiac pacing wires and central venous lines. Ventricular fibrillation has resulted from capacitive coupling with thermistor wires in a pulmonary artery catheter.1
INDUCTIVE CURRENTS
Inductive coupling from the strong magnetic fields produced by magnetic resonance imaging can cause overheating of wires and equipment. Severe burns have resulted from the use of pulse oximetry during magnetic resonance imaging, and specially designed wiring and probes are recommended.2 Similar problems can exist with any intravascular device containing wires, such as a pulmonary artery catheter. More recently, problems have arisen from the interference caused by personal computers, mobile phones and related devices with patient equipment. Many hospitals have banned the use of such devices in areas where patients are treated.
ELECTRICAL SAFETY STANDARDS
Most Western countries have standards of electrical safety that apply to the use of medical equipment. For example, Australian Standards (AS 3003 and AS 3200) set minimum requirements for Australian hospitals. AS 2500 covers the safe use of electricity in patient care areas.18 Britain and Europe follow the International Electrotechnical Commission Code19,20 and the USA follows the National Electric Code 1993.21 These standards have not changed significantly over the last few decades and are now easily accessible on the internet. Hospitals should establish their own committees to ensure that adequate standards are applied. However, patient care areas differ in their safety requirements and commonly used classifications are listed below. The ICU should conform to (1b) and preferably (1c).
MEASURES TO PROTECT STAFF AND PATIENTS22,23
POWER SUPPLY ISOLATION
MAINS ISOLATION
The power supply is isolated from earth using a mains isolation transformer. If contact is made with live faultycircuitry, the risk of electric shock is reduced because stray currents no longer preferentially flow through patient or staff member to earth. Presence of stray earth leakage currents can be detected by using a line isolation monitor. This type of system is particularly useful in wet locations where the body may offer a very low resistance to earth.
1 McNulty SE, Cooper M, Staudt S. Transmitted radiofrequency current through a flow directed pulmonary artery catheter. Anesth Analg. 1994;78:587-589.
2 Peden CJ, Menon DK, Hall AS, et al. Magnetic resonance for the anaesthetist. Anaesthesia. 1992;47:508-517.
3 Hayes DL, Carrillo RG, Findlay GK, et al. State of the science: pacemaker and defibrillator interference from wireless communication devices. Pacing Clin Electrophysiol. 1996;19:1407-1409.
4 Apfelberg DB, Masters FW, Robinson DW. Pathophysiology and treatment of lightning injuries. J Trauma. 1974;14:453-460.
5 Bruner JMR. Hazards of electrical apparatus. Anesthesiology. 1976;28:396-424.
6 Fontneau NM, Mitchell A. Miscellaneous neurologic problems in the intensive care unit. In: Irwin RS, Cerra FB, Rippe JM, editors. Intensive Care Medicine. 4th edn. Philadelphia: Lippincott-Raven; 1999:2127-2135.
7 Loughman J, Watson AB. Electrical safety in hospitals and proposed standards. Med J Aust. 1971;2:349-355.
8 Lewin RF, Arditti A, Sclarovsky S. Non-invasive evaluation of cardiac injury. Br Heart J. 1983;49:190-192.
9 Jensen PJ, Thomsem PEB, Bagger JP, et al. Electrical injury causing ventricular arrhythmias. Br Heart J. 1987;57:279-283.
10 Walton AS, Harper RW, Coggins GL. Myocardial infarction after electrocution. Med J Aust. 1988;148:365-367.
11 Karras DJ, Kane DL. Serum markers in the emergency department diagnosis of acute myocardial infarction. Emerg Med Clin North Am. 2001;19:321-337.
12 Hunt JL, McManus WF, Haney WP, et al. Vascular lesions in acute electric injuries. J Trauma. 1974;14:461-473.
13 Solem L, Fischer RP, Strate RG. The natural history of electrical injury. J Trauma. 1977;17:487-492.
14 Ogren FP, Edmunds AL. Neuro-otologic findings in the lightning-injured patient. Semin Neurol. 1995;15:256-262.
15 Watson AB, Wright JS, Loughman J. Electrical thresholds for ventricular fibrillation in man. Med J Aust. 1973;1:1179-1182.
16 Burke JF, Quinby WC, Bondoc C, et al. Patterns of high tension electric injury in children and adolescents and their management. Am J Surg. 1977;133:492-494.
17 Hanson GC, McIlwaith GR. Lightning injury: two case histories and a review of management. Br Med J. 1973;4:271-274.
18 Australian Standard 2500. Guide to the Safe Use of Electricity in Patient Care. Sydney: Standards Association of Australia, 1988.
19 CEI-IEC 601-1&2. Medical Electrical Equipment, 2nd edn., Geneva: International Electrotechnical Commission, 1988.
20 Herrmann D. A preview of IEC safety requirements for programmable electronic medical systems. Med Dev Diag Indust. 1995;17:106-111.
21 Early MW, Murray RH, Caloggero JM. National Electrical Code Handbook, 6th edn., Quincy: National Fire Protection Association, 1993.
22 Litt L, Ehrenwerth J. Electrical safety in the operating room: important old wine, disguised new bottles. Anesth Analg. 1994;78:417-419.
23 Ehrenwerth J. Electrical Safety in and around the Operating Room. Philadelphia: JB Lippincott, 1994;123. ASA Refresher Course in Anesthesia