Chapter 302 Cleft Lip and Palate
Incidence and Epidemiology
The incidence of cleft lip with or without cleft palate is ∼1/750 white births; the incidence of cleft palate alone is ∼1/2,500 white births. Clefts of the lip are more common in males. Possible causes include maternal drug exposure, a syndrome-malformation complex, or genetic factors. Although both appear to occur sporadically, the presence of susceptibility genes appears important. There are ∼400 syndromes associated with cleft lip and palates. There are families in which a cleft lip or palate, or both, is inherited in a dominant fashion (van der Woude syndrome), and careful examination of parents is important to distinguish this type from others, because the recurrence risk is 50%. The IRF6 gene is responsible for the van der Woude syndrome and some cases of nonsyndromic clefts. The severity of the disease is independent of predisposing genes. Ethnic factors also affect the incidence of cleft lip and palate; the incidence is highest among Asians (∼1/500) and Native Americans (∼1/300), and lowest among blacks (∼1/2500). The incidence of associated congenital malformations (chromosomal aneuploidy, holoprosencephaly) and of impairment in development is increased in children with cleft defects, especially in those with cleft palate alone. The risks of recurrence of cleft defects within families were discussed in Chapters 72 and 75.
Clinical Manifestations
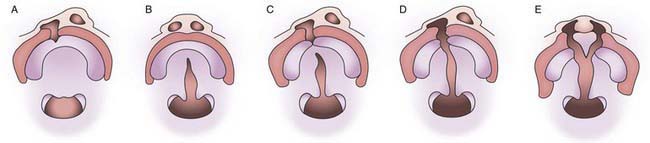
Cleft lip can vary from a small notch in the vermilion border to a complete separation involving skin, muscle, mucosa, tooth, and bone. Clefts may be unilateral (more often on the left side) or bilateral and can involve the alveolar ridge (Fig. 302-1).
Birnbaum S, Ludwig K, Reutter H, et al. Key susceptibility locus for nonsyndromic cleft lip with or without cleft palate on chromosome 8q24. Nat Genetics. 2009;41:473-477.
Grant SFA, Wang K, Zhang H, et al. A genome-wide association study identifies a locus for nonsyndromic cleft lip with or without cleft palate on 8q24. J Pediatr. 2009;155:909-913.
Kasten EF, Schmidt SP, Zickler CF, et al. Team care of the patient with cleft lip and palate. Curr Prob Pediatr Adolesc Health Care. 2008;38:133-164.
Mossey PA, Little J, Munger RG, et al. Cleft lip and palate. Lancet. 2009;374:1773-1782.
Sell D, Ma L. A model of practice for the management of velopharyngeal dysfunction. Br J Oral Maxillofacial Surg. 1996;34:357-363.
Sivertsen A, Wilcox AJ, Skjaerven R, et al. Familial risk of oral clefts by morphological type and severity: population based cohort study of first degree relatives. BMJ. 2008;336:432-434.
Tollefson TT, Senders CW, Sykes JM. Changing perspectives in cleft lip and palate. Arch Facial Plast Surg. 2008;10:395-400.