Cardiopulmonary Rehabilitation
After reading this chapter you will be able to:
 State the definition and general goals of pulmonary rehabilitation programs.
State the definition and general goals of pulmonary rehabilitation programs.
 Explain the rationale for exercise conditioning and psychosocial support of patients with chronic pulmonary disease.
Explain the rationale for exercise conditioning and psychosocial support of patients with chronic pulmonary disease.
 Describe how to evaluate and select patients for pulmonary rehabilitation.
Describe how to evaluate and select patients for pulmonary rehabilitation.
 Describe pulmonary rehabilitation program design including format and content.
Describe pulmonary rehabilitation program design including format and content.
 List the educational content to be addressed in a pulmonary rehabilitation program.
List the educational content to be addressed in a pulmonary rehabilitation program.
 Describe the implementation of a pulmonary rehabilitation program, including staffing, facilities, scheduling, class size, equipment, costs, and reimbursement.
Describe the implementation of a pulmonary rehabilitation program, including staffing, facilities, scheduling, class size, equipment, costs, and reimbursement.
 Discuss the outcome measures that can be used to evaluate pulmonary rehabilitation programs.
Discuss the outcome measures that can be used to evaluate pulmonary rehabilitation programs.
 Identify the potential hazards associated with pulmonary rehabilitation.
Identify the potential hazards associated with pulmonary rehabilitation.
Steady improvements in acute care are presenting new medical and social problems. As more patients survive acute illnesses, there are increasing numbers of individuals with chronic disorders. These chronic disorders are associated with a wide spectrum of physiologic, psychologic, and social disabilities. Foremost among these individuals with chronic disorders are individuals with chronic cardiopulmonary disease. Chronic obstructive pulmonary disease (COPD) is expected to be the third leading cause of death in the United States by 2020.1
Definitions and Goals
The Council on Rehabilitation defines rehabilitation as “the restoration of the individual to the fullest medical, mental, emotional, social, and vocational potential of which he or she is capable.”2 The overall goal is to maximize functional ability and to minimize the impact the disability has on the individual, the family, and the community. Pulmonary rehabilitation is the “art of medical practice wherein an individually tailored, multidisciplinary program is formulated, which through accurate diagnosis, therapy, emotional support, and education stabilizes or reverses both the physio- and psychopathology of pulmonary diseases and attempts to return the patient to the highest possible functional capacity allowed by his or her pulmonary handicap and overall life situation.”3
The general goals of pulmonary rehabilitation are to control and alleviate symptoms, restore functional capabilities as much as possible, and improve quality of life.4 Pulmonary rehabilitation does not reverse or stop progression of the disease, but it can improve a patient’s overall quality of life. Health care providers from various disciplines are needed to reach these goals.
Historical Perspective
Pulmonary rehabilitation is not a new concept. In 1952, Barach and colleagues5 recommended reconditioning programs for patients with chronic lung disease to help improve their ability to walk without dyspnea. Decades passed before clinicians paid any attention to this concept. Instead of having their patients participate in reconditioning programs, most physicians simply prescribed oxygen (O2) therapy and bed rest. The result was a vicious cycle of skeletal muscle deterioration, progressive weakness and fatigue, and increasing levels of dyspnea including at rest. Patients became homebound, then room-bound, and eventually bed-bound. Improved avenues of therapy and rehabilitation were needed.
In 1962, Pierce and associates6 published results confirming Barach’s insight into the value of reconditioning. They observed that patients with COPD who participated in physical reconditioning exhibited lower pulse rates, respiratory rates, minute volumes, and carbon dioxide (CO2) production during exercise. However, they also found that these benefits occurred without significant changes in pulmonary function. Soon thereafter, Paez and associates7 showed that reconditioning could improve both the efficiency of motion and O2 use in patients with COPD. Subsequently, Christie8 showed that the benefits of reconditioning could be achieved on an outpatient basis with minimal supervision. Since Christie’s work in 1968, other investigators have continued to research the benefits of pulmonary rehabilitation.
The available evidence at the present time consistently indicates that pulmonary rehabilitation benefits patients with chronic obstructive and restrictive pulmonary disease.9–12 When combined with smoking cessation, optimization of blood gases, and proper medication use, pulmonary rehabilitation offers the best treatment option for patients with symptomatic pulmonary disease. Programs for pulmonary rehabilitation must be founded on the sound application of current knowledge in the clinical and social sciences. In fall 2006, the American College of Chest Physicians (ACCP) and the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) released their evidence-based guidelines relating to pulmonary rehabilitation aimed at improving the way pulmonary rehabilitation programs are designed, implemented, and evaluated through patient outcomes.13
Scientific Basis
Physical Reconditioning
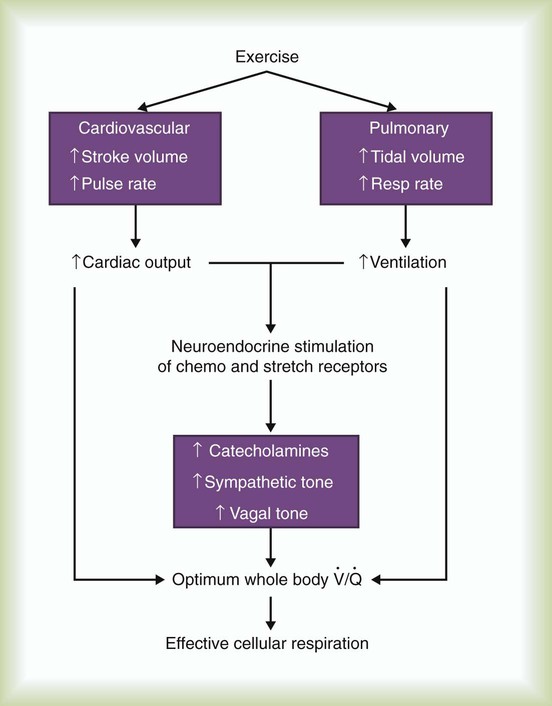
At rest, an individual maintains homeostasis by balancing external, internal, and cellular respiration. Physical activity, such as exercise, increases energy demands. To maintain homeostasis during exercise, the cardiorespiratory system must keep pace. Figure 50-1 shows how the body responds to exercise. Ventilation and circulation increase to supply tissues and cells with additional O2 and to eliminate the higher levels of CO2 produced by metabolism.
As depicted in Figure 50-2, O2 consumption and CO2 production also increase in linear fashion as exercise intensity increases. If the body cannot deliver sufficient O2 to meet the demands of energy metabolism, blood lactate levels increase above normal. In exercise physiology, this point is called the onset of blood lactate accumulation (OBLA). As this excess lactic acid is buffered, CO2 levels increase, and the stimulus to breathe increases. The result is an abrupt upswing in both CO2 and  (referred to as the ventilatory threshold). Beyond this point, metabolism becomes anaerobic, the efficiency of energy production decreases, lactic acid accumulates, and fatigue sets in.
(referred to as the ventilatory threshold). Beyond this point, metabolism becomes anaerobic, the efficiency of energy production decreases, lactic acid accumulates, and fatigue sets in.
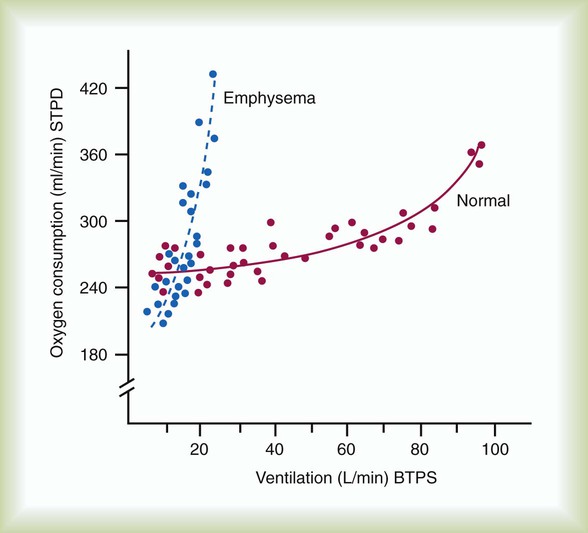
Patients with COPD who lack adequate pulmonary function have severe limitations to their exercise capabilities. Their high rate of CO2 production during exercise results in respiratory acidosis and a shortness of breath out of proportion to the level of activity. In addition, as ventilation increases, the rate of O2 consumption in a patient with COPD increases significantly (Figure 50-3). Together, these factors limit patient tolerance for any significant increase in physical activity.
Pulmonary rehabilitation must include efforts to recondition patients physically and increase their exercise tolerance. Reconditioning involves strengthening essential muscle groups, improving overall O2 use, and enhancing the body’s cardiovascular response to physical activity (Box 50-1).
Psychosocial Support
If the overall goal of pulmonary rehabilitation is to improve the quality of patients’ lives, physical reconditioning alone is insufficient. Psychosocial indicators generally are good predictors of morbidity in patients with COPD. Studies show that the relative success of reconditioning plays less of a role in determining whether patients complete a program than meeting their psychosocial support needs.14
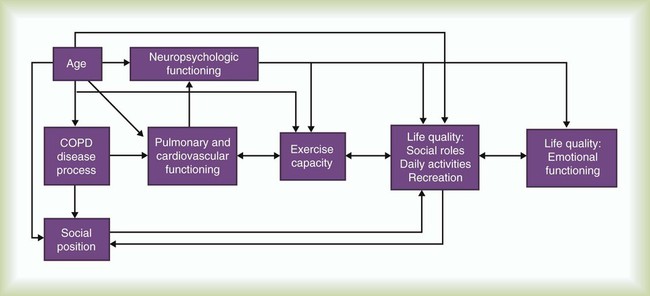
Figure 50-4 presents elements of how chronic lung disease and other variables can have an impact on a patient’s quality of life. It is here that the link between the physical reconditioning and psychosocial support components of rehabilitation becomes most evident. By reducing exercise intolerance and enhancing the body’s cardiovascular response to physical activity, patients can develop a more independent and active lifestyle. For some patients, simply being able to walk to the market or play with their grandchildren can contribute to a greater feeling of social importance and self-worth. For others, physical conditioning may allow a return to near-normal levels of activity, including vocational pursuits.
Structure of A Pulmonary Rehabilitation Program
Program Goals and Objectives
Pulmonary rehabilitation programs vary in their design and implementation but generally share common goals. Examples of these common goals are listed in Box 50-2. These general goals assist planners in formulating more specific program objectives. When determining objectives, both patients and members of the rehabilitation team should have input. These objectives should always be stated in measurable terms because this helps facilitate the determination of both patient outcomes and the therapeutic success and value of pulmonary rehabilitation. Depending on the specific needs of the participants, program objectives can include the following:
• Development of diaphragmatic breathing skills
• Development of stress management and relaxation techniques
• Involvement in a daily physical exercise regimen to condition both skeletal and respiratory-related muscles
• Adherence to proper hygiene, diet, and nutrition
• Smoking cessation (if applicable)
• Proper use of medications, O2, and breathing equipment (if applicable)
• Application of airway clearance techniques (when indicated)
Patient Evaluation and Selection
Patient Evaluation
Pulmonary rehabilitation programs must have a qualified medical director, usually a pulmonologist, to provide overall medical direction of the program and to screen prospective patients.17 Patient evaluation begins with a complete patient history—medical, psychologic, vocational, and social. A well-designed patient questionnaire and interview form assist with this step. The patient history should be followed by a complete physical examination (see Chapter 15). A recent chest film, resting electrocardiogram (ECG), complete blood count, serum electrolytes, and urinalysis provide additional information on the patient’s current medical status (see Chapter 16).
To determine the patient’s cardiopulmonary status and exercise capacity, both pulmonary function testing and a cardiopulmonary exercise evaluation may be performed. Pulmonary function testing includes assessment of pulmonary ventilation, lung volume determinations, diffusing capacity (DLCO), and spirometry before and after bronchodilator use (see Chapter 19).
The cardiopulmonary exercise evaluation serves two key purposes in pulmonary rehabilitation. First, it quantifies the patient’s initial exercise capacity. This quantification provides the basis for the exercise prescription (including setting a target heart rate) and yields the baseline data for assessing a patient’s progress over time. In addition, the evaluation helps determine the degree of hypoxemia or desaturation that can occur with exercise; this provides the objective basis for titrating O2 therapy during the exercise program. To guide practitioners in implementing exercise evaluation, the American Association for Respiratory Care (AARC) has published clinical practice guidelines on exercise testing for evaluation of hypoxemia or desaturation or both18 and pulmonary rehabilitation. Excerpts from these guidelines appear in Clinical Practice Guidelines 50-1 and 50-2.19
Modified Borg Dyspnea Scale (With Dyspnea Descriptors)
| 10 | Maximal (worst possible you can imagine) |
| 9 | Very, very severe |
| 8 | Very, very severe |
| 7 | Very severe |
| 6 | Very severe |
| 5 | Severe |
| 4 | Somewhat severe |
| 3 | Moderate |
| 2 | Slight |
| 1 | Very slight |
| 0.5 | Very, very slight (just noticeable) |
| 0 | None at all |
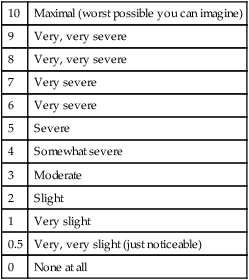
The exercise evaluation procedure involves serial or continuous measurements of several physiologic parameters during various graded levels of exercise on either an ergometer or a treadmill (Box 50-3). To allow for steady-state equilibration, these graded levels are usually spaced at 3-minute intervals. Work levels are increased progressively until either (1) the patient cannot tolerate a higher level or (2) an abnormal or hazardous response occurs.
Relative contraindications to exercise testing include the following:
• Inability or unwillingness of patient to perform the test
• Severe pulmonary hypertension or cor pulmonale
• Known electrolyte disturbances (hypokalemia, hypomagnesemia)
• Resting diastolic blood pressure greater than 110 mm Hg or resting systolic blood pressure greater than 200 mm Hg
• Neuromuscular, musculoskeletal, or rheumatoid disorders exacerbated by exercise
• Uncontrolled metabolic disease (e.g., diabetes)
• SaO2 or SpO2 less than 85% with the subject breathing room air
Exercise evaluation also can help differentiate among patients with primary respiratory or cardiac limitations to increased work capacity. Table 50-1 summarizes these key similarities and differences. Besides helping to differentiate between the underlying cause of exercise intolerance, test results can assist in placing patients in the appropriate type of rehabilitation program.
TABLE 50-1
| Parameter* | Cardiac† | COPD† |
Maximum  |
↓ | ↓ |
| Maximum HR | N or ↓ | ↓ |
| O2 pulse | ↓ | N |
Maximum  |
↓ | ↓ |
 |
↓ | N |
| PaO2 | N | ↓ |
| PaCO2 | ↓ | ↑ |
 |
↑ | ↑ |
| VT | ↓ | N |
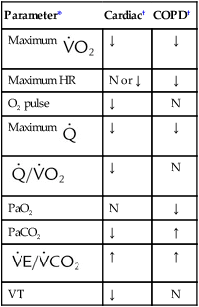
*HR, Heart rate;  , cardiac output;
, cardiac output;  , ratio of ventilation to CO2 production;
, ratio of ventilation to CO2 production;  , oxygen consumption; VT, ventilatory threshold.
, oxygen consumption; VT, ventilatory threshold.
†N, Normal; ↑, increased; ↓, decreased.
Modified from Lane EE, Walker JF: Clinical arterial blood gas analysis, St Louis, 1987, Mosby.
Patient Selection
Patients most likely to benefit from participation in pulmonary rehabilitation are patients with persistent symptoms caused by COPD who have low maximum O2 uptakes at baseline. Pulmonary rehabilitation should be a part of the discharge planning process when a patient is released from the hospital after an exacerbation of the existing chronic respiratory condition. The feasibility of rehabilitation should be reviewed with the patient, physician, and respiratory therapist (RT). Other indications for pulmonary rehabilitation are listed in Box 50-4. Regardless of underlying conditions, patients also should be ex-smokers. Any patients who smoke should enroll in a smoking cessation program before starting pulmonary rehabilitation. Patients are excluded from pulmonary rehabilitation activities if (1) concurrent problems limit or preclude participation in exercise or (2) their condition is complicated by malignant neoplasms, such as lung cancer (see Box 50-4).
Objectively, candidates considered for inclusion in a pulmonary rehabilitation program generally fall into one of the following groups:20
• Patients in whom there is a respiratory limitation to exercise resulting in termination at a level less than 75% of the predicted maximum O2 consumption ( )
)
• Patients in whom there is significant irreversible airway obstruction with a forced expiratory volume in 1 second (FEV1) of less than 2 L or an FEV1% (ratio of FEV1 to forced vital capacity [FVC]) of less than 60% (consider the Global Initiative on Obstructive Lung Disease [GOLD] standards for COPD severity here)
• Patients in whom there is significant restrictive lung disease with a total lung capacity (TLC) of less than 80% of predicted and single breath carbon monoxide diffusing capacity (DLCO) of less than 80% of predicted
• Patients with pulmonary vascular disease in whom single breath DLCO is less than 80% of predicted or in whom exercise is limited to less than 75% of maximum predicted O2 consumption (predicted  )
)
Program Design
Format
Regardless of the format used, long-term improvements cannot be expected without planned follow-up.21 Follow-up must be ongoing and available to all patients who complete the program. Frequently, this essential element of the process is difficult, especially when it is not covered by most insurance plans, but program coordinators must ensure that it is routinely scheduled. Follow-up or reinforcement could be open-ended (available during regular rehabilitation sessions and offering open attendance) or could be scheduled weekly, monthly, bimonthly, or quarterly. The important thing is to have some type of follow-up available.22,23
Content
The content of the rehabilitation program usually combines physical reconditioning with education activities. Table 50-2 outlines a sample session incorporating these two complementary components. Programs providing reconditioning or education alone are unlikely to be effective.
TABLE 50-2
Sample Pulmonary Rehabilitation Session
| Component | Focus | Time Frame |
| Educational | Welcome (group interaction) | 5 min |
| Review of program diaries (activities of past week) | 20 min | |
| Presentation of educational topic | 20 min | |
| Questions, answers, and group discussion | 15 min | |
| Physical reconditioning | Physical activity and reconditioning | 45 min |
| Individual goal setting and session summary | 15 min | |
| Total session | 120 min (2 hr) |
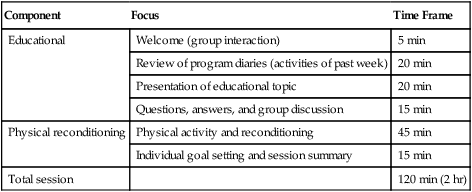
As shown in Table 50-2, the ideal rehabilitation session should last about 2 hours. Group size, available equipment, and group interaction dictate session length. Patients should arrive 10 to 15 minutes before a scheduled session to allow for informal group interaction and support. Classes should begin on time and conclude promptly as scheduled. Educational presentations should be brief and to the point. The use of audiovisuals or demonstrations should enhance understanding. To facilitate patient comprehension, the language should be simple, and unnecessary technical terms or concepts should be avoided. Handouts that enhance certain points made during a presentation are both useful and desirable. A folder or notebook in which program activities may be recorded and handout materials kept should be maintained by each patient.
Physical Reconditioning
Typically, the exercise prescription includes the following four related components:24,25
1. Lower extremity (leg) aerobic exercises
2. Timed walking (6- or 12-minute walk)
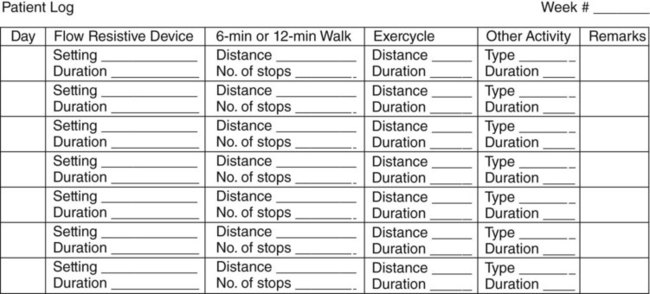
To ensure compliance with the program, a daily log or diary sheet is completed. Figure 50-5 depicts a sample log sheet that makes up a section of the patient manual. These log or diary forms are reviewed each time the patient attends a session. Based on this information, further individualized reconditioning goals are set.
Aerobic upper extremity exercises improve rehabilitation outcomes for patients whose regular activities involve lifting or raising the arms.24,26 Arm ergometers or rowing machines are available for this purpose; however, simple calisthenics using either a broomstick or free weights (by prescription and with training) are a satisfactory alternative. Upper body endurance generally is more limited, with many patients capable of only 2 to 3 minutes of daily activity to start. This limitation usually is related to the fact that patients may revert to using accessory muscles for breathing while doing the upper body exercise. Patients need to breathe diaphragmatically and perform the exercises at the same time. Arm exercises should get progressively longer, up to 20 minutes if possible. Upper body conditioning helps patients perform numerous useful activities at home and can increase overall physical endurance. As with other activity, patients should record daily results in their logs or manuals.
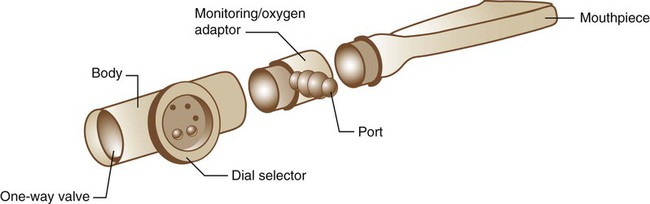
Although controversy exists, ventilatory muscle training probably can enhance the benefits of these more traditional exercises.27 Ventilatory muscle training is based on the concept of progressive resistance. By imposing progressively greater loads on the inspiratory muscles (mainly the diaphragm) over time, the patient’s strength and endurance should increase. These improvements should increase the patient’s exercise tolerance.
Figure 50-6 shows a typical inspiratory resistance breathing device. The device is an adjustable flow resistor with a one-way breathing valve. The inspiratory load is created by forcing the patient to inhale through a restricted orifice. Varying the size of this orifice varies the inspiratory load, as do changes in the patient’s inspiratory flow. During expiration, gas flows unimpeded out the one-way exhalation valve. Other types of devices are also available. One model replaces the variable size orifice with an adjustable spring-loaded valve. This valve ensures a constant load regardless of how quickly or slowly the patient breathes.
Because variations in breathing strategy during ventilatory muscle training can affect outcomes, proper patient evaluation, training, and follow-up are required. The RT initially measures the patient’s maximum inspiratory pressure (PImax) using a calibrated pressure manometer. The RT next compares the patient’s maximum with established norms (Table 50-3). This preliminary measure of inspiratory pressure helps to establish initial loads and provides the basis for the subsequent monitoring of patient progress.
TABLE 50-3
Normal Maximum Inspiratory Pressure by Age and Sex
| pimax from residual volume (cm h2o), mean ± sd | ||
| Age Group (yr) | Male | Female |
| 9-18 | 96 ± 35 | 90 ± 25 |
| 19-50 | 127 ± 28 | 91 ± 25 |
| 51-70 | 112 ± 20 | 77 ± 18 |
| >70 | 76 ± 27 | 66 ± 18 |
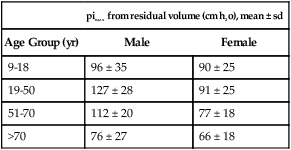
From Rochester DF, Hyatt RE: Respiratory muscle failure, Med Clin North Am 67:573, 1983.
Educational Component
The educational portion of the program covers topics that are both useful and necessary to the patient. Table 50-4 lists examples of topics covered during a 12-week rehabilitation program. Recommendations regarding the best facilitators for each session are included. Naturally, other topics can be included depending on the program schedule, but in terms of relative importance, the ones listed in Table 50-4 generally have the highest priority.
TABLE 50-4
Typical Educational Topic Schedule for a 12-Week Pulmonary Rehabilitation Program
| Session (Week) | Topic(s) | Recommended Facilitator(s) |
| 1 | Introduction and welcome; program orientation | Program administrator or rehabilitation team |
| 2 | Respiratory structure, function, and pathology | Physician or RT |
| 3 | Breathing control methods | PT or RT |
| 4 | Relaxation and stress management | Clinical psychologist |
| 5 | Proper exercise techniques and personal routines | PT or RT |
| 6 | Methods to aid secretion clearance (bronchial hygiene) | PT or RT |
| 7 | Home oxygen and aerosol therapy | RT |
| 8 | Medications—their use and abuse | Pharmacist, physician, or nurse practitioner |
| 9 | Medications—use of MDIs and spacers | RT |
| 10 | Dietary guidelines and good nutrition | Dietitian or nutritionist |
| 11 | Recreation and vocational counseling | Occupational therapist |
| Activities of daily living | ||
| 12 | Follow-up planning and program evaluation | Rehabilitation team |
| Graduation |
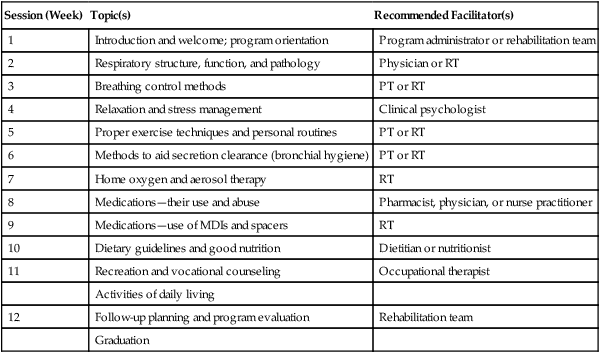
MDIs, Metered dose inhalers; PT, physical therapist; RT, respiratory therapist.
Program Implementation
In 1987, the AARC and the AACVPR jointly conducted the first national survey of pulmonary rehabilitation programs. This National Pulmonary Rehabilitation Survey was published in 1988 and showed the variation existing in rehabilitation program structure, content, staffing, and cost throughout the United States.28 In 2006, the ACCP, in conjunction with the AACVPR, released new evidence-based guidelines pertaining to the design and implementation of pulmonary rehabilitation programs.13
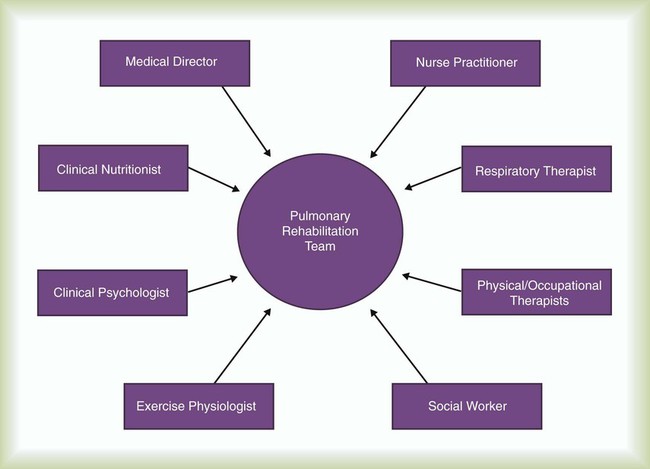
Staffing
Pulmonary rehabilitation is a multidisciplinary endeavor. Team care is enhanced by involving various health care professionals in the planning, implementation, and evaluation components of the program (Figure 50-7). It is recommended that any staff conducting pulmonary rehabilitation program sessions be certified in basic life support or advanced cardiac life support through the American Heart Association. In addition to professional involvement, family members are needed to provide feedback and ensure that instructions and the exercise prescription are carried out at home.
Equipment
• Maintaining individual patient manuals, including daily log forms or activity diaries
• Providing light refreshments for program participants
• Developing a communication network to announce schedule changes because of emergencies or cancellation of class sessions because of illness or weather
• Identifying available durable medical equipment providers for participants in need of specialized home care equipment
• Developing a system of charges and mechanism for patient payment
Cost, Fees, and Reimbursement
Rehabilitation programs usually project their fees based on the average cost per participant. According to regional labor and material prices, costs vary throughout the United States. Several factors must be considered when projecting program costs (Box 50-5). The larger the class size and the more participants involved in the overall program, the lower the cost would be per patient. The aim should be to offer and conduct the highest quality program possible at a reasonable cost that meets any existing budgetary constraints.
By following recognized guidelines, Medicare has established an allowable charge for pulmonary rehabilitation and reimburses 80% of this rate after the patient meets the annual prescribed deductible. In the past, inpatient and outpatient pulmonary rehabilitation programs obtained reimbursement from third-party payers by charging for rehabilitation sessions as physical therapy exercises for COPD, reconditioning exercise sessions, office visits with therapeutic exercises, serial pulse oximetry determinations, or physician office visits. The goal was to obtain as much insurance reimbursement as possible, decreasing the financial burden on the patient. Box 50-6 lists all possible sources of reimbursement.29,30
1. Physician-prescribed exercise, including aerobic exercise, which is performed during each session
2. Education and training that relate to an individual patient’s needs
5. Treatment plan that details how these components are used for each individual patient
At the present time, there is provision to reimburse pulmonary rehabilitation programs for two 1-hour rehabilitation sessions per patient per day up to 36 sessions. An additional 36 sessions over an extended period can be approved by the individual Medicare contractor based on patient need for continued rehabilitation and physician referral. Documentation of programs is essential for payment of services rendered. In 2010, coding for pulmonary rehabilitation under Medicare Part B uses the HCPCS G0424 code. Provision has been made for face-to-face patient sessions and for group (two or more patients) sessions. Individual sessions must be at least 31 minutes in length. If two sessions are performed on the same day, services may be reported only if the duration of the combined treatments is at least 91 minutes. It is essential that the practitioner who conducts pulmonary rehabilitation is familiar with all current practices so that therapy provided and billed for complies with current Medicare policy, is properly documented for each patient, and is submitted in a timely fashion.31,32
Program Results
Patient and program outcomes must be evaluated at the conclusion of the program and periodically thereafter (Box 50-7). Evaluation results must compare patient status before the program with current patient status and may include physiologic, psychologic, and sociologic data. Common outcome measures include exercise tolerance, levels of dyspnea at rest and with exertion, and quality-of-life surveys.
Results of pulmonary rehabilitation must be communicated to the patient, family, referring physician, and home care company, if appropriate. Further goals and objectives for continued improvement may be established to provide the basis for follow-up and reinforcement activities. Quality of life for patients with chronic lung diseases is an outcome measure that many pulmonary rehabilitation programs are documenting.33 A major predictor for improvement in health-related quality of life of a patient with COPD is frequent attendance in a maintenance program.3,34
Finally, pulmonary rehabilitation has become recognized as a prerequisite for certain patients with emphysema who are able to undergo lung volume reduction surgery. Physical reconditioning and patient education before the procedure help to increase the chances for a successful outcome. Pulmonary rehabilitation appears to have favorable results with this specific patient population because of added patient and practitioner commitment and focus. Patients who do not complete the presurgical rehabilitation protocol are at higher risk for postsurgical complications.35–38

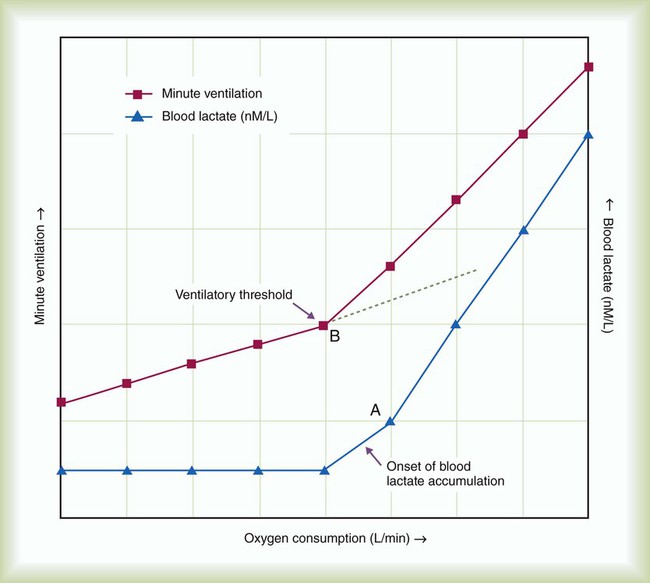
 and
and  during submaximal exercise. Point A represents OBLA. At the same time,
during submaximal exercise. Point A represents OBLA. At the same time,  and
and  “break” from their extrapolated rate of increase and abruptly rise (point B). This is referred to as the ventilatory threshold.
“break” from their extrapolated rate of increase and abruptly rise (point B). This is referred to as the ventilatory threshold. 

 )
) or METS)
or METS) )
) :heart rate)
:heart rate)