Burning mouth syndrome (glossodynia)
Cooper C. Wriston, Ashley B. Wentworth and Rochelle R. Torgerson
Specific investigations
Table 33.1
| History | |
| Oral symptoms | Timing, quality, duration, location, alleviating/exacerbating factors |
| Medications | Efavirenz, clonazepam, fluoxetine, sertraline, venlafaxine, enalapril, captopril, lisinopril, candesartan, eprosartan, omeprazole, topiramate, hormone replacement therapy |
| Dental | Prostheses, recent procedures, dentifrices, topical medicaments |
| Parafunctional habits | Bruxism, tongue thrusting |
| Review of symptoms | Weakness, headache, fatigue, concentration, sleep disturbance, arthralgia |
| Physical examination | |
| Oral | Complete oral exam, including head and neck (remove any dental prostheses) |
| Nodal | Adenopathy |
| Musculoskeletal | Temporomandibular joint |
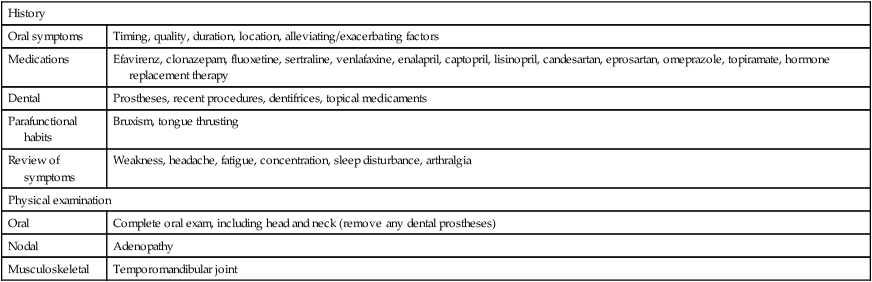
Table 33.2
| Hematologic | Complete blood count; ferritin; serum folate, cobalamin (+ methylmalonic acid, homocysteine) |
| Metabolic | Serum thiamine, riboflavin, pyridoxine, zinc (+ alkaline phosphatase), magnesium |
| Endocrinologic | Glycosylated hemoglobin, thyrotropin (+ free thyroxine) |
| Immunologic | Antinuclear factor, ( +Ro/SSA, La/SSB) |
| Dermatologic | Biopsy (+ direct immunofluorescence) if visible abnormality on oral exam |
| Microbiology testing | Herpes simplex (PCR); varicella zoster (PCR); candidosis (swab from site of pain for direct examination and culture); human immunodeficiency virus screening |
Table 33.3
| Otolaryngology | Nasopharyngoscopy |
| Gastroenterology | Esophagogastroduodenoscopy |
| Oral/maxillofacial | Periapical radiographs, magnetic resonance imaging |
| Mental health | Psychiatry consultation |
| Neurology | Neurologic examination, magnetic resonance imaging |
| Hypersensitivity testing | Epicutaneous patch testing (preservatives, oral flavors, metals, adhesives) |
First-line therapies
Second-line therapies
Third-line therapies

 Acknowledge and validate patient symptoms and experience; reassure
Acknowledge and validate patient symptoms and experience; reassure Avoid contact irritants (alcohol-based oral rinses, caustic mouthwashes, flavored dentrifices, acidic foods, carbonated beverages)
Avoid contact irritants (alcohol-based oral rinses, caustic mouthwashes, flavored dentrifices, acidic foods, carbonated beverages) Treat xerostomia (sialogogues, artificial oral lubricants)
Treat xerostomia (sialogogues, artificial oral lubricants) Discontinue or change causative medications (ACE inhibitor, ARB, SSRI, SNRI, benzodiazepine, NNRTI, PPI, anticonvulsant, anticholinergics)
Discontinue or change causative medications (ACE inhibitor, ARB, SSRI, SNRI, benzodiazepine, NNRTI, PPI, anticonvulsant, anticholinergics) Replace thiamine, riboflavin, pyridoxine, folate, cobalamin, iron, zinc, ascorbic acid, magnesium
Replace thiamine, riboflavin, pyridoxine, folate, cobalamin, iron, zinc, ascorbic acid, magnesium Manage concomitant psychiatric illness
Manage concomitant psychiatric illness Assess and address parafunctional habits (bruxism, tongue thrusting)
Assess and address parafunctional habits (bruxism, tongue thrusting) Assess oral prostheses and dental work
Assess oral prostheses and dental work Imidazole/azole therapy (presence of functional pain)
Imidazole/azole therapy (presence of functional pain) Topical capsaicin
Topical capsaicin Topical clonazepam
Topical clonazepam Low-dose clonazepam
Low-dose clonazepam Low-dose tricyclic antidepressant (doxepin)
Low-dose tricyclic antidepressant (doxepin) Paroxetine
Paroxetine Milnacipran
Milnacipran Low-dose pregabalin
Low-dose pregabalin Duloxetine
Duloxetine Low-dose olanzapine
Low-dose olanzapine Cognitive behavioral therapy
Cognitive behavioral therapy Avoid contact allergens
Avoid contact allergens Group psychotherapy
Group psychotherapy Low-level laser therapy (diode)
Low-level laser therapy (diode)