Bradyarrhythmias
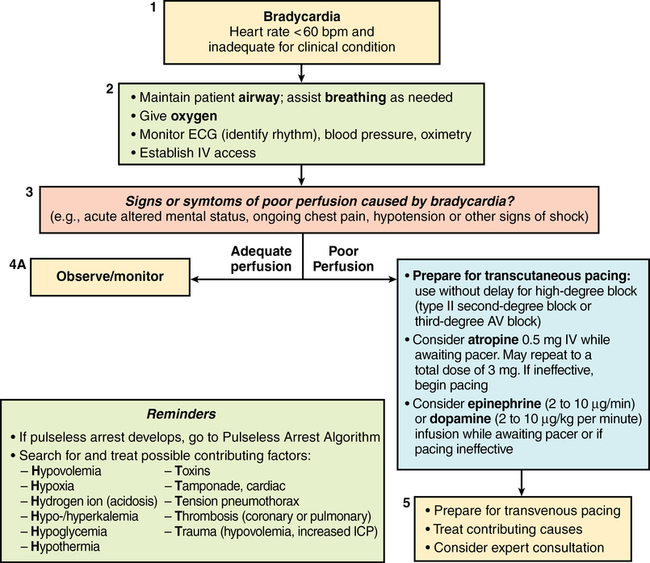
Regardless of the presentation, bradycardia should be treated immediately if hypotension or signs of hypoperfusion (e.g., acute altered mental status, seizures, syncope, ischemic chest pain, or congestive heart failure) are present. The goal of initial therapy is to administer a chronotropic drug, such as atropine or glycopyrrolate, that treats bradycardia of any cause. Patients with bradycardia that is unresponsive to atropine or glycopyrrolate are candidates for treatment with external or transvenous pacing if hypotension or hypoperfusion persists. Pacing devices provide controlled heart rate management without the risk of adverse effects associated with medications. Pharmacologic alternatives to atropine (second-line drug therapy) include dopamine, epinephrine, and isoproterenol, all of which can be titrated to the heart rate response. Isoproterenol, a pure β-sympathomimetic agent, increases myocardial oxygen demand and produces peripheral vasodilation, both of which are poorly tolerated in patients with acute myocardial ischemia. Glucagon can be used to treat patients with symptomatic bradycardia related to an overdose of β-receptor or calcium channel blocking agents (Table 37-1).
Table 37-1
Intravenously Administered Pharmacologic Treatment of Bradycardia
| Medication | Dose |
| Atropine* | 0.5 mg q 3-5 min to a maximum total dose of 3 mg Doses of atropine sulfate of < 0.5 mg may paradoxically result in further slowing of the heart rate. |
| Dopamine | Initial: 5 μg·kg−1·min−1 Titrate to response |
| Epinephrine | Initial: 2-10 μg/min Titrate to response |
| Isoproterenol | Initial: 2 to 10 μg/min Titrate to response |
| Glucagon | Initial: 3 mg Infusion: 3 mg/h, if necessary |
*Atropine administration should not delay implementation of external pacing for patients with poor perfusion.
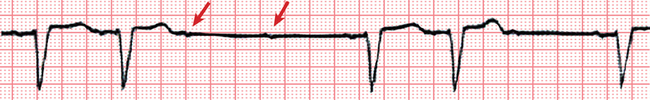
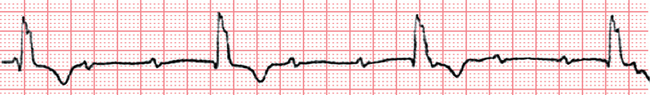
Patients with sinus bradycardia, AV junctional rhythm, or Mobitz I second-degree AV block (Figure 37-1) presenting with strong vagal tone and slow sinus node discharge or impaired AV node conduction will generally respond to treatment with atropine. Patients with complete heart block and an AV junctional escape rhythm will also respond to treatment with atropine. However, in patients with Mobitz II second-degree AV block (Figure 37-2) or new-onset wide QRS complex complete heart block (Figure 37-3), the heart block is usually infranodal, and increased vagal tone is not a significant cause of the bradycardia. These rhythms are less likely to respond to treatment with atropine; therefore, cardiac pacing is the treatment of choice.
Patients with Mobitz II second-degree AV block, even if asymptomatic, can progress without warning to complete heart block with a slow and unstable idioventricular rhythm; external pacing electrode pads or transvenous pacing electrodes should be placed prophylactically in this group of patients. Transcutaneous pacing is noninvasive but can be painful and may fail to produce effective mechanical capture. Transvenous (endocardial) pacing is accomplished by passing a pacing electrode into the right ventricle directly through a central vein catheter or through a pacing pulmonary artery catheter (if the catheter is already in place). The American Heart Association algorithm for bradycardia (Figure 37-4) provides a convenient framework for managing patients with bradycardia.