Bacteria and Archaea
After reading this chapter, the student will be able to:
• Identify bacterial shapes and arrangements
• Discuss the basis of bacterial growth
• Explain the bacterial population growth curve
• Discuss factors that influence microbial growth
• Describe methods for measuring microbial growth
• Discuss the nutritional requirements for bacterial growth
• Discuss replication and expression of bacterial DNA
• Describe bacterial mutations and genetic transfer
• Describe the criteria used in the classification of bacteria
• Discuss medically important bacteria and their classification according to Bergey’s Manual
Bacterial Structure
Shapes
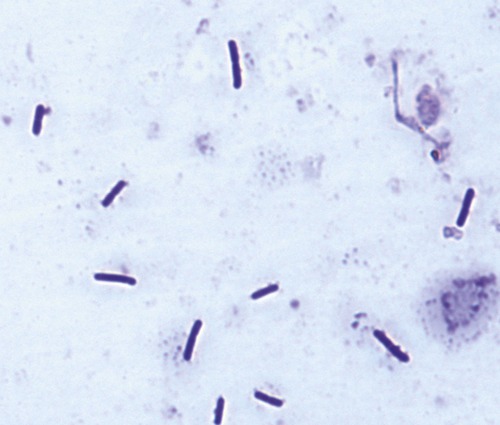
Bacterial cell morphology displays a variety of different shapes and sizes (Figure 6.1), and the cells are generally much smaller than eukaryotic cells. According to their morphological characteristics most bacteria are classified into different basic shapes: coccus, bacillus, spirochetes (spiral or helical), and pleomorphic (see Chapter 4, Microbiological Laboratory Techniques).
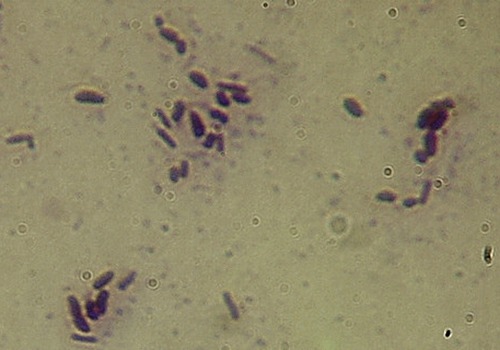
• Cocci (singular, coccus) are bacteria whose overall shape is spherical or nearly spherical (Figure 6.2). Several cocci are human pathogens causing, for example, urinary tract infections, food poisoning, toxic shock syndrome, gonorrhea, some forms of meningitis, throat infections, pneumonias, and sinusitis.
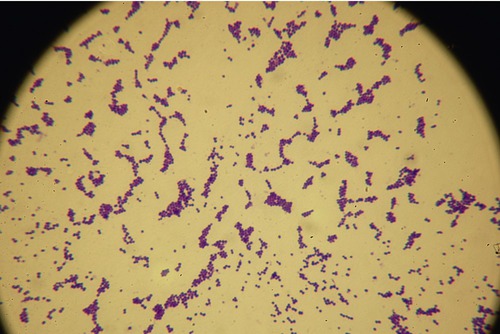
This gram-positive coccus, appearing as grapelike clusters, is one of the most common causes of staph infections.
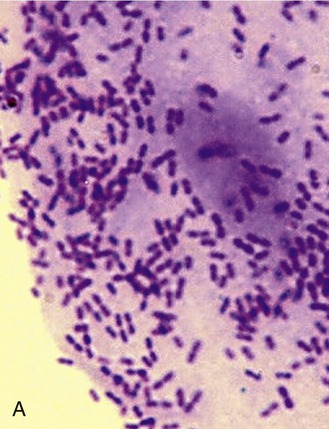
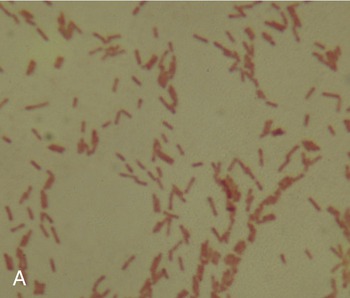
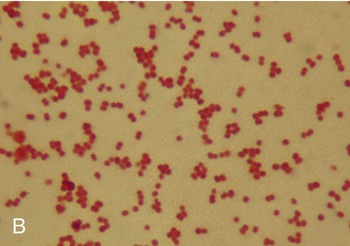
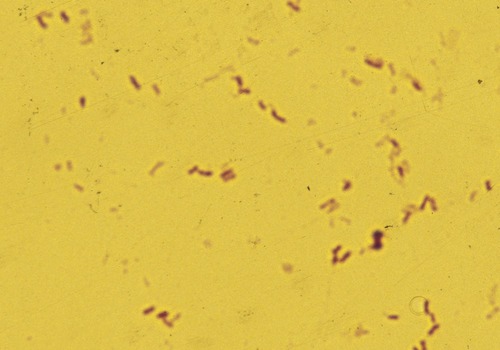
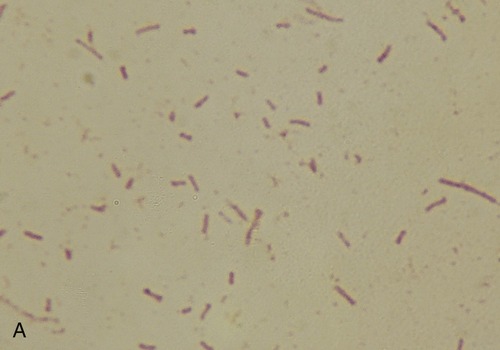
• Bacilli (singular, bacillus) are rod-shaped bacteria, some of which are endospore forming (Figure 6.3). Diseases caused by bacilli include anthrax, botulism, and tetanus, and gastrointestinal infections caused by bacilli such as Escherichia coli and Salmonella.
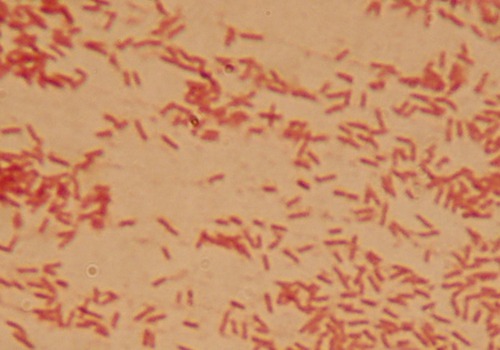
This micrograph shows a Gram stain of E. coli, a typical gram-negative bacillus.
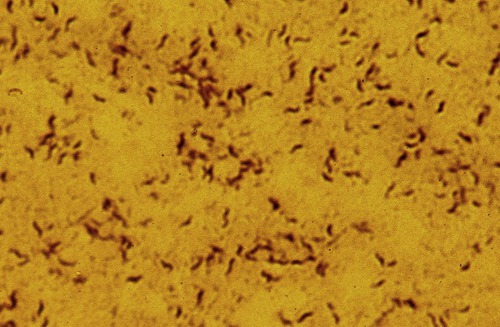
• Pleomorphic bacteria are bacterial species that are morphologically indistinct, depending on environmental conditions. This group includes Coccobacillus (coccobacilli), which are bacilli that are elongated as well as spherical in shape (Figure 6.4).
This micrograph illustrates a Gram stain of an organism from the genus Corynebacterium. The cells are variable in shape, from spheres to short rods, and therefore are considered pleomorphic (cells with a variable or indistinct shape).
• Spirals occur as vibrios, spirilla, or spirochetes.
• Vibrios are curved or comma-shaped rods (Figure 6.5) and several species are human pathogens associated with gastroenteritis, cholera, food poisoning, and septicemia. Vibrio fischeri and V. harveyi are symbiotes of marine organisms such as jellyfish and produce light via bioluminescence.
The micrograph shows a Gram stain of Vibrio natriegens, demonstrating the vibrioid shape, a simple curved rod. Note that not all cells appear curved, due to the viewing of the cells on the side with the convex/concave faces of the cell pointing directly at or away from the viewer.
• A spirillum (plural, spirilla) is a thick, rigid, spiral organism (Figure 6.6) that can cause rat bite fever, an uncommon but worldwide condition caused by rodent bites. These bacteria are present in the oropharyngeal flora of approximately 50% of healthy wild and laboratory rats, as well as in other rodents.
This micrograph is taken from a Gram stain of the genus Campylobacter, showing the corkscrew or “snakelike” shape referred to as spirilla. Although a spirilla and a spirochete may appear very similar in overall shape, the spirilla often have flagella as a means of locomotion, whereas the spirochetes have a structure called an axial filament that facilitates movement and lack flagella.
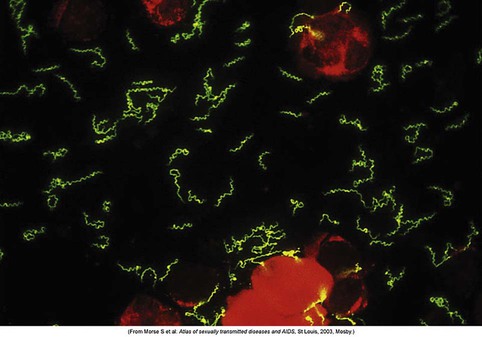
• Spirochetes are thin, flexible spirals (Figure 6.7) and can cause leptospirosis, Lyme disease, and syphilis.
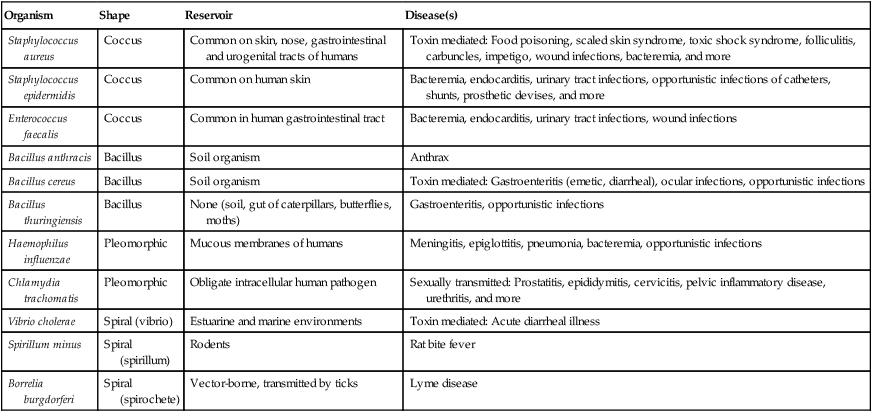
HEALTHCARE APPLICATION
Examples of Pathogens and Opportunistic Pathogens by Shape
| Organism | Shape | Reservoir | Disease(s) |
| Staphylococcus aureus | Coccus | Common on skin, nose, gastrointestinal and urogenital tracts of humans | Toxin mediated: Food poisoning, scaled skin syndrome, toxic shock syndrome, folliculitis, carbuncles, impetigo, wound infections, bacteremia, and more |
| Staphylococcus epidermidis | Coccus | Common on human skin | Bacteremia, endocarditis, urinary tract infections, opportunistic infections of catheters, shunts, prosthetic devises, and more |
| Enterococcus faecalis | Coccus | Common in human gastrointestinal tract | Bacteremia, endocarditis, urinary tract infections, wound infections |
| Bacillus anthracis | Bacillus | Soil organism | Anthrax |
| Bacillus cereus | Bacillus | Soil organism | Toxin mediated: Gastroenteritis (emetic, diarrheal), ocular infections, opportunistic infections |
| Bacillus thuringiensis | Bacillus | None (soil, gut of caterpillars, butterflies, moths) | Gastroenteritis, opportunistic infections |
| Haemophilus influenzae | Pleomorphic | Mucous membranes of humans | Meningitis, epiglottitis, pneumonia, bacteremia, opportunistic infections |
| Chlamydia trachomatis | Pleomorphic | Obligate intracellular human pathogen | Sexually transmitted: Prostatitis, epididymitis, cervicitis, pelvic inflammatory disease, urethritis, and more |
| Vibrio cholerae | Spiral (vibrio) | Estuarine and marine environments | Toxin mediated: Acute diarrheal illness |
| Spirillum minus | Spiral (spirillum) | Rodents | Rat bite fever |
| Borrelia burgdorferi | Spiral (spirochete) | Vector-borne, transmitted by ticks | Lyme disease |
Arrangements
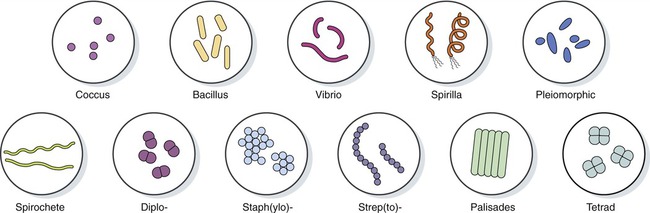
• Aggregations of cocci occur after cell division and can be classified as the following (Figure 6.8):
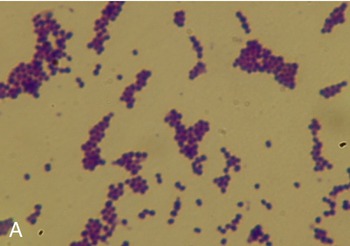
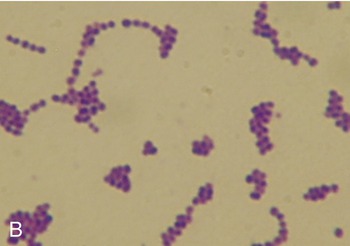
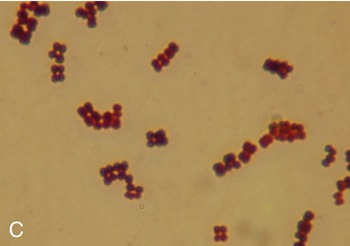
Cocci occur in five basic arrangements: diplo, in pairs; staph(ylo), in grapelike irregular clusters; strep(to), in chains; tetrads, in squares of four; and sarcinae, three-dimensional cubes. A, Staphylococcus; B, Streptococcus; C, Micrococcus in tetrads.
• Diplo– is a prefix typically describing cells that occur in pairs of two, joined in one plane only. Examples of diplococci are Streptococcus pneumoniae, Neisseria gonorrhoeae, and Neisseria meningitidis.
• Strepto– is a prefix used to indicate an arrangement of cells in beadlike chains, because cell division occurs along a single axis, in contrast to staphylococci, which divide along multiple axes. Individual species of Streptococcus are identified primarily on the basis of their hemolytic properties on blood agar. The species Streptococcus pyogenes is responsible for strep throat, many cases of meningitis, bacterial pneumonia, endocarditis, erysipelas (acute skin infection), and necrotizing fasciitis (“flesh-eating” infections).
• Tetrads are produced by division within two planes, with the cocci arranged in squares of four in irregular clusters. Micrococcus luteus, which can be found in many areas including the human skin, water, dust, and soil, shows this growth pattern. It is considered to be a harmless bacterium but some cases of Micrococcus infections have been reported in people with a compromised immune system (e.g., HIV patients).
• Sarcinae are cocci arranged in cubes of eight as a result of division in three planes. This coccal grouping occurs when any cocci fail to separate after they divide and the resultant daughter cells remain attached.
• Staphylo– is a prefix indicating arrangements in grapelike clusters formed by cell division in random planes. Most members of the genus Staphylococcus are harmless and are part of the normal flora of the skin and mucous membranes in humans. A small percentage of staphylococci are also part of the soil microbial flora. The organism can cause an array of diseases in humans and other animals by invasion and also by toxin production. The toxins of Staphylococcus are a common cause of food poisoning because the bacteria can grow in improperly stored food. Although the organism is killed by the cooking process, the enterotoxin is heat resistant and can survive boiling for several minutes.
• Bacilli divide in one plane, producing diplobacilli and streptobacilli (Figure 6.9).
Bacterial Growth
Growth is an increase in the quantity of cellular material and depends on the ability of the cell to form new protoplasm from available nutrients. Bacterial growth requires a source of energy for protein synthesis and to maintain bacterial metabolism. Bacteria must obtain or synthesize nucleic acids, carbohydrates, and lipids that are used as building blocks of cells. The minimal requirements for growth are a source of carbon and nitrogen, an energy source, water, and a variety of ions and minerals. Oxygen is necessary for some bacteria but can be lethal for many others (see Atmospheric Conditions, later in this chapter).
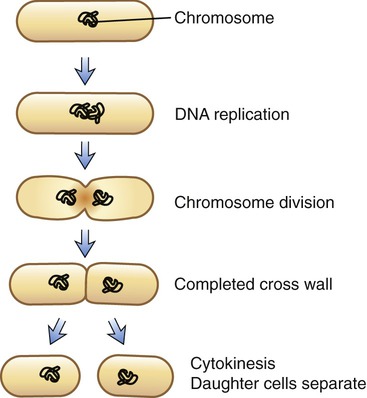
Basis of Bacterial Growth: Binary Fission
Bacterial replication is a coordinated process accomplished primarily by binary fission. Binary fission results in two identical daughter cells (Figure 6.10). In order for growth to occur sufficient metabolites are necessary to support the synthesis of bacterial components. A cascade of regulatory events must occur to initiate replication. Once replication is started DNA synthesis must run to completion. Chromosome replication starts at the plasma membrane and each daughter chromosome is anchored to a different portion of the membrane. Membrane, peptidoglycan synthesis, and cell division are linked together and as the bacterial membrane grows, the daughter chromosomes are pulled apart. At the end of chromosome replication septum formation between the daughter cells starts, indicating cell division (see Chapter 3, Cell Structure and Function). New initiation may begin even before chromosome duplication and cell division are complete.
Population Growth Curve
To produce a bacterial culture in a laboratory environment, the organism must be added to a medium (see Types of Culture Media in Chapter 4, Microbiological Laboratory Techniques). Under favorable conditions a growing bacterial culture doubles at regular intervals. Under ideal conditions, bacterial growth can be described by four different phases: the lag phase, the exponential or logarithmic growth phase, the stationary phase, and the death phase (Figure 6.11).
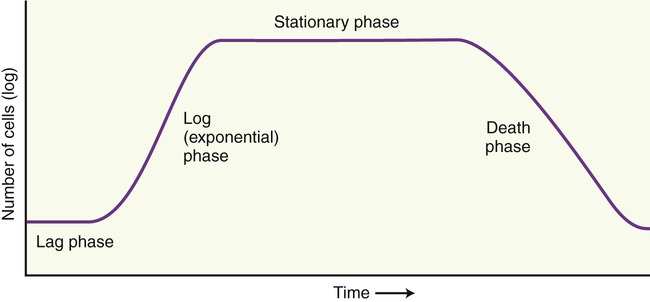
Bacterial growth can be described by four different phases: the lag phase, the exponential or logarithmic growth phase, the stationary phase, and the death phase.
• Lag phase: Bacteria must adapt to the medium before cell division starts. This period of time is referred to as the lag phase of the bacterial growth curve. During this phase the cells are metabolically active, producing molecules necessary for cell division; the individual bacteria are maturing, yet they are not able to divide at this time.
• Logarithmic or exponential growth phase: The rate of growth increases with time in the so-called logarithmic or exponential growth phase. Each cell introduced to the medium divides by binary fission into two cells. With each subsequent binary fission a doubling of the bacterial cells occurs as long as the growth conditions are favorable. The time required for doubling of the population is called the generation time. In other words the number of new bacteria per unit of time is proportional to the present population, and the actual rate of growth depends on the growth conditions, which directly affect the frequency of cell division.
• Stationary phase: A stationary phase occurs when essential nutrients are depleted or by-products of metabolism accumulate. A depletion of nutrients causes cells to decrease in size and toxic metabolic by-products limit the ability to undergo cell division. During this phase the total number of viable cells remains constant. This phase of population growth can last for a few hours to several days, depending on the environmental conditions.
• Death phase: Finally, the death phase begins when growth stops and the number of dead cells is larger than the number of viable cells.
Measuring Growth
Measurement of Cell Mass
• Dry weight measurements allow a more accurate estimation of cell masses but are more time consuming and only useful when dealing with massive populations of cells. With this procedure the cells need to be washed thoroughly and then dried before weighing. The dry weight of cells is roughly 20% to 25% of their wet weight.
• Microbial growth in liquid media causes turbidity and can be measured with a spectrophotometer. The turbidity is measured in optical density (OD) units, which is the logarithm of the ratio of intensity of light striking the suspension to the amount that is transmitted. The greater the cell mass the less light will pass through the spectrophotometer, an instrument that can measure light intensity. Measurement of very large populations will require dilution in order to obtain accurate estimates of cell mass.
Measurement of Cell Number
• Direct (total) cell counts can be obtained microscopically in counting chambers known as Petroff-Hauser chambers (Figure 6.12). Such a chamber consists of a slide with a grid of 25 small squares etched within 1 mm2 under a coverslip.

Several different slide counting chambers are available including the Petroff-Hausser chamber, the Sedgwick-Rafter chamber, and the Neubauer chamber (pictured).
• Viable counts only count the viable cells in a culture and can be accomplished by:
Factors Influencing Microbial Growth
Nutritional Requirements
The nutritional requirements for different microbes vary significantly from one to another. Microorganisms that acquire energy from light are called phototrophs, and those that require chemical compounds for energy are called chemotrophs. The pathways for the generation of cellular energy are photosynthesis, fermentation, and respiration (see Chapter 3, Cell Structure and Function).
• Photoautotrophs use sunlight as the energy source and atmospheric carbon dioxide as their carbon source. Photoautotrophs include photosynthetic bacteria, algae, and green plants. They transform carbon dioxide and water into carbohydrates and oxygen by way of photosynthesis.
• Chemoautotrophs use inorganic chemical compounds as the source of energy and carbon dioxide as the carbon source.
• Photoheterotrophs use sunlight for energy, but cannot convert carbon dioxide into energy; instead, they use organic compounds as the source for carbon.
• Chemoheterotrophs use organic compounds for both the source of energy and a carbon source. Some chemoheterotrophs such as Pseudomonas can use many different organic compounds as energy and carbon source, and therefore can grow in many different environments such as in soap dispensers. This makes this organism a particular problem in hospital environments, where Pseudomonas can also grow in respiratory equipment.
Temperature
Most microorganisms can grow in a wide range of temperatures, but optimal growth occurs within a narrow range. The minimal growth temperature is the lowest temperature that supports the growth of an organism, and the maximal growth temperature is the highest temperature that allows growth. The optimal growth temperature is the range of temperature that provides ideal conditions for the growth of a particular microbe. Depending on the range of temperature in which a microbe will grow, they are classified as mesophiles, thermophiles, psychrophiles, and psychrotrophs (Table 6.1).
TABLE 6.1
Examples of Bacteria Growing at Different Temperatures
| Pathogens | Nonpathogens | |
| Mesophiles | Salmonella typhi | Micrococcus luteus |
| Thermophiles | Campylobacter spp. | Bacillus thermophilus |
| Psychrophiles | Yersinia enterocolitica | Pseudomonas spp. |
| Psychrotrophs | Listeria monocytogenes | Bacillus spp. |
• Mesophiles: Mesophiles are microorganisms that have optimal growth in moderate temperature, generally between 25° C and 40° C. The habitats of these organisms include soil, the human body, and animals. They also play an important role in food preparations such as the production of cheese and yogurt, as well as beer and wine production. Most medically important bacteria are mesophiles, and pathogenic organisms generally grow best at temperatures that are optimal for the cells of the host. In the laboratory environment these microbes are generally grown in incubators set at 37° C (human body temperature). Bacteria of the normal human flora are mesophiles.
• Thermophiles: These heat-loving organisms grow best at temperatures of 45° C or higher. Examples of such environments include hot springs, deep sea hydrothermal vents, tropical soil composts, and decomposing hay stacks. Some bacteria grow in water-boiling environments up to 110° C. Most photosynthetic prokaryotes are limited to environments of 70° C to 73° C, and most eukaryotic microbes cannot grow above 60° C.
• Psychrophiles (cryophiles): These bacteria are cold-loving and can grow at 0° C or lower, with an optimal growth around 15° C. They are usually found in Arctic and Antarctic regions and in streams that are fed by glaciers.
• Psychrotrophs: These organisms grow very slowly at 0° C but have an optimal growth range of 25° C to 30° C. Psychrotrophs are not considered to be psychrophiles. They are abundant in nature and can cause food spoilage at refrigerator temperatures.
Atmospheric Conditions
Prokaryotes exist in nature under various physical conditions including different oxygen concentrations in the atmosphere (Table 6.2). It is necessary to know the atmospheric requirement of microorganisms when obtaining, transporting, and culturing microbes. Metabolic pathways or organisms often require oxygen to generate ATP molecules, but some pathways can produce energy without the presence of oxygen, and some organisms will be killed in the presence of oxygen.
TABLE 6.2
Examples of Bacteria Growing Under Different Atmospheric Conditions
| Pathogens | Nonpathogens | |
| Obligate aerobes | Mycobacterium leprae | Pseudomonas fluorescens |
| Obligate anaerobes | Clostridium botulinum | Clostridium sporogenes |
| Aerotolerant anaerobes | Fusobacterium spp. | Bifidobacterium spp. |
| Facultative anaerobes | Escherichia coli | Staphylococcus epidermidis |
| Microaerophiles | Campylobacter jejunae | Thiovuhlum majus |
| Capnophiles | Neisseria gonorrhoeae | Mannheimia succiniciproducens |
• Obligate aerobes are organisms that grow only in the presence of oxygen and therefore they obtain their energy through aerobic respiration.
• Obligate anaerobes grow only in the absence of oxygen and are often inhibited or killed by the presence of oxygen. They obtain their energy through anaerobic respiration or fermentation.
• Aerotolerant anaerobes cannot use oxygen for energy requirements but can grow in the presence of oxygen. They can transform energy by fermentation only and are also called obligate fermenters.
• Facultative anaerobes can grow either in the absence or presence of oxygen. They use aerobic respiration in the presence of oxygen, and anaerobic respiration or fermentation in the absence of oxygen.
• Microaerophiles are organisms that require a low concentration of oxygen, about 2% to 10% (much less than atmospheric oxygen at 21%); a higher oxygen concentration will inhibit their growth. They acquire their energy through aerobic cellular respiration.
• Capneic bacteria (capnophiles) require more carbon dioxide than is present in earth’s surface atmosphere.
Genetics
• A gene is a unit that codes for particular information located on a DNA molecule. The total number of genes in an organism is called the genome. Bacteria and archaea have a smaller genome compared with eukaryotes.
• A chromosome is a single DNA molecule that includes proteins called histones in eukaryotes, but prokaryotic cells do not have a nucleus and their DNA is not associated with histones. In general, bacteria and archaea store their genomes in a single large circular chromosomal DNA molecule to be found in an area that is non-membrane bound and called the nucleoid area. In addition, many bacteria contain small extrachromosomal (nonchromosomal) DNA molecules called plasmids. Linear chromosomes and plasmids previously unknown have now been found in some species of gram-positive and gram-negative bacteria.
• A plasmid is independent from the chromosomal DNA of the organism; it is generally circular, self-replicating, and usually carries between 5 and 100 genes. Plasmids are not essential for normal bacterial growth and therefore bacteria may lose or gain plasmids without causing harm. However, plasmids often contain genes that provide a selective advantage to a bacterium under certain environmental conditions such as the presence of antibiotics, when an antibiotic resistance gene in a plasmid can code for an enzyme capable of denaturing the antibiotic. These types of plasmids provide antibiotic resistance to an increasing number of bacteria, causing serious problems in hospitals and other healthcare environments.
• An episome is a unit of genetic material composed of a series of genes, such as a plasmid, that is capable of integrating itself into the chromosomal DNA of the organism and therefore can stay intact and is duplicated with every cell division. It becomes a basic part of the genetic makeup of the organism and therefore is no longer considered a plasmid or separate unit, because it became part of the chromosomal DNA.
Genotype and Phenotype
• The genotype of an organism represents its exact genetic makeup and, in the case of bacteria, a specific species such as E. coli can have various strains, each strain with its specific and often only slightly altered genotype.
• The phenotype of an individual organism represents the observable characteristics of that organism. While an organism’s genotype has the greatest influence on the phenotype, environmental factors can somewhat alter the appearance. This phenomenon is referred to as phenotypic plasticity, describing the degree to which an organism’s phenotype is determined by its genotype. In the case of bacteria, high levels of plasticity indicate that environmental factors such as pH or temperature, or the type of medium they grow on, have a strong influence on the appearance of the bacterial culture.
• The relationship between genotype and phenotype can be simply expressed as: genotype + environment = phenotype.
Mutations
• Spontaneous mutations occur naturally with no known cause.
• Induced mutations can occur in nature through exposure to radiation or chemicals affecting the DNA. Genetic changes can also be produced in the laboratory. Physical, chemical, or biological agents that alter the DNA are called mutagens or mutagenic agents.
• Point mutations occur when a single nucleotide base is altered. A base substitution involves the replacement of one base pair with another. This type of point mutation represents the most frequent type. When a purine or a pyrimidine replaces another purine or pyrimidine base, the substitution is referred to as a transition. If a purine replaces a pyrimidine or vice versa, the substitution is called a transversion. Silent mutations occur when a codon (three-nucleotide sequence; see Chapter 2, Chemistry of Life) is changed by substitution of one base but the codon still contains the code for the same amino acid, and therefore the end product of protein synthesis is the same. However, when a base substitution codes for a different amino acid the end product is different, changing the shape and function of the protein. The consequence can be minor, harmful, or lethal.
• Frameshift mutations involve the deletion or insertion of one or more bases. This mutation results in a misreading, or shift in the reading, of the genetic code, and a different end product. For example, if the original code reads “The dog was bad” and the letter (base) “o” is deleted, the reading would end up as a nonsense message, because the codons are read in three-letter words.
• Inversions are macrolesions in which the order of bases is switched or inverted. The change in the base sequence due to inversions produces nonsense codons with a high probability of gene dysfunction.
• Transposons (jumping genes) are genes that move from one segment of DNA to another on chromosomes, on plasmids, or within viruses. They contain inverted repeat segments of bases at the ends and a transposonase gene. Transposonase is an enzyme needed to transpose the sequence. Transposons can contain other genes also, such as drug resistance genes. A transposon can insert itself into chromosomal DNA, interrupting the gene sequence, and therefore is a potential mutagen.
• Reversions are mutants that can revert back to the wild-type phenotype. This back mutation restores the original phenotype and can be due to the action of mutagens.
Genetic Transfer in Prokaryotes
• Transformation is the transfer of free DNA or genetic elements from one cell to another. This process occurs naturally in many bacterial species. Transformation is an important tool in the genetic manipulation of bacteria performed in the laboratory environment. This process is routinely used in genetic engineering.
• Transduction is the transfer of DNA from one bacterium to another, via a bacteriophage (virus). Bacteriophages transferring the genetic material are called transducing particles. Transfer of a limited number of specific genes is called specialized transduction and the transfer of any segment of DNA is generalized transduction.
• Conjugation is the transfer of genetic material during cell-to-cell contact. This process can take place between mating cells of the same species or between closely related species. In mating types the donor carries a sex pilus (F-pilus) whereas the recipient does not.
Classification of Bacteria and Archaea
Criteria
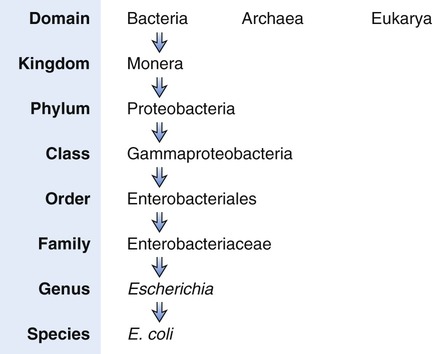
A bacterial species is defined as a group of bacteria that exhibit a large number of similar characteristics. The originally described bacterium is referred to as the prototype. Any subsequent bacterium isolated that has only a few modifications from the prototype is called a strain of the original species prototype. Bacteria are named according to the binominal system of nomenclature, which was first proposed by Carolus (Carl) Linnaeus (1707–1778), a Swedish botanist, physician, and zoologist, and who is considered to be the “father of modern taxonomy.” He classified nature within a hierarchy, starting with kingdoms, which are divided into classes and then into orders, which are divided into genera, followed by division into species (Figure 6.13).
Phenotypic classifications of bacteria involve the microscopic and macroscopic morphologies and were the first used to identify bacteria. For example, bacteria can be classified by Gram-staining properties and by the shape of the individual organism, such as gram-positive cocci. The appearance of bacterial colonies (see Chapter 4, Microbiological Laboratory Techniques) also can be used for identification of the organism. More discriminating methods can then be applied for more specific identification.
Classification According to Bergey’s Manual of Systematic Bacteriology
“Prokaryotes are described in 33 sections of the 4 volumes comprising the first edition of Bergey’s Manual of Systematic Bacteriology (a second edition is forthcoming).” This section of the chapter provides an overview of some major groups of bacteria important in human health and disease. A more complete outline is illustrated in Appendix A: Bergey’s Manual of Systematic Bacteriology.
Spirochetes
Spirochetes are a group of helical, motile bacteria with a length from 5 to 500 micrometers (µm). They are flexible and motile with twisting motions of their axial fibrils. These fibrils are a type of endocellular flagella that are wound around their cell body. Free-living spirochetes can be found in various aqueous environments and in association with human or animal hosts. Pathogenic spirochetes include Treponema pallidum, Borrelia burgdorferi, and Leptospira interrogans (Figure 6.14). Treponema is the causative agent of syphilis (see Chapter 17, Sexually Transmitted Infections/Diseases), Borrelia burgdorferi is the causative agent of Lyme disease, and Leptospira interrogans is the causative agent of leptospirosis.

Silver staining shows the tightly coiled body with hooked ends. From Murray PR, Rosenthal KS, Pfaller MA: Medical Microbiology, ed 5, St. Louis, Mosby, 2005.
HEALTHCARE APPLICATION
Pathogenic Spirochetes
| Disease | Cause | Symptoms | Treatment |
| Lyme disease | Borrelia burgdorferi | Acute: Skin rash, including “bull’s-eye” rash; fever, fatigue, headache, muscle and joint aches. Not all symptoms occur in every case of the disease Chronic: Fatigue; myalgia; neuropathy, meningitis, and more |
Antibiotics: Early stages: Doxycycline (except in children) and amoxicillin. Refractile or late stages: Prolonged treatment with ceftriaxone |
| Syphilis | Treponema pallidum | Primary, secondary, tertiary, and latent* | Antibiotics in primary and secondary stages: Penicillin, doxycycline, ceftriaxone, or azithromycin |
| Leptospirosis | Leptospira interrogans | Influenza-like symptoms; complications of hepatitis, jaundice, hemorrhage in the liver, uremia bacteriuria, aseptic meningitis; conjunctival hemorrhages | Antibiotics: Doxycycline or penicillin |
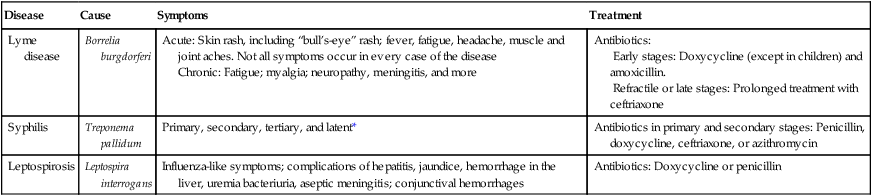
*See Chapter 17 (Sexually Transmitted Infections/Diseases).
Aerobic/Microaerophilic Helical Vibroid Gram-negative Bacteria
The helical/vibroid gram-negative bacteria are either slightly curved or have multiple helical turns. They are motile with the help of their flagella. These bacteria can live in fresh or coastal waters and some may cause disease in humans or animals. This group of bacteria includes Campylobacter, Helicobacter, Bdellovibrio, and Vampirovibrio (Table 6.3). Bdellovibrio and Vampirovibrio prey on other gram-negative bacteria and on algae.
TABLE 6.3
Medically Important Aerobic/Microaerophilic Helical Vibroid Gram-negative Bacteria
| Organism | Disease(s) |
| Campylobacter | Gastrointestinal tract infections: diarrhea, fever, and cramps |
| Helicobacter pylori | Peptic ulcers, gastritis, duodenitis |
Gram-negative Aerobic Rods and Cocci
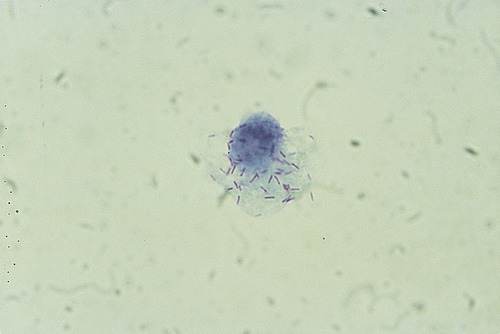
Gram-negative aerobic rods and cocci are a diverse group of bacteria that have been extensively investigated. They are widely distributed in nature and many are human and animal pathogens. Their metabolism is respiratory in nature and not based on fermentation. Bacteria in this category include Rhizobium, Legionella, Bordetella, and Francisella. Rhizobia are soil bacteria that fix nitrogen after they are established inside the roots of legumes (Figure 6.15). They cannot fix nitrogen independently, require a plant host, and play a major role in agriculture. Medically important bacteria are shown in Table 6.4.
TABLE 6.4
Medically Important Gram-negative Aerobic Rods and Cocci
| Organism | Disease(s) |
| Legionella pneumophila | Legionellosis: Pontiac fever, Legionnaires’ disease |
| Neisseria gonorrhoeae | Gonorrhea |
| Neisseria meningitidis | Meningitis |
| Bordetella pertussis | Whooping cough |
| Francisella tularensis | Tularemia |
| Pseudomonas aeruginosa | Infections in burn victims |
Facultatively Anaerobic Gram-negative Rods
Facultatively anaerobic gram-negative rods are a large group of bacteria with simple nutritional requirements. With the exception of the genus Tatumella, all motile bacteria in this group have peritrichous flagella. Bacilli are present in soil, water, and in the intestinal tract of animals and humans. Bacteria found in the intestinal tracts of humans and animals are referred to as enteric bacteria and include the genera Escherichia, Salmonella, Shigella, Enterobacter, Proteus, and Providencia (Table 6.5). The best known enteric bacterium is E. coli (Figure 6.16), which is an extremely valuable tool used in genetic engineering and recombinant DNA technology. It is often referred to as the “workhorse” in molecular biology.
TABLE 6.5
Medically Important Facultative Anaerobic Gram-negative Rods
| Organism | Disease(s) |
| Escherichia | Urinary tract infections, peritonitis, meningitis, pneumonia, septicemia |
| Salmonella | Foodborne illnesses; typhoid fever |
| Shigella | Bacillary dysentery |
| Klebsiella | Pneumonia |
| Enterobacter | Opportunistic infections, most commonly of the urinary and respiratory tracts |
| Proteus | Urinary tract infections; hospital-acquired wound infection, septicemia, pneumonia in the compromised host |
| Providenciaz | Urinary tract infections |
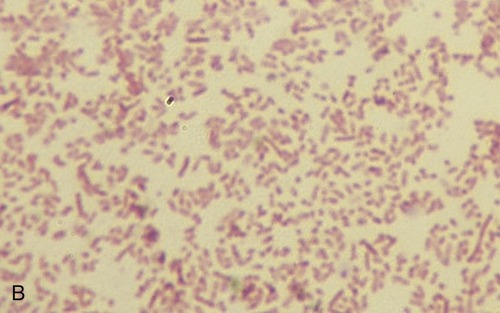
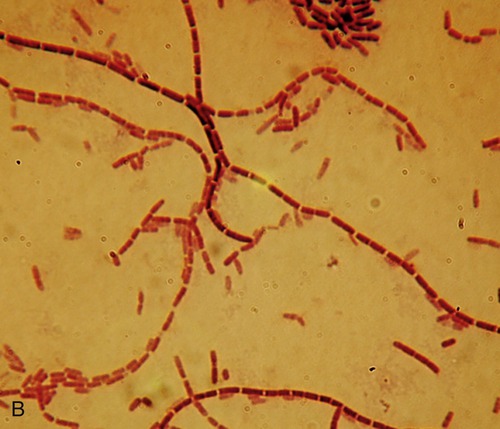
A, Gram stain of Escherichia coli. B, Gram stain of Proteus vulgaris.
Klebsiella pneumoniae is a coliform found in the normal flora of the mouth and skin, but also in the intestine, and can cause bacterial pneumonia (see Chapter 11, Infections of the Respiratory System). The genus Citrobacter can be found in many different environments including soil, water, and wastewater and can also be found in the human intestine. In general, Citrobacter does not cause illness but occasionally can be the source of urinary tract infections and infant meningitis.
Rickettsias and Chlamydias
Rickettsias and chlamydias are very small gram-negative bacteria. The majority of these organisms require a host for replication. In general, rickettsias and chlamydias are rod shaped but also may look coccoidal (Figure 6.17). Host-dependent organisms often cause diseases in humans and animals. Rickettsias need a vertebrate and an arthropod host, whereas chlamydias do not infect invertebrates but have a complex developmental cycle. Medically important organisms include Rickettsia rickettsii, Rickettsia prowazekii, Rickettsia typhi, Chlamydia trachomatis, Chlamydophila pneumoniae, and Chlamydophila psittaci (Table 6.6). Orientia tsutsugamushi is the agent of scrub typhus, a widely endemic disease in Asian Pacific regions that was formerly classified with Rickettsia. It is a gram-negative obligate intracellular bacterium belonging to the family Rickettsiaceae.
TABLE 6.6
Medically Important Rickettsias and Chlamydias
| Organism | Disease(s) |
| Rickettsia rickettsii | Rocky Mountain spotted fever |
| Rickettsia prowazekii | Epidemic typhus; recrudescent typhus, sporadic typhus |
| Rickettsia typhi | Endemic or murine typhus |
| Chlamydia trachomatis | Trachoma, adult inclusion conjunctivitis, neonatal conjunctivitis, infant pneumonia, urogenital infections, lymphogranuloma venereum |
| Chlamydofilia pneumoniae | Respiratory infections, atherosclerosis |
| Chlamydophila psittaci | Respiratory infections |
Mycoplasmas and Ureaplasmas
Mycoplasma and Ureaplasma organisms are the smallest free-living bacteria. They are unique among bacteria because they do not have cell walls, resulting in a variable or indistinct shape, and therefore are pleomorphic. They measure 0.3 to 0.8 µm in diameter and are spherical to pear shaped with branched or helical filaments. Because of the absence of the cell wall the mycoplasmas are resistant to penicillins, cephalosporins, vancomycin, and other antibiotics that interfere with cell wall synthesis. Mycoplasmas have special growth requirements and most pathogenic species are host specific. These organisms can cause disease in humans (Table 6.7), animals, and plants.
TABLE 6.7
Medically Important Mycoplasmas
| Organism | Disease(s) |
| Mycoplasma pneumoniae | Upper respiratory infections, lower respiratory infections including tracheobronchitis and bronchopneumonia |
| Mycoplasma genitalium | Nongonococcal urethritis |
| Mycoplasma hominis | Pyelonephritis, pelvic inflammatory disease, postpartum fever |
Gram-positive Cocci
Gram-positive cocci include aerobic and anaerobic spherical cells, ranging from harmless to virulent forms. These cocci include the genera Micrococcus, Staphylococcus, Streptococcus, and Peptococcus. Some medically important gram-positive cocci are shown in Table 6.8.
TABLE 6.8
Selected Medically Important Gram-positive Cocci
| Organism | Disease(s) |
| Micrococcus | Opportunistic organisms |
| Staphylococcus aureus | Minor skin infections, pneumonia, meningitis, endocarditis, toxic shock syndrome, septicemia |
| Streptococcus pyogenes | Pharyngitis (“strep throat”), scarlet fever, pyoderma, erysipelas, cellulitis, necrotizing fascilitis, streptococcal toxic shock syndrome |
| Streptococcus pneumoniae | Pneumonia, meningitis, bacteremia |
| Peptococcus and Peptostreptococcus | Opportunistic organisms |
• Micrococci are aerobic organisms not associated with disease; however; they can be opportunistic pathogens in hosts with a compromised immune system. These organisms are found in soil, water, dust, and dairy products and are part of the normal flora of the skin.
• Staphylococci are gram-positive facultative anaerobes. They can cause a wide variety of diseases in humans and other animals through their production of toxins or tissue invasion. Staphylococcus toxins are a common cause of food poisoning because of the heat resistance of the enterotoxin and the ability of staphylococci to grow in foods with relatively low water activity. Staphylococcus epidermidis (Figure 6.18) is a commensal organism of the skin, but can cause severe infections in immunosuppressed patients, in those with central venous catheters, and in patients with prosthetic limbs. The pathogenic species Staphylococcus aureus produces up to 18 extracellular products that can harm human and animal hosts. Methicillin-resistant Staphylococcus aureus (MRSA) is a specific strain that has developed resistance to all penicillins. MRSA infections occur most frequently in hospital and healthcare environments and are commonly termed as a “superbug” infections.
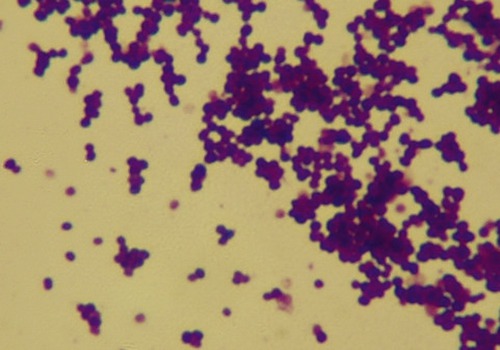
This is a gram-positive bacterium and a normal resident of the human skin; it can become an opportunistic pathogen.
• Streptococci are microaerophilic or facultatively anaerobic, organisms that produce lactic acid. The classification of Streptococcus spp. is based on the hemolytic patterns of their colonies on blood agar. Alpha hemolysis is due to the reduction of iron in hemoglobin, resulting in partial hemolysins, producing a greenish color on blood agar. Beta hemolysis is a result of complete rupture of red blood cells, resulting in clear areas around bacterial colonies on blood agar. No hemolytic action occurs with the nonhemolytic or gamma-hemolytic strains. Although a number of the Streptococcus species are pathogenic (see Table 6.8), many of the species are nonpathogenic and are part of the normal human flora of the mouth, skin, intestine, and upper respiratory tract, but can be opportunistic pathogens. Streptococcus thermophilus is not a pathogen and is used in the manufacture of Swiss cheese.
• Peptococcus and Peptostreptococcus are anaerobic gram-positive cocci and part of the normal flora in the mouth, skin, and gastrointestinal and urinary tracts. They can infect normal hosts with a compromised immune system or damaged tissues. Under these conditions the organisms can become pathogenic and can cause brain, liver, breast, and lung abscesses due to septicemia.
Endospore-forming Gram-positive Rods and Cocci
Endospore-forming rods and cocci include the genera Bacillus and Clostridium (Figure 6.19), both of which play an important role in medicine and the food industry. The spores of these genera are resistant to heat and disinfectants and both genera are widespread in the soil. Bacillus species are either obligate aerobes or facultative anaerobes; they include free-living and pathogenic species. Medically important Bacillus species include B. anthracis and B. cereus (Table 6.9). Bacillus coagulans is associated with food spoilage, B. thuringiensis is an insect pathogen, and B. subtilis is an important model organism.
TABLE 6.9
Selected Medically Important Endospore-forming Gram-positive Rods and Cocci
| Organism | Disease(s) |
| Bacillus anthracis | Anthrax (cutaneous, gastrointestinal, inhalation) |
| Bacillus cereus | Gastroenteritis, ocular infections |
| Clostridium botulinum | Botulism |
| Clostridium difficile | Antibiotic-associated diarrhea, pseudomembranous colitis |
| Clostridium perfringens | Gas gangrene, suppurative myositis, myonecrosis, gastroenteritis, food poisoning, necrotizing enteritis |
| Clostridium tetani | Tetanus |
Clostridium perfringens is widely distributed in the environment and can be found as a normal component of decaying matter, in marine sediment, and also in the intestinal tract of humans and other animals. Food poisoning by this organism is a fairly common intestinal intoxication caused by toxins produced by the bacterium. The source of this problem is usually food contaminated by soil or feces or inadequately heated or reheated food (see Chapter 12, Infections of the Gastrointestinal System). Clostridium tetani is found in soil as spores or as a parasite in the gastrointestinal tract of animals. The organism produces tetanospasmin, the causative agent of tetanus (see Chapter 13, Infections of the Nervous System and Senses). Clostridium botulinum can cause a severe type of food poisoning initiated by the ingestion of foods containing the organism’s potent neurotoxin, which is formed during the growth of the bacterium (see Chapter 13).
Irregular Nonsporulating Gram-positive Rods
Irregular nonsporulating gram-positive rods have unusual shapes (often cubelike), are pleomorphic, and are mostly facultative anaerobes with a few obligate aerobes. Organisms important to humans include but are not limited to the genera Actinomyces, Corynebacterium, and Propionibacterium. Propionibacterium shermanii is used in the production of Swiss cheese. Medically important organisms for this group are shown in Table 6.10.
TABLE 6.10
Selected Medically Important Irregular Nonsporulating Gram-positive Rods
| Organism | Disease(s) |
| Actinomyces | Opportunistic pathogens, particularly in the oral cavity, formation of abscesses in mouth, lungs, or gastrointestinal tract |
| Corynebacterium diphtheriae | Diphtheria |
| Propionibacterium acnes | Acne |
| Actinomyces israelii | Periodontal abscesses; lung infections |
Mycobacteria
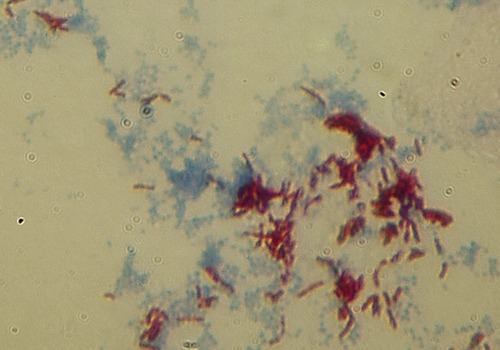
The genus Mycobacterium includes gram-positive, aerobic, acid-fast rods that have the tendency to form filaments (Figure 6.20). They are widespread organisms in water, soil, and food sources, whereas some are obligate intracellular parasites (usually infecting mononuclear phagocytes) in animals and humans. Although mycobacteria have a tendency to be difficult to grow in culture, they are classified into two categories, the fast-growing type and the slow-growing type, based on laboratory growth characteristics. In general, mycobacteria can colonize in the host without showing signs and symptoms of host infection. Many people around the world are infected with M. tuberculosis and never develop symptoms, yet they are carriers of the disease. Mycobacterial infections usually are difficult to treat because of their cell wall structure, which is neither truly gram negative nor gram positive. This makes them naturally resistant to many antibiotics whose mechanism of action is the destruction of cell walls (e.g., penicillin). Some medically important mycobacteria are shown in Table 6.11.
TABLE 6.11
Selected Medically Important Mycobacteria
| Organism | Disease(s) |
| Mycobacterium tuberculosis | Tuberculosis |
| Mycobacterium leprae | Leprosy |
| Nontuberculous mycobacteria (NTM) | Pulmonary disease resembling tuberculosis, lymphadenitis, skin disease, or dispersed disease |
Streptomycetes
Streptomycetes are gram positive, found predominantly in the soil and in decaying vegetation, and most of them are spore forming. In general they are not pathogenic, but many of the species are important sources of antibiotics (Table 6.12). Very infrequently they cause human disease, most often manifesting itself as a localized, chronic infection of the skin and underlying soft tissue. Invasive Streptomyces infections are extremely rare.
TABLE 6.12
Streptomycetes: A Source of Antibiotics
| Organism | Antibiotic |
| Streptomyces griseus | Streptomycin |
| Amycolatopsis mediterranei | Rifamycin |
| Saccharopolyspora erythraea | Erythromycin |
| Streptomyces antibioticus | Oleandomycin |
Methanogens
Methanogens are archaea that grow in anaerobic environments such as swamps, marshes, marine sediments, sludge, and hydrothermal vents and they produce methane as a metabolic by-product. They are common in wetlands, in the intestinal tracts of ruminants and humans, and are also found in soil with oxygen depletion. They are rapidly killed by the presence of oxygen. There are more than 50 species of methanogens and some of them have been found in extreme environments such as under kilometers of ice in Greenland (see Life Application: Inside a Glacier, in Chapter 1, Scope of Microbiology) or in the hot, dry desert soil. Although methanogens have not been considered to be human pathogens, several research groups are studying methanogens as potential human pathogens, especially in connection with root canal infections. Some methanogens are in endosymbiont relationships with protozoans. Endosymbiosis occurs when one organisms is housed by another, with each of the organisms benefiting from the relationship.
Extreme Thermophiles
Extreme thermophiles are different from bacterial thermophiles because they flourish in extreme heat, with optimal growth temperatures of 50° C or more, and some of them can grow at temperatures up to 150° C under extreme hydrostatic pressure such as in the deep ocean springs. Some of them also can grow in highly acidic environments. These organisms have been of great use in biotechnology because enzymes isolated from thermophiles are able to function under temperatures that would normally denature the enzymes of other organisms. Some of these enzymes are used in the polymerase chain reaction (PCR), a technique of enzymatically replicating small amounts of DNA or DNA fragments (see Chapter 25, Microorganisms in Biotechnology). PCR is commonly used in medical and biological research laboratories for the detection of hereditary diseases, identification of DNA fingerprints, diagnosis of infectious diseases, cloning of genes, paternity testing, and more.
Summary
• Bacteria are prokaryotic unicellular organisms capable of living as an individual cell or attached to others, forming colonies or groupings.
• On the basis of their morphological characteristics they are classified into basic shapes: coccus, spherically shaped; bacillus, rod shaped; spiral, twisted or helical rods; or pleomorphic, variable or indistinct in shape.
• According to their arrangements and grouping after cell division bacteria can be categorized as follows: diplo, in pairs; strep(to), in chains; tetrads, in packets of four; sarcina, in a cube; staph(ylo), in irregular clumps or clusters.
• Bacteria divide primarily by binary fission and their population growth curve can be divided into a lag phase, a logarithmic or exponential growth phase, a stationary phase, and a death phase.
• Bacterial growth can be measured by the increase in cell mass or numbers. Methods include dry weight measurement, turbidity in liquid media, direct cell counts, and viable plate counts.
• Bacterial growth is dependent on nutrient availability as well as the presence of oxygen or absence of oxygen. Depending on the need for oxygen, bacteria are organized as follows: obligate anaerobes, where oxygen is lethal; obligate aerobes, oxygen is required; facultative anaerobes (facultative aerobes), oxygen is not required but its presence benefits the organism’s growth; microaerophiles, oxygen is required but in small amounts; or aerotolerant anaerobes, oxygen is not required and its presence neither hinders nor helps the growth of the organism.
• Depending of the source of carbon necessary for bacterial growth, bacteria are classified as photoautotrophs, chemoautotrophs, photoheterotrophs, and chemoheterotrophs.
• Depending on the range of temperature at which bacteria will grow, they are classified as mesophiles, 25° C to 40° C; thermophiles, 45° C and above; psychrophiles, 0° C to 15° C; and psychrotrophs, 25° C to 30° C.
• Bacterial and archaeal chromosomal DNA is a single large circular molecule. These organisms also contain DNA independent of the chromosomal DNA, called plasmids, which are generally smaller, circular, self-replicating, and independent of cell division.
• Mutations in bacteria can be classified according to the type of change occurring in the DNA. These changes include point mutations, frameshift mutations, inversions, transposons, and reversions.
• Bacteria can obtain new genetic material from another closely related organism by transformation, transduction, or conjugation.
• Bacteria are named according to the binomial system of nomenclature and are generally classified according to Bergey’s Manual of Systematic Bacteriology.
Review Questions
1. Straight, rod-shaped bacteria, some of which are endospore forming, are referred to as:
2. Beadlike chains of cocci formed after cell division along a single axis are called:
3. Bacteria that use oxygen, but only at low concentration, are classified as:
4. Bacteria that use organic compounds for both the source of carbon and energy are referred to as:
5. Microorganisms that show optimal growth at moderate temperatures (between 25° C and 40° C) are called:
6. A mutation that involves the deletion or insertion of one or more bases is a:
7. Treponema pallidum and Borrelia burgdorferi belong to the group of:
a. Gram-negative aerobic rods and cocci
b. Anaerobic gram-negative rods
8. Legionella and Neisseria are examples of:
9. Staphylococci and streptococci are best classified in the group of:
10. Which of the following is a host-dependent bacterium?
11. Bacteria whose overall shape is spherical or nearly spherical are referred to as __________.
12. Microorganisms that acquire energy from light are called __________.
13. Microorganisms that grow only in the presence of oxygen are called __________.
14. Nonchromosomal DNA molecules in bacteria are __________.
15. The transfer of genetic material during cell-to-cell contact is a(n) __________.
16. Describe the different stages of the bacterial population growth curve.
17. Discuss four methods to measure bacterial growth.
18. Describe the nutritional requirement for bacterial growth, with regard to carbon.