Anticholinesterases and the reversal of neuromuscular blocking agents
Classification
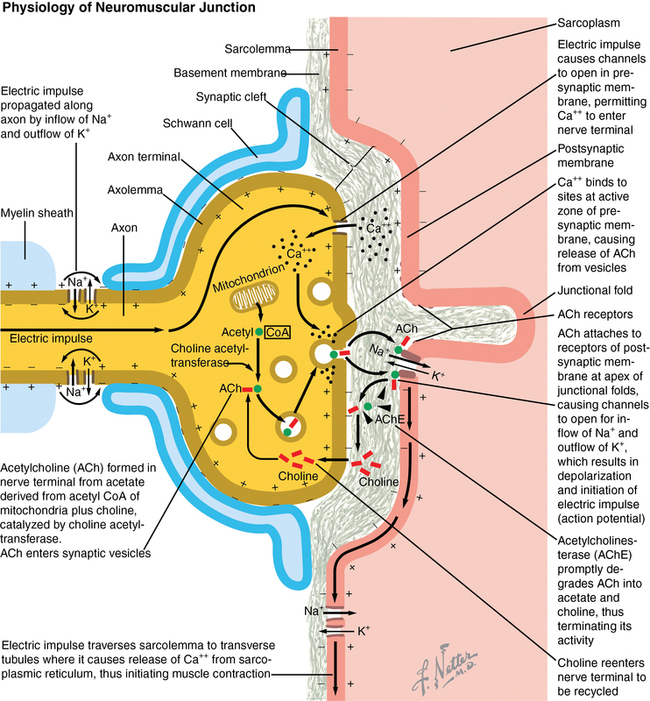
Acetylcholinesterase (AChE) inhibitors (neostigmine, pyridostigmine, physostigmine, and edrophonium) are reversible inhibitors and are commonly administered to accelerate the reversal of nondepolarizing neuromuscular blockade of nicotinic receptors in the neuromuscular junction. AChE the enzyme that metabolizes acetylcholine (ACh) into choline and acetic acid, is one of the most efficient enzymes known; a single molecule has the capacity to hydrolyze an estimated 300,000 molecules of ACh per minute. When the enzyme is inhibited, the concentration of ACh in the neuromuscular junctional cleft is increased, allowing ACh to compete for ACh receptor sites from which neuromuscular blocking agents (NMBAs) have dissociated (Figure 82-1).