CHAPTER 287 Adult Thoracolumbar Scoliosis
Adult scoliosis is defined as any lateral curvature of the spine in a skeletally mature individual with a Cobb angle of greater than 10 degrees in the coronal plane, the lumbar and thoracolumbar levels most often being affected.1 Adult scoliosis can be further divided into two main types: type 1, or curves that develop de novo after skeletal maturity, and type 2, or curves that began before skeletal maturity.2,3 Although curves of the second type may be asymptomatic in children and adolescents, they often cause symptoms of pain, radiculopathy, or both in adults from continued progression of the curve and sagittal and coronal imbalance, even after skeletal maturity.3 Osteoporosis in an adult may hasten progression of the curve and the onset of symptoms. In addition to a thorough history and physical examination, the diagnostic work-up of a patient with symptomatic adult scoliosis includes static and dynamic plain radiographs, 36-inch standing scoliosis films, magnetic resonance imaging (MRI), computed tomography (CT) myelography, or any combination of these studies. Diskography, facet blocks, and epidural steroid injections may be used as ancillary tests to further correlate the clinical symptoms with radiographic abnormalities. The decision to initiate treatment is based mostly on evidence of continued curve progression and unrelieved pain. Cosmetic concerns are less often an indication for treatment in the general adult population, although they may become more important to young adults. Nonoperative management, including exercise, nonsteroidal anti-inflammatory agents, smoking cessation, and external bracing, is aimed at alleviating symptoms but does not prevent curve progression. The goals of surgical treatment are both elimination of symptoms and restoration of spinal balance. Surgical treatment of adult scoliosis has evolved tremendously within the past 30 years, mostly as a result of advancements in spinal instrumentation by Harrington, Dwyer, Luque, Zielke, Cotrel-Dubousset, and their colleagues.4–10 More recent advancements in segmental pedicle screw-rod fixation, as well as in anesthesia and perioperative care, have further improved surgical outcomes. This chapter discusses the diagnosis, management, and clinical outcomes of patients with adult scoliosis with an emphasis on involvement of the thoracolumbar spine.
Classification and Etiology
Adult scoliosis is divided into two main types based on the timing of curve development relative to skeletal maturity.2
Type 1 (Primary Degenerative (De Novo) Scoliosis)
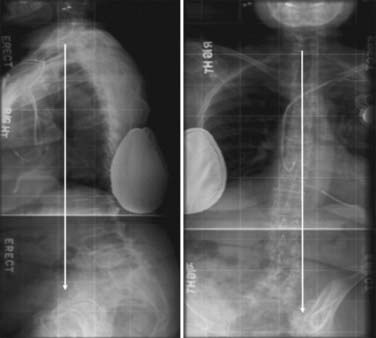
Primary degenerative, or de novo, scoliosis refers to adult scoliosis in which the curve develops in a previously straight spine after skeletal maturity and most often affects the lumbar and thoracolumbar spine. Type 1 includes scoliosis secondary to iatrogenic causes, vertebral fractures, degenerative changes, and osteoporotic disease.3 Type 1 adult scoliosis is the result of a spondylotic process in that it develops from asymmetrical degeneration of the intervertebral disk at one or more motion segments. A primary degenerative curve can also be referred to as a “diskogenic” curve.2 In addition, it can occur as a result of asymmetrical facet degeneration/hypertrophy. The asymmetrical degeneration of the intervertebral disk results in a coronal deviation with subsequent rotation of the vertebral body, which pivots on a facet joint.1 The apex of type 1 adult scoliosis curves is usually between L3 and L4, L2 and L3, or L1 and L2, in descending order of frequency. In general, de novo scoliotic curves have less of a coronal plane component than type 2, or progressive idiopathic scoliosis.11,12 Consequently, patients with primary degenerative adult scoliosis are usually affected by sagittal plane abnormalities secondary to lumbar hypolordosis or frank kyphosis (Fig. 287-1).13–16 Patients often have significant back or radicular pain (or both) as their chief complaint from this loss of normal sagittal balance. Because de novo scoliosis is primarily the result of a degenerative process, spinal stenosis from disk degeneration and facet hypertrophy is more common in these patients than in those with progressive idiopathic scoliosis.17,18
Type 2 (Progressive Idiopathic Scoliosis)
Progressive idiopathic scoliosis refers to scoliotic curves that began before skeletal maturity and includes idiopathic, congenital, and paralytic curves.3 Although idiopathic curves may be asymptomatic in children and adolescents, they often cause symptoms of pain, radiculopathy, or both in adults as a result of continued curve progression and sagittal and coronal imbalance, which occurs even after skeletal maturity (Fig. 287-2).3,19,20 In addition to pain, patients younger than 40 years have cosmetic concerns from progression of a (usually) thoracic curve.
Clinical Findings and Evaluation
Pain
Pain is the most common complaint of adults with scoliosis and is the deciding factor for surgical intervention in approximately 85% of such cases.3,14,21,22 The pain may be musculoskeletal or radicular in nature. Musculoskeletal back pain can be localized at the apex of the curve or at its concavity, and the areas above and below the curve may also be painful from excessive stress on the facet joints. This type of musculoskeletal pain is a result of both excessive strain and fatigue on the paravertebral muscles as they attempt to compensate for the loss of normal spinal balance, as well as a result of true spinal instability causing abnormal stress on the facet joints.2 Back pain is most often associated with loss of normal lumbar lordosis.23 Radicular pain is frequently encountered in patients with de novo scoliosis and is due to neural foraminal compression as a result of disk degeneration, bulging, and facet hypertrophy, especially on the concave side of the curve. Radicular pain may also be caused by traction of nerve roots on the convexity of the curve. Intercostal neuralgia secondary to rib cage deformity can be seen in patients with severe thoracic and thoracolumbar curves.3 The pain may be diffuse and constant in nature, or it may occur only with axial loading of the spine on standing. In the latter situation, the back and radicular pain is often relieved when recumbent because the spine, disks, facet joints, and neural foramina are unloaded.
The visual analogue scale should be used to quantify the severity of pain and is valuable in reporting changes in pain after treatment. The 36-item short-form health survey (SF-36) is a validated outcome measure that can be used to determine the effects of not only pain but also the scoliotic condition in general on the patient’s physical and mental well-being. SF-36 scores have been found by several authors to be significantly lower in adult scoliosis patients than in controls.24,25
Neurogenic Claudication and Neurological Deficit
Neurogenic claudication secondary to lumbar stenosis often occurs in patients with primary degenerative scoliosis.26 Long thoracolumbar curves fused to shorter lumbar or lumbosacral curves can be associated with areas of severe canal stenosis at the transition zone and resultant claudicatory symptoms.2
Curve Progression
Progression of scoliotic curves can be manifested as changes in clothing size or height or frank alterations in body shape, such as a rib hump. Progression occurs in both adult degenerative and adult idiopathic scoliosis, although it has been found to occur more quickly in the latter group.19 Risk factors for lumbar curve progression include a Cobb angle of 30 degrees or greater, significant apical rotation, lateral listhesis of 6 mm or greater, and an intercrest line through or below the L4-5 disk space.27
Diagnostic Evaluation
History and Physical Examination
The physical examination should begin with a general inspection of the patient in the standing position with knees and hips fully extended (Fig. 287-3). The location and severity of spinal curves, rib humps, sagittal and coronal balance, pelvic obliquity, curve flexibility, and any leg length discrepancies should be noted. Moreover, an assessment of hip flexibility should be performed to rule out a hip contracture as the cause of the sagittal imbalance. Improvement in posture after sitting generally indicates a hip flexion contracture. The patient should also be examined in the supine position for evidence of improvement in sagittal and coronal alignment. A rigid thoracic kyphosis is usually indicated by the persistence of a kyphotic deformity in the supine position. A thorough neurological examination is performed to assess for abnormalities resulting from compression of nerve roots or the cord (or both). Gait and reflexes should be evaluated for evidence of myelopathy from thoracic canal stenosis. A left thoracic curve, toe clawing, asymmetrical abdominal reflexes, and gait/balance difficulties may indicate that syringomyelia, a tethered cord, or a neuromuscular syndrome is the primary abnormality, and treatment should subsequently be directed at these entities.
Imaging Studies
After a thorough history and physical examination, 36-inch standing plain anteroposterior and lateral radiographs should be obtained for every adult deformity patient. For proper radiographic assessment of sagittal balance, the patient’s knees and hips must be fully extended during this examination. Dynamic lateral bending and flexion-extension radiographs are useful to assess for curve flexibility, as well as to reveal evidence of abnormal segmental motion or instability. Oblique Stagnara views can be used to evaluate kyphosis in the setting of significant rotational deformities.3
Diskography, Facet Blocks, Epidural Injections
Provocative diskography can be used as both a diagnostic and therapeutic measure for painful lumbar intervertebral disks. The presence of a positive provocative diskogram has been shown by some to be correlated with improved outcomes after lumbar fusion.28 Accordingly, provocative diskography can be helpful in identifying painful lumbar intervertebral disks that should be included in the distal construct. Facet blocks are used in similar fashion to identify painful lumbar facets that should be included in the fusion. Epidural steroid injections or nerve root blocks can also be helpful in both identifying and treating symptomatic compression of neural elements.
Nonoperative Management
Nonoperative management strategies for adult scoliosis of the thoracolumbar spine are aimed at alleviating pain in an attempt to improve functionality and quality of life. It is important for both the physician and patient to understand that nonoperative treatment does not prevent progression of the curve and that surgical intervention may be required at a later point. The foundation of nonoperative management for adult scoliosis patients is similar to that for patients without deformity and consists of relief of symptoms through the use of exercise and strength training, pain medications, and muscle relaxants.2,29,30 Swimming, low-impact aerobics, and cycling are particularly useful for older adult deformity patients.3 An external orthosis may help provide additional support for a strained, painful spine; however, there is no evidence that external bracing prevents progression of scoliotic curves in adults.3 Epidural nerve root and facet blocks may also provide temporary pain relief, but they are not the mainstay of nonoperative management.
Surgical Management
Indications
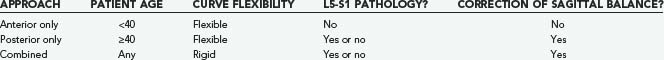
Although the timing and type of surgical intervention must be tailored to each individual patient, there are four general indications for surgical intervention in adults with a scoliotic deformity: (1) unrelieved pain, (2) progressive deformity, (3) neurological deficit, and (4) cosmesis (rare in patients younger than 40 years). Surgical strategies and techniques for decompression of neural elements and correction of deformity are divided into anterior, posterior, and combined procedures. The choice of surgical technique is dictated mainly by the characteristics of the deformity being treated, particularly the flexibility of the main curve. Unlike adolescents, in whom flexible curves are common, adult curves are generally stiff. Whatever technique is chosen, the most important goal in correcting adult scoliosis is to achieve anatomic sagittal alignment postoperatively.31 Other general principles include avoiding termination of the construct at the thoracolumbar junction or at the apex of the thoracic kyphosis. This section focuses on correction of lumbar/thoracolumbar deformities (Table 287-1). Restoration of lumbar lordosis and reestablishment of anatomic sagittal balance are important goals during correction of lumbar/thoracolumbar deformities. It should be noted that these goals can be accomplished only from a posterior approach, and consequently, indications for anterior-only approaches are relatively limited in the setting of adult scoliosis of the lumbar/thoracolumbar spine.
Anterior Approaches
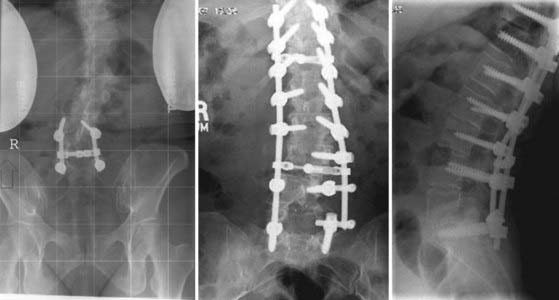
An anterior-only approach for correction of deformity is ideally suited for younger adults (20 to 40 years) with flexible lumbar/thoracolumbar curves, a healthy L5-S1 disk space, and no significant kyphotic deformity. Correction of deformity is achieved after complete diskectomy and interbody graft placement, followed by segmental bicortical vertebral body screw-rod fixation. Asymmetrical placement of an interbody graft in the anterior interbody space prevents the development of kyphosis during compression of the curve convexity (Fig. 287-4). All segments involved in the curve should be fused.
Posterior Approaches
Posterior-only approaches for correction of adult deformity are useful in older patients (≥40 years of age) with flexible lumbar/thoracolumbar curves with or without pathology of the L5-S1 disk space. It is thought that older patients have a higher risk for incisional hernia and abdominal bulging after anterior approaches than younger patients do.3 Moreover, osteopenic bone may not provide adequate fixation for vertebral body screws via an anterior-only approach, thus making pedicle screw fixation preferred for maintenance of the correction until solid arthrodesis occurs. Because of the high rates of pseudarthrosis associated with posterior-only fusions to the sacrum, an anterior interbody graft at L5-S1 can be used to provide a load-bearing interbody surface and increase arthrodesis rates at the lumbosacral junction in the setting of a degenerated or deformed L5-S1 disk space that requires fusion to the sacrum (Fig. 287-5).
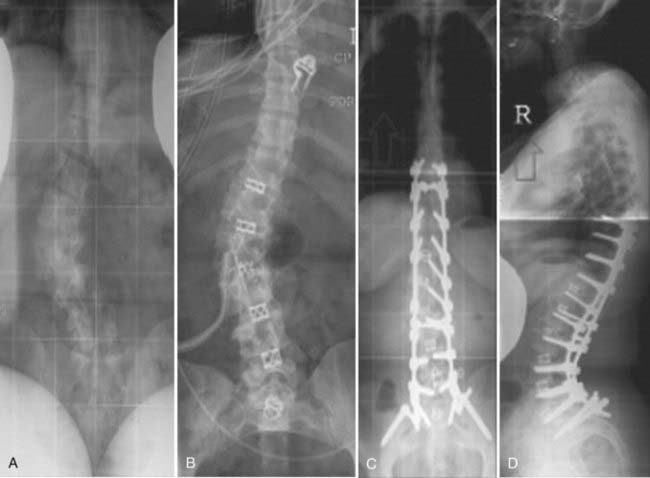
Combined (Anterior-Posterior) Approaches
Combined approaches are well suited for correction of rigid lumbar/thoracolumbar curves with or without pathology of the L5-S1 joint (Fig. 287-6). In these cases, anterior release is performed, followed by a staged or same-day posterior segmental instrumentation and fusion. Most of the correction of the deformity, including vertebral body derotation and restoration of sagittal alignment, is achieved during posterior instrumentation and fusion.
Intraoperative Considerations
Procedures for correction of scoliotic deformity are complex and lengthy operations usually place a great deal of physical stress on the patient. Significant blood loss and fluid shifts occur during the course of these procedures, and the surgeon and anesthesiologist should be prepared to deal with these problems appropriately. Suboptimal fluid management has been shown to adversely affect the recovery of patients undergoing surgery for correction of spinal deformity.32 Packed red blood cells, fresh frozen plasma, platelets, and clotting factors should be administered in a timely fashion, beginning when blood loss is estimated to approach 1000 mL. Autotransfusion with a cell salvage system is also beneficial, although large volumes of cell-salvaged blood can induce a coagulopathy.
Outcomes
When the appropriate surgical strategy is selected and tailored to the specific pathology of a particular patient, outcomes after correction of scoliotic deformity are generally quite good. Jackson and colleagues found that at an average follow-up of 5 years, 83% of patients reported early and significant relief of pain after surgery for adult idiopathic scoliosis.33 Common complications include lumbosacral pseudarthrosis and improper coronal or sagittal alignment after surgery.
Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925.
Aebi M. Correction of degenerative scoliosis of the lumbar spine. A preliminary report. Clin Orthop Relat Res. 1988;232:80.
Albert TJ, Purtill J, Mesa J, et al. Health outcome assessment before and after adult deformity surgery. A prospective study. Spine. 1995;20:2002.
Ascani E, Bartolozzi P, Logroscino CA, et al. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine. 1986;11:784.
Benner B, Ehni G. Degenerative lumbar scoliosis. Spine. 1979;4:548.
Berven S, Deviren V, Demir-Deviren S, et al. Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: validation, reliability, and discriminatory capacity. Spine. 2003;28:2164.
Bradford DS. Adult scoliosis. Current concepts of treatment. Clin Orthop Relat Res. 1988;229:70.
Colhoun E, McCall IW, Williams L, et al. Provocation discography as a guide to planning operations on the spine. J Bone Joint Surg Br. 1988;70:267.
Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10.
Dickson JH. An eleven-year clinical investigation of Harrington instrumentation. A preliminary report on 578 cases. Clin Orthop Relat Res. 1973;93:113.
Dwyer AF. Experience of anterior correction of scoliosis. Clin Orthop Relat Res. 1973;93:191.
Epstein JA, Epstein BS, Jones MD. Symptomatic lumbar scoliosis with degenerative changes in the elderly. Spine. 1979;4:542.
Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682.
Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024.
Grubb SA, Lipscomb HJ, Coonrad RW. Degenerative adult onset scoliosis. Spine. 1988;13:241.
Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine. 1994;19:1619.
Jackson RP, Simmons EH, Stripinis D. Incidence and severity of back pain in adult idiopathic scoliosis. Spine. 1983;8:749.
Kostuik JP. Decision making in adult scoliosis. Spine. 1979;4:521.
Kostuik JP, Anderson DG, Kebaish KM. Surgery for adult spinal deformity. In: Heary RF, Albert TJ, editors. Spinal Deformities: The Essentials. New York: Thieme Medical; 2007:217.
Kostuik JP, Bentivoglio J. The incidence of low-back pain in adult scoliosis. Spine. 1981;6:268.
Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res. 1982;163:192.
Luque ER. The anatomic basis and development of segmental spinal instrumentation. Spine. 1982;7:256.
Marty-Poumarat C, Scattin L, Marpeau M, et al. Natural history of progressive adult scoliosis. Spine. 2007;32:1227.
Nachemson A. Adult scoliosis and back pain. Spine. 1979;4:513.
Nahtomi-Shick O, Kostuik JP, Winters BD, et al. Does intraoperative fluid management in spine surgery predict intensive care unit length of stay? J Clin Anesth. 2001;13:208.
Robin GC, Span Y, Steinberg R, et al. Scoliosis in the elderly: a follow-up study. Spine. 1982;7:355.
Schwab F, Dubey A, Pagala M, et al. Adult scoliosis: a health assessment analysis by SF-36. Spine. 2003;28:602.
Schwab F, el-Fegoun AB, Gamez L, et al. A lumbar classification of scoliosis in the adult patient: preliminary approach. Spine. 2005;30:1670.
Schwab FJ, Smith VA, Biserni M, et al. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002;27:387.
Shapiro GS, Taira G, Boachie-Adjei O. Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical radiographic outcomes. Spine. 2003;28:358.
Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg. 2003;11:174.
Winter RB, Lonstein JE, Denis F. Pain patterns in adult scoliosis. Orthop Clin North Am. 1988;19:339.
Zielke K, Stunkat R, Beaujean F. [Ventrale derotations-spondylodesis (author’s transl).]. Arch Orthop Unfallchir. 1976;85:257.
1 Schwab F, el-Fegoun AB, Gamez L, et al. A lumbar classification of scoliosis in the adult patient: preliminary approach. Spine. 2005;30:1670.
2 Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925.
3 Kostuik JP, Anderson DG, Kebaish KM. Surgery for adult spinal deformity. In: Heary RF, Albert TJ, editors. Spinal Deformities. The Essentials. New York: Thieme Medical; 2007:217.
4 Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10.
5 Dickson JH. An eleven-year clinical investigation of Harrington instrumentation. A preliminary report on 578 cases. Clin Orthop Relat Res. 1973;93:113.
6 Dwyer AF. Experience of anterior correction of scoliosis. Clin Orthop Relat Res. 1973;93:191.
7 Luque ER. The anatomic basis and development of segmental spinal instrumentation. Spine. 1982;7:256.
8 Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res. 1982;163:192.
9 Schwab F, Dubey A, Pagala M, et al. Adult scoliosis: a health assessment analysis by SF-36. Spine. 2003;28:602.
10 Zielke K, Stunkat R, Beaujean F. [Ventrale derotations-spondylodesis (author’s transl).]. Arch Orthop Unfallchir. 1976;85:257.
11 Grubb SA, Lipscomb HJ, Coonrad RW. Degenerative adult onset scoliosis. Spine. 1988;13:241.
12 Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine. 1994;19:1619.
13 Ascani E, Bartolozzi P, Logroscino CA, et al. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine. 1986;11:784.
14 Benner B, Ehni G. Degenerative lumbar scoliosis. Spine. 1979;4:548.
15 Epstein JA, Epstein BS, Jones MD. Symptomatic lumbar scoliosis with degenerative changes in the elderly. Spine. 1979;4:542.
16 Kostuik JP, Bentivoglio J. The incidence of low-back pain in adult scoliosis. Spine. 1981;6:268.
17 Aebi M. Correction of degenerative scoliosis of the lumbar spine. A preliminary report. Clin Orthop Relat Res. 1988;232:80.
18 Nachemson A. Adult scoliosis and back pain. Spine. 1979;4:513.
19 Marty-Poumarat C, Scattin L, Marpeau M, et al. Natural history of progressive adult scoliosis. Spine. 2007;32:1227.
20 Robin GC, Span Y, Steinberg R, et al. Scoliosis in the elderly: a follow-up study. Spine. 1982;7:355.
21 Albert TJ, Purtill J, Mesa J, et al. Health outcome assessment before and after adult deformity surgery. A prospective study. Spine. 1995;20:2002.
22 Winter RB, Lonstein JE, Denis F. Pain patterns in adult scoliosis. Orthop Clin North Am. 1988;19:339.
23 Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024.
24 Berven S, Deviren V, Demir-Deviren S, et al. Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: validation, reliability, and discriminatory capacity. Spine. 2003;28:2164.
25 Schwab FJ, Smith VA, Biserni M, et al. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002;27:387.
26 Shapiro GS, Taira G, Boachie-Adjei O. Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical radiographic outcomes. Spine. 2003;28:358.
27 Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg. 2003;11:174.
28 Colhoun E, McCall IW, Williams L, et al. Provocation discography as a guide to planning operations on the spine. J Bone Joint Surg Br. 1988;70:267.
29 Bradford DS. Adult scoliosis. Current concepts of treatment. Clin Orthop Relat Res. 1988;229:70.
30 Kostuik JP. Decision making in adult scoliosis. Spine. 1979;4:521.
31 Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682.
32 Nahtomi-Shick O, Kostuik JP, Winters BD, et al. Does intraoperative fluid management in spine surgery predict intensive care unit length of stay? J Clin Anesth. 2001;13:208.
33 Jackson RP, Simmons EH, Stripinis D. Incidence and severity of back pain in adult idiopathic scoliosis. Spine. 1983;8:749.