Chapter 569 Adrenocortical Insufficiency
In primary adrenal insufficiency, congenital or acquired lesions of the adrenal cortex prevent production of cortisol and often aldosterone (Table 569-1). Acquired primary adrenal insufficiency is termed Addison disease. Dysfunction of the hypothalamus or anterior pituitary gland can cause a deficiency of corticotropin (ACTH) and lead to hypofunction of the adrenal cortex; this is termed secondary adrenal insufficiency (Table 569-2).
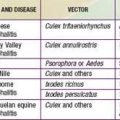
Table 569-1 CAUSES OF PRIMARY ADRENAL INSUFFICIENCY
| DIAGNOSIS | CLINICAL FEATURES IN ADDITION TO ADRENAL INSUFFICIENCY | PATHOGENESIS OR GENETICS |
|---|---|---|
| AUTOIMMUNE ADRENALITIS | ||
| Isolated autoimmune adrenalitis | No other features | Associations with HLA-DR, CTLA4 |
| Autoimmune adrenalitis as part of APS | ||
| APS type 1 (APECED) | Hypoparathyroidism, chronic mucocutaneous candidiasis, other autoimmune disorders | Mutations in AIRE |
| APS type 2 | Thyroid disease, type 1 diabetes mellitus, other autoimmune diseases (unusual in children) | Associations with HLA-DR, CTLA4 |
| APS type 4 | Other autoimmune diseases, excluding thyroid disease or diabetes (unusual in children) | Associations with HLA-DR, CTLA4 |
| INFECTIOUS ADRENALITIS | ||
| Tuberculous adrenalitis | Other organ manifestations of tuberculosis | Tuberculosis |
| AIDS | Other AIDS-associated diseases | HIV-1, cytomegalovirus |
| Fungal adrenalitis | Mostly in immunosuppressed patients | Cryptococcosis, histoplasmosis, coccidioidomycosis |
| GENETIC DISORDERS LEADING TO ADRENAL INSUFFICIENCY | ||
| Adrenoleukodystrophy, adrenomyeloneuropathy | Demyelination of CNS (cerebral adrenoleukodystrophy), spinal cord, or peripheral nerves (adrenomyeloneuropathy) | Mutation in the ABCD1 gene encoding a peroxisomal fatty acid transport protein |
| Congenital lipoid adrenal hypoplasia | XY sex reversal | Mutations in the STAR gene encoding steroidogenic acute regulatory protein; rare mutations in CYP11A encoding P-450scc |
| CYP oxidoreductase deficiency | Antley-Bixler syndrome | Mutations in POR encoding CYP oxidoreductase |
| Smith-Lemli-Opitz syndrome | Mental retardation, craniofacial malformations, growth failure | Mutations in DHCR7 encoding 7-dehydrocholesterol reductase |
| Pallister-Hall syndrome | Hypothalamic hamartoblastoma, hypopituitarism, imperforate anus, postaxial polydactyly | Mutations in GLI3 |
| IMAGe syndrome | Intrauterine growth retardation, metaphyseal dysplasia, adrenal insufficiency, genital anomalies | Unknown |
| Kearns-Sayre syndrome | External ophthalmoplegia, retinal degeneration, and cardiac conduction defects; other endocrinopathies | Mitochondrial DNA deletions |
| ACTH insensitivity syndromes (familial glucocorticoid deficiency) | Glucocorticoid deficiency, but no impairment of mineralocorticoid synthesis | |
| Type 1 | Tall stature | Mutations in MC2R encoding the ACTH receptor |
| Type 2 | No other features | Mutations in MRAP |
| Triple A syndrome (Allgrove’s syndrome) | Alacrimia, achalasia; additional symptoms, including neurologic impairment, deafness, mental retardation, hyperkeratosis | Mutations in AAAS |
| Congenital Adrenal Hyperplasia | ||
| 21-Hydroxylase deficiency | Ambiguous genitalia in girls | Mutations in CYP21A2 |
| 11β-Hydroxylase deficiency | Ambiguous genitalia in girls and hypertension | Mutations in CYP11B1 |
| 3β-hydroxysteroid dehydrogenase deficiency | Ambiguous genitalia in boys, postnatal virilization in girls | Mutations in HSD3B2 |
| 17α-Hydroxylase deficiency | Ambiguous genitalia in boys, lack of puberty in both sexes, hypertension | Mutations in CYP17 |
| Adrenal Hypoplasia Congenita | ||
| X-linked | Hypogonadotropic hypogonadism | Mutations in NR0B1 (DAX1) |
| Xp21 contiguous gene syndrome | Duchenne muscular dystrophy and glycerol kinase deficiency (psychomotor retardation) | Deletion of the Duchenne muscular dystrophy, glycerol kinase, and NR0B1 (DAX1) genes |
| SF-1 linked | XY sex reversal | Mutations in NR5A1 (SF1) |
| OTHER CAUSES | ||
| Bilateral adrenal hemorrhage | Symptoms of underlying disease | Septic shock, specifically meningococcal sepsis (Waterhouse-Friderichsen syndrome); primary antiphospholipid syndrome; anticoagulation |
| Adrenal infiltration | Symptoms of underlying disease | Adrenal metastases, primary adrenal lymphoma, sarcoidosis, amyloidosis, hemochromatosis |
| Bilateral adrenalectomy | Symptoms of underlying disease | |
| Drug-induced adrenal insufficiency | No other symptoms | Treatment with mitotane, aminoglutethimide, etomidate, ketoconazole, suramin, mifepristone, etomidate |
ACTH, adrenocorticotropin hormone; APS, autoimmune polyendocrinopathy; CYP, cytochrome P-450; P-450scc, cytochrome P-450 side chain cleavage enzyme.
Adapted from Arlt W, Allolio B: Adrenal insufficiency, Lancet 361:1881–1892, 2003.
Table 569-2 CAUSES OF SECONDARY ADRENAL INSUFFICIENCY
| DIAGNOSIS | COMMENT |
|---|---|
| Pituitary tumors | Secondary adrenal insufficiency mostly as part of panhypopituitarism; additional symptoms (visual-field impairment): generally adenomas, carcinoma is a rarity; consequence of tumor growth, surgical treatment, or both |
| Other tumors of the hypothalamic-pituitary region | Craniopharyngioma, meningioma, ependymoma, germinoma, and intrasellar or suprasellar metastases |
| Pituitary irradiation | Craniospinal irradiation in leukemia, irradiation for tumors outside the hypothalamic-pituitary axis, irradiation of pituitary tumors |
| Lymphocytic hypophysitis | |
| Isolated | Autoimmune hypophysitis; most often in relation to pregnancy (80%); mostly hypopituitarism, but also isolated adrenocorticotropic hormone deficiency |
| As part of APS | Associated with autoimmune thyroid disease and, less often, with vitiligo, primary gonadal failure, type 1 diabetes, and pernicious anemia |
| Isolated congenital ACTH deficiency |
Pro-opiomelanocortin cleavage enzyme defect? |
| Pro-opiomelanocortin-deficiency syndrome | Pro-opiomelanocortin gene mutations; clinical triad of adrenal insufficiency, early-onset obesity, and red hair pigmentation |
| Combined pituitary-hormone deficiency | Mutations in the gene encoding the pituitary transcription factor PROP1 (Prophet of Pit1), progressive development of panhypopituitarism in the order GH, PRL, TSH, LH/FSH, (ACTH) Mutations in the homeobox gene HESX1, combined pituitary hormone deficiency, optic-nerve hypoplasia, and midline brain defects (septo-optic dysplasia) |
| Pituitary apoplexy (Sheehan’s syndrome) | Onset mainly with abrupt severe headache, visual disturbance, and nausea or vomiting Histiocytosis syndromes, pituitary apoplexy or necrosis with peripartal onset, e.g., due to high blood loss or hypotension |
| Pituitary infiltration or granuloma | Tuberculosis, actinomycosis, sarcoidosis, Wegener granulomatosis |
| Head trauma | For example, pituitary stalk lesions |
| Previous chronic glucocorticoid excess | Exogenous glucocorticoid administration for >2 wk, endogenous glucocorticoid hypersecretion due to Cushing syndrome |
ACTH, adrenocorticotropin hormone; APS, autoimmune polyendocrinopathy; FSH, follicle stimulating hormone; GH, growth hormone; LH, luteinizing hormone; PRL, prolactin; TSH, thyrotropin.
Adapted from Arlt W, Allolio B: Adrenal insufficiency, Lancet 361:1881–1892, 2003.
569.1 Primary Adrenal Insufficiency
Inherited Etiologies
Inborn Defects of Steroidogenesis
The most common causes of adrenocortical insufficiency in infancy are the salt-losing forms of congenital adrenal hyperplasia (Chapter 570). Approximately 75% of infants with 21-hydroxylase deficiency, almost all infants with lipoid adrenal hyperplasia, and most infants with a deficiency of 3β-hydroxysteroid dehydrogenase manifest salt-losing symptoms in the newborn period because they are unable to synthesize either cortisol or aldosterone.
Other Genetic Causes of Adrenal Hypoplasia
The transcription factor SF-1 is required for adrenal and gonadal development (Chapter 568). Males with a heterozygous mutation in SF-1 (NR5A1) have impaired development of the testes despite the presence of a normal copy of the gene on the other chromosome and can appear to be female, similar to patients with lipoid adrenal hyperplasia (Chapter 570). Rarely, such patients have adrenal insufficiency as well.
Adrenal hypoplasia is also occasionally seen in patients with Palister-Hall syndrome caused by mutations in the GLI3 oncogene (Chapter 568).
Adrenoleukodystrophy
In adrenoleukodystrophy (ALD), adrenocortical deficiency is associated with demyelination in the central nervous system (Chapters 80 and 592.3). High levels of very long chain fatty acids are found in tissues and body fluids, resulting from their impaired β-oxidation in the peroxisomes.
Type I Autoimmune Polyendocrinopathy
Although autoimmune Addison disease most often occurs sporadically (see later), it can occur as a component of 2 syndromes, each consisting of a constellation of autoimmune disorders (Chapter 560). Type I autoimmune polyendocrinopathy (APS-1), also known as autoimmune polyendocrinopathy–candidiasis–ectodermal dystrophy (APECED) syndrome, is inherited in mendelian autosomal recessive manner, whereas APS-2 (described later) has complex inheritance. Chronic mucocutaneous candidiasis is most often the first manifestation of APS-1, followed by hypoparathyroidism and then by Addison disease, which typically develops in early adolescence. Other closely associated autoimmune disorders include gonadal failure, alopecia, vitiligo, keratopathy, enamel hypoplasia, nail dystrophy, intestinal malabsorption, and chronic active hepatitis. Hypothyroidism and type 1 diabetes mellitus occur in less than 10% of affected patients. Some components of the syndrome continue to develop as late as the 5th decade. The presence of antiadrenal antibodies and steroidal cell antibodies in these patients usually indicates a high likelihood of the development of Addison disease or, in female patients, ovarian failure. Adrenal failure can evolve rapidly in APS-1; death in patients with a previous diagnosis and unexplained deaths in siblings of patients with APS-1 have been reported, indicating the need to closely monitor patients with APS-1 and to thoroughly evaluate apparently unaffected siblings of patients with this disorder.
Disorders of Cholesterol Synthesis and Metabolism
Patients with disorders of cholesterol synthesis or metabolism, including abetalipoproteinemia with deficient lipoprotein B-containing lipoproteins, and familial hypercholesterolemia, with decreased or impaired LDL receptors, have been demonstrated to have limited adrenocortical function. Adrenal insufficiency has been reported in patients with Smith-Lemli-Opitz syndrome (SLOS), an autosomal recessive disorder manifesting with facial anomalies, microcephaly, limb anomalies, and developmental delay (Chapter 80.3). Mutations in the gene coding for sterol Δ7-reductase, mapped to 11q12-q13, resulting in impairment of the final step in cholesterol synthesis with marked elevation of 7-dehydrocholesterol, abnormally low cholesterol, and adrenal insufficiency, have been identified in SLOS. Wolman disease is a rare autosomal recessive disorder caused by mutations in the gene encoding human lysosomal acid lipase on chromosome 10q23.2-23.3. Cholesteryl esters accumulate in lysosomes in most organ systems, leading to organ failure. Infants during the 1st or 2nd mo of life have hepatosplenomegaly, steatorrhea, abdominal distention, and failure to thrive. Adrenal insufficiency and bilateral adrenal calcification are present, and death usually occurs in the first year of life.
Acquired Etiologies
Autoimmune Addison Disease
Addison disease can occur as a component of 2 autoimmune polyendocrinopathy syndromes. Type I (APS-1) was discussed previously. Type II autoimmune polyendocrinopathy (APS-2) consists of Addison disease associated with autoimmune thyroid disease (Schmidt syndrome) or type 1 diabetes (Carpenter syndrome). Gonadal failure, vitiligo, alopecia, and chronic atrophic gastritis, with or without pernicious anemia, can occur. HLA-D3 and HLA-D4 are increased in these patients and appear to confer an increased risk for development of this disease; alleles at the major histocompatibility complex class I chain-related genes A and B (MICA and MICB) also have been associated with this disorder. The disorder is most common in middle-aged women and can occur in many generations of the same family. Antiadrenal antibodies, specifically antibodies to the CYP 21, CYP 17, and CYP 11A1 enzymes, are also found in these patients. Autoimmune adrenal insufficiency may also be seen in celiac disease (Chapter 330.2).
Infection
Tuberculosis was a common cause of adrenal destruction in the past but is much less prevalent now. The most common infectious etiology for adrenal insufficiency is meningococcemia (Chapter 184); adrenal crisis from this cause is referred to as the Waterhouse-Friderichsen syndrome. Patients with AIDS can have a variety of subclinical abnormalities in the hypothalamic-pituitary-adrenal axis, but frank adrenal insufficiency is rare. However, drugs used in the treatment of AIDS can affect adrenal hormone homeostasis.
Drugs
Ketoconazole, an antifungal drug, can cause adrenal insufficiency by inhibiting adrenal enzymes. Rifampicin and anticonvulsive drugs such as phenytoin and phenobarbital reduce the effectiveness and bioavailability of corticosteroid replacement therapy by inducing steroid-metabolizing enzymes in the liver. Mitotane (o,p′-DDD), used in the treatment of adrenal carcinoma and refractory Cushing syndrome (Chapters 571 and 574), is cytotoxic to the adrenal cortex and can also alter extra-adrenal cortisol metabolism. Signs of adrenal insufficiency occur in a substantial percentage of patients treated with mitotane. Etomidate, used in the induction and maintenance of general anesthesia, inhibits 11β-hydroxylase (CYP 11B1), and a single induction dose can block cortisol synthesis for 4-8 hr or longer. This may be problematic in severely stressed patients, particularly if repeated doses are used in a critical care setting.
Clinical Manifestations
Primary adrenal insufficiency leads to cortisol and often aldosterone deficiency. The signs and symptoms of adrenal insufficiency are most easily understood in the context of the normal actions of these hormones, which were discussed in Chapter 568.
Differential Diagnosis
Upon presentation, Addison disease often needs to be distinguished from more acute illnesses such as gastroenteritis with dehydration or sepsis. Additional testing is directed at identifying the specific cause for adrenal insufficiency. When congenital adrenal hyperplasia is suspected, serum levels of cortisol precursors (17-hydroxyprogesterone) should be measured along with cortisol in an ACTH stimulation test (Chapter 570). Elevated levels of very long chain fatty acids are diagnostic of adrenoleukodystrophy. The presence of antiadrenal antibodies suggests an autoimmune pathogenesis. Patients with autoimmune Addison disease must be closely observed for the development of other autoimmune disorders. In children, hypoparathyroidism is the most commonly associated disorder, and it is suspected if hypocalcemia and elevated phosphate levels are present.
Ultrasonography, CT, or MRI can help define the size of the adrenal glands.
Treatment
After the acute manifestations are under control, most patients require chronic replacement therapy for their cortisol and aldosterone deficiencies. Hydrocortisone (cortisol) may be given orally in daily doses of 10 mg/m2/24 hr in 3 divided doses; some patients require 15 mg/m2/24 hr to minimize fatigue, especially in the morning. Timed-release preparations of hydrocortisone are undergoing clinical trials but are not yet generally available. Equivalent doses (20-25% of the hydrocortisone dose) of prednisone or prednisolone may be used and divided and given twice daily. ACTH levels may be used to monitor adequacy of glucocorticoid replacement in primary adrenal insufficiency; in congenital adrenal hyperplasia, levels of precursor hormones are used instead (Chapter 570). Blood samples for monitoring should be obtained at a consistent time of day and in a consistent relation to (i.e., before or after) the hydrocortisone dose. Normalizing ACTH levels is unnecessary and can require excessive doses of hydrocortisone; generally morning ACTH levels high in the normal range to 2-3 times normal are satisfactory. Because untreated or severely undertreated patients can acutely decompensate during relatively minor illnesses, assessment of symptoms (or lack thereof) must not be used as a substitute for biochemical monitoring. During situations of stress, such as periods of infection or minor operative procedures, the dose of hydrocortisone should be increased 2- to 3-fold. Major surgery under general anesthesia requires high intravenous doses of hydrocortisone similar to those used for acute adrenal insufficiency.
Additional therapy might need to be directed at the underlying cause of the adrenal insufficiency in regard to infections and certain metabolic defects. Therapeutic approaches to adrenoleukodystrophy include administration of glycerol trioleate and glycerol trierucate (Lorenzo’s oil), bone marrow transplantation, and lovastatin (Chapter 592.3).
Aneja R, Carcillo JA. What is the rationale for hydrocortisone treatment in children with infection-related adrenal insufficiency and septic shock? Arch Dis Child. 2007;92:165-169.
Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003;361:1881-1893.
Bornstein SR. Predisposing factors for adrenal insufficiency. N Engl J Med. 2009;360:2328-2339.
Chan LF, Clark AJ, Metherell LA. Familial glucocorticoid deficiency: advances in the molecular understanding of ACTH action. Horm Res. 2008;69:75-82.
Debono M, Ghobadi C, Rostami-Hodjegan A, et al. Modified-release hydrocortisone to provide circadian cortisol profiles. J Clin Endocrinol Metab. 2009;94:1548-1554.
Lin L, Gu WX, Ozisik G, et al. Analysis of DAX1 (NR0B1) and steroidogenic factor-1 (NR5A1) in children and adults with primary adrenal failure: ten years’ experience. J Clin Endocrinol Metab. 2006;91:3048-3054.
Lundy JB, Slane ML, Frizzi JD. Acute adrenal insufficiency after a single dose of etomidate. J Intensive Care Med. 2007;22:111-117.
Magnotti M, Shimshi M. Diagnosing adrenal insufficiency: which test is best—the 1-microg or the 250-microg cosyntropin stimulation test? Endocr Pract. 2008;14:233-238.
Marik PE, Varon J. Requirement of perioperative stress doses of corticosteroids: a systematic review of the literature. Arch Surg. 2008;143:1222-1226.
Michels AW, Eisenbarth GS. Autoimmune polyendocrine syndrome type 1 (APS-1) as a model for understanding autoimmune polyendocrine syndrome type 2 (APS-2). J Intern Med. 2009;265:530-540.
Moser HW, Mahmood A, Raymond GV. X-linked adrenoleukodystrophy. Nat Clin Pract Neurol. 2007;3:140-151.
Robles DT, Fain PR, Gottlieb PA, et al. The genetics of autoimmune polyendocrine syndrome type II. Endocrinol Metab Clin North Am. 2002;31:353-vii.
Russo C, DAvis EJ, Betts PR, Davies JH. The importance of re-evaluation, re-investigation and follow-up of adrenal insufficiency. Arch Dis Child Educ Pract Ed. 2007;92:ep109-ep113.
Shulman DI, Palmert MR, Kemp SF. Adrenal insufficiency: still a cause of morbidity and death in childhood. Pediatrics. 2007;119:e484-e494.
Ten S, New M, Maclaren N. Clinical review 130: Addison’s disease 2001. J Clin Endocrinol Metab. 2001;86:2909-2922.
Vaidya B, Chakera AJ, Dick C. Addison’s disease. BMJ. 2009;339:104-105.
569.2 Secondary Adrenal Insufficiency
Etiology
Corticotropin Deficiency
Pituitary or hypothalamic dysfunction can cause corticotropin deficiency (Chapter 551), usually associated with deficiencies of other pituitary hormones such as growth hormone and thyrotropin. Destructive lesions in the area of the pituitary, such as craniopharyngioma and germinoma, are the most common causes of corticotropin deficiency. In many cases the pituitary or hypothalamus is further damaged during surgical removal or radiotherapy of tumors in the midline of the brain. In rare instances, autoimmune hypophysitis is the cause of corticotropin deficiency.
Congenital lesions of the pituitary also occur. The pituitary alone may be affected, or additional midline structures may be involved, such as the optic nerves or septum pellucidum. The latter type of abnormality is termed septo-optic dysplasia, or de Morsier syndrome (Chapter 585.9). More-severe developmental anomalies of the brain, such as anencephaly and holoprosencephaly, can also affect the pituitary. These disorders are usually sporadic, although a few cases of autosomal recessive inheritance have occurred. Isolated deficiency of corticotropin has been reported, including in several sets of siblings. Patients with multiple pituitary hormone deficiencies caused by mutations in the PROP1 gene have been described with progressive ACTH/cortisol deficiency. Isolated deficiency of corticotropin-releasing hormone has been documented in an Arab kindred as an autosomal recessive trait.
It has recently been recognized that up to 60% of children with Prader-Willi syndrome (Chapter 76) have some degree of secondary adrenal insufficiency as assessed by provocative testing with metyrapone (see later), although diurnal cortisol levels are normal. The clinical significance of this finding is uncertain, but it can contribute to the relatively high incidence of sudden death with infectious illness that occurs in this population. Although it is not yet a standard of care, some endocrinologists advocate treating patients who have Prader-Willi syndrome with hydrocortisone during febrile illness.
Ahmad T, Borchert M, Geffner M. Optic nerve hypoplasia and hypopituitarism. Pediatr Endocrinol Rev. 2008;5:772-777.
de Lind van Wijngaarden RF, Joosten KF, van den BS, et al. The relationship between central adrenal insufficiency and sleep-related breathing disorders in children with Prader-Willi syndrome. J Clin Endocrinol Metab. 2009;94:2387-2393.
Gonc EN, Kandemir N, Kinik ST. Significance of low-dose and standard-dose ACTH tests compared to overnight metyrapone test in the diagnosis of adrenal insufficiency in childhood. Horm Res. 2003;60:191-197.
Kazlauskaite R, Evans AT, Villabona CV, et al. Corticotropin tests for hypothalamic-pituitary-adrenal insufficiency: a metaanalysis. J Clin Endocrinol Metab. 2008;93:4245-4253.
Kelberman D, Dattani MT. Role of transcription factors in midline central nervous system and pituitary defects. Endocr Dev. 2009;14:67-82.
Rose SR, Danish RK, Kearney NS, et al. ACTH deficiency in childhood cancer survivors. Pediatr Blood Cancer. 2005;45:808-813.
Zollner EW. Hypothalamic-pituitary-adrenal axis suppression in asthmatic children on inhaled corticosteroids (Part 2)—the risk as determined by gold standard adrenal function tests: a systematic review. Pediatr Allergy Immunol. 2007;18:469-474.
569.3 Adrenal Insufficiency in the Critical Care Setting
Etiology
Adrenal insufficiency in the context of critical illness is encountered in up to 20-50% of pediatric patients, often as a transient condition. In many cases, it is considered to be “functional” or “relative” in nature, meaning that cortisol levels are within normal limits but cannot increase sufficiently to meet the demands of critical illness. The causes are heterogeneous, and some were discussed in Chapter 569.1. They include adrenal hypoperfusion from shock, particularly septic shock, as is often seen in meningococcemia. Inflammatory mediators during septic shock, particularly interleukin-6, can suppress ACTH secretion, directly suppress cortisol secretion, or both. Etomidate, used as sedation for intubation, inhibits steroid 11β-hydroxylase and thus blocks cortisol biosynthesis. Neurosurgical patients with closed head trauma, or with tumors that involve the hypothalamus or pituitary, might have ACTH deficiency in the context of panhypopituitarism. Some children have been previously treated with systemic corticosteroids (e.g., children with leukemia) and have suppression of the hypothalamic-pituitary-adrenal axis for that reason. In the intensive care nursery, premature infants have not yet developed normal cortisol biosynthetic capacity (Chapter 568.2) and thus may not be able to secrete adequate amounts of this hormone when ill.
Clinical Manifestations
Cortisol is required for catecholamines to have their normal pressor effects on the cardiovascular system (Chapter 568.4). Accordingly, adrenal insufficiency is often suspected in hypotensive patients who do not respond to intravenous pressor agents. Patients may be at increased risk for hypoglycemia or a presentation resembling the syndrome of inappropriate antidiuretic hormone secretion (SIADH), but these conditions commonly occur in the context of sepsis, and the contribution of adrenal insufficiency may be difficult to distinguish.
Laboratory Findings
Although low random cortisol levels in severely stressed patients are certainly abnormal, very high levels are also associated with poor outcome such patients; the latter situation presumably reflects a maximally stimulated adrenal cortex with diminished reserve. ACTH (cosyntropin) stimulation testing is generally considered the best way to diagnose adrenal insufficiency in this setting (Chapter 569.1); evidence suggests that the low-dose (1 µg/1.73 m2) test may be superior to the 250 µg standard dose test, although this remains controversial. Generally, a peak cortisol level <18 µg/dL or an increment of <9 µg/dL from baseline is considered suggestive for adrenal insufficiency in this context. In evaluating cortisol levels, it should be remembered that cortisol in the circulation is normally mostly bound to cortisol binding globulin; in hypoproteinemic states total cortisol levels may be decreased, whereas free cortisol levels might be normal. It may be prudent to measure free cortisol before initiating treatment when total cortisol is low and albumin is <2.5 g/dL, but such measurements are not readily available in all institutions.
Aneja R, Carcillo JA. What is the rationale for hydrocortisone treatment in children with infection-related adrenal insufficiency and septic shock? Arch Dis Child. 2007;92:165-169.
Brierley J, Carcillo JA, Choong K, et al. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. 2009;37:666-688.
Cooper MS, Stewart PM. Corticosteroid insufficiency in acutely ill patients. N Engl J Med. 2003;348:727-734.
Langer M, Modi BP, Agus M. Adrenal insufficiency in the critically ill neonate and child. Curr Opin Pediatr. 2006;18:448-453.
Pizarro CF, Troster EJ, Damiani D, et al. Absolute and relative adrenal insufficiency in children with septic shock. Crit Care Med. 2005;33:855-859.